Cigna Group - Annual Report: 2021 (Form 10-K)
UNITED STATES
SECURITIES AND EXCHANGE COMMISSION
Washington, D.C. 20549
FORM 10-K
(Mark One)
| ☒ | ANNUAL REPORT PURSUANT TO SECTION 13 OR 15(d) OF THE SECURITIES EXCHANGE ACT OF 1934 | ||||
For the fiscal year ended December 31, 2021 | |||||
| OR | |||||
| ☐ | TRANSITION REPORT PURSUANT TO SECTION 13 OR 15(d) OF THE SECURITIES EXCHANGE ACT OF 1934 | ||||
For the transition period from ______________ to ______________
Commission file number 001-38769
Cigna Corporation
(Exact name of registrant as specified in its charter)
| Delaware | 82-4991898 | ||||
| (State or other jurisdiction of incorporation or organization) | (I.R.S. Employer Identification No.) | ||||
900 Cottage Grove Road, Bloomfield, Connecticut | 06002 | ||||
| (Address of principal executive offices) | (Zip Code) | ||||
(860) 226-6000 | |||||
| Registrant's telephone number, including area code | |||||
Securities registered pursuant to Section 12(b) of the Act: | ||||||||
| Title of each class | Trading Symbol(s) | Name of each exchange on which registered | ||||||
| Common Stock, Par Value $0.01 | CI | New York Stock Exchange, Inc. | ||||||
Securities registered pursuant to Section 12(g) of the Act: | ||
| NONE | ||
| Yes | No | |||||||||||||||||||
Indicate by check mark if the registrant is a well-known seasoned issuer, as defined in Rule 405 of the Securities Act. | ☒ | ☐ | ||||||||||||||||||
Indicate by check mark if the registrant is not required to file reports pursuant to Section 13 or Section 15(d) of the Act. | ☐ | ☒ | ||||||||||||||||||
Indicate by check mark whether the registrant (1) has filed all reports required to be filed by Section 13 or 15(d) of the Securities Exchange Act of 1934 during the preceding 12 months (or for such shorter period that the registrant was required to file such reports), and (2) has been subject to such filing requirements for the past 90 days. | ☒ | ☐ | ||||||||||||||||||
Indicate by check mark whether the registrant has submitted electronically every Interactive Data File required to be submitted pursuant to Rule 405 of Regulation S-T during the preceding 12 months (or for such shorter period that the registrant was required to submit such files). | ☒ | ☐ | ||||||||||||||||||
Indicate by check mark whether the registrant is a large accelerated filer, an accelerated filer, a non-accelerated filer, a smaller reporting company or an emerging growth company. See definitions of "large accelerated filer," "accelerated filer," "smaller reporting company" and "emerging growth company" in Rule 12b-2 of the Exchange Act. | ||||||||||||||||||||
| Large accelerated filer | ☒ | Accelerated filer | ☐ | Non-accelerated filer | ☐ | |||||||||||||||
| Smaller reporting company | ☐ | Emerging growth company | ☐ | |||||||||||||||||
If an emerging growth company, indicate by check mark if the registrant has elected not to use the extended transition period for complying with any new or revised financial accounting standards provided pursuant to Section 13(a) of the Exchange Act. | ☐ | |||||||||||||||||||
Indicate by check mark whether the registrant has filed a report on and attestation to its management's assessment of the effectiveness of its internal control over financial reporting under Section 404(b) of the Sarbanes-Oxley Act (15 U.S.C. 7262(b)) by the registered public accounting firm that prepared or issued its audit report. | ☒ | |||||||||||||||||||
Indicate by check mark whether the registrant is a shell company (as defined in Rule 12b-2 of the Act). | ☐ | ☒ | ||||||||||||||||||
The aggregate market value of the voting stock held by non-affiliates of the registrant as of June 30, 2021 was approximately $80.8 billion.
As of January 31, 2022, 320,953,245 shares of the registrant's Common Stock were outstanding.
DOCUMENTS INCORPORATED BY REFERENCE
Part III of this Form 10-K incorporates by reference information from the registrant's definitive proxy statement related to the 2022 annual meeting of shareholders.
TABLE OF CONTENTS
FREQUENTLY REQUESTED 10-K INFORMATION | |||||
| Page | |||||
| Page | ||||||||
| A. Directors of the Registrant | |||||||||||
| B. Executive Officers of the Registrant | |||||||||||
| C. Code of Ethics and Other Corporate Governance Disclosures | |||||||||||
| D. Delinquent Section 16(a) Reports | |||||||||||
FS-1 | |||||||||||
| Exhibits | |||||||||||
CAUTIONARY NOTE REGARDING FORWARD-LOOKING STATEMENTS
This Annual Report on Form 10-K contains forward-looking statements within the meaning of the Private Securities Litigation Reform Act of 1995. Forward-looking statements are based on Cigna's current expectations and projections about future trends, events and uncertainties. These statements are not historical facts. Forward-looking statements may include, among others, statements concerning future financial or operating performance, including our ability to deliver affordable, predictable and simple solutions for our customers and clients, including in light of the challenges presented by the COVID-19 pandemic; future growth, business strategy and strategic or operational initiatives; economic, regulatory or competitive environments, particularly with respect to the pace and extent of change in these areas; financing or capital deployment plans and amounts available for future deployment; our prospects for growth in the coming years; strategic transactions, including the sale of our international life, accident and supplemental benefits businesses; and other statements regarding Cigna's future beliefs, expectations, plans, intentions, liquidity, cash flows, financial condition or performance. You may identify forward-looking statements by the use of words such as "believe," "expect," "project," "plan," "intend," "anticipate," "estimate," "predict," "potential," "may," "should," "will" or other words or expressions of similar meaning, although not all forward-looking statements contain such terms.
Forward-looking statements are subject to risks and uncertainties, both known and unknown, that could cause actual results to differ materially from those expressed or implied in forward-looking statements. Such risks and uncertainties include, but are not limited to: our ability to achieve our strategic and operational initiatives; our ability to adapt to changes in an evolving and rapidly changing industry; the scale, scope and duration of the COVID-19 pandemic and its potential impact on our business, operating results, cash flows or financial condition; our ability to compete effectively, differentiate our products and services from those of our competitors and maintain or increase market share; price competition and other pressures that could compress our margins or result in premiums that are insufficient to cover the cost of services delivered to our customers; the potential for actual claims to exceed our estimates related to expected medical claims; our ability to develop and maintain satisfactory relationships with physicians, hospitals, other health service providers and with producers and consultants; our ability to maintain relationships with one or more key pharmaceutical manufacturers or if payments made or discounts provided decline; changes in the pharmacy provider marketplace or pharmacy networks; changes in drug pricing or industry pricing benchmarks; political, legal, operational, regulatory, economic and other risks that could affect our multinational operations; risks related to strategic transactions and realization of the expected benefits of such transactions, including with respect to the sale of our international life, accident and supplemental benefits businesses, as well as integration or separation difficulties or underperformance relative to expectations; dependence on success of relationships with third parties; risk of significant disruption within our operations or among key suppliers or third parties; our ability to invest in and properly maintain our information technology and other business systems; our ability to prevent or contain effects of a potential cyberattack or other privacy or data security incident; potential liability in connection with managing medical practices and operating pharmacies, onsite clinics and other types of medical facilities; the substantial level of government regulation over our business and the potential effects of new laws or regulations or changes in existing laws or regulations; uncertainties surrounding participation in government-sponsored programs such as Medicare; the outcome of litigation, regulatory audits and investigations; compliance with applicable privacy, security and data laws, regulations and standards; potential failure of our prevention, detection and control systems; unfavorable economic and market conditions, stock market or interest rate declines and risks related to a downgrade in financial strength ratings of our insurance subsidiaries; the impact of our significant indebtedness and the potential for further indebtedness in the future; unfavorable industry, economic or political conditions; credit risk related to our reinsurers; as well as more specific risks and uncertainties discussed in Part I, Item 1A – Risk Factors and Part II, Item 7 – Management's Discussion and Analysis of Financial Condition and Results of Operations of this Form 10-K and as described from time to time in our future reports filed with the Securities and Exchange Commission (the "SEC").
You should not place undue reliance on forward-looking statements, which speak only as of the date they are made, are not guarantees of future performance or results and are subject to risks, uncertainties and assumptions that are difficult to predict or quantify. Cigna undertakes no obligation to update or revise any forward-looking statement, whether as a result of new information, future events or otherwise, except as may be required by law.
PART I
Item 1. BUSINESS
OVERVIEW
Cigna Corporation, together with its subsidiaries (either individually or collectively referred to as "Cigna," the "Company," "we," "our" or "us") is a global health services organization.
Our Purpose and Mission To improve the health, well-being and peace of mind of those we serve | ||||||||
| Our Strategy | ||||||||
| To make health care affordable, predictable and simple for those who count on us | ||||||||
Making it affordable: We build on our leading, differentiated position to lower the total cost of care. | ||||||||
Making it predictable: We take the surprise out of the system and help people make informed health care choices. | ||||||||
Making it simple: We make it easier for the people we serve to get the care they need. | ||||||||
Cigna is a global health services company uniquely capable of driving affordable, predictable and simple health care, with expansive and deep capabilities that accelerate our strategy to achieve our mission of improving health, well-being and peace of mind. It starts with the strength of our Evernorth and Cigna Healthcare platforms. Evernorth is our services portfolio that is highly attractive to our clients and partners because of the depth of its capabilities and expertise and enables us to deepen existing relationships across our entire book of business. Our Cigna Healthcare platform, consisting of our U.S. Commercial, U.S. Government and International Health operating segments, allows us to harness our partnership relationship with physicians to deliver affordable and coordinated health care to employers and individuals. Together, our Evernorth and Cigna Healthcare platforms provide a strong and diverse foundation that allows us to capitalize on growth opportunities by leading with our strengths – medical and pharmacy solutions – and then expanding those relationships by addressing additional client needs and innovating and delivering new services and solutions.
Cigna's employees are champions for the people we serve and over the past decade, our focus has shifted to helping individuals and families thrive by offering solutions to prevent and better manage health challenges. When sickness or disability do occur, we support our customers by offering broad choices to help them best access high quality, affordable, whole person care. We see three primary ways to help individuals maintain, improve or recover their physical or mental health: 1) behavioral and lifestyle changes – with more than 1,000 health coaches helping individuals set and meet health goals; 2) affordable, effective medication options – with access to our leading pharmacy services improving health and driving affordability; and 3) targeted medical and surgical interventions – with a clear and proven strategy around partnerships and value-based care quality programs, powered by data and analytics and aligned incentives. We maximize use of evidence-based care, while delivering best-in-class service for our customers with acute and chronic conditions through enhanced real-time insights across an expanded platform with industry-leading solutions to support care decisions.
Our portfolio of offerings solves diverse challenges across the health care system. We offer a differentiated set of pharmacy, medical, behavioral, dental and supplemental products and services, primarily through two brands: Cigna and Evernorth. Our capabilities include: 1) a broad portfolio of solutions and services, some of which can be offered on a stand-alone basis; 2) integrated behavioral, medical and pharmacy management solutions; 3) leading specialty pharmacy, clinical and care management expertise; and 4) advanced analytics that help us engage more meaningfully with individuals, the plan sponsors we serve and our provider partners.
We differentiate ourselves in the market through a number of capabilities. We improve whole-person health, in body and mind by treating physical and behavioral health together to improve outcomes and by providing early behavioral and lifestyle interventions. We make it easier to access quality care by improving navigation at every step in a patient's health journey and by meeting customers wherever they are - virtually, digitally and in home. We connect care for the most pressing conditions by closing gaps between hospitals, primary care providers, specialists and other health care providers. We also develop personalized treatment paths across every dimension of care. We continue to build upon our network of value-based provider arrangements for better customer experiences, better overall health outcomes and greater affordability. We have a significant number of our eligible customers aligned to hundreds of our Accountable Care programs nationally. We make medicine more affordable by reducing costs from start to finish, including those related to drug access, delivery and treatment and by identifying appropriate medication alternatives. We partner and
1
innovate to enable us to deliver differentiated value and broaden our reach in new geographies or through the introduction of new solutions and offerings.
Our key to success revolves around how deeply we care about our customers, patients and co-workers. We intend to create a better future together by innovating and adapting, acting with speed and purpose, partnering, collaborating and keeping our promises.
During the fourth quarter of 2021, we approved a strategic plan to drive operational efficiencies. We believe this plan, coupled with the previously announced divestiture of the international life, accident and supplemental health benefits businesses (described below), will further leverage the Company's ongoing growth to drive operational efficiency through enhancements to organization structure and increased use of automation and shared services. In connection with these plans, we have updated our reporting segments to align with the new business reporting structure and recognized a charge in the fourth quarter of 2021 in the amount of $168 million, pre-tax ($119 million, after-tax). Although a substantial portion of the actions associated with these strategic steps have been reflected in the current charge recognized in the fourth quarter of 2021, additional amounts are expected to be recorded in the second quarter of 2022 as we finalize our plans following the completion of the divestiture. See Note 15 for further information regarding our organizational efficiency charge.
Information about Segments
As previously disclosed, we entered into a definitive agreement in October 2021 to sell our life, accident and supplemental benefits businesses in seven countries to Chubb INA Holdings, Inc. ("Chubb") for $5.75 billion cash (the "Chubb Transaction"). Subject to applicable regulatory approvals and customary closing conditions, we expect to complete the sale of our life, accident and supplemental benefits businesses in Hong Kong, Indonesia, New Zealand, South Korea, Taiwan, Thailand and our interest in a joint venture in Turkey in the second quarter of 2022.
In connection with the pending Chubb Transaction, we revised our business reporting structure. As such, we adjusted our segment reporting effective in the fourth quarter of 2021 so that the results previously reported in the International Markets segment are now reported as follows:
•The businesses to be retained by Cigna are now reported in the newly created International Health operating segment that will be aggregated with our existing U.S. Commercial and U.S. Government operating segments in the renamed Cigna Healthcare reporting segment (previously named U.S. Medical).
•The businesses to be sold pursuant to the Chubb Transaction are now reported in Other Operations.
Throughout this Form 10-K, segment results for the years ended December 31, 2020 and 2019 have been restated to conform to the new segment presentation (see "Executive Overview" section of the Management Discussion and Analysis of Financial Condition and Results of Operations ("MD&A") located in Part II, Item 7 of this Form 10-K for a Financial Summary). A full description of our segments follows:
Evernorth includes a broad range of coordinated and point solution health services and capabilities, as well as those from partners across the health care system, in pharmacy solutions, benefits management solutions, care delivery and care management solutions and intelligence solutions, which are provided to health plans, employers, government organizations and health care providers.
Cigna Healthcare includes Cigna's U.S. Commercial, U.S. Government and International Health operating segments that provide comprehensive medical and coordinated solutions to clients and customers. U.S. Commercial products and services include medical, pharmacy, behavioral health, dental, vision, health advocacy programs and other products and services for insured and self-insured customers. U.S. Government solutions include Medicare Advantage, Medicare Supplement and Medicare Part D plans for seniors, and individual health insurance plans both on and off the public exchanges. International Health solutions include health care coverage in our international markets, as well as health care benefits for globally mobile individuals and employees of multinational organizations. The Cigna Healthcare segment is comprised of the previously named U.S. Medical segment and the businesses to be retained from the previous International Markets segment.
Other Operations contains the remainder of our business operations, consisting of the following:
•Ongoing business:
•Corporate-Owned Life Insurance ("COLI") offers permanent insurance contracts sold to corporations to provide coverage on the lives of certain employees for the purpose of financing employer-paid future benefit obligations.
2
•Exiting businesses:
•International Life, Accident and Supplemental Benefits Businesses in seven countries to be sold pursuant to the Chubb Transaction.
•Group Disability and Life. Prior to the sale of the U.S. Group Disability and Life business on December 31, 2020, this operating segment provided group long-term and short-term disability, group life, accident, voluntary and specialty insurance products and related services.
•Run-off businesses:
•Reinsurance: predominantly comprised of guaranteed minimum death benefit ("GMDB") and guaranteed minimum income benefit ("GMIB") business effectively exited through reinsurance with Berkshire Hathaway Life Insurance Company of Nebraska ("Berkshire") in 2013.
•Settlement Annuity business in run-off.
•Individual Life Insurance and Annuity and Retirement Benefits Businesses: comprised of deferred gains from the sales of these businesses.
Other Operations was previously named Group Disability and Other.
Corporate reflects amounts not allocated to operating segments, including net interest expense (defined as interest on corporate debt less net investment income on investments not supporting segment and other operations), certain litigation matters, expense associated with our frozen pension plans, charitable contributions, severance, certain overhead and enterprise-wide project costs and intersegment eliminations for products and services sold between segments.
COVID-19
Cigna's commitment to the health, well-being and peace of mind of our employees and the people we serve remains the primary focus as the pandemic continues to impact all aspects of daily life. Cigna is leveraging its resources, expertise, data and actionable intelligence to assist customers, clients and care providers navigate the evolving dynamics of the pandemic. The Company continues to encourage COVID-19 vaccinations across all eligible populations to help control the spread of the virus, limit the severity of the disease and save lives. Cigna has also expanded access to testing, care and supportive resources to help everyone it serves take care of their physical and mental health during this time and will continue to do so. We continue to actively manage our response and assess impacts to our financial position and operating results, as well as mitigate adverse developments in our business. In response to the pandemic, U.S. federal and state governments have enacted new regulatory requirements as discussed in the "Business - Regulation" section of this Form 10-K. Additionally, see "Item 1A. Risk Factors" section of this Form 10-K for further discussion of COVID-19.
Other Information
The financial information included in this Form 10-K for the fiscal year ended December 31, 2021 is in conformity with accounting principles generally accepted in the United States of America ("GAAP") unless otherwise indicated. In the segment discussions that follow, we use the terms "adjusted revenues" and "pre-tax adjusted income (loss) from operations" to describe segment results. See Note 23 to the Consolidated Financial Statements of this Form 10-K for definitions of those terms. Industry rankings and percentages set forth herein are for the year ended December 31, 2021 unless otherwise indicated. In addition, statements set forth in this document concerning our rank or position in an industry or particular line of business have been developed internally based on publicly available information unless otherwise noted.
Cigna Holding Company (formerly Cigna Corporation) was incorporated in Delaware in 1981. Halfmoon Parent, Inc. was incorporated in Delaware in March 2018. Halfmoon Parent, Inc. was renamed Cigna Corporation and Cigna Holding Company became its subsidiary concurrent with the consummation of the combination with Express Scripts on December 20, 2018.
You can access our website at http://www.cigna.com to learn more about our company. We make annual, quarterly and current reports and proxy statements and amendments to those reports available, free of charge through our website as soon as reasonably practicable after we electronically file these materials with, or furnish them to, the Securities and Exchange Commission ("SEC"). We also use our website as a means of disclosing material information and for complying with our disclosure obligations under the SEC's Regulation FD (Fair Disclosure). Important information, including news releases, analyst presentations and financial information regarding Cigna is routinely posted on our website. Accordingly, investors should monitor the Investor Relations portion of our website, in addition to following our press releases, SEC filings and public conference calls and webcasts. The information contained on, or that may be accessed through, our website is neither incorporated by reference into nor a part of this report. See also "Code of Ethics and Other Corporate Governance Disclosures" in Part III, Item 10 of this Form 10-K for additional information regarding the availability of our Codes of Ethics on our website.
3
EVERNORTH
Evernorth includes a broad range of coordinated and point solution health services and capabilities, as well as those from partners across the health care system, in pharmacy solutions, benefits management solutions, care delivery and care management solutions and intelligence solutions to deliver custom and flexible solutions that meet the needs of our clients and customers. In 2021, Evernorth reported adjusted revenues of $131.9 billion and pre-tax adjusted income from operations of $5.8 billion.
In 2021, Evernorth continued to execute on our strategic initiatives through the acquisition of MDLIVE, Inc. ("MDLIVE"). See "Care Delivery and Care Management Solutions" below for more information about MDLIVE.
| HOW WE WIN | ||
Evernorth accelerates delivery of innovative and flexible solutions to create value and meet the diverse needs of health plans, employers, health care providers and government organizations by: ·Partnering in unconventional ways to solve complex problems across a fragmented health care ecosystem, fueled by connected data and expertise that drives purposeful innovation ·Creating flexible and focused solutions tailored to client needs, using Evernorth's combined strengths and capabilities, as well as strategic partnerships, to deliver: better, more efficient care for patients; better experiences for clients, providers and customers; and enhanced choices for clients and customers through our open architecture model ·Evaluating medicines, digital therapeutics and other health solutions for efficacy, adherence, value and price to assist clients in selecting a cost-effective formulary ·Offering home delivery, virtual and in-person care, and specialty customer-centric solutions that meet the needs of our clients and customers in ways that unlock greater value and better health services while providing better and specialized clinical care ·Delivering more affordable solutions that provide more discounts and drive risk-sharing and value-based care across the pharmaceutical supply chain ·Promoting the use of generics and lowest-cost, clinically effective brands of medications | ||
4
The following chart depicts a high-level summary of our principal products and services in this segment with definitions on subsequent pages.
| Principal Products & Services | Brands/ Subsidiaries | Key Relationships | Primary Competitors | ||||||||
| Pharmacy Solutions | Express Scripts Pharmacy®, Accredo®, Freedom Fertility Pharmacy®, Therapeutic Resource Center® | Clients, Customers, Health Care Providers | Independent Pharmacy Benefit Managers ("PBMs"), Managed Care PBMs, Retail Pharmacies, Specialty Pharmacies | ||||||||
| Benefits Management Solutions | eviCore Healthcare®, Express Scripts PBM, myMatrixx®, Care Continuum, Embarc Benefit Protection®, Express Scripts MedRx ManagementSM, FamilyPathSM, Value Based Programs (Express Scripts SafeGuardRx®, Express Scripts Patient Assurance®), National Preferred Formulary, Advanced Utilization Management, Enhanced Fraud, Waste & Abuse, Advanced Opioid Management®, ScreenRx®, SaveOnSP, Ascent Health Services, Econdisc, Inside Rx®, Evernorth Wholesale MarketplaceSM | Clients, Customers, Health Care Providers, Consultants, Health Plans, Commercial and Government Payors, Self-paying customers (InsideRx only), Pharmacy Providers | Health Plans, Independent PBMs, Managed Care PBMs, Third Party Benefit Administrators, Group Purchasing Organizations, Clinical Solutions and Health Care Data Analytics Companies | ||||||||
| Care Delivery and Care Management Solutions | inMyndSM, Health Connect 360®, RationalMed®, Evernorth Digital Health FormularySM, Behavioral Health, Cigna Medical Group, MDLIVE®, Evernorth Direct Health, Alegis | Clients, Customers | Independent PBMs, Managed Care PBMs, Managed Care Organizations, Care Delivery and Care Management Solutions Providers, Third-Party Benefit Administrators | ||||||||
| Evernorth Intelligence Solutions | Express Scripts Lab, MediCUBE®, HealthPredictSM, ScriptVision® | Health Care Providers, Clients | Health Care Data Analytics Companies | ||||||||
| Provider Services | CuraScript SD® | Health Care Providers, Clinics, Hospitals | Specialty Drug Distributors | ||||||||
Principal Products & Services
•Pharmacy Solutions. The pharmacy operations consist of 13 order processing home delivery and specialty pharmacies, six patient contact centers, 30 specialty dispensing pharmacies and four high-volume automated dispensing pharmacies located throughout the United States. Our high-volume automated dispensing pharmacies are located in Arizona, Indiana, Missouri and New Jersey.
◦Express Scripts Pharmacy. Express Scripts Pharmacy dispenses approximately 1.6 billion adjusted prescriptions(1) annually to members of pharmacy plans managed by our Express Scripts PBM. The service offers free standard shipping of medications nationwide, usually in a 90-day supply, directly to the customer's home. The service allows for automatic refills on eligible medications and unrestricted telephone access to specially trained pharmacists to answer customer questions. The front-end of our pharmacy is organized into Therapeutic Resource Centers, where pharmacists focus their practice of pharmacy by condition, which offers customers a more personalized experience while providing enhanced clinical care. Our differentiated practice of pharmacy, coupled with our advanced automated dispensing technology, results in safer and more accurate pharmacy operations when compared to retail pharmacies, convenient access to maintenance medications and better management of our clients' drug costs through operating efficiencies and generic substitutions. Our research shows that Express Scripts Pharmacy achieves a higher level of therapeutic interventions, better adherence, more cost savings and a consistently higher Net Promoter Score ("NPS") compared to retail pharmacies.
◦Specialty Pharmacy Services. Specialty medications are primarily characterized as high-cost medications for the treatment of complex and rare diseases. These medications broadly include those with frequent dosing adjustments, intensive clinical monitoring, the need for customer training, specialized product administration requirements or medications limited to certain specialty pharmacy networks by manufacturers. Through a combination of assets and capabilities, we work to provide an enhanced level of predictable care and therapy management for customers taking specialty medications, increased visibility and improved outcomes for payors and custom programs for biopharmaceutical manufacturers. Accredo is focused on dispensing injectable, infused, oral and inhaled drugs that require a higher level of clinical service and support than traditional pharmacies typically offer. Accredo supports successful outcomes for customers and reduces waste for clients through specialty trained clinicians, a nationwide footprint and a network of in-home nursing services, reimbursement and customer assistance programs and biopharmaceutical services. Drug manufacturers may select Accredo for exclusive dispensing of highly specialized therapies. Freedom Fertility Pharmacy is dedicated exclusively to supporting customers undergoing
(1) Non-specialty network scripts filled through 90-day programs and home delivery scripts are multiplied by three. All other network and specialty scripts are counted as one script.
5
fertility treatment. Accredo and Freedom Fertility Pharmacy serve customers within a pharmacy benefit plan administered by Express Scripts PBM, as well as customers in plans administered by other PBMs and health plans.
•Benefits Management Solutions. We drive high-quality, cost-effective care through prescription drug utilization and cost management services. We support our clients' plan design selections to deliver balanced affordability, choice, simplicity and convenience. We focus our solutions to align with our clients' service, care and cost management needs. As a result, we believe we deliver better outcomes, higher customer satisfaction and a more affordable prescription drug benefit. We process drug claims via Express Scripts Pharmacy, Accredo and our retail networks by integrating retail network pharmacy administration, benefit design consultation, drug utilization review, drug formulary management and pharmacy fulfillment services. We administer payments to retail networks and bill benefits costs to our clients through our end-to-end adjudication services.
◦Drug Utilization Review program. When pharmacies submit claims for prescription drugs to us, we review them electronically in real time for health and safety. We then alert the dispensing pharmacy of any detected issues. Clients may also choose to enroll in programs that result in communications about potential therapy concerns being sent to prescribers after the initial claim submission.
◦Benefits Design Consultation. We consult with our clients on how best to structure and leverage the pharmacy benefit to meet plan objectives for affordable access to the prescription medications customers need to stay healthy and to ensure the safe and effective use of those medications.
◦myMatrixx. myMatrixx is a unique PBM with an exclusive focus on workers' compensation. We combine high touch customer service with clinical expertise and state-of-the-art business intelligence systems to deliver simplified solutions and positive outcomes. myMatrixx leverages Express Scripts' robust pharmacy network and provides a smooth and personalized experience for clients and injured workers.
◦eviCore Medical Benefits Management. eviCore healthcare is a leading provider of integrated health benefit management solutions that focus on driving adherence to evidence-based clinical guidelines, improving the quality of patient outcomes and reducing the cost of care. eviCore provides technology-enabled managed solutions in clinical diagnostic areas such as advanced imaging, cardiology and gastroenterology, as well as in whole person (longitudinal) areas such as musculoskeletal, oncology, fertility and post-acute care. eviCore contracts with health plans and other commercial and government payors to promote the appropriate use of health care services by the customers they serve. In certain instances, this occurs through capitated risk arrangements, when we assume the financial obligation for the cost of health care services provided to eligible customers covered by eviCore health care management programs.
◦Medical Drug Management. We offer a comprehensive range of services and guaranteed savings for managing medically billed specialty drugs. Our solutions apply utilization management, site of care management and claims prepayment review to effectively reduce wasteful spend, while providing services tailored to customers ensuring safety and healthier outcomes. We also offer Express Scripts MedRx Management, a suite of solutions and consultative services for medical rebates contracting, medically-billed drug preferencing and value-based contracting.
◦Embarc Benefit Protection. Embarc shields clients and members from the high costs of life-saving gene therapies, so that customers who need treatment can get it. Additionally, the program provides access to quality, cost-effective in-network providers and support from a dedicated gene therapy case management team.
◦FamilyPath. FamilyPath is raising the bar for fertility health by providing more comprehensive, more flexible coverage and proactive care for growing families, including expanded medical and pharmacy benefit management; access to vetted provider and lab networks; and dedicated Fertility Advisors to proactively support and guide customers.
◦Retail Network Pharmacy Administration. We contract with retail pharmacies to provide prescription drugs to customers of the pharmacy benefit plans we manage. We negotiate with pharmacies throughout the United States to discount drug prices provided to customers and manage national and regional networks responsive to client preferences related to cost containment, convenience of access for customers and network performance. We also manage networks of pharmacies customized for or under direct contract with specific clients and have contracted with pharmacy provider networks to comply with the Center for Medicare and Medicaid Services ("CMS") access requirements for the federal Medicare Part D prescription drug program ("Medicare Part D"). All retail pharmacies in our network communicate with us online and in real-time to process prescription drug claims. When a plan customer presents their identification card at a network pharmacy, the pharmacy sends specific customer, prescriber and prescription information in an industry-standard format through our systems, which process the claim and respond to the pharmacy with relevant information to process the prescription.
◦Drug Formulary Management. Formularies are lists of drugs with designations that may be used to determine drug coverage, customer out-of-pocket costs and communicate plan preferences in competitive drug categories. Our formulary management services support clients in establishing formularies that assist customers and physicians in choosing clinically-appropriate, cost-effective drugs and prioritize access, safety and affordability. We administer specific formularies on behalf of our clients, including standard formularies developed and offered by Express Scripts and custom formularies in which we play a more limited role. Most of our clients select standard formularies, governed by our National Pharmacy & Therapeutics Committee, which is comprised of a panel of independent physicians and pharmacists in active clinical practice representing
6
a variety of specialties and practice settings, typically with major academic affiliations. In making formulary recommendations, this committee considers only the drug's safety and efficacy and not the cost of the drug, including any negotiated manufacturer discount or rebate arrangement. This process is designed to ensure the clinical recommendation is not affected by our financial arrangements. We fully comply with this committee's clinical recommendations regarding drugs that must be included or excluded from the formulary based on their assessment of safety and efficacy.
◦Advanced Utilization Management. These programs include prior authorization, drug quantity management and step therapy designed to decrease client spend on pharmacy.
◦Enhanced Fraud, Waste & Abuse. Evernorth helps plan sponsors identify potential problem customers and prescribers with unusual or excessive utilization patterns. The program is designed to help identify outliers and situations of abnormal use or prescribing patterns by analyzing types of prescriptions, refill patterns and pharmacy utilization.
◦Administration of Group Purchasing Organizations. Evernorth operates various group purchasing organizations that negotiate pricing for the purchase of pharmaceuticals and formulary rebates with pharmaceutical manufacturers on behalf of their participants. They also provide various administrative services to their participants including management and reporting.
◦Copay Solutions. Our first-to-market innovative copay solutions helps customers afford their medications, protect plan design preferences and achieve lower trend. In partnership with SaveOnSP on the first non-essential health benefits copay assistance solution, we've driven significant savings by targeting high-cost, high-volume drugs. SaveOnSP recommends plan design and coverage changes for certain drugs, enabling maximum savings and reducing plan and client costs. As manufacturer programs and regulations change, this aggressive solution adapts, delivering lower specialty plan cost and enhanced customer support.
◦Inside Rx. Inside Rx is a prescription medication savings program that offers eligible customers discounts on many brand and generic medications for self-paying customers. This program is not insurance but offers savings at more than 60,000 participating retail pharmacies (including all major chains) in the United States and Puerto Rico. The program also offers discounts on prescription medications through private label solutions. Inside Rx earns a small fee from our supply chain partners every time a customer fills a prescription via the program. This lets us provide access to our savings card at no cost to the customer.
◦Evernorth Wholesale Marketplace. Evernorth Wholesale Marketplace offers a suite of flexible, private label solutions including Pharmacy Rebate Program services, Retail Network Program services, SafeGuardRx, Medical Rebate Program and Utilization Management. As the needs of the market evolve, we will continue to partner with clients and develop additional offerings that align with their goals and objectives.
◦Value-Based Programs.
▪Express Scripts SafeGuardRx. We offer a solution platform aimed at therapy classes that pose budgetary threats and clinical challenges to customers. Our solutions are designed to keep our clients ahead of the drug cost curve while providing customers the personalized care and access they need. These solutions are offered throughout our pharmacy benefit management services and include, but are not limited to care for: cardiovascular, diabetes, hepatitis, HIV, inflammatory conditions, neurological, multiple sclerosis, oncology, pulmonary, rare conditions and weight management. Innovative programs, such as Express Scripts SafeGuardRx, combine utilization management, formulary management, specialized care from our Therapeutic Resource Centers and financial savings, to help us to change the market in key categories. These services optimize the safe and appropriate dispensing of therapeutic agents, minimize waste and improve clinical and financial outcomes.
▪Express Scripts Patient Assurance Program. This program addresses the need for greater affordability and access to medications by providing a fixed out-of-pocket cost to customers in non-government funded benefit plans.
•Care Delivery and Care Management Solutions. We offer clinical programs to help our clients drive better whole-person health outcomes at a lower cost by identifying and addressing potentially unsafe or wasteful prescribing, dispensing and use of prescription drugs and communicating with, or supporting communications with, physicians, pharmacies and customers.
◦MDLIVE telehealth services provide flexibility for the customer to access a network of telehealth providers for routine primary care and wellness, urgent care, dermatology care and behavioral health care needs.
◦Our inMynd Behavioral Health solution provides access to expert guidance and support for anxiety, depression and insomnia, including access to individualized support and resources, condition-specific care through our Neuroscience Therapeutic Resource Centers and a digital Cognitive Behavioral Therapy.
◦Health Connect 360 is a transformational, outcomes based, clinical management model that bridges pharmacy, medical, lab and biometric data to develop insights and deliver personalized health care clinical support. Clinical outcomes and quality metrics are tailored to meet client needs.
◦RationalMed improves patient health and safety by integrating medical, pharmacy and laboratory claims data to initiate changes and correct errors in care, lowering both medical and prescription drug costs.
7
◦Through the Evernorth Digital Health Formulary, we evaluate, procure, implement and manage digital health solutions on behalf of clients, alleviating administrative burden and ensuring clinical effectiveness, data security, user-friendly experiences and financial value.
•Evernorth Intelligence Solutions. By bringing together world-class talent, multi-disciplinary expertise and advanced data and analytics, we unlock actionable insights to help drive greater affordability, simplicity, predictability and growth. We work together with our clients and partners to create dynamic solutions, services and platforms that guide better decisions and improved performance (see "Business - Digital, Data and Technology" section of this Form 10-K for further information).
◦Evernorth Labs. We accelerate innovation through increased collaboration with clients, customers and partners to develop solutions for launch in their businesses. With our Labs, which are state-of-the-art research facilities and shared spaces for collaboration, ideation and innovation, we gather with our clients and industry leaders to solve the toughest challenges in the health care system, including: better managing the most complex and expensive disease states, such as oncology; improving care access and delivery, such as worksite, home and virtual care; and planning for emerging trends, such as artificial intelligence, and industry disruptors, such as COVID-19.
◦Data, advanced analytics and platforms. We use advanced predictive modeling to shape solutions that help decrease health care fragmentation, drive optimized care coordination, reduce key cost drivers and improve health outcomes. In-depth trend analysis helps us to identify and effectively address challenges like opioid abuse, COVID-19 and other emerging health crises. We use market surveillance and forecasting to pinpoint and proactively address cost drivers. Our platform strategy as a service gives clients the tools to build successful businesses in a flexible, customizable way: Trend Central® provides access to key performance indicators to help plan sponsors reduce costs and work towards healthier outcomes; HealthPredict produces high patient-level risk scores, to show the highest value opportunities for proactive intervention; MediCUBE gives our academic detailing pharmacists the analytical power to identify ways to save plans from significant unnecessary spend and improve quality metrics; and ScriptVision provides a suite of real-time, data-driven capabilities that empower physicians to make the best prescribing choices, including ePrescribing (including controlled substances), real-time prescription benefit information, electronic prior authorizations, clinical care messages such as drug interactions and high-risk medication alerts and data on patient adherence rates.
•Provider Services. CuraScript SD is a specialty distributor of pharmaceuticals and medical supplies (including injectable and infusible pharmaceuticals and medications to treat specialty and rare or orphan diseases) directly to health care providers, clinics and hospitals in the United States for office or clinic administration. Through this business, we provide distribution services primarily to office and clinic-based physicians who treat customers with chronic diseases and regularly order costly specialty pharmaceuticals. This business provides competitive pricing on pharmaceuticals and medical supplies, operates three distribution centers and ships most products overnight within the United States; it also provides distribution capabilities to Puerto Rico and Guam. It is a contracted supplier with most major group purchasing organizations and leverages our distribution platform to operate as a third-party logistics provider for several pharmaceutical companies.
Customers
We provide products and services in the Evernorth segment to clients and customers, as described below. Also described below are our current and former significant clients.
•Clients. We provide services to managed care organizations, health insurers, third-party administrators, employers, union-sponsored benefit plans, workers' compensation plans, government health programs, providers, clinics, hospitals and others. We provide services to a majority of customers in our Cigna Healthcare segment.
•Customers. Prescription drugs are dispensed to patients connected to the service offerings we provide to clients. Prescription drugs are dispensed primarily through networks of retail pharmacies under non-exclusive contracts with us and via home delivery from Express Scripts Pharmacy and specialty drug fulfillment pharmacies.
The Department of Defense ("DoD") TRICARE® Pharmacy Program is the military health care program serving active-duty service customers, National Guard and Reserve customers and retirees, as well as their dependents. Under this contract, we provide online claims adjudication, home delivery services, specialty pharmacy clinical services, claims processing and contact center support and other services critical to managing pharmacy trend. In 2021, the DoD awarded Express Scripts a 7-year pharmacy program contract beginning January 1, 2023. Under the new contract, Express Scripts will provide enhanced specialty care and expanded care coordination capabilities, while continuing to support current pharmacy operations, through 2029. Revenues from this contract are significant to the segment.
In 2019, Express Scripts and Prime Therapeutics LLC ("Prime") entered into an agreement effective on April 1, 2020 to deliver improved choice and affordability for Prime's clients and their customers by enhancing retail pharmacy networks and pharmaceutical
8
manufacturer value. In 2021, the relationship with Prime was expanded to include the option for Prime's plans to access the Accredo specialty pharmacy and Express Scripts home delivery in-network pharmacies. Revenues from these contracts are significant to the segment.
On January 30, 2019, Anthem, Inc. ("Anthem"), a former customer, exercised its right to early termination of its pharmacy benefit management services agreement, effective March 1, 2019. As of December 31, 2019, the transition of customers was substantially complete. For further discussion of our Anthem relationship, see the "Executive Overview – Key Transactions and Business Developments" section of our MD&A located in Part II, Item 7 of this Form 10-K.
Competition
The health care industry has undergone periods of substantial consolidation and may continue to consolidate in the future. Many of the largest managed care organizations now also own health services businesses that compete with Evernorth in the verticals in which we participate. We believe the primary competitive factors in the industry include the ability to: negotiate with retail pharmacies to ensure our retail pharmacy networks meet the needs of our clients and customers; provide home delivery and specialty pharmacy services; negotiate discounts and rebates on prescription drugs with drug manufacturers; navigate the complexities of government-reimbursed business including Medicare, Medicaid and the public exchanges; manage cost and quality of specialty drugs; use the information we obtain about drug utilization patterns and consumer behavior to reduce costs for our clients and customers and the level of service we provide.
•Managed Care PBMs. CVS Caremark (owned by CVS Health Corporation), Humana, IngenioRx (owned by Anthem, Inc.), OptumRx (owned by UnitedHealth Group Inc.) and Prime Therapeutics (owned by a collection of Blue Cross / Blue Shield Plans) compete with us on a variety of products and in various regions throughout the United States.
•Independent PBMs. MedImpact, Navitus Health Solutions, Elixir (owned by Rite Aid Corporation) and many other regional PBMs compete with us on a variety of products across the United States.
•Pharmacies. CVS, Walgreens Boots Alliance, Inc., WalMart, Inc., Rite Aid, Kroger and other independent pharmacies compete with us for the delivery of prescription drug needs to our customers. In addition, many PBMs own and operate home delivery and specialty pharmacies including CVS, OptumRx, Walgreens, Humana and Elixir. New entrants continue to emerge including Amazon Pharmacy, Capsule and Hims.
•Third-Party Benefits Administrators. Third parties that specialize in claim adjudication and benefit administration, such as SS&C Health, are direct competitors. With the emergence of alternative benefit models through private exchanges, the competitive landscape also includes brokers, health plans and consultants. Some of these competitors may deploy greater financial, marketing and technological resources than we do and new market entrants, including strategic alliances aimed at modifying the current health care delivery models or entering the prescription drug sector from another sector of the health care industry, may increase competition as barriers to entry are relatively low. For example, GoodRx is an entrant focused on serving the uninsured and underinsured in the cash pay pharmacy administration space.
•Care Delivery and Care Management Solutions Providers. OptumHealth, NaviHealth and Landmark (UnitedHealth Group Inc.); Beacon, Aspire and CareMore (Anthem, Inc.); CVS' HealthHubs and MinuteClinics; Kindred and oneHome (Humana Inc.); Community and Bayless (Centene Corporation); VillageMD, Teladoc, Doctor on Demand, MeMD, WalmartHealth and AmazonCare are among the companies that compete with us in this market.
•Clinical Solutions and Health Care Data Analytics Companies. Optum (owned by UnitedHealth Group Inc.), Anthem, Magellan Health (owned by Centene Corporation), Apixio, HealthHelp, Cotiviti and Inovalon are among the companies that compete with us in this market.
Operations
•Sales and Account Management. Our sales and account management teams market and sell pharmacy benefit management solutions and are supported by client service representatives, clinical pharmacy managers and benefit analysis consultants. These teams work with clients to develop innovative strategies that put medicine within reach of customers while helping health benefit providers improve access to and affordability of prescription drugs.
•Supply Chain. Our supply chain contracting and strategy teams negotiate and manage pharmacy retail network contracts, pharmaceutical and wholesaler purchasing contracts and manufacturer rebate contracts. As our clients continue to experience increased cost trends, our supply chain teams develop innovative solutions such as our Express Scripts SafeGuardRx platform and preferred pharmacy networks to combat these cost increases. In addition, our Formulary Consulting team, consisting of pharmacists and financial analysts, provides services to our clients to support formulary decisions, benefit design consultation and utilization management programs.
•Clinical Support. Our staff of highly trained health care professionals provides clinical support for our pharmacy, medical and behavioral customers. Our services include access to:
9
◦Triage for crisis care, safely guiding customers in their most vulnerable moments
◦Comprehensive behavioral health offerings including network access, utilization management and coordination of care to treat conditions ranging from depression and anxiety to substance use, autism and eating disorders
◦Condition-specific specialized customer care through our Therapeutic Resource Center facilities staffed with specialist pharmacists, nurses and other clinicians
◦Clinical development and operational support for our pharmacy benefit management services by our clinical solutions staff of pharmacists and physicians who conduct a wide range of activities including: identifying emerging medication-related safety issues and alerting physicians, clients and customers (as appropriate); providing drug information services; managing formulary; identifying and closing gaps in care; and developing utilization management, safety (drug utilization review) and other clinical interventions
Suppliers
We maintain an inventory of brand-name and generic pharmaceuticals in our home delivery and specialty pharmacies. Our specialty pharmacies also carry biopharmaceutical products to meet the needs of our customers, including pharmaceuticals for the treatment of rare or chronic diseases; if a drug is not in our inventory, we can generally obtain it from a supplier within a reasonable amount of time.
We purchase pharmaceuticals either directly from manufacturers or through authorized wholesalers. Evernorth uses one wholesaler more than others in the industry, but holds contracts with other wholesalers if needs for an alternate source arise. Generic pharmaceuticals are generally purchased directly from manufacturers.
Key Transactions and Business Developments
See the "Executive Overview - Key Transactions and Business Developments" section of our MD&A located in Part II, Item 7 of this Form 10-K for discussion of key developments impacting this segment.
Intellectual Property Rights
The trademarks and service marks covering products, services and businesses provided under the Evernorth segment include, but are not limited to, the following: EXPRESS SCRIPTS®, EVERNORTHSM, EVERNORTH HEALTHSM, MEDCO®, ACCREDO®, CURASCRIPTSD®, MYMATRIXX®, EVICORE HEALTHCARE®, FREEDOM FERTILITY PHARMACY®, VERITY®, MDLIVE®, QUALLENT PHARMACEUTICALSSM, RATIONALMED®, SCREENRX®, EXPRESSALLIANCE®, EVERNORTH DIGITAL HEALTH FORMULARYSM, THERAPEUTIC RESOURCE CENTER®, ADVANCED OPIOID MANAGEMENT®, EXPRESS SCRIPTS SAFEGUARDRX®, HIV CARE VALUE®, RARE CONDITIONS CARE VALUE®, NEUROLOGICAL CARE VALUE®, CARDIOVASCULAR CARE VALUE®, HEPATITIS CURE VALUE®, MARKET EVENTS PROTECTIONSM, ONCOLOGY CARE VALUESM, PULMONARY CARE VALUE®, MULTIPLE SCLEROSIS CARE VALUESM, CHOLESTEROL CARE VALUESM, HEALTH CONNECT 360®, EMBARC BENEFIT PROTECTION®, INMYNDSM, EXPRESS SCRIPTS PATIENT ASSURANCE®, MEDICUBE®, EXPRESS SCRIPTS PHARMACY®, FAMILYPATHSM, SCRIPTVISION®, INSIDE RX®, EXPRESS SCRIPTS MEDRX MANAGEMENT®, WEIGHT MANAGEMENT CARE VALUESM and EVERNORTH WHOLESALE MARKETPLACESM. We, or our affiliated companies, own trademarks and trademark registrations for these and other company marks.
We also hold a portfolio of patents and pending patent applications. We are not substantially dependent on any single patent or group of related patents.
10
CIGNA HEALTHCARE
Cigna Healthcare includes Cigna's U.S. Commercial, U.S. Government and International Health operating segments that provide comprehensive medical and coordinated solutions to clients and customers. U.S. Commercial products and services include medical, pharmacy, behavioral health, dental, vision, health advocacy programs and other products and services for insured and self-insured customers. U.S. Government solutions include Medicare Advantage, Medicare Supplement and Medicare Part D plans for seniors, and individual health insurance plans both on and off the public exchanges. International Health solutions include health care coverage in our international markets, as well as health care benefits for globally mobile individuals and employees of multinational organizations. In 2021, Cigna Healthcare reported adjusted revenues of $44.7 billion and pre-tax adjusted income from operations of $3.6 billion.
In 2021, in connection with the pending Chubb Transaction described in the "Overview" section of this Form 10-K, we updated our reporting segments to align with the new management structure. The Cigna Healthcare segment is comprised of the previously named U.S. Medical segment and the businesses to be retained from the previous International Markets segment.
| HOW WE WIN | ||
·Broad and deep portfolio of solutions across U.S. Commercial, U.S. Government and International Health operating segments ·Commitment to highest-quality health outcomes and customer experiences ·Collaborative physician engagement models emphasizing value over volume of services ·Integrated and coordinated benefit solutions that deliver value for our customers, clients and partners ·Technology and data analytics powering actionable insights and affordable, predictable solutions ·Talented and caring people embracing change and putting customers at the center of all we do | ||
Our results are driven by our ability to deliver value through our integrated product and service offerings and to leverage data and analytics to control medical costs and enable better health outcomes. We differentiate ourselves by providing innovative, personalized and affordable health care benefit solutions based on the unique needs of the individuals and clients we serve. We deliver value through our integrated approach and use of technology, including digital and data analytics, to enhance patient engagement and health care outcomes, underscoring our strategic focus on delivering an industry-leading customer experience. We continue to strengthen our collaborative relationships with providers through value-based reimbursement.
We offer a mix of medical insurance products and services to employers, other groups and individuals along with specialty products and services designed to improve the quality of care, lower costs and help customers achieve better health outcomes. Many of these products are available on a standalone basis, but we believe they create additional value when integrated with a Cigna-administered health plan. Our products are available through several distribution channels including brokers, direct sales and public and private exchanges. Our three funding solutions (i.e., administrative services only ("ASO"), insured – guaranteed cost ("GC") and insured – experience-rated ("ER") arrangements) enable us to customize the amount of risk taken by, and lower costs for, our clients.
11
The following chart depicts a high-level summary of our principal products and services in this segment, with definitions on subsequent pages.
| Principal Products & Services | Major Brand(s) | Geography | Funding Solution(s) | Market Segment(s) | Primary Distribution Channel(s) | Primary Competitors | ||||||||||||||
U.S. Commercial Medical | ||||||||||||||||||||
| Managed Care | Cigna | Nationwide | GC, ER, ASO | U.S. Commercial | Brokers, Private Exchanges, Direct | National Insurers, Local Healthplans, Third-Party Administrators ("TPAs") | ||||||||||||||
| Preferred Provider Organization ("PPO") | Cigna | Nationwide | National Insurers, Local Healthplans, TPAs | |||||||||||||||||
| Consumer-Driven | Cigna | Nationwide | National Insurers, Local Healthplans | |||||||||||||||||
U.S. Government Medical | ||||||||||||||||||||
| Individual and Family Plans | Cigna | 10 states (1) | GC | U.S. Government | Public Exchanges, Brokers, Direct | Local Healthplans, Provider-led Plans, National Insurers | ||||||||||||||
| Medicare Advantage | Cigna | 25 states (2) & District of Columbia | GC | U.S. Government | Direct, Brokers | National Insurers, Local Healthplans | ||||||||||||||
| Medicare Stand –Alone Prescription Drug Plans | Cigna, Express Scripts | Nationwide | GC, ASO | U.S. Government | Direct, Brokers | National Insurers | ||||||||||||||
| Medicare Supplement | Cigna | 48 states (3) & District of Columbia | GC | U.S. Government | Brokers, Direct, Private Exchanges | National Insurers | ||||||||||||||
| Specialty Products and Services | ||||||||||||||||||||
| Stop-Loss | Cigna | Nationwide | GC | U.S. Commercial | Brokers, Direct | National Insurers, Specialty Companies | ||||||||||||||
| Cost Containment | Cigna | Nationwide | GC, ER, ASO | U.S. Commercial | Direct | National Insurers, Specialty Companies | ||||||||||||||
| Consumer Health Engagement | Cigna | Nationwide | GC, ER, ASO | U.S. Commercial, U.S. Government | Brokers, Direct | National Insurers, Specialty Companies | ||||||||||||||
| Pharmacy Management | Cigna | Nationwide | GC, ER, ASO | U.S. Commercial, U.S. Government | Brokers, Direct | National PBMs | ||||||||||||||
| Behavioral Health | Cigna | Nationwide | GC, ER, ASO | U.S. Commercial | Brokers, Direct | National Insurers, Specialty Companies | ||||||||||||||
| Dental & Vision | Cigna Dental Care® | Nationwide | GC, ER, ASO | U.S. Commercial, U.S. Government | Brokers, Direct | Dental Insurers, National Insurers | ||||||||||||||
(1) AZ, CO, FL, IL, KS, MO, NC, TN, UT, VA.
(2) AL, AZ, AR, CO, CT, DE, FL, GA, IL, KS, MD, MS, MO, NC, NJ, NM, OH, OK, OR, PA, SC, TN, TX, UT, VA.
(3) All states except MA and NY.
12
| Principal Products & Services | Major Brand(s) | Geography | Funding Solution(s) | Market Segment(s) | Primary Distribution Channel(s) | Primary Competitors | ||||||||||||||
| International Health Products and Services | ||||||||||||||||||||
| Global Health Care | Cigna Global Health Benefits, Cigna Global Individual Health | Worldwide (except as limited by applicable law) | GC, ER, ASO | International Health | Brokers, Direct | Global insurers | ||||||||||||||
| Local Health Care | Cigna, ManipalCigna, CignaCMB | United Kingdom, Spain, Hong Kong, India, China, Singapore, Middle East, Thailand | GC, ER, ASO | International Health | Brokers, Direct | Global insurers and local non-U.S. insurers | ||||||||||||||
Principal Products & Services
U.S. Commercial Medical
•Managed Care Plans are offered through our insurance companies, Health Maintenance Organizations ("HMOs") and TPA companies. HMO, Surefit®, LocalPlus®, Network and Open Access Plus plans use meaningful cost-sharing incentives to encourage the use of "in-network" versus "out-of-network" health care providers. The national provider network for Managed Care Plans is smaller than the national network used with the PPO plan product line.
•PPO Plans feature a network with broader provider access than the Managed Care Plans.
•Consumer-Driven Products are typically paired with a high-deductible medical plan and offer customers a tax-advantaged way to pay for eligible health care expenses. These products, consisting of health savings accounts, health reimbursement accounts and flexible spending accounts, encourage customers to play an active role in managing their health and health care costs.
U.S. Government Medical
•Individual and Family Plans are Patient Protection and Affordable Care Act ("ACA") compliant exclusive provider organization ("EPO") or HMO plans marketed to individuals under age 65 who do not have access to health care coverage through an employer or government program such as Medicare or Medicaid. Customers receive comprehensive health care benefits and have access to a local network of health care providers who have been selected with cost and quality in mind.
•Medicare Advantage Plans allow Medicare-eligible customers to receive health care benefits, including prescription drugs, through a managed care health plan such as our coordinated care plans. Our Medicare Advantage Plans include HMO and PPO plans marketed to individuals. A significant portion of our Medicare Advantage customers receive medical care from our value-based models that focus on developing highly engaged physician networks, aligning payment incentives to improve health outcomes and using timely and transparent data sharing.
•Medicare Stand-Alone Prescription Drug ("Part D") Products provide a number of prescription drug plan options, as well as service and information support to Medicare-eligible individuals or individuals through a qualified employer group. Our stand-alone plans offer the coverage of Medicare combined with the flexibility to select a product that provides enhanced benefits and a formulary that meets an individual's specific needs. Eligible customers benefit from broad network access and enhanced service intended to promote adherence, wellness and affordability.
•Medicare Supplement Plans provide Medicare-eligible customers with federally standardized Medigap-style plans. Customers may select among the various plans with specific plan options to meet their unique needs and may visit, without the need for a referral, any health care provider or facility that accepts Medicare throughout the United States.
Specialty Products and Services
•Stop-Loss insurance coverage is offered to self-insured clients whose group health plans are administered by Cigna. Stop-loss insurance provides reimbursement for claims in excess of a predetermined amount for individuals, the entire group, or both.
•Cost Containment Programs are designed to contain the cost of covered health care services and supplies. These programs reduce out-of-network utilization and costs, protect customers from balance billing and educate customers regarding the availability of lower cost in-network services. In addition, under these programs we negotiate discounts with out-of-network
13
providers, review provider bills and recover overpayments. We charge fees for providing or arranging for these services. These programs may be administered by third-party vendors that have contracted with Cigna.
•Consumer Health Engagement services are offered to customers covered under plans administered by Cigna or by third-party administrators. These services consist of an array of health management, disease management and wellness services. Our Medical Management programs include case, specialty and utilization management and a 24/7 Health Information line which ensures around the clock access to a medical professional. Our Health Advocacy program services include early intervention in the treatment of chronic conditions and an array of health and wellness coaching. We administer incentives programs designed to encourage customers to engage in health improvement activities.
•Pharmacy Management services and benefits can be combined with our medical offerings. The comprehensive suite of pharmacy management services are available to clients and customers through our integration with Evernorth's capabilities.
•Behavioral Health services consist of a broad national network of behavioral health providers which includes one of the largest virtual networks in the United States, behavioral health specialty case and utilization management, a crisis intervention line accessible anytime, employee assistance programs and work/life programs. We integrate our programs and services with medical, pharmacy and disability programs to facilitate customized, holistic care as well as to provide resources that increase resiliency and address non-medical factors that affect overall well-being.
•Dental & Vision solutions include dental HMO plans, dental PPO plans, exclusive dental provider organization plans, traditional dental indemnity plans and a dental discount program. Employers and other groups can purchase our products on either an insured or self-insured basis as standalone products or in conjunction with medical products. Additionally, individual customers can purchase insured dental PPO plans as standalone products or in conjunction with individual medical policies.
International Health
•Global Health Care products and services include insurance and administrative services for medical, dental, pharmacy, vision and life, accidental death and dismemberment and disability risks. We are leading providers of products and services that meet the needs of multinational employers, intergovernmental and nongovernmental organizations and globally mobile individuals with a focus on keeping employees healthy and productive. The employer benefits products and services are offered through guaranteed cost, experience-rated and administrative services only funding solutions, while individuals purchase guaranteed cost coverage.
•Local Health Care products and services include medical, dental, pharmacy and vision as well as life coverage. The customers of local health care businesses are employers and individuals located in specific countries where the products and services are purchased. These employer services can similarly be funded through a range of options; individuals purchase on a guaranteed cost basis.
Revenues: Premiums and Fees
•ASO. Plan sponsors (i.e., employers, unions and other groups) self-fund all claims, but may purchase stop-loss insurance to limit exposure. We collect fees from plan sponsors for providing access to our participating provider network and for other services and programs including: claims administration; behavioral health services; disease management; utilization management; cost containment; dental and pharmacy benefit management. Approximately 85% of our U.S. Commercial medical customers are in ASO arrangements.
•Insured: GC and ER. In most states, individual and group insurance premium rates must be approved by the applicable state regulatory agency (typically department of insurance). State or federal laws may restrict or limit the use of rating methods. Premium rates are established at the beginning of a policy period and, depending on group size, may be based in whole or in part on prior experience of the policyholder or on a pool of similar policyholders. With the exception of ER policies, we generally cannot subsequently adjust premiums to reflect actual claim experience until the next policy period; the policyholder does not participate, or share in, actual claim experience; and we keep any experience surplus or margin if costs are less than the premium charged (subject to minimum medical loss ratio rebate requirements discussed below). For all insured arrangements, we bear the risk for actual costs in excess of the premium charged. Approximately 15% of our U.S. Commercial medical customers are in insured arrangements.
For Medicare Advantage plans, we receive fixed monthly payments from CMS for each plan customer based on customer demographic data and actual customer health risk factors compared to the broader Medicare population. Premiums may be received from customers when our plan premium exceeds the revenue received from CMS. We also may earn additional revenue from CMS related to quality performance measures (known as "Star Ratings").
14
The ACA subjects individual and small group policy rate increases above an identified threshold to review by the United States Department of Health and Human Services ("HHS"). Our U.S. Commercial and U.S. Government medical plans are subject to minimum medical loss ratio ("MLR") requirements. The MLR represents the percentage of premiums used to pay claims and expenses for activities that improve the quality of care. If we do not satisfy the prescribed MLR, statutes require premium refunds to policyholders or to CMS.
See the "Business - Regulation" section of this Form 10-K for additional information about premiums, MLR requirements, Star Ratings and risk adjustment and risk mitigation programs of the ACA.
Market Segments
•U.S. Commercial comprises employers from the following market segments:
◦National. Multi-state employers with 5,000 or more eligible employees. We offer primarily ASO funding solutions in this market segment.
◦Middle Market. Employers generally with 500 to 4,999 eligible employees. This segment also includes single-site employers with more than 5,000 employees and Taft-Hartley plans and other groups. We offer ASO and insured funding solutions in this market segment.
◦Select. Employers generally with 51 to 499 eligible employees. We usually offer ASO with stop-loss insurance coverage and guaranteed cost insured funding solutions in this market segment.
◦Small Group. Employers generally with 2 to 50 eligible employees. We offer guaranteed cost insured funding solutions in select geographies with a strategic partner, Oscar Health, in this market segment.
•U.S. Government comprises the following market segments:
◦Individual. Includes individuals under age 65 who do not have access to health care coverage through an employer or government program such as Medicare or Medicaid. We offer guaranteed cost, medical ACA-compliant and dental plans in this segment.
◦Medicare. Includes individuals who are Medicare-eligible customers, as well as employer group sponsored pre- and post-65 retirees. We receive revenue from CMS based on customer demographic data and health risk factors. Revenues from CMS were significant to the segment.
•International Health market segments include multinational employers, globally mobile individuals and employers and individuals in specific countries.
Customers
We provide clients and customers with access to a mix of medical and specialty products and services.
•Clients. Our clients include employers, union-sponsored benefit plans, workers' compensation plans, government health programs and other groups which span our operating segments.
•Customers. Our customers include individuals who access our offerings through an employer-sponsored plan, government-sponsored plan, or other insured group, either through in-person providers or virtual telehealth providers.
Primary Distribution Channels
•Brokers. Sales representatives distribute our products and services to a broad group of insurance brokers and consultants.
•Direct. Cigna sales representatives distribute our products and services directly to employers, unions and other groups or individuals. Various products may also be sold directly to insurance companies, HMOs and third-party administrators. Direct distribution may take the form of in-person contact, telephone or group selling venues, or an online direct to consumer enrollment platform for our individual market segment.
•Private Exchanges. We partner with select companies that have created private exchanges where individuals and organizations can acquire health insurance. We evaluate private exchange participation opportunities as they emerge in the market and target our participation to those models that best align with our mission and value proposition.
•Public Exchanges. Cigna offers individual ACA-compliant policies through public health insurance exchanges in select geographies.
Competition
The primary competitive factors affecting our business are quality of care and cost effectiveness of service and provider networks; effectiveness of medical care management; products that meet the needs of employers and their employees; total cost management; technology; and effectiveness of marketing and sales. Financial strength, as indicated by ratings issued by nationally recognized rating
15
agencies, is also a competitive factor. Our health advocacy capabilities, holistic approach to consumer engagement, breadth of product offerings, clinical care and health management capabilities along with an array of product funding solutions are competitive advantages. We believe our focus on improving the health, well-being and peace of mind of those we serve and how we deliver better affordability, predictability and simplicity in health care will allow us to further differentiate ourselves.
•National Insurers. United HealthGroup Inc., Aetna Inc. (owned by CVS Health Corporation), Anthem Inc., Humana Inc. and Blue Cross Blue Shield plans compete with us in a variety of products and regions.
•Local Healthplans. Blue Cross Blue Shield plans, local affiliates of major insurance companies and hospitals and regional stand-alone managed care and specialty companies compete with us in the states in which we offer managed care products. Additionally, plan sponsors may contract directly with providers.
•TPAs. Third-party administrators compete with us for ASO business.
•Provider-led Plans. Emerging participants include alternative health service models and other health plans seeking to disrupt, often through competitive technology.
•Dental Insurers. Various companies offering primarily dental insurance compete with us on these products.
•Specialty Companies. Specialty insurance or service companies that offer niche products and services compete with us.
•International Companies. Global insurers and local non-U.S. insurers compete with us through product and service offerings.
Partnering to Deliver on the Promise of More Affordable, Predictable, Simple Health Care
Cigna's strategy engages customers in their health, collaborates with providers to help them improve their performance and connects customers and providers through aligned health goals, incentives and actionable information to help enable informed decisions and drive better outcomes. Fueled by advanced insights and predictive analytics, Cigna is committed to developing innovative solutions that span the health care delivery system and can be applied to a multitude of providers.
•Accountable Care Program. We have approximately 240 collaborative care arrangements with primary care groups built on the patient-centered medical home and accountable care organization ("ACO") models. We have made adjustments to the program to deepen our partnerships in responding to the challenges and needs arising from the COVID-19 pandemic.
•Hospital Quality Program. We have contracts with approximately 125 hospital systems, involving over 420 hospitals, with reimbursements tied to quality metrics.
•Site of Care Redirection. We encourage the use of clinically appropriate settings to reduce the cost of care. This results in significant cost savings compared to receiving the same care in a hospital setting, while ensuring high quality care and service.
•Specialist Programs. We have approximately 280 arrangements with specialist groups in value-based reimbursement arrangements. These arrangements include specialties in orthopedics, obstetrics and gynecology, cardiology, gastroenterology, oncology, nephrology and neurology. Arrangements include incentives for enhanced care coordination and episodes of care reimbursements for meeting cost and quality goals. We have expanded these programs to include prospective bundled payment arrangements beginning with orthopedics.
•Independent Practice Associations. We have value-based physician engagement models in our Medicare Advantage plans that allow physician groups to share financial outcomes with us. This clinical model also includes outreach to new and at-risk patients to ensure they are accessing their primary care physician.
•Participating Provider Network. We provide our customers with an extensive network of participating health care providers, hospitals and other facilities, pharmacies and providers of health care services and supplies. In addition, we have strategic alliances with several regional managed care organizations to gain access to their provider networks and discounts.
•Virtual Care. We encourage access for customers through MDLIVE telehealth services as a way to support the patient/provider relationship. MDLIVE telehealth services provide flexibility for the customer to access a network of telehealth providers for routine primary care and wellness, urgent care, dermatology care and behavioral health care needs.
Key Transactions and Business Developments
See the "Executive Overview - Key Transactions and Business Developments" section of our MD&A located in Part II, Item 7 of this Form 10-K for discussion of key developments impacting this segment.
16
OTHER OPERATIONS
Other Operations includes the following businesses:
•Ongoing business:
•Corporate-Owned Life Insurance ("COLI") offers permanent insurance contracts sold to corporations to provide coverage on the lives of certain employees for financing employer-paid future benefit obligations.
•Exiting businesses:
•International Life, Accident and Supplemental Benefits Businesses in seven countries to be sold pursuant to the Chubb Transaction as described in the "Overview" section of this Form 10-K.
•Group Disability and Life. Prior to the sale of the U.S. Group Disability and Life business on December 31, 2020 (see Note 4 to the Consolidated Financial Statements for additional information), this operating segment provided group long-term and short-term disability, group life, accident, voluntary and specialty insurance products and related services.
•Run-off businesses:
•Reinsurance is predominantly comprised of guaranteed minimum death benefit ("GMDB") and guaranteed minimum income benefit ("GMIB") business effectively exited through reinsurance with Berkshire Hathaway Life Insurance Company of Nebraska ("Berkshire") in 2013.
•Settlement Annuity business in run-off.
•Individual Life Insurance and Annuity and Retirement Benefits Businesses are comprised of deferred gains from the sales of these businesses.
In 2021, Other Operations reported adjusted revenues of $4.0 billion and pre-tax adjusted income from operations of $889 million. Other Operations was previously named Group Disability and Other.
Ongoing Business
Corporate-Owned Life Insurance
The principal products of the COLI business are permanent insurance contracts sold to corporations to provide coverage on the lives of certain employees for financing employer-paid future benefit obligations. Permanent life insurance provides coverage that, when adequately funded, does not expire after a term of years. The contracts are primarily non-participating universal life policies. Fees for universal life insurance products consist primarily of mortality and administrative charges assessed against the policyholder's fund balance. Interest credited and mortality charges for universal life and mortality charges on variable universal life may be adjusted prospectively to reflect expected interest and mortality experience. To reduce our exposure to large individual losses, we purchase reinsurance from unaffiliated reinsurers.
Exiting Businesses
International Life Accident and Supplemental Benefits
These businesses, which are subject to a definitive sales agreement (Chubb Transaction) described in the "Overview" section of this Form 10-K, offer life, accident and supplemental benefits insurance products and services in Hong Kong, Indonesia, New Zealand, South Korea, Taiwan, Thailand and our interest in a joint venture in Turkey. South Korea represents our single largest geographic market for these businesses.
Supplemental health, life and accident insurance products and services generally provide simple, affordable coverage of risks for the health and financial security of individuals. Supplemental health products provide stated benefit payments for certain specified health risks and include personal accident, accidental death, critical illness, hospitalization, travel, dental, dementia, cancer and other specified condition coverages. We also offer customers term and variable universal life insurance and certain savings products in select markets.
Group Disability and Life
Prior to the sale in 2020, our Group Disability and Life operating segment included our commercial long-term and short-term disability products and our term life group insurance products. We also offered personal accident insurance and will continue to offer voluntary products and services that were not part of the sale. Beginning in 2021, voluntary products and services are reported in the Cigna Healthcare segment.
17
Run-off Businesses
Settlement Annuity Business
Our settlement annuity business is a closed, run-off block of single premium annuity contracts. These contracts are primarily liability settlements with approximately 20% of the liabilities associated with guaranteed payments not contingent on survivorship. Non-guaranteed payments are contingent on the survival of one or more parties involved in the settlement.
Reinsurance
Our reinsurance operations are an inactive business in run-off.
In February 2013, we effectively exited the GMDB and GMIB business by reinsuring 100% of our future exposures, net of retrocessional arrangements in place at that time, up to a specified limit. For additional information regarding this reinsurance transaction and the arrangements that secure our reinsurance recoverables, see Note 10 to the Consolidated Financial Statements.
Individual Life Insurance and Annuity and Retirement Benefits Businesses
This business includes deferred gains recognized from the 1998 sale of the individual life insurance and annuity business and the 2004 sale of the retirement benefits business. For more information regarding the arrangements that secure our reinsurance recoverables for the retirement benefits business, see Note 10 to the Consolidated Financial Statements.
DIGITAL, DATA AND TECHNOLOGY
Cigna's investments in digital, data and technology are focused on cultivating robust digital-first capabilities to better engage with customers and stakeholders. This engagement drives affordability, simplicity, predictability and growth across all of our business platforms. We deliver value for our clients, customers and other stakeholders by creating better health outcomes, improving customer experience and lowering total cost of care.
Innovation. Customer-centric, digital-first innovation remains at the forefront of our priorities. The advancement of our internal capabilities and strategic partnerships continues to produce new and more effective ways to engage with our customers to help close gaps in care, optimize treatment and improve outcomes. During 2021, our technology continued to deliver cost synergies and differentiated innovation in areas such as pharmacy supply chain, specialty pharmacy and retail networks. In the future, we expect continued value realization with focus on customer-facing systems and opportunities for enhanced value in specialty, claims and retail. (See Evernorth Intelligence Solutions section of the "Business - Evernorth" discussion of this Form 10-K for additional information on our intelligent solutions and capabilities).
Data and Analytics. Our rich, integrated data allows us to provide differentiated outcomes. We conduct timely, rigorous and objective research and analysis that informs evidence-based medical and pharmacy benefit management and evaluates the clinical, economic and individual impact of enhanced benefit designs and programs. The combination of our predictive analytics, as well as our machine and deep learning capabilities create actionable intelligence that informs decision-making of our health care professionals. Our data-driven approach to behavioral health provides personalized and customized care across the entire continuum for the populations we serve. These solutions predict emerging health needs, close gaps in care and drive cost savings - all while empowering whole-person and whole-family health.
During 2021, we continued to leverage both internal and external data related to COVID-19 to develop vaccination incentive programs, identify and address health disparities and better understand the long-term medical and behavioral complications among the American workforce. Employers can leverage this data to proactively offer physical and behavioral health support to ease their employees' recovery and return to work.
Digital. We continue to bring new technology-enabled products and services to the market, including biometric stress prediction and focused insights in spaces such as women's health and opioid addiction. Our digital health focus has shown value across the enterprise by creating engaging experiences that give customers the right information at the right time. This includes an enhanced MyCigna.com experience with new mobile features, including refill and payment options and better access to virtual care through our acquisition of MDLIVE. Cybersecurity protections, such as multi-factor authentication, have been launched across Cigna's digital offerings providing better peace of mind and a stronger sense of security.
18
Technology Operations. Our technology team, powered by approximately 8,000 employees and several thousand external resources working with our partners, supports the various information systems essential to our operations, including the health benefit claims processing systems and specialty and home delivery pharmacy systems. Uninterrupted point-of-sale electronic retail pharmacy claims processing is a significant operational requirement for our business. We believe we have substantial capacity for growth in our United States pharmacy claims processing facilities. Our pharmacy technology platform allows us to safely, rapidly and accurately adjudicate over one billion adjusted prescriptions annually. Our technology helps retail pharmacies focus on patient care and our real-time safety checks help avoid medication errors. The Cigna companies hold over 270 United States patents. We use these patents to protect our proprietary technological advances and to differentiate ourselves in the market.
INVESTMENT MANAGEMENT
Our investment operations provide investment management and related services for our various businesses, including the insurance-related invested assets in our General Account ("General Account Invested Assets"). We acquire or originate, directly or through intermediaries, a broad range of investments, including private placement and public securities, commercial mortgage loans, real estate, mezzanine, private equity partnerships and short-term investments. Invested assets also include policy loans that are fully collateralized by insurance policy cash values. We also enter into derivative financial instruments, primarily to minimize the risk of changes in foreign currency exchange rates on our investments and to manage the interest rate exposures of our long-term debt. Invested assets are managed primarily by our subsidiaries and, to a lesser extent, external managers with whom our subsidiaries contract. Net investment income is included as a component of adjusted income from operations for each of our segments and Corporate. Realized investment gains (losses) are reported by segment but excluded from adjusted income from operations. For additional information about invested assets, see the "Investment Assets" section of the MD&A and Notes 11 and 12 to the Consolidated Financial Statements.
We manage our investment portfolios to reflect the underlying characteristics of related insurance and contractholder liabilities and capital requirements, as well as regulatory and tax considerations pertaining to those liabilities and state investment laws. Insurance and contractholder liabilities range from short duration health care products to longer-term obligations associated with life insurance products and the run-off settlement annuity business. Assets supporting these liabilities are managed in segregated investment portfolios to facilitate matching of asset durations and cash flows to those of corresponding liabilities. Investment results are affected by the amount and timing of cash available for investment, economic and market conditions and asset allocation decisions. We routinely monitor and evaluate the status of our investments, obtaining and analyzing relevant investment-specific information and assessing current economic conditions, trends in capital markets and other factors such as industry sector, geographic and property-specific information.
Separate Accounts
Our subsidiaries or external advisors manage invested assets of Separate Accounts on behalf of contractholders, including the Cigna Pension Plan, variable universal life products sold through our corporate-owned life insurance business and other life insurance products. These assets are legally segregated from our other businesses and are not included in General Account Invested Assets. Income, gains and losses generally accrue directly to the contractholders.
STRATEGIC INVESTMENTS
In addition to the portfolio investments in our general and separate accounts discussed above (see "Investment Management" section) that support our insurance operations, we do targeted investing within the health care industry specifically. In 2018, Cigna committed $250 million to Cigna Ventures, our strategic corporate venture fund to invest in promising startups and growth-stage companies who, like us, are unlocking new growth possibilities in health care. Specifically, we invest in companies making groundbreaking progress in three strategic areas: insights / analytics, digital health / experience and care delivery / enablement. As of December 31, 2021, Cigna Ventures has seven venture capital partners and 15 existing direct investments. Through these deep partnerships we collaborate, innovate and develop new solutions that address critical market challenges of affordability, predictability and simplicity impacting the people we serve.
In 2021, Cigna made targeted investments to further drive growth. We continued to invest in our technology capabilities to produce new and more effective ways to operate, as well as engage with our customers. We intend to lead with digital engagement by creating connections between points of care and guiding customers to the optimal location and provider. Our modernized data and technology
19
ecosystem will empower us to integrate our assets, gather insights and engage with prospects and customers in new ways. For the year ended December 31, 2021, our capital expenditures for property, equipment and computer software were $1.2 billion.
Our acquisition of virtual telehealth leader MDLIVE demonstrates how we are responding to the dramatic increase in new models for accessing care and we see virtual care as accelerating improved affordability. Through MDLIVE, we have expanded access to virtual care services for millions of customers, with capabilities that now include primary and dermatological care, as well as behavioral health for conditions including anxiety and depression, and we plan to continue introducing additional services. Recently, we developed an approach for patients diagnosed with orthopedic and musculoskeletal conditions to provide highly personalized and actionable information to guide their choices and support improved health outcomes and affordability. We also launched an innovative virtual-first health plan option for employers, another step forward in providing convenient and comprehensive care experiences for our customers. See Note 4 to the Consolidated Financial Statements for further information on the MDLIVE acquisition.
In 2021, we committed to invest $550 million in preferred stock of Bright Health Group, Inc. ("Bright Health"), a technology-enabled health insurance carrier. This investment was completed in January 2022. We are committed to improving and expanding access to quality, affordable health care and our investment in Bright Health aligns with our vision. We seek to be partners of choice and look forward to exploring new ways to partner with Bright Health.
HUMAN CAPITAL MANAGEMENT
Cigna's mission is to improve the health, well-being and peace of mind of those we serve by enabling affordable, predictable and simple health care. A global healthy and diverse workforce is essential to achieving our mission and our business growth strategies. We are continually investing in our global workforce to support our employees' health and well-being, further drive diversity and inclusion, provide fair and market-competitive pay and foster their growth and development. As of the end of 2021, we had approximately 73,700 employees, with 89% of our employees based in the United States. Almost all of our employees are full-time, with less than 2% of employees regularly working fewer than 30 hours per week.
Health, Well-Being and Other Benefits
Tending to our employees' health, well-being and peace of mind is more than just our mission – it is a critical business imperative for our company. At Cigna, we believe that the provision of health and well-being benefits for our employees is our responsibility as an employer and should not be outsourced to the government or other third parties. Ensuring that our employees have comprehensive health and well-being benefits is not only the right thing to do from a societal perspective – it is also one of the most important investments in our enterprise that we make each year. That is because we strongly believe that a healthy workforce is more productive, has fewer absences and is a critical enabler for us to drive our business and our strategy forward, thereby creating significant shareholder value. In 2021, Cigna invested approximately 19% of total payroll in health, well-being and other benefits, including life and disability programs, 401(k) contributions and retirement-related benefits for its employees in the United States, which represents an increase from prior year attributed to medical spend and COVID-related benefits offered to employees.
In addition to traditional medical and pharmacy benefits, we provide mental health support to employees, including: employee assistance program (EAP) benefits that are free to all employees and to any member of their household, digital tools that provide access to education and therapy to help individuals build greater resilience and cope with stress, anxiety and depression.
Diversity, Equity & Inclusion
At Cigna, we take an expansive view of diversity including race, ethnicity, nationality, gender, veteran status, ability, sexual orientation and gender identity. As of the end of 2021, 70% of our employees were women, and 26% of our employees in the United States were from underrepresented groups (which includes Black/African American, Hispanic or Latinx, Pacific Islander and American Indian/Alaskan employees).
Our compensation practices, rooted in our pay-for-performance philosophy, promote equity in pay through measures such as benchmarking compensation by role, eliminating inquiries regarding applicants' compensation history from the hiring process and monitoring for potential disparities. Our most recent pay equity analysis, conducted in 2022, showed that in the United States, female employees at Cigna earn more than 99 cents for every dollar earned by similarly-situated male employees, and employees from underrepresented groups (as defined above) earn more than 99 cents for every dollar earned by similarly-situated white employees.
We are committed to attracting and recruiting key diverse talent across various leadership development programs and other entry level positions with the business. This success is rooted in strategic relationships with diverse student groups at our partner colleges and universities, as well as our commitment to multiple national, regional and local organizations, which provide us focused recruiting opportunities with women, the LGBTQA+ community, military veterans and underrepresented minority groups.
20
Talent Acquisition, Development and Retention
Our talent acquisition and rewards strategies are designed to ensure we attract and retain skilled employees who are engaged in our mission. Our compensation program is rooted in market competitive base salaries and incentives that reward contributions that advance the Company's strategy and mission. The COVID-19 pandemic has continued to impact our employee population, including increased worker attrition throughout the last year, which has affected many companies in what the media has dubbed the "great resignation." In 2021, the voluntary turnover rate was 8% for exempt employees in the United States.
Our online learning platform and career development tools and events offer a broad range of training, education and development resources to all employees. In 2021, U.S. employees on average engaged in 62 hours of learning through these resources. Enterprise leadership development programs were provided to executive, high-potential and new manager audiences to develop and expand leadership capability across the enterprise. Cigna also offers an education reimbursement program for both full and part-time employees who meet the continuing education criteria. We believe these strategies and programs contribute to employee engagement and retention.
MISCELLANEOUS
•Revenues from U.S. Federal Government agencies, under a number of contracts, represent 14% of our consolidated revenues in 2021 and 15% in 2020.
•The Company is not dependent on business from one or a few brokers or agents.
REGULATION
The laws and regulations governing our business continue to increase each year and are subject to frequent change. We are regulated by federal, state and international legislative bodies and agencies, which generally have discretion to issue regulations and interpret and enforce laws and rules. These regulations can vary significantly from jurisdiction to jurisdiction, and the interpretation of existing laws and rules also may change periodically. Domestic and international governments continue to enact and consider various legislative and regulatory proposals, which could materially impact the health care system. We expect continued legislative and regulatory debate of issues related to our businesses. As has become increasingly common with public policy reforms in the health services industry, executive, judicial or legislative intervention could alter, slow or eliminate the impact of any proposal following the related regulation's promulgation.
Many aspects of our business are directly regulated by federal and state laws and administrative agencies, such as the Department of Health and Human Services ("HHS"), Centers for Medicare and Medicaid Services ("CMS"), the Internal Revenue Service ("IRS"), the U.S. Departments of Labor ("DOL") and Treasury, the Office of Personnel Management ("OPM"), the Federal Trade Commission ("FTC"), the U.S. Securities and Exchange Commission ("SEC"), the Office of the National Coordinator for Health Information Technology ("ONC"), state departments of insurance and state boards of pharmacy. Our business practices may also be shaped by enforcement actions of federal agencies, such as the Department of Justice ("DOJ"), state agencies, as well as judicial decisions.
In addition, aspects of our business are subject to indirect regulation. The self-funded benefit plans sponsored by our U.S. employer clients are regulated under federal law. These self-funded clients expect us to ensure that our administration of their plans complies with the regulatory requirements applicable to them.
Our business operations and the books and records of our regulated businesses are routinely subject to examination and audit at regular intervals by state insurance and HMO regulatory agencies, state boards of pharmacy, CMS, DOL, IRS, OPM and comparable international regulators to assess compliance with applicable laws and regulations. Our operations are also subject to non-routine examinations, audits and investigations by various state and federal regulatory agencies, generally as the result of a complaint. In addition, we may be implicated in investigations of our clients whose group benefit plans we administer on their behalf. As a result, we routinely receive subpoenas and other demands or requests for information from various state insurance and HMO regulatory agencies, state attorneys general, the HHS Office of Inspector General ("HHS-OIG"), the DOJ, the DOL and other state, federal and international authorities. We may also be called upon by members of the U.S. Congress to provide information, including testifying before Congressional committees and subcommittees, regarding certain of our business practices. If Cigna is determined to have failed to comply with applicable laws or regulations, these examinations, audits, investigations, reviews, subpoenas and demands may:
•result in fines, penalties, injunctions, consent orders or loss of licensure;
•suspend or exclude us from participation in government programs or limit our ability to sell or market our products;
21
•require changes in business practices;
•damage relationships with the agencies that regulate us and affect our ability to secure regulatory approvals necessary for the operation of our business; or
•damage our brand and reputation.
Our international subsidiaries are subject to regulations in international jurisdictions, including in certain cases many regulations similar to the federal and state regulations described below, which are complex and where foreign insurers may face more rigorous regulations than their domestic competitors and may also be affected by geopolitical developments or tensions.
The laws and regulations governing our business, as well as the related interpretations, are subject to frequent change and can be inconsistent or in conflict with each other. Changes in our business environment are likely to continue as elected and appointed officials at the national and state levels continue to propose and enact significant modifications to existing laws and regulations. Even where we believe that we are in compliance with the various laws and regulations, any enforcement actions by federal, state or international government officials alleging non-compliance with these rules and regulations could subject us to penalties or restructuring or reorganization of our business. For a discussion of the risks related to our compliance with these laws and regulations see the Risk Factors section located in Part I, Item 1A of this Form 10-K. Management continues to be actively engaged with regulators and policymakers with respect to legislation and rulemaking.
COVID-19-related Regulatory Actions
In response to COVID-19 and its variants, U.S. federal and state governments have increasingly enacted new legislative and regulatory requirements, as well as provided flexibility to industry participants within existing legal requirements. These regulatory actions primarily provide for:
•client and customer premium relief to avoid the cancellation or non-renewal of policies;
•mandating or requesting waiver of customer cost-sharing and other related costs such as COVID-19 testing or treatment, as well as establishing provider reimbursement and vaccine immunizations coverage requirements;
•extending claims filing deadlines for providers, customers and facilities;
•mandating or encouraging waiver of customer cost-share related to telemedicine services, as well as requiring certain reimbursement levels for telemedicine providers to encourage its utilization;
•increasing the Medicare fee-for-service reimbursement for certain items and services;
•enacting coverage and reimbursement requirements at in-network levels for certain services received from out-of-network providers;
•clarification regarding permissible sharing of information and coordination among health care providers;
•revising or suspending the use of certain medical management procedures;
•mandating prescription drug benefit administration requirements primarily related to formulary exceptions and restrictions, and prior authorization and prescription drug refill limits; and
•requiring vaccinations for certain employee populations.
These actions are in effect for various durations, but generally track the different states of emergency that have been declared at the state and federal levels. Of particular significance is the Public Health Emergency declared by the Secretary of HHS on January 31, 2020, which sets the effective period for certain of the requirements established through federal COVID-19 legislation, such as covering testing without cost sharing.
Patient Protection and the Affordable Care Act
The Patient Protection and Affordable Care Act ("ACA") mandated broad changes to the U.S. health care system that affect insured and self-insured health benefit plans and pharmacy benefit managers. Our business model is impacted by the ACA, including our relationships with current and future producers and health care providers, products, service providers and technologies. The provisions of the ACA imposed, among other things, certain assessments on health insurers, created health insurance exchanges for individuals and small group employers to purchase insurance coverage and implemented minimum medical loss ratios ("MLRs") for our Medicare and commercial businesses. Certain states have adopted MLR requirements applicable to our commercial businesses that are more stringent than those established by the ACA. Other provisions of the ACA in effect include reduced Medicare Advantage payment rates, the requirement to cover preventive services with no enrollee cost-sharing, banning the use of lifetime and annual limits on the
22
dollar amount of essential health benefits, increasing restrictions on rescinding coverage, extending coverage of dependents up to age 26, restrictions on differential pricing, enforcement mechanisms and rules related to health care fraud and abuse enforcement activities and certain pharmacy benefit transparency requirements. The employer mandate requires employers with 50 or more full-time employees to offer affordable health insurance that provides minimum value (each as defined under the ACA) to full-time employees and their dependents, including children up to age 26, or be subject to penalties based on employer size. The ACA also changed certain tax laws to effectively limit tax deductions for certain employee compensation paid by health insurers. In December 2019, the federal government repealed the non-deductible health insurance industry fee effective for 2021, as well as the enacted but never implemented 40% excise tax on certain employer-sponsored coverage (known as the "Cadillac Tax") and the medical device tax. In 2021, in response to the COVID-19 pandemic, the federal government temporarily expanded eligibility for ACA subsidies to higher-income people who did not otherwise qualify, increased ACA subsidies for lower-income people who already qualify for 2021 and 2022, provided subsidies for individuals who receive unemployment benefits in 2021 and prevented taxpayers who misestimated their income in 2020 from having to repay excess premium tax credits. These subsidies may be extended further through proposed legislation.
Medicare and Medicaid Regulations
Through our subsidiaries, we offer individual and group Medicare Advantage, Medicare Prescription Drug ("Part D") and Medicare Supplement products. We also provide Medicare Part D-related products and services to other Medicare Part D sponsors, Medicare Advantage Prescription Drug Plans and employers and clients offering Medicare Part D benefits to Medicare Part D eligible beneficiaries, including those dually eligible for Medicare and Medicaid benefits ("dual-eligible"). As part of our Medicare Advantage and Medicare Part D business, we contract with CMS to provide services to Medicare beneficiaries. We offer dual-eligible products and participate in state Medicaid programs directly or indirectly through our clients who are Medicaid managed care contractors. We also perform certain Medicaid subrogation services and certain delegated services for clients, including utilization management, which are regulated by federal and state laws. Our dual-eligible products are regulated by CMS and state Medicaid agencies audit our performance to determine compliance with contracts and regulations. Our ability to obtain payment (and the determination of the amount of such payments), market to, enroll and retain customers and expand into new service areas is subject to compliance with CMS' numerous and complex regulations and requirements that are frequently modified and subject to administrative discretion, review and enforcement.
CMS evaluates Medicare Advantage plans and Part D plans under its "Star Rating" system. The Star Rating system considers various measures adopted by CMS, including, for example, quality of care, preventive services, chronic illness management, coverage determinations and appeals and customer satisfaction. A plan's Star Rating affects its image in the market and plans that perform very well are able to offer enhanced benefits and market more effectively and for longer periods of time than other plans. Medicare Advantage plans' quality-bonus payments are determined by the Star Rating, with plans receiving a rating of four or more stars eligible for such payments. The Star Rating system is subject to change annually by CMS, which may make it more difficult to achieve and maintain four stars or greater. For example, beginning with Star Ratings for payment year 2024, CMS will place more emphasis on patient experience survey-based measures which could reduce Star Ratings predictability year over year. Additionally, as a result of the COVID-19 pandemic's impact on 2020 care patterns and utilization, CMS finalized rules applying relief to Medicare Advantage and Part D Plan Star Ratings for payment year 2023 by utilizing the higher of the payment year 2023 or 2022 measure level Star Ratings.
CMS uses a risk-adjustment model that adjusts premiums paid to Medicare Advantage plans according to customers' health status. The risk-adjustment model generally pays more where a plan's membership is expected to have increased costs because of the health status of its members. Under this model, rates paid to Medicare Advantage plans are based on actuarially determined bids, which include a process whereby our prospective payments are based on our estimated cost of providing standard Medicare-covered benefits to an enrollee with a "national average risk profile." That baseline payment amount is adjusted to reflect the health status of our enrolled membership. Under the risk-adjustment methodology, Medicare Advantage plans must collect and submit the necessary diagnosis code information from hospital inpatient, hospital outpatient and physician providers to CMS within prescribed deadlines. We generally rely on providers to appropriately document their claims and other submissions with appropriate diagnoses from which we extract hierarchical condition codes to submit to CMS as the basis for our payments received under the actuarial risk-adjustment model. The CMS risk-adjustment model uses the diagnosis data to calculate the risk-adjusted premium payment to the plans. CMS may conduct audits to validate risk-adjustment data submitted by health plans. In 2012, CMS released a payment methodology that provided for sample audit error rates to be extrapolated to the entire Medicare Advantage contract after comparing audit results with a similar audit of Medicare Fee for Service (the "FFS Adjuster") and applying an FFS Adjuster to establish actuarial equivalency in payment rates as required by the Medicare statute. However, a methodology to calculate the FFS Adjuster was not finalized and CMS has, to date, not completed any Risk Adjustment Data Validation ("RADV") audits using extrapolation.
23
On November 1, 2018, CMS released a proposed rule titled "Proposed Rule on Changes to MA and Part D Programs for CY 2020 and 2021" that would revise its RADV methodology for RADV audits of contract year 2011 and all subsequent years by, among other things, extrapolating the error rate related to RADV audit findings without applying the FFS Adjuster. If the proposed rule is adopted in its current form, it could result in some combination of degraded plan benefits, higher monthly premiums and reduced choice for the population served by all MA insurers. The Company, along with other Medicare Advantage organizations and additional interested parties, submitted comments to CMS on the proposed rule as part of the notice-and-comment rulemaking process. The comment period concluded on August 28, 2019 and CMS issued guidance on October 20, 2021 extending the timeline to finalize the proposed rule until November 2022. RADV audits for our contract years 2011 through 2015 are currently in process. It is uncertain whether CMS will finalize the rule as proposed. See below under "Federal and State Oversight of Government-Sponsored Health Care Programs" for a discussion of RADV audits.
Coverage of prescription drugs under Medicare Part D is also regulated by CMS and our contracts with CMS contain provisions for risk sharing and certain payments for prescription drug costs for which we are not at risk. These provisions affect our ultimate payments from CMS. For example, premiums from CMS are subject to risk corridor payments that compare costs targeted in our annual bids with actual prescription costs, limited to actual costs that would have been incurred under the standard coverage as defined by CMS. Variances exceeding certain thresholds may result in CMS making additional payments to us or require us to refund to CMS a portion of the payments we received.
We expect CMS, HHS-OIG, DOJ and other federal agencies to continue to closely scrutinize each component of the Medicare Advantage program and modify the terms and requirements of the program through rulemaking or enforcement activities. Noncompliance with these laws and regulations may result in significant consequences, including fines and penalties, enrollment sanctions, exclusion from the Medicare and Medicaid programs, limitations on expansion and criminal penalties.
False Claims Act and Anti-Kickback Laws
Our products and services are also subject to the federal False Claims Act (the "False Claims Act"), state false claims acts and federal and state anti-kickback laws. Additionally, the federal government has made investigating and prosecuting health care fraud, waste and abuse a priority. Fraud, waste and abuse prohibitions encompass a wide range of activities, including kickbacks in return for customer referrals, billing for unnecessary medical services, upcoding and improper marketing. The regulations and contractual requirements in this area are complex, frequently modified and subject to administrative discretion and judicial interpretation.
False Claims Act and Related Criminal Provisions. The False Claims Act imposes civil penalties on any person who knowingly, as defined by the statute, makes, conspires to make, or causes to be made false claims, records, or statements, or fails to return known overpayments, in connection with reimbursement by federal government programs such as Medicare and Medicaid. Private individuals may bring qui tam or "whistleblower" suits under the False Claims Act, which authorizes the payment of a portion of any recovery to the individual bringing suit. The ACA amended the federal anti-kickback laws to state any claim submitted to a federal or state health care program that violates the anti-kickback laws is also a false claim under the False Claims Act. The False Claims Act generally provides for the imposition of civil penalties and for treble damages, creating the possibility of substantial financial liabilities. Criminal statutes similar to the False Claims Act provide that if a corporation is convicted of presenting a claim or making a statement it knows to be false, fictitious or fraudulent to any federal agency, the corporation may be fined. Conviction under these statutes may also result in exclusion from participation in federal and state health care programs. Many states have also enacted laws similar to the False Claims Act, some of which may include criminal penalties, substantial fines and treble damages.
Anti-Kickback and Referral Laws. Subject to certain exceptions and "safe harbors," the federal anti-kickback statute generally prohibits, among other things, knowingly and willfully paying, receiving or offering any payment or other remuneration to induce a person to purchase, lease, order or arrange for items (including prescription drugs) or services reimbursable in whole or in part under Medicare, Medicaid or another federal health care program. Many states have similar laws, some of which are not limited to items or services paid for with government funds. Sanctions for violating these federal and state anti-kickback laws may include criminal and civil fines and exclusion from participation in federal and state health care programs.
Anti-kickback laws have been cited as a partial basis, along with state consumer protection laws described below, for investigations and multi-state settlements relating to financial incentives provided by drug manufacturers to pharmacies or payors in connection with "product conversion" or promotion programs. Other anti-kickback and referral laws may also be applicable including criminal and civil laws restricting illegal kickbacks and conflicts of interest in connection with plans governed by the Employee Retirement Income Security Act of 1974, as amended ("ERISA"), the federal "Stark Law," and various state anti-kickback restrictions.
In November 2020, HHS and HHS-OIG released a final rule that eliminates an anti-kickback regulatory safe harbor protection for price concessions, including rebates, that are offered by pharmaceutical manufacturers to plan sponsors or pharmacy benefit managers
24
under the Medicare Part D program. The final rule creates two new safe harbors: (i) for price reductions by manufacturers to plan sponsors under Medicare Part D and Medicaid managed care organizations that are reflected at the time of dispense and (ii) for fixed-fee service arrangements between manufacturers and pharmacy benefit managers. The effective date of the final rule has been postponed to January 2026. A full repeal of the final rule is included in pending legislation.
Federal Civil Monetary Penalties Law. The federal civil monetary penalty statute provides for civil monetary penalties against any person who gives something of value to a Medicare or Medicaid program beneficiary that the person knows or should know is likely to influence the beneficiary's selection of a particular provider for Medicare or Medicaid items or services. Under this law, our wholly-owned home delivery pharmacies, specialty pharmacies and home health providers are restricted from offering certain items of value to influence a Medicare or Medicaid patient's use of services. The ACA also includes several civil monetary provisions, such as penalties for the failure to report and return a known overpayment and failure to grant timely access to the HHS-OIG under certain circumstances.
Federal and State Oversight of Government-Sponsored Health Care Programs
Participation in government-sponsored health care programs subjects us to a variety of federal and state laws and regulations and risks associated with audits conducted under these programs. These audits may occur years after the provision of services. Risks include potential fines and penalties, restrictions on our ability to participate or expand our presence in certain programs and restrictions on marketing our plans. For example, with respect to our Medicare Advantage business, CMS and the HHS-OIG perform audits to determine a health plan's compliance with federal regulations and contractual obligations, including program audits and Risk Adjustment Data Validation Audits, which focus on compliance with proper coding practices. Certain of our contracts are currently subject to audits by CMS and the HHS-OIG, including RADV audits. CMS has announced that its goal is to subject all Medicare Advantage contracts to either a comprehensive or a targeted RADV audit for each contract year. The DOJ is also currently conducting industry-wide investigations of the risk adjustment data submission practices and business processes of Cigna and a number of other Medicare Advantage organizations. See Note 22 to the Consolidated Financial Statements for more information.
For our Medicare Part D business, compliance with certain contractual provisions and regulatory requirements is subject to review by Recovery Audit Contractor audits in which third-party contractors conduct post-payment reviews on a contingency fee basis to detect and correct improper payments.
Government Procurement Regulations
We have a contract with the U.S. Department of Defense ("DoD"), which subjects us to applicable Federal Acquisition Regulations ("FAR") and the DoD FAR Supplement, which govern federal government contracts. Further, there are other federal and state laws applicable to our DoD arrangement and our arrangements with other clients that may be subject to government procurement regulations. In addition, certain of our clients participate as contracting carriers in the Federal Employees Health Benefits Program administered by the OPM, which includes various pharmacy benefit management standards.
Employee Retirement Income Security Act
Our domestic subsidiaries sell most of their products and services to sponsors of employee benefit plans that are governed by ERISA. ERISA is a complex set of federal laws and regulations enforced by the IRS and the DOL, as well as the courts. ERISA regulates certain aspects of the relationship between us, the employers that maintain employee welfare benefit plans subject to ERISA and the participants in such plans. Certain of our domestic subsidiaries are also subject to requirements imposed by ERISA affecting claim payment and appeals procedures for individual health insurance and insured and self-insured group health plans and for the insured plans we administer. Certain of our domestic subsidiaries also may contractually agree to comply with these requirements on behalf of the self-insured plans they administer. We believe the conduct of our pharmacy benefit management business is not generally subject to the fiduciary obligations of ERISA. However, there can be no assurances that the DOL may not assert that pharmacy benefit managers are fiduciaries. From time to time, states have considered legislation to declare a pharmacy benefit manager or health benefit manager a fiduciary with respect to its clients.
Plans subject to ERISA may also be subject to state laws and the legal question of whether and to what extent ERISA preempts a state law is likely to continue to be a subject for interpretation by the courts for years to come.
Privacy, Security and Data Standards Regulations
Many of our activities involve the receipt or use of confidential health and other personal information. In addition, we use aggregated and de-identified data for our own research and analysis purposes and, in some cases, provide access to such de-identified data, or analytics created from such data, to pharmaceutical manufacturers and third-party data aggregators. We may also use such information
25
to create analytic models designed to predict, and potentially improve, outcomes and patient care. There are also industry standards for handling credit card data known as the Payment Card Industry Data Security Standard, which are a set of requirements designed to help ensure that entities that process, store or transmit credit card information maintain a secure environment. Certain states have incorporated these requirements into state laws or enacted other requirements for using and disclosing personal information. Additionally, over the past several years, various broad privacy laws have been introduced into one or both chambers of Congress, however, to date, none have been enacted.
The federal Health Insurance Portability and Accountability Act of 1996 and its implementing regulations ("HIPAA") impose minimum standards on health insurers, pharmacy benefit managers, HMOs, health plans, health care providers and clearinghouses for the privacy and security of protected health information. HIPAA regulations may also hold us liable for violations by our business associates (e.g., entities that provide services to health plans and providers). HIPAA also established rules that standardize the format and content of certain electronic transactions, including, but not limited to, eligibility and claims. To the extent insurers offer plans through a public exchange, participants and their downstream entities such as pharmacy benefit managers must adhere to privacy and security standards for personally identifiable information and to impose standards that are at least as protective as those the exchange has implemented for itself. These standards may differ from, and be more stringent than, HIPAA.
The Health Information Technology for Economic and Clinical Health Act ("HITECH") imposes additional contracting requirements for covered entities, the extension of privacy and security provisions to business associates, the requirement to provide notification to various parties in the event of a data breach of protected health information and enhanced financial penalties for HIPAA violations, including potential criminal penalties for individuals. In the conduct of our business, depending on the circumstances, we may act as either a covered entity or a business associate.
The federal Gramm-Leach-Bliley Act ("GLBA") and its implementing regulations generally place restrictions on the disclosure of nonpublic information to nonaffiliated third parties, and requires financial institutions, including insurers, to provide customers with notice regarding how their nonpublic personal information is used, including an opportunity to "opt out" of certain disclosures. State departments of insurance and certain federal agencies adopted implementing regulations as required by federal law.
State and local authorities are increasingly focused on protecting individuals from identity theft and a number of states have adopted comprehensive data security laws and regulations requiring, among other things, certain minimum data security standards and security breach notifications that may apply to us in certain circumstances, as well as certain limitations on access to and use of personal information. Neither HIPAA nor the GLBA privacy regulations preempt more stringent state laws and regulations which may differ in approach and enforcement.
States have, in recent years, begun to adopt their own omnibus, industry-neutral privacy statutes. To date, three states have passed such laws: California, which originally went into effect in 2020 and has been subsequently amended to strengthen consumer rights; as well as Colorado and Virginia, both effective in 2023. Generally, these statutes are not applicable to data regulated by GLBA and HIPAA but are, in varying respects, applicable to other data we collect, such as personal data provided by website visitors, employees and business partners. We anticipate federal and state legislators and regulators to continue to enact legislation related to privacy and cybersecurity, including with respect to ransomware incidents.
Under Section 5 of the Federal Trade Commission Act ("FTC Act"), the FTC has jurisdiction over certain privacy and security practices. Section 5 of the FTC Act bars unfair and deceptive acts and practices in or affecting commerce and the FTC has charged companies with violating this act based on failures to appropriately and transparently safeguard personal information and respect consumers' privacy rights. In addition to the FTC Act, the FTC also enforces other federal laws relating to consumers' privacy and security. The FTC has also been active with respect to companies' use of big data and artificial intelligence ("AI"), specifically ensuring fair and equitable use of these tools, and the FTC has named AI as an area of enforcement focus. State legislatures and regulators are similarly interested in the use of AI, particularly as it is used in modeling, and a handful of states have either passed legislation or issued regulatory guidance concerning AI. Additionally, the National Association of Insurance Commissioners ("NAIC"), an organization of state insurance regulators, recently established the Innovation, Cybersecurity and Technology Committee to provide a forum for regulators to learn, monitor and confer on emerging technology issues, including, among others, cybersecurity and AI.
The Cybersecurity Information Sharing Act of 2015 ("CISA") encourages organizations to share cyber threat indicators with the federal government and, among other things, directs HHS to develop a set of voluntary cybersecurity best practices for organizations in the health care industry. States have also begun to issue regulations specifically related to cybersecurity, which may differ or conflict from state to state. In October 2017, the NAIC adopted the Insurance Data Security Model Law that creates rules for insurers and other covered entities addressing data security, investigation and notification of breaches. This includes maintaining an information security program based on ongoing risk assessment, overseeing third-party service providers, investigating data breaches
26
and notifying regulators of a cybersecurity event. As the model law is intended to serve as model legislation only, states will need to enact legislation for the model law to become mandatory and enforceable. To date, eleven states have enacted some form of the model law.
HHS, including the ONC, the Office for Civil Rights and CMS, has enacted regulations, and proposed additional regulations, to support the seamless and secure access, exchange and use of electronic health information by or between patients, enrollees and entities such as payers and health care providers, which is generally termed "interoperability." These regulations include, among others, proposed changes to HIPAA designed to promote greater patient access and control over health information maintained by health plans and health care providers and improve information sharing for case management and care coordination. Other interoperability regulations prohibit information blocking by certain entities and require certain regulated plans to make specified patient, clinical and plan-related data available to enrollees via interoperable technology and applications. These regulations apply to a variety of entities, including health plans like Medicare plans and qualified health plans, as well as health care providers, certified health information technology developers and health information networks and exchanges and generally require significant enhancements to information technology and data governance practices. The regulations and proposals demonstrate an increased interest in information sharing and will impact how industry participants, including us, comply with disclosure requirements and share information with individuals and other healthcare organizations. We continue to monitor developments and to submit comments on proposed regulations where appropriate.
In addition, international laws, rules and regulations governing the use and disclosure of personal information can be more stringent than those in the United States, and they vary from jurisdiction to jurisdiction. The European Union's General Data Protection Regulation ("GDPR"), which became effective May 2018, enhanced or created obligations regarding the handling of personal data relating to European residents (such as regarding notices, data protection impact assessments and individual rights) and provides for greater penalties for noncompliance than the previous European Directive or laws. In addition, many countries outside of Europe where we conduct business have implemented or may implement data protection laws and regulations, some of which include requirements modeled after those in the GDPR. Some non-U.S. jurisdictions are also instituting data residency regulations requiring that data be maintained within the respective jurisdiction or otherwise restricting transfer of personal data across borders unless specified regulatory requirements are met.
See Part I. Item 1A, "Risk Factors" for a discussion of the risks related to compliance with privacy and security regulations.
Consumer Protection Laws
We engage in direct-to-consumer activities and are increasingly offering mobile and web-based solutions to our customers. We are therefore subject to federal and state regulations applicable to electronic communications and other consumer protection laws and regulations, such as the Telephone Consumer Protection Act and the CAN-SPAM Act. With the ever increasing reliance and demand by consumers on using their mobile devices for convenient communications, we face increased risk under these laws. The FTC is also increasingly exercising its enforcement authority in the areas of consumer privacy and data security, with a focus on web-based, mobile data and "big data." Federal consumer protection laws may also apply in some instances to privacy and security practices related to personally identifiable information.
State and federal policymakers have taken actions intended to increase transparency and predictability of health care costs for consumers. For example, in October 2020, the HHS, the DOL and the Department of the Treasury issued a final rule that requires most group health plans and health insurance issuers in the individual and group markets to disclose price and cost-sharing information for all items and services to participants and enrollees. The cost-sharing information requirements under the rule take effect in a phased approach beginning January 1, 2023. In addition to providing personalized cost-sharing information, beginning January 1, 2022, health plans and health insurers must also publicly disclose (i) in-network provider negotiated rates, (ii) historical out-of-network allowed amounts and billed charges and (iii) in-network negotiated rates and historical net prices for all covered prescription drugs. Beginning in 2021, insurers will be able to receive credit in their MLR calculations for certain savings they share with enrollees. In August 2021, the departments jointly released guidance regarding the implementation of the rule. Importantly, the guidance announced that the agencies will (i) indefinitely defer enforcement of the rule's requirement that plans and issuers publish machine-readable files relating to prescription drug pricing pending further rulemaking and (ii) defer enforcement of the rule's requirement to publish the remaining machine-readable files until July 1, 2022. Congress also passed the Consolidated Appropriations Act, 2021 ("CAA"), which included a number of transparency requirements on plans and issuers that are duplicative or overlap with the October 2020 rule issued by the departments. The indefinite enforcement deferral of the prescription drug pricing file under the October 2020 rule is, in part, due to the subsequent enactment of the CAA, which requires plans to report information regarding prescription drug spending to federal regulators beginning in 2022.
27
As part of the aforementioned CAA, Congress passed the No Surprises Act, which prohibits health care providers, in certain situations, from balance billing the patient and requires that they work directly with insurers to agree on out-of-network reimbursement, including utilizing an independent dispute resolution process outlined in the act. The act is effective January 1, 2022. Many states already have addressed balance billing, or surprise medical bills. These laws and regulations vary in their approach, resulting in different impacts on the health care system as a whole.
Additionally, most states have consumer protection laws that have been the basis for investigations and multi-state settlements relating to financial incentives provided by drug manufacturers to retail pharmacies in connection with product conversion programs. Such statutes have also been cited as the basis for claims or investigations by state attorneys general relative to privacy and data security.
Office of Foreign Assets Control Sanctions and Anti-Money Laundering
We are also subject to regulation by the Office of Foreign Assets Control of the U.S. Department of the Treasury, which administers and enforces economic and trade sanctions against targeted foreign countries and regimes based on U.S. foreign policy and national security goals. Certain of our products are subject to the Department of the Treasury anti-money laundering regulations under the Bank Secrecy Act. In addition, we are subject to similar regulations in non-U.S. jurisdictions in which we operate.
Corporate Practice of Medicine and Other Laws
Many states in which our subsidiaries operate limit the practice of medicine to licensed individuals or professional organizations comprised of licensed individuals, and business corporations generally may not exercise control over the medical decisions of physicians. Statutes and regulations relating to the practice of medicine, fee-splitting between physicians and referral sources and similar issues vary widely from state to state. Under management agreements between certain of our subsidiaries and physician-owned professional groups, these groups retain sole responsibility for all medical decisions, as well as for hiring and managing physicians and other licensed health care providers, developing operating policies and procedures, implementing professional standards and controls and maintaining malpractice insurance. We believe that our health services operations comply with applicable state statutes regarding corporate practice of medicine, fee-splitting and similar issues. However, any enforcement actions by governmental officials alleging noncompliance with these statutes could subject us to penalties or restructuring or reorganization of our business.
Utilization Management Laws
State legislatures have begun to propose and enact laws exempting certain providers from pre-authorization requirements of insurers. These exemptions reduce the ability for insurers and medical management entities from reviewing services for medical necessity if the provider meets the law's established thresholds for approval rates in the preceding six months. The inability to apply pre-authorization requirements could lead to increased costs to plan issuers by way of the provision of unnecessary services. States are also standardizing the process for, and restricting the use of, utilization management rules and shortening the time frames within which prescription drug prior authorization determinations must be made. Even where states do not regulate pharmacy benefit or utilization management companies directly, these laws will apply to many of our clients, including managed care organizations and health insurers.
Laws and Legislation Affecting Pharmacy Benefit Plan Design, Administration and Pharmacy Network Access
Some states have enacted laws that prohibit managed care plan sponsors from implementing certain restrictive benefit plan design features, and many states have laws or have introduced legislation to regulate various aspects of managed care plans, including provisions relating to the pharmacy benefit. For example, some states, under so-called "freedom of choice" legislation, provide customers of the plan may not be required to use network providers, but must instead be provided with benefits even if they choose to use non-network providers. Some states have also enacted legislation that can negatively impact the use of cost-saving network configurations for plan sponsors, such as limiting the implementation of pharmacy benefit designs and reimbursement structures that leverage affiliate pharmacies to reduce costs. Other states have enacted legislation purporting to prohibit health plans from offering customers financial incentives for use of home delivery pharmacies. Medicare and some states have issued guidance and regulations that limit our ability to fill or refill prescriptions electronically submitted by a physician to our home delivery pharmacy without first obtaining consent from the patient. Such restrictions generate additional costs and limit our ability to maximize efficiencies, which could otherwise be gained through the electronic prescription and automatic refill processes. Legislation has been introduced in some states to prohibit or restrict therapeutic intervention, or to require coverage of all Food and Drug Administration approved drugs. Other states mandate coverage of certain benefits or conditions, and require health plan coverage of specific drugs if deemed medically necessary by the prescribing physician.
Additionally, Medicare Part D and a majority of states now have laws, regulations or some form of legislation affecting our ability, or our clients' ability, to limit access to a pharmacy provider network or remove a provider from a network. Such laws, regulations or
28
legislation may require us or our clients to admit any retail pharmacy or provider willing to meet the plan's terms and conditions for network participation ("any willing provider") or may direct that a provider may not be removed from a network except in compliance with certain procedures ("due process").
Certain states have laws prohibiting certain pharmacy benefit management clients from imposing additional copayments, deductibles, limitations on benefits, or other conditions on covered individuals utilizing a retail pharmacy when the same conditions are not otherwise imposed on covered individuals utilizing home delivery pharmacies. However, the laws require the retail pharmacy to agree to the same reimbursement amounts and terms and conditions as are imposed on the home delivery pharmacies. An increase in the number of prescriptions filled at retail pharmacies may have a negative impact on the number of prescriptions filled through home delivery.
Pharmacy Benefit Manager and Drug Pricing Regulation
Our pharmacy benefit management services are subject to numerous laws and regulations. These laws and regulations govern, and proposed legislation and regulations may govern, critical practices, including: disclosure, receipt and retention of rebates and other payments received from pharmaceutical manufacturers; certain pharmacy contracting practices including disclosure of cost information to customers; the receipt and retention of transmission fees from contracted pharmacies; use of, administration of, or changes to drug formularies, the use and disclosure of maximum allowable cost ("MAC") pricing, or clinical programs; "most favored nation" pricing, which provides that a pharmacy participating in a specific government program must give the program the best price the pharmacy makes available to any third-party plan; disclosure of data to third parties; drug utilization management practices; the level of duty a pharmacy benefit manager owes its clients or customers; configuration of pharmacy networks; the operations of our subsidiary pharmacies; disclosure of negotiated provider reimbursement rates; disclosure of negotiated drug rebates, calculation of certain customer cost-share for prescription drug claims; pricing that includes differential or spread (i.e., a difference between the drug price charged to the plan sponsor by a pharmacy benefit manager and the price paid by the manager to the dispensing provider); disclosure of fees associated with administrative service agreements and patient care programs that are attributable to customers' drug utilization; and registration or licensing of pharmacy benefit managers.
We expect federal and state governments to continue to prioritize means of addressing out-of-pocket costs for consumers, particularly related to prescription drug costs. Policy proposals, issued via regulation or legislation, vary broadly in their approaches to achieve that goal. Current proposed legislation includes, among other things: repeal of HHS's final rule amending the anti-kickback safe harbors, as described above under the heading "False Claims Act and Anti-Kickback Laws—Anti-Kickback and Referral Laws" government price negotiation of certain classes of prescription drugs covered by Medicare Part B and D; limits on manufacturer price increases for prescription drugs; and a redesign of the Medicare Part D benefit. Additionally, proposals at the federal and state levels consider increased regulation of pharmacy benefit managers and health plans as a means to limit consumer out-of-pocket costs, including: proposing to limit the use of various pharmacy benefit management tools; mandating the treatment of fees, discounts or financing mechanisms that otherwise are set in private contractual terms; increasing supply chain transparency; expanding regulatory requirements or definitions of fiduciaries; or mandating plan benefit designs that cap consumer out-of-pocket expense.
Some states have enacted statutes regulating the use of MAC pricing. These statutes, referred to as "MAC Transparency Laws," generally require pharmacy benefit managers to disclose specific information related to MAC pricing to pharmacies and provide certain appeal rights for pharmacies. MAC Transparency Laws also restrict the application of MAC and may require operational changes to maintain compliance with the law. Some states have also enacted laws regulating pharmacy pricing and protecting the profitability of pharmacies for dispensing certain MAC-priced drugs. Some states have enacted laws requiring that the customer cost-share for a prescription drug claim not exceed certain price points, such as the pharmacy's usual and customary charge or its contracted reimbursement for the drug. In a recent Supreme Court decision, the Court found that certain MAC Transparency Laws may be applied by states to ERISA plans in addition to health plans regulated by the applicable state. Following this decision, state legislatures and regulators have sought to extend their oversight authority of self-funded ERISA plans to pharmacy benefit management functions and pharmacy benefit plan designs beyond MAC pricing.
In March 2018, the NAIC adopted changes to the Health Carrier Prescription Drug Benefit Management Model Act. The changes address issues relating to: (i) transparency, accuracy and disclosure regarding prescription drug formularies and formulary changes during a policy year; (ii) accessibility of prescription drug benefits using a variety of pharmacy options; and (iii) tiered prescription drug formularies and discriminatory benefit design. While the actions of the NAIC do not have the force of law, they are used as a template to influence states to adopt laws based on the model legislation.
The federal Medicaid Drug Rebate Program requires participating drug manufacturers to provide rebates on all drugs reimbursed through state Medicaid programs, including through Medicaid managed care organizations. Manufacturers of brand-name products must provide a rebate equivalent to the greater of (a) 23.1% of the average manufacturer price ("AMP") paid by retail community
29
pharmacies or by wholesalers for certain drugs distributed to retail community pharmacies, or (b) the difference between AMP and the "best price" available to essentially any customer other than the Medicaid program and certain other government programs, with certain exceptions. We negotiate rebates with drug manufacturers and, in certain circumstances, sell services to drug manufacturers. Investigations are being and have been conducted by certain government entities which call into question whether a drug's "best price" was properly calculated and reported with respect to rebates paid by the manufacturers to the Medicaid programs. We are not responsible for such calculations, reports or payments.
Pharmacy Regulation
Our home delivery and specialty pharmacies also subject us to extensive federal, state and local regulation. The practice of pharmacy is generally regulated at the state level by state boards of pharmacy. We are licensed to do business as a pharmacy in the states in which our pharmacies are located. Most of the states into which we deliver pharmaceuticals have laws that require out-of-state home delivery pharmacies to register with, or be licensed by, the board of pharmacy or a similar regulatory body in the state. These states generally permit the pharmacy to follow the laws of the state where the pharmacy is located, although some states require compliance with certain laws in that state as it impacts or relates to drugs distributed or dispensed into that state.
Our various pharmacy facilities also provide services under certain Medicare and state Medicaid programs. Participation in these programs requires our pharmacies to comply with the applicable Medicare and Medicaid provider rules and regulations, and exposes the pharmacies to various changes the federal and state governments may impose regarding reimbursement methodologies and amounts to be paid to participating providers under these programs. In addition, several of our pharmacy facilities are participating providers under Medicare Part D and are required to adhere to certain requirements applicable to Medicare Part D. Additionally, we are subject to CMS rules regarding the administration of our Medicare plans and pricing between our plans and related parties, including our pharmacy business.
Other statutes and regulations affect our home delivery and specialty pharmacy operations, including the federal and state anti-kickback laws and the federal civil monetary penalty law described above. Federal and state statutes and regulations govern the labeling, packaging, advertising, adulteration and security of prescription drugs and the dispensing of controlled substances and certain of our pharmacies must register with the U.S. Drug Enforcement Administration and individual state controlled substance authorities. The FTC requires mail order sellers of goods generally to engage in truthful advertising, to stock a reasonable supply of the product to be sold, to fill mail orders within thirty days and to provide clients with refunds when appropriate. The United States Postal Service also has significant statutory authority to restrict the delivery of drugs and medicines through the mail.
Financial Reporting, Internal Control and Corporate Governance
Regulators closely monitor the financial condition of licensed insurance companies and HMOs. States regulate the form and content of statutory financial statements, the type and concentration of permitted investments and corporate governance over financial reporting. Our insurance and HMO subsidiaries are required to file periodic financial reports and schedules with regulators in most of the jurisdictions in which they do business as well as annual financial statements audited by independent registered public accounting firms. Certain insurance and HMO subsidiaries are required to file an annual report of internal control over financial reporting with most jurisdictions in which they do business. Insurance and HMO subsidiaries' operations and financial statements are subject to examination by such agencies. Many states have expanded regulations relating to corporate governance and internal control activities of insurance and HMO subsidiaries as a result of model regulations adopted by the NAIC with elements similar to corporate governance and risk oversight disclosure requirements under federal securities laws.
Guaranty Associations, Indemnity Funds, Risk Pools and Administrative Funds
Most states and certain non-U.S. jurisdictions require insurance companies to support guaranty associations or indemnity funds that are established to pay claims on behalf of insolvent insurance companies. Some states have similar laws relating to HMOs and other payors, such as consumer operated and oriented plans (co-ops) established under the ACA. In the United States, these associations levy assessments on member insurers licensed in a particular state to pay such claims. Certain states require HMOs to participate in guaranty funds, special risk pools and administrative funds. For additional information about guaranty funds and other assessments, see Note 22 to the Consolidated Financial Statements.
Certain states continue to require health insurers and HMOs to participate in assigned risk plans, joint underwriting authorities, pools or other residual market mechanisms to cover risks not acceptable under normal underwriting standards, although some states have eliminated these requirements as a result of the ACA.
30
Solvency and Capital Requirements
Many states have adopted some form of the NAIC model solvency-related laws and risk-based capital ("RBC") rules for life and health insurance companies and HMOs. The RBC rules recommend a minimum level of capital depending on the types and quality of investments held, the types of business written and the types of liabilities incurred. If the ratio of the insurer's adjusted surplus to its RBC falls below statutorily required minimums, the insurer could be subject to regulatory actions ranging from increased scrutiny to conservatorship.
In addition, various non-U.S. jurisdictions prescribe minimum surplus requirements that are based upon solvency, liquidity and reserve coverage measures. Our HMOs and life and health insurance subsidiaries, as well as non-U.S. insurance subsidiaries, are compliant with applicable RBC and non-U.S. surplus rules.
The Risk Management and Own Risk and Solvency Assessment Model Act ("ORSA"), adopted by the NAIC, provides requirements and principles for maintaining a group solvency assessment and a risk management framework and reflects a broader approach to U.S. insurance regulation. ORSA includes a requirement to file an annual ORSA Summary Report in the lead state of domicile. To date, an overwhelming majority of the states have adopted the same or similar versions of ORSA. We file our ORSA report annually as required.
Holding Company Laws
Our domestic insurance companies and certain of our HMOs are subject to state laws regulating subsidiaries of insurance holding companies. Under such laws, certain dividends, distributions and other transactions between an insurance company or an HMO subsidiary and its affiliates may require notification to, or approval by, one or more state insurance commissioners. In addition, the holding company acts of states in which our subsidiaries are domiciled restrict the ability of any person to obtain control of an insurance company or HMO subsidiary without prior regulatory approval. State holding company laws and regulations also subject our insurance companies and certain HMO subsidiaries to additional regulatory scrutiny related to their oversight of affiliates performing regulated services on behalf of the insurance company or HMO and require the Company to file an annual Enterprise Risk Report, which summarizes material risks that could pose enterprise risk to the insurance company subsidiaries.
Marketing, Advertising and Products
In most states, our insurance companies and HMO subsidiaries are required to certify compliance with applicable advertising regulations on an annual basis. Our insurance companies and HMO subsidiaries are also required by most states to file and secure regulatory approval of products prior to the marketing, advertising and sale of such products.
Licensing and Registration Requirements
Our insurance companies and HMO subsidiaries must be licensed by the jurisdictions in which they conduct business. Additionally, certain subsidiaries contract to provide claim administration, utilization management and other related services for the administration of self-insured benefit plans. These subsidiaries may be subject to state third-party administration and other licensing requirements and regulation, as well as third-party accreditation requirements.
We have received full accreditation for Utilization Review Accreditation Commission Pharmacy Benefit Management version 2.2 Standards, which includes quality standards for drug utilization management, and select subsidiaries have received full accreditation for Utilization Review Accreditation Commission for Health Utilization Management version 7.2, which includes quality standards for medical utilization management.
Certain states have adopted pharmacy benefit management registration, licensure or disclosure laws. In addition to registration laws, some states have adopted legislation mandating disclosure of various aspects of our financial practices, including those concerning pharmaceutical company revenue, as well as prescribing processes for prescription switching programs and client and provider audit terms.
Our international subsidiaries are often required to be licensed when entering new markets or starting new operations in certain jurisdictions. The licensure requirements for these subsidiaries vary by country and are subject to change.
International Regulations
Our operations outside the United States expose us to laws of multiple jurisdictions and the rules and regulations of various governing bodies and regulators, including those related to the provision of insurance, financial and other disclosures, the provision of health
31
care-related services, corporate governance, privacy, data protection, data mining, data transfer, intellectual property, labor and employment, consumer protection, direct-to-consumer communications activities, tax, anti-corruption and anti-money laundering. Foreign laws and rules may include requirements that are different from, or more stringent than, similar requirements in the United States.
Our operations in countries outside the United States:
•are subject to local regulations of the jurisdictions where we operate;
•in some cases, are subject to regulations in the jurisdictions where customers reside; and
•in all cases, are subject to the Foreign Corrupt Practices Act ("FCPA").
In particular, in South Korea, regulators are focused on protecting the rights of individual customers by enforcing "Treating Customers Fairly" concepts. This regulatory focus has resulted in rigorous data localization requirements, network separation obligations and system monitoring restrictions, as well as obligations to closely monitor marketing communications and sales scripts. Anti-money laundering requirements in South Korea and other countries where we do business also may impose obligations to collect certain information about each customer at time of sale or to risk rank each customer to determine possible future money laundering risk.
The FCPA prohibits offering, promising, providing or authorizing others to give anything of value to a foreign government official or employee to obtain or retain business or otherwise secure a business advantage. Outside of the United States, we may interact with government officials in several different capacities: as regulators of our insurance business; as clients or partners who are state-owned or partially state-owned; as health care providers who are employed by the government; as hospitals that are state-owned; and as officials issuing permits in connection with real estate transactions. Violations of the FCPA and other anti-corruption laws may result in severe criminal and civil sanctions as well as other penalties, and the SEC and DOJ have increased their enforcement activities with respect to FCPA. The UK Bribery Act of 2010 applies to all companies with a nexus to the United Kingdom. Under this act, any voluntary disclosures of FCPA violations may be shared with United Kingdom authorities, thus potentially exposing companies to liability and potential penalties in multiple jurisdictions. Other countries in which we do business also have anti-corruption laws to which we are subject.
32
Item 1A. RISK FACTORS
As a large global health services company operating in a complex industry, we encounter a variety of risks and uncertainties, which could have a material adverse effect on our business, liquidity, results of operations, financial condition or the trading price of our securities. You should carefully consider each of the risks and uncertainties discussed below, together with other information contained in this Form 10-K, including MD&A. These risks and uncertainties are not the only ones we face. Additional risks and uncertainties not presently known to us or that we currently believe to be immaterial may also adversely affect us. The following risk factors have been organized by category for ease of use; however many of the risks may have impacts in more than one category. These categories, therefore, should be viewed as a starting point for understanding the significant risks facing us and not as a limitation on the potential impact of the matters discussed. Risk factors are not necessarily listed in order of importance.
Strategic and Operational Risks
Future performance of our business will depend on our ability to execute our strategic and operational initiatives effectively.
The future performance of our business will depend in large part on our ability to effectively implement and execute our strategic and operational initiatives. Successfully executing on these initiatives depends on a number of factors, including our ability to:
•differentiate our products, services and solutions from those of our competitors;
•develop and bring to market new and innovative products, solutions or programs that focus on improving patient outcomes and experiences and assist in controlling costs or in response to government regulation;
•develop and create data and analytic solutions to support and improve outcomes for our products, services and solutions, including creating and developing solutions and services through partnerships with other industry participants;
•grow and support our product portfolio, expand our addressable markets and identify and introduce the proper mix, coordination or integration of products that will be accepted by the marketplace;
•evaluate drugs for efficacy, value and price to assist clients in selecting a cost-effective formulary;
•offer cost-effective home delivery pharmacy and specialty services;
•access or continue accessing key drugs and successfully penetrate key treatment categories in our specialty pharmacy business;
•attract and retain sufficient numbers of qualified employees, particularly in an increasingly competitive job market;
•attract, develop and maintain collaborative relationships with a sufficient number of qualified partners;
•attract new and maintain existing customer and client relationships;
•leverage purchase volume to deliver discounts to health benefit providers;
•transition health care providers from volume-based fee-for-service arrangements to a value-based system;
•improve medical cost competitiveness in our targeted markets;
•manage our medical, pharmacy, administrative and other operating costs effectively; and
•contract with health care providers, pharmacy providers and pharmaceutical manufacturers on market competitive terms.
For our strategic initiatives to succeed, we must effectively collaborate across our operations, integrate our acquired businesses, actively work to ensure consistency throughout the organization and promote a global mindset along with a focus on individual customers and clients. If we fail to do so, our business may be unable to grow as planned, or the result of expansion may be unsatisfactory. We will be unable to rapidly respond to competitive, economic and regulatory changes if we do not make important strategic and operational decisions quickly, define our appetite for risk, implement new governance, managerial and organizational processes smoothly and communicate roles and responsibilities clearly. If these initiatives fail or are not executed effectively, our consolidated financial position and results of operations could be negatively affected.
We operate in a highly competitive, evolving and rapidly changing industry and our failure to adapt could negatively impact our business.
The health service industry continues to be dynamic and rapidly evolving. Any significant shifts in the structure of the industry could alter industry dynamics and adversely affect our ability to attract or retain clients and customers. Industry shifts could result (and have resulted) from, among other things:
•a large intra- or inter-industry merger or industry consolidation;
•strategic alliances;
33
•new or alternative business models or new government options or offerings;
•continuing consolidation among physicians, hospitals and other health care providers, as well as changes in the organizational structures chosen by physicians, hospitals and health care providers;
•new market entrants, including those not traditionally in the health service industry;
•the ability of larger employers and clients to contract directly with providers;
•technological changes and rapid shifts in the use of technology, such as telehealth;
•the impact or consequences of legislation or regulatory changes;
•changes in the United States Postal Service or the consolidation of shipping carriers;
•increased drug acquisition cost or unexpected changes to drug pricing trend;
•changes in the generic drug market or the failure of new generic drugs to come to market; or
•changes in utilization of health care, prescription drugs or other covered services and items, including under risk-based contracts in the health benefit management market and for those businesses that utilize risk adjustment methodology.
Our failure to anticipate or appropriately adapt to changes in the industry could negatively impact our competitive position and adversely affect our business and results of operations.
The scale, scope and duration of the ongoing COVID-19 pandemic continues to be unknown and the overall impact on our business, operating results, cash flows or financial condition has been and may continue to be material.
The COVID-19 pandemic has adversely affected, and is continuing to affect, global economies, financial markets and the overall environment for our business, and the extent to which it may impact our future results of operations and overall financial performance remains uncertain. While vaccination rates continue to rise, the COVID-19 pandemic, including vaccination efficacy, the implementation of and reaction to vaccination and testing mandates and the occurrence of new variants (including the delta and omicron variants), could continue to effect such economies and financial markets as well as the health and availability of our workforce. As a result, we may experience new disruptions to our business operations and our business could be adversely affected further, directly or indirectly, by the ongoing pandemic. National, state and local governments in affected regions have implemented and may continue to implement varying safety precautions, including quarantines, border closures, increased border controls, travel restrictions, shelter-in-place orders and shutdowns, business closures, cancellations of public gatherings and other measures.
The COVID-19 pandemic has in some instances, and may continue to, heighten the potential adverse effects on our business, operating results, cash flows or financial condition as described below or in other risk factors within this section of the Form 10-K including, but not limited to, the likelihood of and impact from:
•unfavorable economic conditions on our clients and customers (both employers and individuals), health care and pharmacy providers, pharmaceutical manufacturers and third-party vendors, as well as federal and state entities and programs;
•changes in medical claims submission and processing patterns or procedures; changes in customer base and product mix; changes in utilization of prescription drugs, medical or other covered items or services, including increased behavioral health services utilization; changes in medical cost trends; changes in our health management practices; and the introduction of new benefits and products causing actual claims to exceed our estimates;
•changes in health care utilization patterns, provider billing practices and other external events that we cannot forecast or project and over which we have little or no control impacting our ability to accurately predict, price for and manage health care costs and ultimately our profitability, including impacts from care deferral on, among other things, risk adjustment revenue and acuity of future care;
•increased costs or reductions in revenue, including costs for COVID-19-related care, testing and treatment; vaccine and other coverage mandates; inflation; and support for employees, clients, customers and providers;
•significant disruptions in service within our operations or among our key suppliers or other third parties, including delivery delays and other supply chain impacts and decreased worker productivity, increased worker attrition and operational and sales disruptions, including as a result of remote working arrangements, increased medical, emergency or other leave, quarantines, government actions or restrictions, including as it relates to vaccination mandates;
•compliance with substantial government regulation, including privacy and security requirements associated with providing telehealth and remote care options and new laws or regulations or changes in existing laws or regulations, such as vaccine, testing and coverage mandates and premium deferrals, which laws or regulations may vary significantly by jurisdiction;
34
•prioritization of matters relating to COVID-19 resulting in delays in responsiveness by regulatory agencies and other third parties in matters arising in the ordinary course of business;
•cyberattacks or other privacy or data security incidents, including as a result of the transition to a remote work environment by substantially all of our workforce and the workforces of third parties with whom we contract;
•significant shifts in the structure of the industry which could alter dynamics and, if we fail to adapt, negatively impact our business;
•risks inherent in foreign operations, including political, legal, operational, regulatory, economic and other risks;
•economic and market conditions affecting the value of our financial instruments and the value of particular assets and liabilities; and
•fluctuations in equity market prices, interest rates and credit spreads limiting our ability to raise or deploy capital and affecting our overall liquidity.
Additionally, if we do not respond appropriately to the pandemic, or if our clients or customers do not perceive our response to be adequate, we could suffer damage to our reputation, which could adversely affect our business.
We believe COVID-19 and its variants' adverse impact on our business, operating results, cash flows or financial condition will be driven primarily by the severity and duration of the pandemic, including the impact of the breadth and timing of implementation and the efficacy and costs of vaccination programs, the pandemic's continued impact on our employees, clients, customers, suppliers and partners, as well as the U.S. and global economies and the continued actions taken by governmental authorities and other third parties in response to the pandemic. Those primary drivers are largely beyond our knowledge and control, and may be more adverse than our current expectations. Given these uncertainties, we cannot estimate the full impact COVID-19 will have on our business, operating results, cash flows or financial condition, but the adverse impact could be material.
Our failure to compete effectively, to differentiate our products and services from those of our competitors and maintain or increase market share could materially adversely affect our results of operations, financial position and cash flows.
We operate in a highly competitive environment and an industry subject to significant market pressures brought about by customer and client needs, legislative and regulatory developments and other market factors. In particular markets, our competitors may have greater, better or more established capabilities, resources, market share, reputation or business relationships, or lower profit margin or financial return expectations. Our clients are well informed and organized and can easily move between our competitors and us. Our Express Scripts client contracts generally have three-year terms and may be subject to periodic renegotiation of pricing terms based on market factors. As described in greater detail in the description of our business in Item 1 of this Form 10-K, one of our key clients in the Evernorth segment is the Department of Defense. If one or more of our large clients terminates or does not renew a contract for any reason, including as a result of being acquired, or if the provisions of a contract with a large client are modified, renewed or otherwise changed with terms less favorable to us, our results of operations could be adversely affected and we could experience a negative reaction in the investment community resulting in decreases in the trading price of our securities or other adverse effects.
Our success depends, in part, on our ability to compete effectively in our markets, set prices appropriately in highly competitive markets to keep or increase our market share, increase customers as planned, differentiate our business offerings by innovating and delivering products and services that provide enhanced value to our customers, provide quality and satisfactory levels of service and retain accounts with favorable medical cost experience or more profitable products versus retaining or increasing our customer base in accounts with unfavorable medical cost experience or less profitable products.
We must remain competitive to attract new customers, retain existing customers and further integrate additional product and service offerings. To succeed in this highly competitive marketplace, it is imperative that we maintain a strong reputation. Increasingly, our customers, clients and investors consider our efforts on a variety of matters that could impact our stakeholders, including our employees and the communities in which we operate, such as our efforts with respect to the environment and diversity, equity and inclusion. The negative reputational impact of a significant event, including a failure to execute on customer or client contracts or strategic or operational initiatives, failure to comply with applicable laws or regulations, or failure to innovate and deliver products and services that demonstrate greater value to our customers, could affect our ability to grow and retain profitable arrangements, which could have a material adverse effect on our business, results of operations, financial position and cash flows.
35
We face price competition and other pressures that could compress our margins or result in premiums that are insufficient to cover the cost of services delivered to our customers.
While we compete on the basis of many service and quality-related factors, we expect that price will continue to be a significant basis of competition. Our client contracts are subject to negotiation as clients seek to contain their costs, including by reducing benefits offered. Increasingly, our clients seek to negotiate performance guarantees that require us to pay penalties if the guaranteed performance standard is not met. Clients can easily move between our competitors and us. Our clients are well informed and typically have knowledgeable consultants that seek competing bids from our competitors before contract renewal. In addition, as brokers and benefit consultants seek to enhance their revenue streams, they look to take on services that we typically provide. Each of these events could negatively impact our financial results.
Federal and state regulatory agencies may restrict or prevent entirely our ability to implement changes in premium rates. Fiscal or other concerns related to the government-sponsored programs in which we participate, such as Medicare Advantage plans and Medicare Part D plans, may cause decreasing reimbursement rates, delays in premium payments, restrictions on implementing changes in premium rates or insufficient increases in reimbursement rates. Any limitation on our ability to maintain or increase our premium or reimbursement levels, or a significant loss of customers or clients resulting from our need to increase or maintain premium or reimbursement levels, could adversely affect our business, cash flows, financial condition and results of operations.
Premiums in the Cigna Healthcare segment are generally set for one-year periods and are priced well in advance of the date on which the contract commences or renews. Our revenue on Medicare Advantage plans, Individual and Family Plans ("IFP") and Medicare Part D plans is based on rates and bids submitted midyear in the year before the contract year. Although we base the premiums we charge and our Medicare Advantage, IFP and Medicare Part D rates and bids on our estimate of future health care costs over the contract period, actual costs may exceed what we estimate in setting premiums. Our health care costs also are affected by external events that we cannot forecast or project and over which we have little or no control, including changes in regulations, as well as provider billing practices and changes in customers' health care utilization patterns, which may, among other things, impact our ability to appropriately document their health conditions. Our participation in health insurance exchanges through our IFP offerings involves uncertainties associated with mix and volume of business and could adversely affect our results of operations, financial position and cash flows. Our profitability depends, in part, on our ability to accurately predict, price for and effectively manage future health care costs. Relatively small differences between predicted and actual medical costs or utilization rates as a percentage of revenue can result in significant changes in our financial results.
Strong competition within the pharmacy benefit business has also generated greater demand for lower product and service pricing, increased revenue sharing and enhanced product and service offerings. These competitive factors have historically applied pressure on our operating margins and caused many companies, including us, to reduce the prices charged for products and services while sharing with clients a greater portion of the formulary fees and related rebates received from pharmaceutical manufacturers. Our inability to maintain positive trends, or failure to identify and implement new ways to mitigate pricing pressures, could negatively impact our ability to attract or retain clients or sell additional services, which could negatively impact our margins and have a material adverse effect on our business and results of operations.
The reserves we hold for expected medical claims are based on estimates that involve an extensive degree of judgment and are inherently variable. If actual claims exceed our estimates, our operating results could be materially adversely affected, and our ability to take timely corrective actions to contain future costs may be limited.
We maintain and record medical claims reserves on our balance sheet for estimated future payments. Our estimates of health care costs payable are based on a number of factors, including historical claim experience, but this estimation process requires extensive judgment. Considerable variability is inherent in such estimates, and the accuracy of the estimates is highly sensitive to changes in medical claims submission and processing patterns or procedures, changes in customer base and product mix, changes in the utilization of prescription drugs, medical or other covered items or services, changes in medical cost trends, changes in our health management practices, changes in regulations and the introduction of new benefits and products. If we are not able to accurately and promptly anticipate and detect medical cost trends, our ability to take timely corrective actions to limit future costs and reflect our current benefit cost experience in our pricing process may be limited. Additionally, we must estimate the amount of rebates payable by us under the ACA's and CMS' minimum loss ratio rules and the amounts payable by us to, and receivable by us from, the United States federal government under the ACA's remaining premium stabilization program. Because establishing reserves is an inherently uncertain process involving estimates of future losses, there can be no certainty that ultimate losses will not exceed existing reserves which may adversely affect our results of operations, financial position and cash flows.
36
If we fail to develop and maintain satisfactory relationships with physicians, hospitals and other health service providers and with producers and consultants, our business and results of operations may be adversely affected.
We contract with or employ physicians, hospitals and other health service providers and facilities to provide health services to our customers. Our results of operations are substantially dependent on our ability to contract for these services at competitive prices. In any particular market, physicians, hospitals and health service providers may enter into exclusive arrangements with competitors or simply refuse to contract with us, demand higher payments or take other actions that could result in higher medical costs or less desirable products or services for our customers. In some markets, certain providers, particularly hospitals, physician/hospital organizations and multispecialty physician groups, may have significant or controlling market positions that could result in a diminished bargaining position for us. If providers refuse to contract with us, use their market position to negotiate more favorable contracts or place us at a competitive disadvantage, our ability to market products or to be profitable in those areas could be materially adversely affected. Additionally, certain regulations may impact our ability to obtain competitive prices. Establishing collaborative arrangements with physician groups, specialist groups, independent practice associations, hospitals and health care delivery systems is key to our strategic focus to transition from volume-based fee-for-service arrangements to a value-based health care system. If such collaborative arrangements do not result in the lower medical costs that we project or if we fail to attract health care providers to such arrangements, or are less successful at implementing such arrangements than our competitors, our attractiveness to customers may be reduced and our ability to profitably grow our business may be adversely affected.
Our ability to develop and maintain satisfactory relationships with providers may also be negatively impacted by other factors not associated with us, such as changes in Medicare or Medicaid reimbursement levels, increasing pressure on revenue and other pressures on health care providers and increasing consolidation activity among hospitals, physician groups and providers. Continuing consolidation among physicians, hospitals and other providers, the emergence of accountable care organizations, vertical integration of providers and other entities, changes in the organizational structures chosen by physicians, hospitals and providers, new market entrants, including those not traditionally in the health care industry, and the increased use of virtual care services (including telehealth) may affect the way providers interact with us and may change the competitive landscape in which we operate. In some instances, these organizations may compete directly with us, potentially affecting the way we price our products and services or causing us to incur increased costs if we change our operations to be more competitive.
Out-of-network providers are not limited by any agreement with us in the amounts they bill. While benefit plans place limits on the amount of charges that will be considered for reimbursement and regulations seek to prescribe payment levels, establish methodologies and dispute resolution processes, providers are increasingly sophisticated and aggressive. As a result, the outcome of disputes where we do not have a provider contract may cause us to pay higher medical or other benefit costs than we projected.
Additionally, certain of our products and services are sold in part through nonexclusive producers and consultants for whose services and allegiance we compete. Our sales could be materially adversely affected if we are unable to attract, retain and support such independent producers and consultants or if our sales strategy is not appropriately aligned across distribution channels.
If we lose our relationship with one or more key pharmaceutical manufacturers, or if the payments made or discounts provided by pharmaceutical manufacturers decline, our business and results of operations could be adversely affected.
We maintain relationships with numerous pharmaceutical manufacturers, which provide us with, among other things:
•discounts for drugs we purchase to be dispensed from our home delivery and specialty pharmacies;
•discounts, in the form of rebates, for drug utilization;
•fees for administering rebate programs, including invoicing, allocating and collecting rebates;
•fees for services provided to pharmaceutical manufacturers by our specialty pharmacies; and
•access to limited distribution specialty pharmaceuticals by our specialty pharmacies.
Our contracts with pharmaceutical manufacturers are typically nonexclusive and terminable on relatively short notice by either party. The consolidation of pharmaceutical manufacturers, the termination or material alteration of our relationships, or our failure to renew contracts on market competitive terms could have a material adverse effect on our business and results of operations. In addition, arrangements between payors and pharmaceutical manufacturers have been the subject of debate in federal and state legislatures and various other public and governmental forums. Adoption of new laws, rules or regulations or changes in, or new interpretations of, existing laws, rules or regulations, relating to any of these programs could materially adversely affect our business and results of operations.
37
If significant changes occur within the pharmacy provider marketplace, or if other issues arise with respect to our pharmacy networks, including the loss of or adverse change in our relationship with one or more key pharmacy providers, our business and financial results could be adversely affected.
More than 67,900 pharmacies participated in one or more of our networks as of December 31, 2021. The ten largest retail pharmacy chains represent approximately 62% of the total number of stores in our largest network. In certain geographic areas of the United States, our networks may be comprised of higher concentrations of one or more large pharmacy chains. Contracts with retail pharmacies are generally nonexclusive and are terminable on relatively short notice by either party. If one or more of the larger pharmacy chains terminates its relationship with us, or is able to renegotiate terms substantially less favorable to us, our customers' access to retail pharmacies or our business could be materially adversely affected. The entry of one or more additional large pharmacy chains into the pharmacy benefit management business, the consolidation of existing pharmacy chains or increased leverage or market share by the largest pharmacy providers could increase the likelihood of negative changes in our relationship with such pharmacies. Changes in the overall composition of our pharmacy networks, or reduced pharmacy access under our networks, could have a negative impact on our claims volume or our competitiveness in the marketplace, which could cause us to fall short of certain guarantees in our contracts with clients or otherwise impair our business or results of operations.
Changes in drug pricing or industry pricing benchmarks could materially impact our financial performance.
Contracts in the prescription drug industry, including our contracts with retail pharmacy networks and our pharmacy and specialty pharmacy clients, generally use pricing metrics published by third parties as benchmarks to establish pricing for prescription drugs. If these benchmarks are no longer published by third parties, we, or our contractual partners, adopt other pricing benchmarks for establishing prices within the industry, legislation or regulation requires the use of other pricing benchmarks, or future changes in drug prices substantially deviate from our expectations, the short- or long-term impacts may have a material adverse effect on our business and results of operations.
As a global company, we face political, legal, operational, regulatory, economic and other risks that present challenges and could negatively affect our multinational operations or our long-term growth.
As a global company, our business is increasingly exposed to risks inherent in foreign operations. These risks can vary substantially by market, and include political, legal, operational, regulatory, economic and other risks, including government intervention that we do not face in our U.S. operations. The global nature of our business and operations may present challenges including, but not limited to, those arising from:
•geopolitical business conditions and demands;
•regulation that may discriminate against U.S. companies, favor nationalization or expropriate assets;
•price controls or other pricing issues and exchange controls; restrictions that prevent us from transferring funds out of the countries in which we operate; foreign currency exchange rates and fluctuations and restrictions on converting currencies from foreign operations into other currencies; uncertainty with respect to the interpretation of tax positions;
•reliance on local employees and interpretations of labor laws in foreign jurisdictions;
•managing our partner relationships in countries outside of the United States;
•providing data protection on a global basis and sufficient levels of technical support in different locations;
•the global trend for companies to enact local data residency requirements;
•acts of civil unrest, war and terrorism, as well as other political and economic conflicts such as through imposition of economic or political sanctions;
•man-made disasters, natural disasters (including those arising as a result of climate change) and pandemics, such as the COVID-19 pandemic, in locations where we operate; and
•general economic and political conditions.
These factors may increase in significance as we continue to expand globally and operating in new foreign markets may require considerable management time before operations generate any significant revenues and earnings. Any one of these challenges could negatively affect our operations or long-term growth. For example, if we're unable to divest our South Korean business, we will continue to be exposed to potential losses resulting from economic and regulatory changes in that country and the geopolitical climate in the Korean Peninsula, as well as foreign currency movements affecting the South Korean currency, that, due to the current concentration of our international business, could have a significant impact on our consolidated financial results.
International operations also require us to devote significant resources to implement controls and systems in new markets to comply
38
with, and to ensure that our vendors and partners comply with, U.S. and foreign laws prohibiting bribery, corruption and money laundering, in addition to other regulations regarding, among other things, our products, direct-to-consumer communications, customer privacy, data protection and data residency. Violations of these laws and regulations could result in fines, criminal sanctions against us, our officers or employees, restrictions or outright prohibitions on the conduct of our business and significant reputational harm. Our success depends, in part, on our ability to anticipate these risks and manage these challenges. Our failure to comply with laws and regulations governing our conduct outside the United States or to establish constructive relations with non-U.S. regulators could have a material adverse effect on our business, results of operations, financial condition, liquidity and long-term growth.
Strategic transactions involve risks and we may not realize the expected benefits because of integration difficulties, underperformance relative to our expectations and other challenges.
As part of our strategy, we regularly consider and enter into strategic transactions, including mergers, acquisitions, joint ventures, licensing arrangements, divestitures and other relationships (collectively referred to as "strategic transactions"). There is significant competition for attractive targets and opportunities and we may be unable to identify and successfully complete strategic transactions in the future. In addition, from time to time, we evaluate alternatives for our businesses that do not meet our strategic, growth or profitability objectives, and we may divest or wind down such businesses. We may be unable to complete any such divestiture on terms favorable to us, within the expected timeframes, or at all. We may have continued financial exposure to divested businesses following the completion of any such transaction, including increased costs due to potential litigation, contingent liabilities and indemnification of the buyer related to, among other things, lawsuits, regulatory matters or tax liabilities.
Our ability to achieve the anticipated benefits of strategic transactions, including synergies, cost savings, innovation and operational efficiencies, is subject to numerous uncertainties and risks, including our ability to successfully combine or separate business operations, resources and systems, including data security systems and internal financial control standards, in an efficient and effective manner. Integration and separation activities may result in additional and unforeseen expenses, and the anticipated benefits may not be fully realized or may take longer to realize than expected. These activities are complex, costly and time-consuming and may divert management's attention from ongoing business concerns. Delays or issues encountered in these activities could have a material adverse effect on the revenues, expenses, operating results and financial condition of the Company. Additionally, the benefits of strategic transactions and the related timing could be impacted by various factors, including political instability, natural disasters, fluctuations in currency exchange rates, delays in obtaining regulatory approval and changes in regulations.
Strategic transactions could result in increased costs, including facilities and systems consolidation or separation costs and costs to retain key employees, decreases in expected revenues, earnings or cash flows and goodwill or other intangible asset impairment charges. As of December 31, 2021, our goodwill and other intangible assets had a carrying value of approximately $80 billion, representing 52% of our total consolidated assets. The value of our goodwill may be materially and adversely impacted if the businesses we acquire do not perform in a manner consistent with our assumptions. Future evaluations requiring an impairment to goodwill and other intangible assets could materially affect our results of operations and shareholders' equity in the period in which the impairment occurs. A material decrease in shareholders' equity could negatively impact our debt ratings or potentially impact our compliance with existing debt covenants. See Note 18 to the Consolidated Financial Statements for more information on goodwill and intangibles. In addition, the trading price of our securities may decline if, among other things, we are unable to achieve our estimates of earnings growth and operational cost savings, or the transaction costs are greater than expected. The trading price also may decline if we do not achieve the perceived benefits of a transaction as rapidly or to the extent anticipated by financial or industry analysts.
Additionally, joint ventures and equity investments present risks that are different from acquisitions, including risks related to: specific operations and finances of the businesses we invest in; selection of appropriate parties; differing objectives of the various parties; competition between and among parties; compliance activities (including compliance with applicable CMS requirements); growing the business in a manner acceptable to all the parties; maintaining positive relationships among the parties, clients and customers; initial and ongoing governance of joint ventures and customer and business disruption that may occur upon a joint venture termination.
Further, we may finance strategic transactions by issuing common stock for some or all of the purchase price that could dilute the ownership interests of our shareholders, or by incurring additional debt that could increase costs and impact our ability to access capital in the future.
In addition, effective internal controls are necessary to provide reliable and accurate financial reports and to mitigate the risk of fraud. The integration of businesses is likely to cause increasing complexity in our systems and internal controls and make them more difficult to manage. Any difficulties in assimilating businesses into our control system could cause us to fail to meet our financial reporting obligations. We also rely on the internal controls and financial reporting controls of joint venture entities and other entities in which we invest and their failure to maintain effectiveness or comply with applicable standards may materially and adversely affect us. Ineffective internal controls could also cause investors to lose confidence in our reported financial information that could
39
negatively impact the trading price of our securities and our access to capital.
We are dependent on the success of our relationships with third parties for various services and functions.
To improve operating costs, productivity and efficiencies, we contract with third parties for the provision of specific services. Our operations may be adversely affected if a third party fails to satisfy its obligations, if the arrangement is terminated in whole or in part or if there is a contractual dispute between us and the third party. Even though contracts are intended to provide certain protections, we have limited control over the actions of third parties. For example, noncompliance with any privacy or security laws and regulations, any security breach involving one of our third-party vendors or a dispute between us and a third-party vendor related to our arrangement could have a material adverse effect on our business, results of operations, financial condition, liquidity and reputation.
Outsourcing also may require us to change our existing operations, adopt new processes for managing these service providers or redistribute responsibilities to realize the potential productivity and operational efficiencies. If there are delays or difficulties in changing business processes or our third-party vendors do not perform as expected, we may not realize, or not realize on a timely basis, the anticipated economic and other benefits of these relationships. This could result in additional costs or regulatory compliance issues or create other operational or financial problems for us. Terminating or transitioning, in whole or in part, arrangements with key vendors could result in additional costs or penalties, risks of operational delays or potential errors and control issues during the termination or transition phase. We may not be able to find an alternative vendor in a timely manner or on acceptable terms. If there is an interruption in business or loss of access to data resulting from a security breach, termination or transition in services, we may not be able to meet the demands of our customers and, in turn, our business and results of operations could be adversely impacted.
A significant disruption in service within our operations or among our key suppliers or other third parties could materially adversely affect our business and results of operations.
Our business is highly dependent upon our ability to perform, in an efficient and uninterrupted fashion, necessary business functions, such as claims processing and payment, internet support and customer call centers, data centers and corporate facilities, processing new and renewal business, maintaining appropriate shipment and storage conditions for prescriptions (such as temperature and protection from contamination) and home delivery processing. In some instances, our ability to provide services or products (including processing and dispensing prescriptions) depends on the availability of services and products provided by suppliers, providers, pharmaceutical manufacturers, vendors or shipping carriers. A disruption, or threat of disruption, in our supply chain, including as a result of the COVID-19 pandemic, or inability to access or deliver products that meet requisite quality safety standards in a timely and efficient manner could adversely impact our business.
Increasing natural disasters in connection with climate change could also be a direct threat to us and our third-party vendors, service providers or other stakeholders. Natural disasters, such as wildfires, hurricanes and snow and ice storms, have impacted and may continue to impact our customers and pose a risk to our employees and facilities located in the impacted region. Responses to such scenarios have and may include, among other things, making temporary policy changes, such as waiving various medical requirements, assisting with replacement medications, transferring prescriptions and expanding our help line. In addition, there is a risk that actions taken to respond to climate change could increase the cost of energy, fuel and other commodities, which would increase our operating costs.
We are also subject to risk as a result of information technology disruptions. Any failure or disruption of our performance of, or our ability to perform, key business functions, including through unavailability or cyberattack of our information technology systems or those of third parties (including cloud service providers), could cause slower response times, decreased levels of service satisfaction and harm to our reputation. Our systems interface with and depend on third-party systems and we could experience service denials if demand for such service exceeds capacity or a third-party system fails or experiences an interruption.
While we have adopted, and continue to enhance, business continuity and disaster recovery plans and strategies, there is no guarantee that such plans and strategies will be effective, which could interrupt the functionality of our information technology systems or those of third parties. Our failure to implement adequate business continuity and disaster recovery strategies could significantly reduce our ability to provide products and services to our customers and clients, which could have material adverse effects on our business and results of operations.
Our business depends on our ability to effectively invest in, implement improvements to and properly maintain the uninterrupted operation, availability and data integrity of our information technology and other business systems.
Our business is highly dependent on maintaining effective information systems as well as the integrity and timeliness of the data we use to serve our customers and health care providers and to operate our business. If our data were found to be inaccurate or unreliable
40
due to fraud or other error, or if we, or any of the third-party providers we engage, were to fail to maintain information systems and data integrity effectively, we could experience operational disruptions that may impact our clients, customers and health care providers and hinder our ability to provide or establish appropriate pricing for products and services, retain and attract clients and customers, establish reserves and report financial results timely and accurately and maintain regulatory compliance, among other things.
Our information technology strategy and execution are critical to our continued success. We must continue to invest in and maintain long-term solutions that will enable us to anticipate customer needs and expectations, enhance the customer experience, act as a differentiator in the market and protect against cybersecurity risks and threats or other events that could disrupt our information technology systems such as man-made or natural disasters (including those as a result of climate change). Our success is dependent, in large part, on maintaining the effectiveness of existing technology systems and continuing to deliver and enhance technology systems that support our business processes in a cost-efficient and resource-efficient manner. Increasing regulatory and legislative changes will place additional demands on our infrastructure that could have a direct impact on resources available for other projects tied to our strategic initiatives. In addition, recent trends toward greater consumer engagement in health care require new and enhanced technologies, including more sophisticated applications for mobile devices. Connectivity among technologies is becoming increasingly important. We must also develop new systems to meet current market standards and keep pace with continuing changes in information processing technology, evolving industry and regulatory standards and customer needs. Failure to do so may present compliance challenges and impede our ability to deliver services in a competitive manner. Further, because system development projects are long-term in nature, they may be more costly than expected to complete and may not deliver the expected benefits upon completion. Our failure to effectively invest in, implement improvements to and properly maintain the uninterrupted operation, availability and data integrity of our systems could adversely affect our results of operations, financial position and cash flow.
As a large health services company, we and our vendors are subject to cyberattacks or other privacy or data security incidents. If we are unable to prevent or contain the effects of any such attacks, or fail to ensure vendors do the same, we may suffer exposure to substantial liability, reputational harm, loss of revenue or other damages.
Our business depends on our clients' and customers' willingness to entrust us with their health-related and other sensitive personal information, including information that is subject to privacy, security or data notification laws. Computer systems may be vulnerable to physical break-ins, computer viruses or malware, programming errors, attacks by third parties or similar disruptive problems. We have been, and will likely continue to be, the target of computer viruses or other malicious codes, unauthorized access, cyberattacks or other computer-related penetrations. There have been, and will likely continue to be, large scale cyberattacks within the health service industry. Additionally, hardware, software or applications we develop or procure from third parties may contain defects in design, manufacturer defects or other problems that could unexpectedly compromise information technology. Human or technological error has and could in the future result in, for example, unauthorized access to, disclosure, modification, misuse, loss, or destruction of company, customer, or other third-party data or systems; theft of sensitive, regulated, or confidential data including personal information and intellectual property; the loss of access to critical data or systems through ransomware, destructive attacks or other means; and business delays, service or system disruptions or denials of service.
As we increase the amount of personal information that we store and share digitally, our exposure to unintended disclosures, data security and related cybersecurity risks increases, including the risk of undetected attacks, damage, loss or unauthorized access or misappropriation of proprietary or personal information, and the cost of attempting to protect against these risks also increases. The healthcare data ecosystem is complex and requires data exchange with vendors, business partners, the government and others. If disruptions, disclosures or breaches are not detected quickly, their effect could be compounded. We have dedicated significant resources to implement security technologies, processes and procedures to protect consumer identity and provide employee awareness training around phishing, malware and other cyber risks; however, there are no assurances that such measures will be effective against all types of breaches. Further, we depend on many vendors to support and assist our business, which requires such vendors to generate, store and use sensitive personal information.
Cybersecurity threats are rapidly evolving and those threats and the means for obtaining access to our proprietary systems are becoming increasingly sophisticated. Cyberattacks can originate from a wide variety of sources including terrorists, nation states, internal actors, or third parties, such as external service providers, and the techniques used change frequently or are often not recognized until after they have been launched. For example, there has been an increase in new financial fraud schemes akin to ransomware attacks on large companies whereby a cybercriminal installs a type of malicious software, or malware, that prevents a user or enterprise from accessing computer files, systems or networks and demands payment of a ransom for their return. Those parties may also attempt to fraudulently induce employees, customers or other users of our systems to disclose sensitive information in order to gain access to our data or that of our customers. In addition, while we have certain standards for all vendors that provide us services, our vendors, and in turn, their own service providers, may become subject to the same types of security breaches. Finally, our offices may be vulnerable to security incidents or security attacks, acts of vandalism or theft, misplaced or lost data, human error or similar events that could negatively affect our systems and our customers' and clients' data.
41
The costs to eliminate or address security threats and vulnerabilities before or after a cyber-incident could be significant. Our remediation efforts may not be successful and could result in interruptions, delays, or cessation of service and loss of existing or potential customers.
In addition, the unauthorized dissemination of sensitive personal information, proprietary information or confidential information about us, our customers or other third parties could expose our customers' and their private information to the risk of financial or medical identity theft. Unauthorized dissemination of confidential and proprietary information about our business and strategy could also negatively affect the achievement of our strategic initiatives. Such events could cause us to breach our contractual obligations and violate applicable laws. These events would negatively affect our ability to compete, others' trust in us, our reputation, customer base and revenues and expose us to mandatory disclosure requirements, government investigations, litigation and other enforcement proceedings, material fines, penalties or remediation costs and compensatory, special, punitive and statutory damages, consent orders and other adverse actions, any of which could adversely affect our business, results of operations, financial condition or liquidity.
In managing medical practices and operating pharmacies, onsite clinics and other types of medical facilities, we may be subject to additional liability that could result in significant time and expense.
In addition to contracting with physicians and other health care providers for services, we employ physicians, pharmacists, nurses and other health care providers at our home delivery and specialty pharmacies, onsite low acuity and primary care practices and infusion clinics that we manage and operate for our customers, as well as certain clinics for our employees. We also provide in-home care through health care providers that we employ, as well as, through third-party contractors. As such, we may be subject to liability for certain acts, omissions, or injuries caused by our employees or agents, or occurring at one of these practices, pharmacies or clinics. The defense of any actions may require the diversion of personnel and other resources and the incurrence of significant costs that could have a material adverse effect on our business, results of operations, financial condition, liquidity and reputation.
Legal and Compliance Risks
Our business is subject to substantial government regulation, as well as new laws or regulations or changes in existing laws or regulations that could have a material adverse effect on our business, results of operations, financial condition and liquidity.
Our business is regulated at the federal, state, local and international levels. The laws and rules governing our business and related interpretations are increasing in number and complexity, are subject to frequent change and can be inconsistent or in conflict with each other. Noncompliance with applicable regulations by us or our third-party vendors could have material adverse effects on our business, results of operations, financial condition, liquidity and reputation.
We must identify, assess and respond to new trends in the legislative and regulatory environment, as well as comply with the various existing regulations applicable to our business. There are currently pending, and in the future there will likely be, legislative or regulatory proposals which seek to manage the health services industry, including managing prescription drug costs and health records, as well as regulating drug distribution. We expect federal and state governments to continue to enact and seriously consider many broad-based legislative and regulatory proposals that will or could materially impact various aspects of the health care and related benefits system. In addition, changes to government policies not specifically targeted to the health services industry, such as a change in tax laws and the corporate tax rate or government spending cuts, could have significant impacts on our business, results of operations, financial condition and liquidity. The trading price of our securities may react to the announcement of such proposals. As disclosed in Part II, Item 5 of this Form 10-K, we have an active share repurchase program authorized by our board of directors. In 2021, proposed legislation was introduced in the United States Senate, which would if passed assess an excise tax on the amount spent by a publicly traded company on buying back its own stock. We are unable to predict whether any such proposals will be enacted, or the specific terms thereof, including their effect on our operations; however, certain of these proposals could, if enacted, adversely impact our business and results of operations.
Existing or future laws, rules, regulatory interpretations or judgments could force us to change how we conduct our business, affect the products and services we offer and where we offer them, restrict revenue and enrollment growth, increase our costs, including medical, operating, health care technology and administrative costs, and require enhancements to our compliance infrastructure and internal controls environment. For example, invalidation, modification, repeal or replacement of the ACA or portions thereof could result in material changes to the way we conduct our business, as well as the loss of subsidies related to our IFP offerings. We are required to obtain and maintain insurance and other regulatory approvals to, among other things, market many of our products, expand into additional geographic or product markets, increase prices for certain regulated products and consummate some of our acquisitions and dispositions. Delays in obtaining or failure to obtain or maintain these approvals could reduce our revenue or increase our costs. Existing or future laws and rules could also require or lead us to take other actions such as changing our business practices, and could increase our liability. Further, failure to effectively implement or adjust our strategic and operational initiatives, such as by reducing
42
operating costs, adjusting premium pricing or benefit design or transforming our business model in response to regulatory changes may have a material adverse effect on our results of operations, financial condition and cash flows.
For more information on regulations affecting our business, see "Business – Regulation" in Part I, Item 1 of this Form 10-K.
There are various risks associated with participating in government-sponsored programs, such as Medicare, including dependence upon government funding, compliance with government contracts and increased regulatory oversight and enforcement.
Through our U.S. Government business, we contract with CMS and various state governmental agencies to provide managed health care services including Medicare Advantage plans and Medicare Part D plans. Additionally, our Evernorth business provides services to government entities and payers participating in government health care programs.
Our revenues from government funded programs, including our Medicare programs and our government clients, are dependent, in whole or in part, upon annual funding from the federal government or applicable state or local governments. Funding for these programs is dependent on many factors outside our control, including general economic conditions, continuing government efforts to contain health care costs and budgetary constraints at the federal or applicable state or local level and general political issues and priorities. These entities generally have the right to not renew or cancel their contracts with us on short notice without cause or if funds are not available. Unanticipated changes in funding, such as the application of sequestration by the federal or state governments or the failure to provide for continued appropriations or regular ongoing scheduled payments to us, could substantially reduce our revenues and profitability.
The Medicare program has been the subject of regulatory reform initiatives. The premium rates paid to Medicare Advantage plans and Medicare Part D plans are established by contract, although the rates differ depending on a combination of factors, some of which are outside our control. For example, the base premium rate paid differs depending upon a combination of various factors such as defined upper payment limits, a member's health status, age, gender, county or region, benefit mix, member eligibility category and risk scores. Additionally, a portion of each Medicare Advantage plan's reimbursement is tied to the plan's Star Rating, with those plans receiving a rating of four or more stars eligible for quality-based bonus payments. A plan's Star Rating affects its image in the market and plans that perform well are able to offer enhanced benefits, market more effectively and for longer periods of time than other plans. The Star Rating system is subject to change annually by CMS, which may make it more difficult to achieve four stars or greater. Our Medicare Advantage plans' and Medicare Part D plans' operating results, premium revenue and benefit offerings are likely to continue to be significantly determined by their Star Ratings. There can be no assurances that we will be successful in maintaining or improving our Star Ratings in future years. In addition, audits of our performance for past or future periods may result in downgrades to our Star Ratings. Accordingly, our plans may not be eligible for full level quality bonuses, which could adversely affect the benefits such plans can offer, reduce membership or impact our financial performance. See the "Executive Overview - Key Transactions and Business Developments" section of MD&A in Part II, Item 7 of this Form 10-K for additional information on our Star Ratings.
Additionally, if we fail to comply with CMS' contractual requirements, including data submission, enrollment and marketing, provider network adequacy, provider directory accuracy, quality measures, claims payment, continuity of care, timely and accurate processing of appeals and grievances, oversight of first tier downstream and related entities and call center performance, we may be subject to administrative actions, including enrollment sanctions or contract termination, fines or other penalties that could impact our profitability. As described under "Business – Regulation" in Part I, Item 1 of this Form 10-K, on November 1, 2018, CMS released a proposed rule that would revise its RADV methodology and, if adopted in its current form, could result in some combination of degraded plan benefits, higher monthly premiums or reduced choice for the population served by all Medicare Advantage insurers. While it is uncertain whether CMS will finalize the rule as proposed, if adopted, it could have a material impact on the Company's future results of operations.
Any failure, or alleged failure, to comply with various state and federal health care laws and regulations, including those directed at preventing fraud and abuse in government funded programs, has resulted in and could in the future result in investigations or litigation, such as actions under the federal False Claims Act and similar whistleblower statutes under state laws. A successful action or claim against us could subject us to damage awards, including treble damages, fines, penalties or other enforcement actions, restrictions on our ability to market or enroll new customers, limits on expansion, restrictions or exclusions from programs or other agreements with federal or state governmental agencies, which could adversely impact our business, cash flows, financial condition, results of operations and reputation.
We face risks related to litigation, regulatory audits and investigations.
We are routinely involved in numerous claims, lawsuits, regulatory audits, investigations and other legal matters arising, for the most part, in the ordinary course of business. These legal matters could include benefit claims, breach of contract actions, tort claims, claims
43
arising from consumer protection laws, false claims act laws, claims disputes under federal or state laws and disputes regarding reinsurance arrangements, employment and employment discrimination-related suits, antitrust claims, employee benefit claims, wage and hour claims, tax, privacy, intellectual property and whistleblower claims, shareholder suits and other securities law claims, real estate disputes, claims related to disclosure of certain business practices and claims arising from customer audits and contract performance, including government contracts. In addition, we have incurred and likely will continue to incur liability for practices and claims related to our health care business, such as marketing misconduct, failure to timely or appropriately pay for or provide health care, provider network structure, poor outcomes for care delivered or arranged, provider disputes including disputes over compensation or contractual provisions, ERISA claims, allegations related to calculations of cost sharing and claims related to our administration of self-funded business. We are also routinely involved in legal matters arising from our health services business, including without limitation claims related to the dispensing of pharmaceutical products by our home delivery and specialty pharmacies, pharmacy benefit management services, such as formulary management services, health benefit management services and provider services. There are currently, and may be in the future, attempts to bring class action lawsuits against the Company and other companies in our industry; individual plaintiffs also may bring multiple claims regarding the same subject matter against us and other companies in our industry.
Court decisions and legislative activity may increase our exposure for any of these types of claims. In some cases, substantial noneconomic or punitive damages may be sought. We procure insurance coverage to cover some of these potential liabilities, however we also self-insure a significant portion of our litigation risks. While we maintain some third-party insurance coverage, including excess liability insurance with third-party insurance carriers, certain liabilities or types of damages, such as punitive damages, may not be covered by insurance, insurers may dispute coverage or the amount of insurance may be insufficient to cover the entire damages awarded. Resolving disputes is often expensive and disruptive, regardless of the outcome. Additionally, it is possible that the resolution of current or future legal matters and claims could result in changes to our industry and business practices, losses material to our results of operations, financial condition and liquidity or damage to our reputation.
We are frequently the subject of regulatory market conduct and other reviews, audits and investigations by state insurance and health and welfare and pharmacy departments, attorneys general, DOJ, CMS, DOL and the OIG and comparable authorities in foreign jurisdictions. Additionally, we are, and may in the future be, subject to qui tam actions in which the government may or may not intervene. With respect to our Medicare Advantage and Medicare Part D businesses, CMS and OIG perform audits to determine a health plan's compliance with federal regulations and contractual obligations, including compliance with proper coding practices and fraud and abuse enforcement practices through audits designed to detect and correct improper payments. Certain of our contracts are currently subject to RADV audits by CMS and the OIG. The DOJ is conducting industry-wide investigations of the risk adjustment data submission practices and business processes of Cigna and a number of other Medicare Advantage organizations. There also continues to be heightened review by federal and state regulators of business and reporting practices within the health services industry, including with respect to claims payment and related escheat practices, and increased scrutiny by other federal and state governmental agencies (such as state attorneys general) empowered to bring criminal actions in circumstances that could have previously given rise only to civil or administrative proceedings.
In addition, various government agencies have conducted investigations and audits into certain pharmacy benefit management practices. Many of these investigations and audits have resulted in other companies being subject to civil penalties, including the payment of money and entry into corporate integrity agreements. We cannot predict what effect, if any, such government investigations and audits may ultimately have on us or on the industry in general. However, we will likely continue to experience government scrutiny and audit activity, which has and may in the future result in civil penalties.
Regulatory audits, investigations or reviews or actions by other government agencies could result in changes to our business practices, retroactive adjustments to certain premiums, significant fines, penalties, civil liabilities, criminal liabilities or other sanctions, including corporate integrity agreements, restrictions on our ability to participate in government programs, market certain products or engage in business-related activities, that could have a material adverse effect on our business, results of operation, financial condition and liquidity. In addition, disclosure of an adverse investigation or audit or the imposition of fines or other sanctions could negatively affect our reputation in certain markets and make it more difficult for us to sell our products and services.
A description of material pending legal actions and other legal and regulatory matters is included in Note 22 to the Consolidated Financial Statements included in this Form 10-K. The outcome of litigation and other legal or regulatory matters is always uncertain.
If we fail to comply with applicable privacy, security and data laws, regulations and standards, our business and reputation could be materially adversely affected.
Most of our activities involve the receipt, use, storage or transmission of a substantial amount of individuals' protected health information and personally identifiable information. We also use aggregated and anonymized data for research and analysis purposes,
44
and in some cases, provide access to such de-identified data, or analytics created from such data, to pharmaceutical manufacturers and third-party data aggregators and analysts. We may also use such information to create analytic models designed to predict, and potentially improve, outcomes and patient care. The collection, maintenance, protection, use, transmission, disclosure and disposal of sensitive personal information are regulated at the federal, state, international and industry levels and requirements are imposed on us by contracts with clients. In some cases, such laws, rules, regulations and contractual requirements also apply to our vendors and require us to obtain written assurances of their compliance with such requirements. We are also subject to various other consumer protection laws that regulate our communications with customers. Certain of our businesses are also subject to the Payment Card Industry Data Security Standard, which is designed to protect credit card account data as mandated by payment card industry entities. International laws, rules and regulations governing the use and disclosure of such information, such as the GDPR, can be more stringent than in the United States, and they vary across jurisdictions. In addition, more jurisdictions are regulating the transfer of data across borders and domestic privacy and data protection laws are generally becoming more onerous.
These laws, rules and contractual requirements are subject to change and the regulatory environment surrounding data security and privacy is increasingly demanding. Compliance with existing or new privacy, security and data laws, regulations and requirements may result in increased operating costs, and may constrain or require us to alter our business model or operations. For more information on privacy regulations to which we are subject, see "Business – Regulation" in Part I, Item 1 of this Form 10-K.
HIPAA requires covered entities to comply with the HIPAA privacy, security and breach rules. In addition, business associates must comply with the HIPAA security and breach requirements. While we endeavor to provide appropriate protections through our contracts with our third-party service providers and in certain cases assess their security controls, we have limited oversight or control over their actions and practices. Several of our businesses act as business associates to their covered entity customers and, as a result, collect, use, disclose and maintain sensitive personal information in order to provide services to these customers. HHS administers an audit program to assess HIPAA compliance efforts by covered entities and business associates. In addition, HHS continues to exercise its enforcement authority, such as enforcement actions resulting from investigations brought on by notification to HHS of a breach. An audit resulting in findings or allegations of noncompliance or the implementation of an enforcement action could have an adverse effect on our results of operations, financial position, cash flows and reputation.
Noncompliance or findings of noncompliance with applicable laws, regulations or requirements, or the occurrence of any privacy or security breach involving the misappropriation, loss or other unauthorized disclosure of protected personal information, whether by us or by one of our third-party service providers, could materially adversely affect our business and reputation, including our results of operations, financial position and cash flows.
Effective prevention, detection and control systems are critical to maintain regulatory compliance and prevent fraud and failure of these systems could adversely affect us.
Federal and state governments have made investigating and prosecuting health care and other insurance fraud and abuse a priority. Fraud and abuse prohibitions encompass a wide range of activities including kickbacks for referral of customers, billing for unnecessary medical services, improper marketing and violations of patient privacy rights. The regulations and contractual requirements applicable to us are complex and subject to change. In addition, ongoing vigorous law enforcement, a highly technical regulatory scheme and the Dodd-Frank Act and related regulations enhance regulators' enforcement powers and whistleblower incentives and protections. Our compliance efforts in this area will continue to require significant resources. Failure of our prevention, detection or control systems related to regulatory compliance or the failure of employees to comply with our internal policies including data systems security or unethical conduct by managers and employees, could adversely affect our reputation and also expose us to litigation and other proceedings, fines and penalties.
In addition, provider or customer fraud that is not prevented or detected could impact our medical costs or those of our self-insured clients. Further, during an economic downturn, we may experience increased fraudulent claims volume that may lead to additional costs due to an increase in disputed claims and litigation.
Economic Risks
Economic and market conditions affect the value of our financial instruments and the value of particular assets and liabilities, investment income and interest expense.
As an insurer, we have substantial investment assets that support insurance and contractholder deposit liabilities and surplus requirements in our regulated companies. The market values of our investments vary depending on economic and market conditions with no offsetting change in the value of a portion of our liabilities. A substantial portion of our investment assets are in fixed interest-yielding debt securities of varying maturities and commercial mortgage loans. The value of these investment assets can fluctuate
45
significantly with changes in market conditions. A rise in interest rates would likely reduce the value of our investment portfolio, increase interest expense on our indebtedness and increase investment income as investment assets mature and are replaced. In addition, an economic contraction could result in delay in payment of principal or interest by issuers, or defaults by issuers, reducing our investment income and requiring us to write down the value of our investments.
Significant stock market or interest rate declines could result in additional unfunded pension obligations resulting in the need for additional plan funding by us and increased pension expenses.
We currently have unfunded obligations in our frozen pension plans. A significant decline in the value of the plans' equity and fixed income investments or unfavorable changes in applicable laws or regulations could materially increase our expenses and change the timing and amount of required plan funding. This could reduce the cash available to us, including our subsidiaries. We are also exposed to interest rate and equity risk associated with our pension obligations. Sustained declines in interest rates could have an adverse impact on the funded status of our pension plans and our reinvestment yield on new investments. See Note 16 to the Consolidated Financial Statements for more information on our obligations under the pension plans.
A downgrade in the financial strength ratings of our insurance subsidiaries could adversely affect new sales and retention of current business, and a downgrade in our debt ratings would increase the cost of borrowed funds and could negatively affect our ability to access capital.
Financial strength, claims paying ability and debt ratings by recognized rating organizations are each important factors in establishing the competitive position of insurance and health benefits companies. Ratings information by nationally recognized ratings agencies is broadly disseminated and generally used throughout the industry. We believe that the claims paying ability and financial strength ratings of our principal insurance subsidiaries are important factors in marketing our products to certain customers. Our debt ratings impact both the cost and availability of future borrowings and, accordingly, our cost of capital. Each of the rating agencies reviews ratings periodically and there can be no assurance that current ratings will be maintained in the future. A downgrade of any of these ratings in the future could make it more difficult to either market our products successfully or raise capital to support business growth.
We maintain significant indebtedness in the ordinary course of business and may incur further indebtedness in the future. Our indebtedness could adversely affect our financial condition, our ability to react to changes in the economy or our industry and could divert our cash flow from operations for debt service costs, leaving us with less cash flow from operations available to fund growth, stock repurchases, dividends and other corporate purposes.
The total indebtedness of Cigna was approximately $33.7 billion as of December 31, 2021. Carrying indebtedness:
•requires us to dedicate a portion of our cash flow from operations to debt payments, thereby reducing the availability of cash flow to fund our operations and growth strategy, including investments, acquisitions and capital expenditures, make stock repurchases, pay dividends and for general corporate purposes;
•increases our vulnerability to general adverse economic and industry conditions, which may require us to dedicate an even greater percentage of our cash flow from operations to the payment of principal and interest on our debt and limit our access to capital markets such that additional capital may not be available or may be available only on unfavorable terms;
•exposes us to increases in interest rates to the extent increased interest expense is not offset by increased income from our investment assets; and
•limits our flexibility in planning for, or reacting to, changes in or challenges relating to our business and industry.
The covenants in our debt instruments may have the effect, among other things, of restricting our financial and operating flexibility to respond to significant changes in business and economic conditions. We may incur or assume significantly more debt in the future which may subject us to additional restrictive covenants and increase the risks described above. If our cash flow and capital resources are insufficient to service our debt obligations, we may be forced to seek additional dividends from our subsidiaries, sell assets, seek additional equity or debt capital or restructure our debt.
Unfavorable developments in economic conditions may adversely affect our business, results of operations and financial condition.
Many factors, including geopolitical issues, future economic downturns, man-made disasters, natural disasters (including those as a result of climate change) and pandemics, availability and cost of credit and other capital and consumer spending can negatively impact the U.S. and global economies. Our results of operations could be materially adversely affected by the impact of unfavorable
46
economic conditions on our clients and customers (both employers and individuals), health care providers, pharmacy manufacturers, pharmacy providers and third-party vendors. For example:
•Employers may take action to reduce their operating costs by modifying, delaying or canceling plans to purchase our products or making changes in the mix of products purchased that are unfavorable to us.
•Higher unemployment rates, employee attrition (including challenges filling open positions in light of an increasingly competitive job market) and workforce reductions could result in lower enrollment in our employer-based plans (including an increase in the number of employees who opt out of employer-based plans) or our individual plans.
•Because of unfavorable economic conditions or the ACA, employers may stop offering health care coverage to employees or elect to offer this coverage on a voluntary, employee-funded basis as a means to reduce their operating costs.
•If clients are not successful in generating sufficient funds or are precluded from securing financing, they may not be able to pay, or may delay payment of, accounts receivable that are owed to us.
•Our clients or potential clients may force us to compete more vigorously on factors such as price and service to retain or obtain their business.
•Our clients may be acquired, consolidated, or otherwise fail to successfully maintain or grow their business or workforce, which could reduce the number of customers we serve or otherwise result in lower than anticipated utilization of our services.
•A prolonged unfavorable economic environment could adversely impact the financial position of hospitals and other health care providers, potentially increasing our medical costs.
•Our third-party vendors could significantly and quickly increase their prices or reduce their output to reduce their operating costs. Our business depends on our ability to perform necessary business functions in an efficient and uninterrupted fashion.
•Other insurers' financial condition may be weakened, increasing the risk that we will receive significant assessments for obligations of insolvent insurers pursuant to guaranty associations, indemnity funds or other similar laws and regulations.
Certain of the foregoing events have occurred and may continue to occur, and the occurrence of these events may, individually or in the aggregate, lead to a decrease in our customer base, revenues or margins or an increase in our operating costs.
In addition, during and following a prolonged unfavorable economic environment, federal and state budgets could be materially adversely affected, resulting in reduced or delayed reimbursements or payments in government programs such as Medicare and Social Security or under contracts with government entities. These budgetary pressures also could cause the government to impose new or a higher level of taxes or assessments on us, such as premium taxes on insurance companies and HMOs and surcharges or fees on select fee-for-service and capitated medical claims. Although we could attempt to mitigate or cover our exposure from such increased costs through, among other things, increases in premiums, there can be no assurance that we will be able to mitigate or cover all of such costs, which may have a material adverse effect on our business, results of operations, financial condition and liquidity.
We are subject to the credit risk of our reinsurers.
We enter into reinsurance arrangements with other insurance companies, primarily in connection with acquisition or divestiture transactions when the underwriting company is not being acquired or sold. Under all reinsurance arrangements, reinsurers assume insured losses, subject to certain limitations or exceptions that may include a loss limit. These arrangements also subject us to various obligations, representations and warranties with the reinsurers. Reinsurance does not relieve us of liability as the originating insurer. We remain liable to the underlying policyholders if a reinsurer defaults on obligations under the reinsurance arrangement. Although we regularly evaluate the financial condition of reinsurers to minimize exposure to significant losses from reinsurer insolvencies, reinsurers may become financially unsound. If a reinsurer fails to meet its obligations under the reinsurance contract or if the liabilities exceed any applicable loss limit, we will be forced to cover the claims on the reinsured policies.
The collectability of amounts due from reinsurers is subject to uncertainty arising from a number of factors, including whether the insured losses meet the qualifying conditions of the reinsurance contract, whether reinsurers or their affiliates have the financial capacity and willingness to make payments under the terms of the reinsurance contract and the magnitude and type of collateral supporting our reinsurance recoverable, such as holding sufficient qualifying assets in trusts or letters of credit issued. Although a portion of our reinsurance exposures are secured, the inability to collect a material recovery from a reinsurer could have a material adverse effect on our results of operations, financial condition and liquidity.
47
Item 1B. UNRESOLVED STAFF COMMENTS
None.
Item 2. PROPERTIES
As of the end of 2021, our global real estate portfolio consisted of approximately 11.7 million square feet of owned and leased properties to support the operations of our reporting segments. Our domestic portfolio had approximately 9.7 million square feet in 43 states, the District of Columbia and the U.S. Virgin Islands. Our international properties contain approximately 2.0 million square feet located throughout the following countries: Australia, Bahrain, Belgium, Canada, Cayman Islands, China, France, Germany, Hong Kong, India, Indonesia, Kenya, Kuwait, Lebanon, Malaysia, New Zealand, Oman, Singapore, South Korea, Spain, Switzerland, Taiwan, Thailand, Turkey, United Arab Emirates and the United Kingdom. Approximately 1.1 million square feet of international properties is held for sale.
Our principal domestic office locations include the Wilde Building located at 900 Cottage Grove Road in Bloomfield, Connecticut (our corporate headquarters), Two Liberty Place located at 1601 Chestnut Street in Philadelphia, Pennsylvania and Evernorth's corporate offices located at and around One Express Way in St. Louis, Missouri. The Wilde Building measures approximately 893,000 square feet and is owned. The St. Louis campus measures approximately 1.2 million square feet of leased space and Two Liberty Place measures approximately 265,000 square feet and is leased space.
The pharmacy operations consist of 13 order processing home delivery and specialty pharmacies, six patient contact centers, 30 specialty dispensing pharmacies and four high-volume automated dispensing pharmacies located throughout the United States. Our high-volume automated dispensing pharmacies are located in Arizona, Indiana, Missouri and New Jersey.
In the fourth quarter of 2021, we approved an additional strategic initiative to drive operational improvements and efficiencies. This initiative includes a reduction in the square footage of owned and leased properties and changes to how sites are utilized.
We believe our properties are adequate and suitable for our business as presently conducted. The foregoing does not include information on investment properties.
Item 3. LEGAL PROCEEDINGS
The information contained under "Litigation Matters" and "Regulatory Matters" in Note 22 to the Consolidated Financial Statements of this Form 10-K is incorporated herein by reference.
Item 4. MINE SAFETY DISCLOSURES
Not applicable.
48
Information about our Executive Officers
The principal occupations and employment histories of our executive officers (as of February 23, 2022) are listed below.
CHARLES G. BERG, 64, President, Government Business of Cigna beginning January 2022; Executive Chairman of DaVita Medical Group from November 2016 until December 2017; and Non-Executive Chairman of WellCare Health Plans, Inc. from January 2011 until May 2013.
DAVID M. CORDANI, 56, Chairman of the Board of Cigna beginning January 2022; Chief Executive Officer beginning December 2009; Director since October 2009; President beginning June 2008; and Chief Operating Officer from June 2008 until December 2009.
NOELLE K. EDER, 52, Executive Vice President, Global Chief Information Officer of Cigna beginning September 2020; Executive Vice President, Chief Information and Digital Officer at Hilton Worldwide Holdings from March 2018 until August 2020; Executive Vice President, Chief Card Customer Experience Officer at Capital One Financial Corporation from November 2016 until 2018; and Executive Vice President, Customer Experience and Operations at Capital One Financial Corporation from September 2014 until November 2016.
BRIAN C. EVANKO, 45, Executive Vice President and Chief Financial Officer beginning January 2021; President, Government Business from November 2017 to January 2021; and President, U.S. Individual Business from August 2013 to November 2017.
NICOLE S. JONES, 51, Executive Vice President and General Counsel of Cigna beginning June 2011; Senior Vice President and General Counsel of Lincoln Financial Group from May 2010 until June 2011; Vice President and Deputy General Counsel of Cigna from April 2008 until May 2010; and Corporate Secretary of Cigna from September 2006 until April 2010.
JOHN M. MURABITO, 63, Executive Vice President and Chief Administrative Officer beginning August 2021; and Executive Vice President, Human Resources and Services from August 2003 until August 2021.
EVERETT NEVILLE, 57, Executive Vice President, Strategy, Corporate Development & Solutions beginning October 2021; Executive Vice President, Strategy and Business Development from January 2021 to October 2021; Senior Vice President, Value Creation and Solutions from January 2020 until January 2021; Chief Value Officer from December 2018 until January 2020; Executive Vice President, Strategy, Supply Chain & Specialty, Express Scripts from January 2018 until December 2018; Senior Vice President, Strategy, Supply Chain & Specialty from November 2016 until January 2018; and Senior Vice President, Supply Chain from March 2015 until November 2016.
ERIC P. PALMER, 45, President and Chief Executive Officer of Evernorth beginning January 2022; President and Chief Operating Officer, Evernorth from January 2021 until December 2021; Executive Vice President and Chief Financial Officer from June 2017 to January 2021; Deputy Chief Financial Officer from February 2017 until June 2017; Senior Vice President, Chief Business Financial Officer from November 2015 to February 2017; and Vice President, Business Financial Officer, Health Care from April 2012 to November 2015.
CYNTHIA RYAN, 48, Executive Vice President, Chief Human Resources Officer beginning August 2021; Senior Vice President, Human Resources from December 2018 to August 2021; Vice President, Human Resources from January 2017 to December 2018; and Vice President, Talent Management from May 2014 to January 2017.
JASON D. SADLER, 53, President, International Markets beginning June 2014; and President, Global Individual Health, Life and Accident from July 2010 until June 2014.
PAUL SANFORD, 54, Executive Vice President, Operations beginning September 2021; Senior Vice President, Operations and Solutions Delivery from January 2021 to September 2021; Senior Vice President, Solutions Delivery from January 2019 to December 2020; Vice President, Solutions Delivery from February 2017 to December 2018; and Vice President, Operating Effectiveness from September 2008 to February 2017.
MICHAEL W. TRIPLETT, 60, President, U.S. Commercial beginning February 2017; and Regional Segment Lead from June 2009 to February 2017.
49
PART II
Item 5. MARKET FOR REGISTRANT'S COMMON EQUITY, RELATED STOCKHOLDER MATTERS AND ISSUER PURCHASES OF EQUITY SECURITIES
As of December 31, 2021, the number of shareholders of record was 31,489. Cigna's common stock is listed with, and trades on, the New York Stock Exchange under the symbol "CI".
In 2021, Cigna initiated a quarterly cash dividend and declared quarterly cash dividends of $1.00 per share of Cigna common stock. Cigna currently intends to pay regular quarterly dividends, with future declarations subject to approval by its Board of Directors and the Board's determination that the declaration of dividends remains in the best interests of Cigna and its shareholders. The decision of whether to pay future dividends and the amount of any such dividends will be based on the Company's financial position, results of operations, cash flows, capital requirements, the requirements of applicable law and any other factors the Board of Directors may deem relevant.
For the years ended December 31, 2020 and 2019, Cigna paid a yearly cash dividend of $0.04 per share of Cigna common stock.
See Note 8 to the Consolidated Financial Statements for further information on dividend payments.
For information on securities authorized for issuance under our existing equity compensation plans, see Item 12 under the heading "Security Ownership of Certain Beneficial Owners and Management and Rebated Stockholder Matters."
Issuer Purchases of Equity Securities
The following table provides information about Cigna's share repurchase activity for the quarter ended December 31, 2021:
| Period | Total # of shares purchased (1) | Average price paid per share (1) | Total # of shares purchased as part of publicly announced program (2) | Approximate dollar value of shares that may yet be purchased as part of publicly announced program (3) | ||||||||||||||||||||||
| October 1-31, 2021 | 567 | $ | 209.40 | — | $ | 6,619,335,337 | ||||||||||||||||||||
| November 1-30, 2021 | 3,744,700 | (1) | 3,742,474 | $ | 6,009,814,491 | |||||||||||||||||||||
| December 1-31, 2021 | 4,913,254 | (1) | 4,905,726 | $ | 5,162,962,098 | |||||||||||||||||||||
| Total | 8,658,521 | (1) | 8,648,200 | N/A | ||||||||||||||||||||||
(1)Includes shares tendered by employees under the Company's equity compensation plans as follows: 1) payment of taxes on vesting of restricted stock (grants and units) and strategic performance shares and 2) payment of the exercise price and taxes for certain stock options exercised. Employees tendered 567 shares in October, 2,226 shares in November and 7,528 shares in December 2021. Amount purchased also reflects the final delivery of 910,182 shares in November 2021 and 932,888 shares in December 2021 pursuant to the ASR agreements discussed in the Liquidity and Capital Resources section of Management's Discussion and Analysis of Financial Condition and Results of Operations in Part I, Item 2. Such repurchases were made pursuant to the Company's share repurchase program described in note (2) of this table. Average price paid per share for shares not purchased pursuant to the ASR agreements was $215.20 in November 2021 and $213.17 in December 2021.
(2)Additionally, the Company maintains a share repurchase program authorized by the Board of Directors. Under this program, the Company may repurchase shares from time to time, depending on market conditions and alternate uses of capital. The timing and actual number of shares repurchased will depend on a variety of factors, including price, general business and market conditions and alternate uses of capital. The share repurchase program may be effected through Rule 10b5-1 plans, open market purchases, each in compliance with Rule 10b-18 under the Exchange Act, or privately negotiated transactions. The program may be suspended or discontinued at any time and does not have an expiration date. In February 2022, the Board increased repurchase authority by an additional $2.0 billion. Share repurchase authority was $6.0 billion as of February 23, 2022.
(3)Approximate dollar value of shares is as of the last date of the applicable month.
50
Stock Price Performance Graph
The graph below compares the cumulative total shareholder return on our common stock for the five years ended December 31, 2021 with the cumulative total return of the Standard & Poor's ("S&P") 500 Index and the S&P 500 Health Care Index. The stock performance shown in the graph is not intended to forecast or be indicative of future performance.
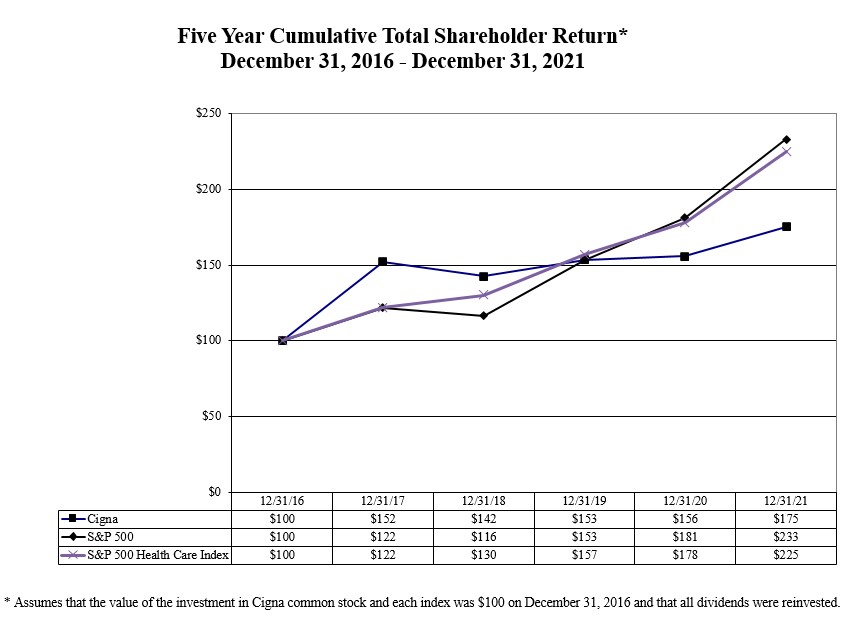
Item 6. [Reserved]
51
Item 7. MANAGEMENT'S DISCUSSION AND ANALYSIS OF FINANCIAL CONDITION AND RESULTS OF OPERATIONS
| PAGE | |||||
Management's Discussion and Analysis of Financial Condition and Results of Operations ("MD&A") is intended to provide information to assist you in better understanding and evaluating our financial condition as of December 31, 2021 compared with December 31, 2020 and our results of operations for 2021 compared with 2020 and 2019 and is intended to help you understand the ongoing trends in our business. We encourage you to read this MD&A in conjunction with our Consolidated Financial Statements included in Part II, Item 8 of this Annual Report on Form 10-K ("Form 10-K") and the "Risk Factors" contained in Part I, Item 1A of this Form 10-K.
Unless otherwise indicated, financial information in this MD&A is presented in accordance with accounting principles generally accepted in the United States of America ("GAAP"). See Note 2 to the Consolidated Financial Statements in this Form 10-K for additional information regarding the Company's significant accounting policies. In some of our financial tables in this MD&A, we present either percentage changes or "N/M" when those changes are so large as to become not meaningful. Changes in percentages are expressed in basis points ("bps").
In this MD&A, our consolidated measures "adjusted income from operations," earnings per share on that same basis and "adjusted revenues" are not determined in accordance with GAAP and should not be viewed as substitutes for the most directly comparable GAAP measures of "shareholders' net income," "earnings per share" and "total revenues." We also use pre-tax adjusted income (loss) from operations and adjusted revenues to measure the results of our segments.
The Company uses "pre-tax adjusted income (loss) from operations" and "adjusted revenues" as its principal financial measures of segment operating performance because management believes these metrics best reflect the underlying results of business operations and permit analysis of trends in underlying revenue, expenses and profitability. We define adjusted income from operations as shareholders' net income (or income before income taxes for the segment metric) excluding net realized investment results, amortization of acquired intangible assets, results of transitioning clients prior to 2020 and special items. Cigna's share of certain realized investment results of its joint ventures reported in the Cigna Healthcare segment using the equity method of accounting are also excluded. Special items are matters that management believes are not representative of the underlying results of operations due to their nature or size. Adjusted income (loss) from operations is measured on an after-tax basis for consolidated results and on a pre-tax basis for segment results. Consolidated adjusted income (loss) from operations is not determined in accordance with GAAP and should not be viewed as a substitute for the most directly comparable GAAP measure, shareholders' net income. See the below Financial Highlights section for a reconciliation of consolidated adjusted income from operations to shareholders' net income.
The Company defines adjusted revenues as total revenues excluding the following adjustments: special items, revenue contribution from transitioning clients prior to 2020 and Cigna's share of certain realized investment results of its joint ventures reported in the Cigna Healthcare segment using the equity method of accounting. Special items are matters that management believes are not representative of the underlying results of operations due to their nature or size. We exclude these items from this measure because management believes they are not indicative of past or future underlying performance of the business. Adjusted revenues is not determined in accordance with GAAP and should not be viewed as a substitute for the most directly comparable GAAP measure, total revenues. See the below Financial Highlights section for a reconciliation of consolidated adjusted revenues to total revenues.
52
EXECUTIVE OVERVIEW
Cigna Corporation, together with its subsidiaries (either individually or collectively referred to as "Cigna," the "Company," "we," "our" or "us") is a global health services organization with a mission of helping those we serve improve their health, well-being and peace of mind by making health care affordable, predictable and simple. Our subsidiaries offer a differentiated set of pharmacy, medical, dental and related products and services. For further information on our business and strategy, see Item 1, "Business" in this Form 10-K.
Financial Highlights
See Note 1 to the Consolidated Financial Statements for a description of our segments.
Summarized below are certain key measures of our performance by segment for the years ended December 31, 2021, 2020 and 2019:
| Financial highlights by segment | ||||||||||||||||||||||||||||||||||||||
| For the Years Ended December 31, | Increase (Decrease) | Increase (Decrease) | ||||||||||||||||||||||||||||||||||||
| (Dollars in millions, except per share amounts) | 2021 | 2020 | 2019 | 2021 vs. 2020 | 2020 vs. 2019 | |||||||||||||||||||||||||||||||||
| Revenues | ||||||||||||||||||||||||||||||||||||||
| Adjusted revenues by segment | ||||||||||||||||||||||||||||||||||||||
| Evernorth | $ | 131,912 | $ | 116,130 | $ | 96,447 | 14 | % | 20 | % | ||||||||||||||||||||||||||||
| Cigna Healthcare | 44,652 | 41,135 | 39,089 | 9 | 5 | |||||||||||||||||||||||||||||||||
| Other Operations | 3,989 | 8,446 | 8,215 | (53) | 3 | |||||||||||||||||||||||||||||||||
| Corporate, net of eliminations | (6,475) | (5,644) | (3,576) | (15) | (58) | |||||||||||||||||||||||||||||||||
| Adjusted revenues | 174,078 | 160,067 | 140,175 | 9 | 14 | |||||||||||||||||||||||||||||||||
| Revenue contribution from transitioning clients | — | — | 13,347 | N/M | N/M | |||||||||||||||||||||||||||||||||
| Net realized investment results from certain equity method investments | — | 130 | 44 | N/M | 195 | |||||||||||||||||||||||||||||||||
| Special item related to contractual adjustment for a former client | — | 204 | — | N/M | N/M | |||||||||||||||||||||||||||||||||
| Total revenues | $ | 174,078 | $ | 160,401 | $ | 153,566 | 9 | % | 4 | % | ||||||||||||||||||||||||||||
| Shareholders' net income | $ | 5,365 | $ | 8,458 | $ | 5,104 | (37) | % | 66 | % | ||||||||||||||||||||||||||||
| Adjusted income from operations | $ | 6,980 | $ | 6,795 | $ | 6,476 | 3 | % | 5 | % | ||||||||||||||||||||||||||||
| Earnings per share (diluted) | ||||||||||||||||||||||||||||||||||||||
| Shareholders' net income | $ | 15.73 | $ | 22.96 | $ | 13.44 | (31) | % | 71 | % | ||||||||||||||||||||||||||||
| Adjusted income from operations | $ | 20.47 | $ | 18.45 | $ | 17.05 | 11 | % | 8 | % | ||||||||||||||||||||||||||||
| Pre-tax adjusted income (loss) from operations by segment | ||||||||||||||||||||||||||||||||||||||
| Evernorth | $ | 5,818 | $ | 5,363 | $ | 5,092 | 8 | % | 5 | % | ||||||||||||||||||||||||||||
| Cigna Healthcare | 3,609 | 4,031 | 3,963 | (10) | 2 | |||||||||||||||||||||||||||||||||
| Other Operations | 889 | 966 | 1,131 | (8) | (15) | |||||||||||||||||||||||||||||||||
| Corporate, net of eliminations | (1,339) | (1,552) | (1,824) | 14 | 15 | |||||||||||||||||||||||||||||||||
| Consolidated pre-tax adjusted income from operations | 8,977 | 8,808 | 8,362 | 2 | 5 | |||||||||||||||||||||||||||||||||
| Adjustment for transitioning clients | — | — | 1,726 | N/M | N/M | |||||||||||||||||||||||||||||||||
| Income attributable to noncontrolling interests | 58 | 37 | 20 | 57 | 85 | |||||||||||||||||||||||||||||||||
Net realized investment gains (losses) (1) | 196 | 279 | 221 | (30) | 26 | |||||||||||||||||||||||||||||||||
| Amortization of acquired intangible assets | (1,998) | (1,982) | (2,949) | (1) | 33 | |||||||||||||||||||||||||||||||||
| Special items | (451) | 3,726 | (810) | N/M | N/M | |||||||||||||||||||||||||||||||||
| Income before income taxes | $ | 6,782 | $ | 10,868 | $ | 6,570 | (38) | % | 65 | % | ||||||||||||||||||||||||||||
(1) Includes the Company's share of certain realized investment results of its joint ventures reported in the Cigna Healthcare segment using the equity method of accounting.
For further analysis and explanation of each segment's results, see the "Segment Reporting" section of this MD&A.
53
| Consolidated Results of Operations (GAAP basis) | |||||||||||||||||||||||||||||||||||||||||||||||
| For the Years Ended December 31, | Increase (Decrease) | Increase (Decrease) | |||||||||||||||||||||||||||||||||||||||||||||
| (Dollars in millions) | 2021 | 2020 | 2019 | 2021 vs. 2020 | 2020 vs. 2019 | ||||||||||||||||||||||||||||||||||||||||||
| Pharmacy revenues | $ | 121,413 | $ | 107,769 | $ | 103,099 | $ | 13,644 | 13 | % | $ | 4,670 | 5 | % | |||||||||||||||||||||||||||||||||
| Premiums | 41,154 | 42,627 | 39,714 | (1,473) | (3) | 2,913 | 7 | ||||||||||||||||||||||||||||||||||||||||
| Fees and other revenues | 9,962 | 8,761 | 9,363 | 1,201 | 14 | (602) | (6) | ||||||||||||||||||||||||||||||||||||||||
| Net investment income | 1,549 | 1,244 | 1,390 | 305 | 25 | (146) | (11) | ||||||||||||||||||||||||||||||||||||||||
| Total revenues | 174,078 | 160,401 | 153,566 | 13,677 | 9 | 6,835 | 4 | ||||||||||||||||||||||||||||||||||||||||
| Pharmacy and other service costs | 117,553 | 103,484 | 97,668 | 14,069 | 14 | 5,816 | 6 | ||||||||||||||||||||||||||||||||||||||||
| Medical costs and other benefit expenses | 33,562 | 32,710 | 30,819 | 852 | 3 | 1,891 | 6 | ||||||||||||||||||||||||||||||||||||||||
| Selling, general and administrative expenses | 13,030 | 14,072 | 14,053 | (1,042) | (7) | 19 | — | ||||||||||||||||||||||||||||||||||||||||
| Amortization of acquired intangible assets | 1,998 | 1,982 | 2,949 | 16 | 1 | (967) | (33) | ||||||||||||||||||||||||||||||||||||||||
| Total benefits and expenses | 166,143 | 152,248 | 145,489 | 13,895 | 9 | 6,759 | 5 | ||||||||||||||||||||||||||||||||||||||||
| Income from operations | 7,935 | 8,153 | 8,077 | (218) | (3) | 76 | 1 | ||||||||||||||||||||||||||||||||||||||||
| Interest expense and other | (1,208) | (1,438) | (1,682) | 230 | 16 | 244 | 15 | ||||||||||||||||||||||||||||||||||||||||
| Debt extinguishment costs | (141) | (199) | (2) | 58 | 29 | (197) | N/M | ||||||||||||||||||||||||||||||||||||||||
| Gain (loss) on sale of business | — | 4,203 | — | (4,203) | N/M | 4,203 | N/M | ||||||||||||||||||||||||||||||||||||||||
| Net realized investment gains (losses) | 196 | 149 | 177 | 47 | 32 | (28) | (16) | ||||||||||||||||||||||||||||||||||||||||
| Income before income taxes | 6,782 | 10,868 | 6,570 | (4,086) | (38) | 4,298 | 65 | ||||||||||||||||||||||||||||||||||||||||
| Total income taxes | 1,367 | 2,379 | 1,450 | (1,012) | (43) | 929 | 64 | ||||||||||||||||||||||||||||||||||||||||
| Net income | 5,415 | 8,489 | 5,120 | (3,074) | (36) | 3,369 | 66 | ||||||||||||||||||||||||||||||||||||||||
| Less: Net income attributable to noncontrolling interests | 50 | 31 | 16 | 19 | 61 | 15 | 94 | ||||||||||||||||||||||||||||||||||||||||
| Shareholders' net income | $ | 5,365 | $ | 8,458 | $ | 5,104 | $ | (3,093) | (37) | % | $ | 3,354 | 66 | % | |||||||||||||||||||||||||||||||||
| Consolidated effective tax rate | 20.2 | % | 21.9 | % | 22.1 | % | (170) | bps | (20) | bps | |||||||||||||||||||||||||||||||||||||
| Medical customers (in thousands) | 17,081 | 16,650 | 17,137 | 431 | 3 | % | (487) | (3) | % | ||||||||||||||||||||||||||||||||||||||
| Reconciliation of Shareholders' Net Income (GAAP) to Adjusted Income from Operations | ||||||||||||||||||||||||||||||||||||||
| Dollars in Millions | Diluted Earnings Per Share | |||||||||||||||||||||||||||||||||||||
| For the Years Ended December 31, | For the Years Ended December 31, | |||||||||||||||||||||||||||||||||||||
| 2021 | 2020 | 2019 | 2021 | 2020 | 2019 | |||||||||||||||||||||||||||||||||
| Shareholders' net income | $ | 5,365 | $ | 8,458 | $ | 5,104 | $ | 15.73 | $ | 22.96 | $ | 13.44 | ||||||||||||||||||||||||||
| After-tax adjustments required to reconcile to adjusted income from operations | ||||||||||||||||||||||||||||||||||||||
Net realized investment (gains) losses (1) | (158) | (244) | (190) | (0.46) | (0.66) | (0.50) | ||||||||||||||||||||||||||||||||
| Amortization of acquired intangible assets | 1,494 | 1,431 | 2,248 | 4.38 | 3.88 | 5.92 | ||||||||||||||||||||||||||||||||
| Adjustment for transitioning clients | — | — | (1,316) | — | — | (3.46) | ||||||||||||||||||||||||||||||||
| Special items | ||||||||||||||||||||||||||||||||||||||
| Charge for organizational efficiency plan | 119 | 24 | 162 | 0.35 | 0.07 | 0.43 | ||||||||||||||||||||||||||||||||
| Debt extinguishment costs | 110 | 151 | — | 0.32 | 0.41 | — | ||||||||||||||||||||||||||||||||
| Integration and transaction-related (benefits) costs | 71 | 404 | 427 | 0.21 | 1.10 | 1.11 | ||||||||||||||||||||||||||||||||
| (Benefits) charges associated with litigation matters | (21) | 19 | 41 | (0.06) | 0.05 | 0.11 | ||||||||||||||||||||||||||||||||
| Risk corridors recovery | — | (76) | — | — | (0.21) | — | ||||||||||||||||||||||||||||||||
| Contractual adjustment for a former client | — | (155) | — | — | (0.42) | — | ||||||||||||||||||||||||||||||||
| (Gain) on sale of business | — | (3,217) | — | — | (8.73) | — | ||||||||||||||||||||||||||||||||
| Total special items | 279 | (2,850) | 630 | 0.82 | (7.73) | 1.65 | ||||||||||||||||||||||||||||||||
| Adjusted income from operations | $ | 6,980 | $ | 6,795 | $ | 6,476 | $ | 20.47 | $ | 18.45 | $ | 17.05 | ||||||||||||||||||||||||||
(1) Includes the Company's share of certain realized investment results of its joint ventures reported in the Cigna Healthcare segment using the equity method of accounting.
54
COVID-19 Update
Cigna's commitment to the health, well-being and peace of mind of our employees and the people we serve remains the primary focus as the pandemic continues to impact all aspects of daily life. Cigna is leveraging its resources, expertise, data and actionable intelligence to assist customers, clients and care providers navigate the evolving dynamics of the pandemic. The Company continues to encourage COVID-19 vaccinations across all eligible populations to help control the spread of the virus, limit the severity of the disease and save lives. Cigna has also expanded access to testing, care and supportive resources to help everyone it serves take care of their physical and mental health during this time, and will continue to do so.
For the fourth quarter of 2021, our Cigna Healthcare segment reflected net unfavorable COVID-19 related impacts, although not as significant when compared to those recognized in the same period in 2020. For the year ended December 31, 2021 compared to 2020, the net unfavorable impacts reflect increased direct costs of COVID-19 testing, treatment and vaccines as well as the significant deferral of care by our customers in 2020. These impacts were partially offset by the absence of the premium relief programs implemented in 2020.
We continue to optimize purchasing volume across the pharmaceutical supply chain in order to mitigate risk of disruption with prescription drug supply due to ongoing global supply disruptions.
The situation surrounding COVID-19 remains fluid with continued uncertainty and a wide range of potential outcomes. We continue to actively manage our response and assess impacts to our financial position and operating results, as well as mitigate adverse developments in our business. There continues to be uncertainty surrounding the pace, duration and extent of the COVID-19 pandemic and its related impacts — including vaccination efforts and new COVID-19 variants (including the delta and omicron variants) — on our results for 2022 and beyond. We believe that such financial results may continue to be impacted by, among other things, higher medical costs to treat those affected by the virus, vaccine-related costs, test reimbursement costs, lower risk adjustment revenue due to disrupted care impeding appropriate documentation of customer risk profiles in our Medicare Advantage plans, the pace at which costs return as well as the severity of costs for those who had previously deferred care, the potential for future deferral of care, lower customer volumes due to a disrupted employment market, or volatility in the economic markets.
For further information regarding the potential impact of COVID-19 on the Company, see "Risk Factors" contained in Part I, Item 1A of this Form 10-K.
Commentary: 2021 versus 2020
The commentary presented below, and in the segment discussions that follow, compare results for the year ended December 31, 2021 with results for the year ended December 31, 2020.
Shareholders' net income decreased, reflecting the absence of the gain on sale of the Group Disability and Life business reported in 2020, partially offset by higher adjusted income from operations.
Adjusted income from operations increased, primarily resulting from higher earnings in Evernorth and lower net interest expense. Improved results in our international businesses held for sale (reported in Other Operations) also contributed to the increase. These favorable effects were partially offset by lower earnings in Cigna Healthcare and the absence of earnings in 2021 from the sold Group Disability and Life business. The increase in earnings in the Evernorth segment was primarily attributable to continued contract affordability improvements and business growth (see "Evernorth Segment" section of this MD&A). Lower earnings in Cigna Healthcare were primarily driven by the unfavorable impacts of COVID-19, partially offset by higher net investment income (see "Cigna Healthcare Segment" section of this MD&A).
Medical customers grew, reflecting a higher customer base in Individual and Medicare Advantage, as well as our Middle Market, Select and International Health market segments, offset by a decline in customers in our National Accounts market segment.
Pharmacy revenues increased, reflecting inflation on branded drugs and higher claim volume, primarily due to our collaboration with Prime Therapeutics. See the "Evernorth Segment" section of this MD&A for further discussion of Pharmacy revenues.
Premiums were lower, reflecting the impact of the sale of the Group Disability and Life business. This effect was partially offset by an increase in Cigna Healthcare premiums resulting from customer growth in our insured businesses, higher premium rates due to anticipated underlying medical cost trend and the absence of premium relief programs implemented in the second quarter of 2020 in response to deferred care due to the COVID-19 pandemic.
55
Fees and other revenues increased, primarily driven by customer growth (see "Evernorth Segment" section of this MD&A).
Net investment income increased due to strong returns on our securities limited partnership investments, partially offset by lower average assets due to the sale of the Group Disability and Life business. See the "Investment Assets" section of this MD&A for further discussion.
Pharmacy and other service costs increased, reflecting inflation on branded drugs and higher claim volume, primarily due to our collaboration with Prime Therapeutics.
Medical costs and other benefit expenses increased, resulting from higher medical costs in Cigna Healthcare primarily driven by net unfavorable COVID-19 related impacts, underlying medical cost trend and customer growth in our insured business. These unfavorable effects were substantially offset by the impact of the sale of the Group Disability and Life business.
Selling, general and administrative expenses decreased, primarily reflecting the impact of the sale of the Group Disability and Life business, lower integration and transaction costs and the repeal of the health insurance industry tax. These favorable effects were partially offset by expense growth in Evernorth and Cigna Healthcare reflecting business growth.
Interest expense and other decreased primarily due to a lower average interest rate and lower levels of average outstanding debt resulting from debt repayments.
Debt extinguishment costs were lower because the debt repaid in 2021 had lower interest rates than the debt repaid in 2020.
Realized investment results improved, primarily due to gains on sales of real estate joint ventures in 2021, favorable market value adjustments on equity securities in 2021 compared with 2020 and lower credit loss reserves on debt securities. These favorable effects were partially offset by lower gains on sales of debt securities in 2021 compared with 2020.
Income tax expense decreased in 2021, reflecting the absence of taxes recorded in 2020 on the sale of the Group Disability and Life business. The consolidated effective tax rate decreased, primarily driven by the repeal of the nondeductible health insurance industry tax in 2021 and the absence of incremental tax expense associated with the sale of the Group Disability and Life business in 2020.
Commentary: 2020 vs 2019
Due to the segment changes made in 2021, the following commentary comparing consolidated 2020 results to 2019 is provided as an update to the commentary provided in our 2020 Form 10-K.
Shareholders' net income increased, driven by the gain on sale of the Group Disability and Life business, lower amortization of acquired intangible assets and higher adjusted income from operations, partially offset by the absence of earnings from transitioning clients.
Adjusted income from operations increased, driven in part by higher earnings in the Evernorth segment reflecting customer growth and increased script volumes and lower interest costs in Corporate due to a lower level of outstanding debt. These favorable effects were partially offset by lower earnings from the sold Group Disability and Life business (reported in Other Operations) primarily reflecting significantly elevated life claims related to the effects of COVID-19.
Medical customers decreased due to declines in the Middle Market and National Accounts market segments and increased disenrollment driven by the impacts of COVID-19. Those decreases were partially offset by growth in the Select and International Health market segments, as well as Medicare Advantage customers.
Pharmacy revenues increased, reflecting the transition of Cigna Healthcare's customers to Evernorth, higher claims volumes, driven by the Evernorth collaboration with Prime Therapeutics and increased prices, primarily due to inflation on branded drugs. These factors were substantially offset by the absence of revenues from the transitioning clients and, to a lesser extent, an increase in the generic fill rate. See the "Evernorth Segment" section of this MD&A for further discussion of pharmacy revenues.
Premiums increased, reflecting customer growth in insured products and rate increases reflecting expected medical cost inflation and the return of the health insurance industry tax. These factors were partially offset by the impact of premium relief programs implemented in response to significantly lower than historical utilization as customers deferred care in 2020 due to the COVID-19 pandemic.
56
Fees and other revenues decreased, primarily reflecting the transition of Cigna Healthcare's commercial customers to Evernorth's retail pharmacy network beginning in the third quarter of 2019 (see Note 3(J) to the Consolidated Financial Statements for further information).
Net investment income decreased, driven by lower yields, including lower income from partnership investments due to current economic conditions. These effects were partially offset by higher average assets.
Pharmacy and other service costs increased, reflecting the transition of Cigna Healthcare's customers to Evernorth, higher claims volumes, driven by the Evernorth collaboration with Prime Therapeutics and an increase in pricing, primarily due to inflation on branded drugs. These factors were substantially offset by the impact of the absence of the transitioning clients and, to a lesser extent, continued contract affordability improvements and the favorable impact of the mix of claims.
Medical costs and other benefit expenses increased, reflecting both customer growth and direct costs associated with COVID-19, partially offset by care deferrals in insured products in Cigna Healthcare and higher life claims in the sold Group Disability and Life business due to the effects of the COVID-19 pandemic.
Selling, general and administrative expenses were essentially flat, primarily reflecting lower charges in 2020 for the 2019 organizational efficiency plan and resolving our Affordable Care Act risk corridors claim against the United States Federal Government in the third quarter of 2020. These decreases were offset by the return of the health insurance industry tax.
Amortization of acquired intangible assets decreased, primarily reflecting lower amortization of customer-related intangibles associated with the transitioning clients.
Income tax expense increased for 2020, largely attributable to the sale of Cigna's Group Disability and Life business. The consolidated effective tax rate decreased slightly, driven by recognition of certain incremental federal and state tax benefits, largely offset by the return of the nondeductible health insurance industry tax.
Key Transactions and Business Developments
Organizational Efficiency Plan
As discussed in Note 15 to the Consolidated Financial Statements, during the fourth quarter of 2021, the Company approved a strategic plan to drive operational efficiencies. We believe this plan, coupled with the previously announced divestiture of the international life, accident and supplemental health benefits businesses (described below), will further leverage the Company's ongoing growth to drive operational efficiency through enhancements to organizational structure and increased use of automation and shared services. In connection with these plans, Cigna has updated its reporting segments to align with the new business reporting structure and recognized a charge in the fourth quarter of 2021 in the amount of $168 million, pre-tax ($119 million, after-tax). We expect to realize annualized after-tax savings of approximately $180 million. A substantial portion of the savings is expected to be realized in 2022. Although a substantial portion of the actions associated with these strategic steps have been reflected in the charge recognized in the fourth quarter of 2021, additional amounts are expected to be recorded in the second quarter of 2022 as we finalize our plans following the completion of the divestiture. See Note 15 for further information regarding our organizational efficiency charge.
Agreement to Sell International Life, Accident and Supplemental Benefits Businesses
We entered into a definitive agreement in October 2021 to sell our life, accident and supplemental benefits businesses in seven countries to Chubb INA Holdings, Inc. ("Chubb") for $5.75 billion cash (the "Chubb Transaction"). Subject to applicable regulatory approvals and customary closing conditions, we expect to complete the sale of our life, accident and supplemental benefits businesses in Hong Kong, Indonesia, New Zealand, South Korea, Taiwan, Thailand and our interest in a joint venture in Turkey in the second quarter of 2022. The "Liquidity and Capital Resources" section of this MD&A provides discussion of the expected impact of this transaction to liquidity.
Purchase of MDLIVE
As discussed in Note 4 to the Consolidated Financial Statements, on April 19, 2021 Cigna's Evernorth segment completed the acquisition of MDLIVE, Inc. ("MDLIVE"), a 24/7 virtual care platform (the "MDLIVE Acquisition"). The acquisition of MDLIVE will enable Evernorth to continue expanding access to virtual care and delivering a more affordable, convenient and connected care experience for consumers. The "Liquidity and Capital Resources" section of this MD&A provides discussion of the impact of the MDLIVE Acquisition on liquidity.
57
Sale of Group Disability and Life Business
As discussed in Note 4 to the Consolidated Financial Statements, Cigna sold its U.S. Group Disability and Life business to New York Life Insurance Company for $6.2 billion on December 31, 2020 (the "New York Life Divestiture"). The "Liquidity and Capital Resources" section of this MD&A provides discussion of the use of proceeds from the New York Life Divestiture.
Merger with Express Scripts
Cigna acquired Express Scripts on December 20, 2018. Costs related to this transaction are reported in "integration and transaction-related costs" as a special item and excluded from adjusted income from operations because they are not indicative of future underlying performance of the business. The integration of this acquisition has been completed.
On January 30, 2019, Anthem, Inc. ("Anthem"), a former client of Express Scripts, exercised its early termination right and terminated its pharmacy benefit management services agreement with us, effective March 1, 2019. There was a twelve-month transition period that ended March 1, 2020. We excluded the results of Express Scripts' contract with Anthem (and also Coventry Health Care, Inc.) from our non-GAAP reporting metrics adjusted revenues and adjusted income from operations for 2019 and refer to these clients as transitioning clients. As of December 31, 2019, the transition was substantially complete; therefore, beginning in 2020, we no longer exclude results of transitioning clients from our reported adjusted revenues and adjusted income from operations. Additionally, for the year ended December 31, 2020, we recorded an adjustment related to this contract that was excluded from adjusted revenues and adjusted income from operations.
Medicare Star Quality Ratings ("Star Ratings")
The Centers for Medicare & Medicaid Services ("CMS") uses a Star Rating system to measure how well Medicare Advantage ("MA") plans perform, scoring how well plans perform in several categories, including quality of care and customer service. Star Ratings range from one to five stars. CMS recognizes plans with Star Ratings of four stars or greater with quality bonus payments and the ability to offer enhanced benefits. Approximately 87% of our MA customers were in four star or greater plans for bonus payments received in 2021 and approximately 89% were in four star or greater plans for bonus payments to be received in 2022; we expect this percentage to decrease to 86% for bonus payments to be received in 2023 based upon the mix of new and existing MA plans.
Medicare Advantage ("MA") Rates
On January 15, 2021, CMS published the Calendar Year 2022 Medicare Advantage and Part D Rate Announcement (the "2022 Final Notice"), finalizing reimbursement rates for 2022. On February 2, 2022, CMS released the Calendar Year 2023 Advance Notice of Methodological Changes for Medicare Advantage Capitation Rates and Part C and Part D Payment Policies (the "Advance Notice"). We do not expect the new rates to have a material impact on our consolidated results of operations in 2022 or 2023. CMS will accept comments on the Advance Notice through March 4, 2022, before publishing the final rate announcement by April 4, 2022. The Advance Notice is subject to the required notice and comment period, and we cannot predict when or to what extent CMS will adopt the proposals in the Advance Notice.
58
LIQUIDITY AND CAPITAL RESOURCES
| (In millions) | ||||||||||||||||||||
| Financial Summary | 2021 | 2020 | 2019 | |||||||||||||||||
| Short-term investments | $ | 428 | $ | 359 | $ | 423 | ||||||||||||||
| Cash and cash equivalents | $ | 5,081 | $ | 10,182 | $ | 4,619 | ||||||||||||||
| Short-term debt | $ | 2,545 | $ | 3,374 | $ | 5,514 | ||||||||||||||
| Long-term debt | $ | 31,125 | $ | 29,545 | $ | 31,893 | ||||||||||||||
| Shareholders' equity | $ | 47,112 | $ | 50,321 | $ | 45,338 | ||||||||||||||
Liquidity
We maintain liquidity at two levels: the subsidiary level and the parent company level.
Cash requirements at the subsidiary level generally consist of:
•pharmacy, medical costs and other benefit payments;
•expense requirements, primarily for employee compensation and benefits, information technology and facilities costs;
•income taxes; and
•debt service.
Our subsidiaries normally meet their liquidity requirements by:
•maintaining appropriate levels of cash, cash equivalents and short-term investments;
•using cash flows from operating activities;
•matching investment durations to those estimated for the related insurance and contractholder liabilities;
•selling investments; and
•borrowing from affiliates, subject to applicable regulatory limits.
Cash requirements at the parent company level generally consist of:
•debt service;
•payment of declared dividends to shareholders;
•lending to subsidiaries as needed; and
•pension plan funding.
The parent company normally meets its liquidity requirements by:
•maintaining appropriate levels of cash and various types of marketable investments;
•collecting dividends from its subsidiaries;
•using proceeds from issuing debt and common stock; and
•borrowing from its subsidiaries, subject to applicable regulatory limits.
Dividends from our insurance, Health Maintenance Organization ("HMO") and certain foreign subsidiaries are subject to regulatory restrictions. See Note 20 to the Consolidated Financial Statements in this Form 10-K for additional information regarding these restrictions. Most of the Evernorth segment operations are not subject to regulatory restrictions regarding dividends and therefore provide significant financial flexibility to Cigna.
59
Cash flows for the years ended December 31 were as follows:
| (In millions) | 2021 | 2020 | 2019 | |||||||||||||||||
| Net cash provided by operating activities | $ | 7,191 | $ | 10,350 | $ | 9,485 | ||||||||||||||
| Net cash (used in) provided by investing activities: | ||||||||||||||||||||
| Cash proceeds from sale of U.S. Group Disability and Life business, net of cash sold | (61) | 5,592 | — | |||||||||||||||||
| Other acquisitions | (1,833) | (139) | (153) | |||||||||||||||||
| Net investment sales (purchases) | (660) | (1,406) | 480 | |||||||||||||||||
| Purchases of property and equipment, net | (1,154) | (1,094) | (1,050) | |||||||||||||||||
| Other, net | 97 | 23 | (11) | |||||||||||||||||
| Net investing activities | (3,611) | 2,976 | (734) | |||||||||||||||||
| Net cash (used in) financing activities: | ||||||||||||||||||||
| Debt (repayments) issuances | 521 | (4,736) | (5,175) | |||||||||||||||||
| Stock repurchase | (7,742) | (4,042) | (1,987) | |||||||||||||||||
| Dividend payments | (1,341) | (15) | (15) | |||||||||||||||||
| Other, net | 350 | 260 | (10) | |||||||||||||||||
| Net financing activities | (8,212) | (8,533) | (7,187) | |||||||||||||||||
| Foreign currency effect on cash | (65) | 41 | (8) | |||||||||||||||||
| Change in cash, cash equivalents and restricted cash | $ | (4,697) | $ | 4,834 | $ | 1,556 | ||||||||||||||
The following discussion explains variances in the various categories of cash flows for the year ended December 31, 2021 compared with the year ended December 31, 2020. For comparisons of liquidity and capital resources for the year ended December 31, 2020 compared with the year ended December 31, 2019, please refer to the previously filed MD&A included in Part II, Item 7 of our Form 10-K for the year ended December 31, 2020.
Operating activities
Cash flows from operating activities consist principally of cash receipts and disbursements for pharmacy revenues and costs, premiums, fees, investment income, taxes, benefit costs and other expenses.
Cash provided by operating activities decreased, driven by increases in accounts receivable due to higher pharmacy claim volume and business growth and a delay in the annual CMS Part D settlement, the timing of pharmacy and other service cost payables as well as higher tax payments largely related to the sale of the Group Disability and Life business. These decreases were partially offset by the absence of the health insurance industry tax payments.
Investing and Financing activities
Cash used in investing activities increased, primarily due to the acquisition of MDLIVE in 2021, the absence of the net proceeds from the sale of the Group Disability and Life business in 2020, partially offset by lower net investment activities.
Cash used in financing activities decreased primarily due to lower debt repayments, offset by higher stock repurchases including shares purchased pursuant to the ASR agreements (described below) and an increase in dividends paid.
Capital Resources
Our capital resources consist primarily of cash, cash equivalents and investments maintained at regulated subsidiaries required to underwrite insurance risks, cash flows from operating activities, our commercial paper program, credit agreements and the issuance of long-term debt and equity securities. Our businesses generate significant cash flow from operations, some of which is subject to regulatory restrictions relative to the amount and timing of dividend payments to the parent company. Dividends from U.S. regulated subsidiaries were $2.8 billion and $2.3 billion for the years ended December 31, 2021 and 2020, respectively. Non-regulated subsidiaries also generate significant cash flow from operating activities, which is typically available immediately to the parent company for general corporate purposes.
60
We prioritize our use of capital resources to:
•Invest in capital expenditures, primarily related to technology to support innovative solutions for our customers, provide the capital necessary to maintain or improve the financial strength ratings of subsidiaries and to repay debt and fund pension obligations if necessary;
•pay dividends to shareholders;
•consider acquisitions that are strategically and economically advantageous; and
•return capital to shareholders through share repurchases.
Funds Available
Commercial Paper Program. Cigna maintains a commercial paper program and may issue short-term, unsecured commercial paper notes privately placed on a discount basis through certain broker dealers at any time not to exceed an aggregate amount of $5.0 billion. The net proceeds of issuances have been and are expected to be used for general corporate purposes.
Revolving Credit Agreements. Our revolving credit agreements provide us with the ability to borrow amounts for general corporate purposes, including for the purpose of providing liquidity support if necessary under our commercial paper program discussed above.
Cigna's revolving credit agreements include: a $3.0 billion five-year revolving credit and letter of credit agreement that expires in April 2026; a $1.0 billion three-year revolving credit agreement that expires in April 2024; and a $1.0 billion 364-day revolving credit agreement that expires in April 2022.
As of December 31, 2021, we had $5.0 billion of undrawn committed capacity under our revolving credit agreements (these amounts are available for general corporate purposes, including providing liquidity support for our commercial paper program), $3.0 billion of remaining capacity under our commercial paper program and $5.5 billion in cash and short-term investments, approximately $1.7 billion of which was held by the parent company or certain non-regulated subsidiaries.
See Note 7 to the Consolidated Financial Statements for further information on our credit agreements and commercial paper program.
At December 31, 2021, our debt-to-capitalization ratio was 41.7%, an increase from 39.5% at December 31, 2020, reflecting higher commercial paper balances and the impact of share repurchase on shareholders' equity.
We actively monitor our debt obligations and engage in issuance or redemption activities as needed in accordance with our capital management strategy.
Subsidiary Borrowings. In addition to the sources of liquidity discussed above, the parent company can borrow an additional $2.0 billion from its subsidiaries without further approvals as of December 31, 2021.
Use of capital resources
Capital Expenditures. Capital expenditures for property, equipment and computer software were $1.2 billion in 2021 compared to $1.1 billion in 2020. We expect to continue to invest in technology that we believe will drive future growth. Anticipated capital expenditures will be funded primarily from operating cash flow.
Dividends. For 2021, Cigna declared and paid quarterly cash dividends of $1.00 per share of Cigna common stock. See Note 8 to the Consolidated Financial Statements for further information on our dividend payments. On February 3, 2022, the Board of Directors declared and increased the quarterly cash dividend to $1.12 per share of Cigna common stock to be paid on March 24, 2022 to shareholders of record on March 9, 2022. Cigna currently intends to pay regular quarterly dividends, with future declarations subject to approval by its Board of Directors and the Board's determination that the declaration of dividends remains in the best interests of Cigna and its shareholders. The decision of whether to pay future dividends and the amount of any such dividends will be based on the Company's financial position, results of operations, cash flows, capital requirements, the requirements of applicable law and any other factors the Board of Directors may deem relevant.
Acquisition. In April 2021, Cigna completed its acquisition of MDLIVE, which was funded with cash on hand and commercial paper borrowings. See Note 4 to the Consolidated Financial Statements for additional information.
Share repurchases. We maintain a share repurchase program authorized by our Board of Directors, under which we may repurchase shares of our common stock from time to time. The timing and actual number of shares repurchased will depend on a variety of factors including price, general business and market conditions and alternate uses of capital. The share repurchase program may be effected through open market purchases in compliance with Rule 10b-18 under the Securities Exchange Act of 1934, as amended, including through Rule 10b5-1 trading plans or privately negotiated transactions. The program may be suspended or discontinued at any time.
61
On August 23, 2021, as part of our existing share repurchase program, we entered into accelerated share repurchase agreements to repurchase $2.0 billion of common stock. The total number of shares repurchased under the ASR agreements was 9.5 million. See Note 8 to the Consolidated Financial Statements for additional information.
For the year ended December 31, 2021, we repurchased 35.2 million shares for approximately $7.7 billion including the $2.0 billion paid under the ASR agreements. From January 1, 2022 through February 23, 2022, we repurchased 5.0 million shares for approximately $1.2 billion. Share repurchase authority was $6.0 billion as of February 23, 2022.
Pension liability. As of December 31, 2021, our unfunded pension liability was $377 million, a decrease of $600 million from December 31, 2020, primarily attributable to strong investment asset returns and an increase in discount rates of 33 basis points. In 2021, we made immaterial contributions to the qualified pension plans as required under the Pension Protection Act of 2006 and we expect the required contributions for 2022 to be immaterial. See Note 16 to the Consolidated Financial Statements for additional information.
Divestitures
Group Disability and Life Sale. In connection with the sale of this business that closed on December 31, 2020, we deployed approximately $3.0 billion to debt repayment by: (i) repaying in full our $1.4 billion 364-Day Term Loan Credit Agreement entered into on April 1, 2020, on December 31, 2020; (ii) redeeming in full the $1.0 billion aggregate principal amount of Cigna's Senior Floating Rate Notes due 2021 on January 15, 2021 at a redemption price calculated in accordance with the terms and conditions of the indenture governing the Notes; and (iii) repaying certain balances of our outstanding commercial paper in January 2021.
Sale of life, accident and supplemental benefits businesses in seven countries. Cigna entered into a definitive agreement in October 2021 to sell its life, accident and supplemental benefits businesses in seven countries to Chubb for $5.75 billion cash. Subject to applicable regulatory approvals and customary closing conditions, we expect to complete the sale of our life, accident and supplemental benefits businesses in Hong Kong, Indonesia, New Zealand, South Korea, Taiwan, Thailand and our interest in a joint venture in Turkey in the second quarter of 2022. Cigna estimates it will receive approximately $5.4 billion of net after-tax proceeds from this transaction and expects to utilize the after-tax proceeds from the transaction primarily for share repurchases.
Risks to our liquidity and capital resources outlook include cash projections that may not be realized and the demand for funds could exceed available cash if our ongoing businesses experience unexpected shortfalls in earnings or we experience material adverse effects from one or more risks or uncertainties described more fully in the "Risk Factors" section of this Form 10-K. Though we believe we have adequate sources of liquidity, significant disruption or volatility in the capital and credit markets could affect our ability to access those markets for additional borrowings or increase costs.
Guarantees and Contractual Obligations
We are contingently liable for various contractual obligations and financial and other guarantees entered into in the ordinary course of business. See Note 22 to the Consolidated Financial Statements for discussion of various guarantees.
On balance sheet:
•Insurance liabilities
◦Insurance liabilities inclusive of the businesses held for sale are $21.5 billion, which include contractholder deposit funds, future policy benefits and unpaid claims and claim expenses.
◦Of the total obligation amount, $4.3 billion of insurance liabilities are associated with the sold retirement benefits, individual life insurance and annuity businesses, as well as the group life and personal accident businesses as their related net cash flows are not expected to impact our cash flows.
◦The $22.3 billion of total obligations exceeds the corresponding insurance and contractholder liabilities of $17.3 billion recorded on the balance sheet. This is because some of the recorded insurance liabilities reflect discounting for interest and the recorded contractholder liabilities exclude future interest crediting, charges and fees. The timing and amount of actual future cash flows may differ from the projected amount disclosed.
◦We expect $5.2 billion of insurance liabilities to be paid within the next twelve months beginning January 1, 2022.
◦See Note 9 to the Consolidated Financial Statements for information regarding insurance liabilities.
•Long-term debt
◦Total scheduled payments on long-term debt are $48.2 billion, which include scheduled interest payments and maturities of long-term debt.
◦We expect $1.7 billion of long-term debt payments, which include scheduled interest payments and current maturities of long-term debt to be paid within the next twelve months beginning January 1, 2022.
62
◦Finance leases are included in long-term debt and primarily represent obligations for information technology network storage, servers and equipment. See Note 19 to the Consolidated Financial Statements for information regarding finance leases.
◦See Note 7 to the Consolidated Financial Statements for information regarding principal maturities of long-term debt.
•Other noncurrent liabilities
◦These include approximately $704 million of estimated payments for guaranteed minimum income benefit ("GMIB") contracts (without considering any related reinsurance arrangements), other postretirement and postemployment benefit obligations, pension, supplemental and deferred compensation plans, interest rate and foreign currency swap contracts and reinsurance liabilities.
◦We expect $121 million of other noncurrent liabilities to be paid within the next twelve months beginning January 1, 2022.
◦See Note 16 to the Consolidated Financial Statements for further information on pension obligations.
•Operating leases
◦These include operating lease payments of $641 million.
◦We expect $152 million of operating lease payments to be due within the next twelve months beginning January 1, 2022.
◦See Note 19 to the Consolidated Financial Statements for additional information.
•Uncertain Tax Positions
◦In the event we are unable to sustain all of our $1.2 billion of uncertain tax positions, it could result in future tax payments of approximately $900 million. We cannot reasonably estimate the timing of such future payments.
◦See Note 21 to the Consolidated Financial Statements for additional information on uncertain tax positions.
Off-balance sheet:
•Purchase obligations
◦These include agreements to purchase goods or services that are enforceable and legally binding. Purchase obligations exclude contracts that are cancellable without penalty and those that do not contractually require minimum levels of goods or services to be purchased.
◦As of December 31, 2021, purchase obligations consisted of a total of $4.3 billion of estimated payments required under contractual arrangements. This includes:
▪$3.4 billion of investment commitments, primarily comprised of other-long-term investments and equity securities.
▪$932 million of future service commitments, primarily comprised of contracts for certain outsourced businesses process and information technology maintenance and support.
◦We expect $2.0 billion of purchase obligations to be paid within the next twelve months beginning January 1, 2022, of which $1.6 billion relates to investment commitments and $368 million relates to future service commitments.
◦See Note 11 of the Consolidated Financial Statements for additional information on investment commitments.
CRITICAL ACCOUNTING ESTIMATES
The preparation of Consolidated Financial Statements in accordance with GAAP requires management to make estimates and assumptions that affect reported amounts and related disclosures in the Consolidated Financial Statements. Management considers an accounting estimate to be critical if:
•it requires assumptions to be made that were uncertain at the time the estimate was made; and
•changes in the estimate or different estimates that could have been selected could have a material effect on our consolidated results of operations or financial condition.
Management has discussed how critical accounting estimates are developed and selected with the Audit Committee of our Board of Directors and the Audit Committee has reviewed the disclosures presented in this Form 10-K. We regularly evaluate items that may impact critical accounting estimates.
In addition to the estimates presented in the following tables, the Notes to the Consolidated Financial Statements describe other estimates that management has made in preparation of the financial statements. Management believes the current assumptions used to estimate amounts reflected in our Consolidated Financial Statements are appropriate. However, if actual experience significantly differs from the assumptions used in estimating amounts reflected in our Consolidated Financial Statements, the resulting changes could have a material adverse effect on our consolidated results of operations and in certain situations, could have a material adverse effect on liquidity and our financial condition. The tables below present the adverse impacts of certain possible changes in assumptions. The effect of assumption changes in the opposite direction would be a positive impact to our consolidated results of
63
operations, liquidity or financial condition, except for assessing impairment of goodwill.
| Balance Sheet Caption / Nature of Critical Accounting Estimate | Effect if Different Assumptions Used | ||||
Goodwill and other intangible assets Goodwill represents the excess of the cost of businesses acquired over the fair value of their net assets at the acquisition date. Intangible assets primarily reflect the value of customer relationships and other intangibles acquired in business combinations. Fair values of reporting units are estimated based on discounted cash flow analysis and market approach models using assumptions that we believe a hypothetical market participant would use to determine a current transaction price. The significant assumptions and estimates used in determining fair value primarily include the discount rate and future cash flows. A discount rate is selected to correspond with each reporting unit's weighted average cost of capital, consistent with that used for investment decisions considering the specific and detailed operating plans and strategies within each reporting unit. Projections of future cash flows differ by reporting unit and are consistent with our ongoing strategy and projection processes. Future cash flows for Evernorth are primarily driven by the forecasted gross margins of the business, as well as operating expenses and long-term growth rates. Future cash flows for our other reporting units are primarily driven by forecasted revenues, benefit expenses, operating expenses and long-term growth rates. The fair value of intangibles and the amortization method were determined using an income approach that relies on projected future cash flows including key assumptions for customer attrition and discount rates. Management revises amortization periods if it believes there has been a change in the length of time that an intangible asset will continue to have value. Our U.S. Government reporting unit contracts with CMS to provide managed health care services, including Medicare Advantage and Medicare-approved prescription drug plans. Estimated future cash flows for this reporting unit's Medicare Advantage business incorporate the current reimbursement structure for 2022 and beyond. Revenues from the Medicare programs are dependent, in whole or in part, upon annual funding from the federal government through CMS. Funding levels for these programs are dependent on many factors including changes to the risk adjustment payment methodology, government efforts to contain health care costs, budgetary constraints and general political issues and priorities. The Company conducts its quantitative evaluation for goodwill impairment at least annually during the third quarter at the reporting unit level and performs qualitative impairment assessments on a quarterly basis to determine if events or changes in circumstances indicate that it is more likely than not that the carrying value of a reporting unit exceeds its estimated fair value. Goodwill and other intangibles as of December 31 were as follows (in millions): ·2021 – Goodwill $45,811; Other intangible assets $34,102 ·2020 – Goodwill $44,648; Other intangible assets $35,179 See Note 18 to the Consolidated Financial Statements for additional discussion of our goodwill and other intangible assets. | We completed our normal annual evaluations for impairment of goodwill and intangible assets during the third quarter of 2021. The evaluations indicated that the fair value estimates of our reporting units exceed their carrying values by significant margins. Changes in assumptions concerning future financial results or other underlying assumptions, including macroeconomic factors, government legislation, changes in the competitive landscape or other market conditions could impact our ability to achieve profitability projections. If we consistently do not achieve our earnings and cash flow projections or our cost of capital rises significantly, the assumptions and estimates underlying the goodwill and intangible asset impairment evaluations could be adversely affected and result in future impairment charges that would negatively impact our operating results and financial position. Specific to the U.S. Government reporting unit, in 2021 we experienced elevated medical claims and lower risk adjustment revenues primarily due to the COVID-19 pandemic. If these factors were to worsen or continue beyond our current expectations, profitability could be further impacted and significantly reduce the fair value of this reporting unit. | ||||
64
| Balance Sheet Caption / Nature of Critical Accounting Estimate | Effect if Different Assumptions Used | ||||
Income taxes – uncertain tax positions We evaluate tax positions to determine whether the benefits are more likely than not to be sustained on audit based on their technical merits. The Company establishes a liability if the probability that the position will be sustained is 50% or less. For uncertain positions that management believes are more likely than not to be sustained, the Company recognizes a liability based upon management's estimate of the most likely settlement outcome with the taxing authority. These amounts primarily relate to federal and state uncertain positions of the value and timing of deductions and uncertain positions of attributing taxable income to states Balances that are included in the Consolidated Balance Sheets are as follows (in millions): ·2021 – $1,230 ·2020 – $1,210 See Note 21 to the Consolidated Financial Statements for additional discussion around uncertain tax positions and the Liquidity and Capital Resources section of this MD&A for a discussion of their potential impact on liquidity. | The factors that could impact our estimates of uncertain tax positions include the likelihood of being sustained upon audit based on the technical merits of the tax position and related assumed interest and penalties. If our positions are upheld upon audit, our net income would increase. | ||||
| Balance Sheet Caption / Nature of Critical Accounting Estimate | Effect if Different Assumptions Used | ||||
Unpaid claims and claim expenses – Cigna Healthcare Unpaid claims and claim expenses include both reported claims and estimates for losses incurred but not yet reported. Unpaid claims and claim expenses in Cigna Healthcare are primarily impacted by assumptions related to completion factors and medical cost trend. Variation of actual results from either assumption could impact the unpaid claims balance as noted below. A large number of factors may cause the medical cost trend to vary from the Company's estimates, including: changes in health management practices, changes in the level and mix of benefits offered and services utilized and changes in medical practices. Completion factors may be affected if actual claims submission rates from providers differ from estimates (that can be influenced by a number of factors, including provider mix and electronic versus manual submissions), or if changes to the Company's internal claims processing patterns occur. Unpaid claims and claim expenses for the Cigna Healthcare segment as of December 31 were as follows (in millions): ·2021 – gross $4,261; net $4,000 ·2020 – gross $3,695; net $3,458 These liabilities are presented above both gross and net of reinsurance and other recoverables. See Note 9 to the Consolidated Financial Statements for additional information regarding assumptions and methods used to estimate this liability. | Based on studies of our claim experience, it is reasonably possible that a 100 basis point change in the medical cost trend and a 50 basis point change in completion factors could occur in the near term. A 100 basis point increase in the medical cost trend rate would increase this liability by approximately $60 million, resulting in a decrease in net income of approximately $50 million after-tax, and a 50 basis point decrease in completion factors would increase this liability by approximately $125 million, resulting in a decrease in net income of approximately $100 million after-tax. | ||||
65
Balance Sheet Caption / Nature of Critical Accounting Estimate | Effect if Different Assumptions Used | ||||
Valuation of debt security investments Most debt securities are classified as available for sale and are carried at fair value with changes in fair value recorded in accumulated other comprehensive income (loss) within shareholders' equity. Fair value is defined as the price at which an asset could be exchanged in an orderly transaction between market participants at the balance sheet date. Determining fair value for a financial instrument requires management judgment. The degree of judgment involved generally correlates to the level of pricing readily observable in the markets. Financial instruments with quoted prices in active markets or with market observable inputs to determine fair value, such as public securities, generally require less judgment. Conversely, private placements including more complex securities that are traded infrequently are typically measured using pricing models that require more judgment as to the inputs and assumptions used to estimate fair value. There may be a number of alternative inputs to select based on an understanding of the issuer, the structure of the security and overall market conditions. In addition, these factors are inherently variable in nature as they change frequently in response to market conditions. Approximately two-thirds of our debt securities are public securities and one-third are private placement securities. Typically, the most significant input in the measurement of fair value is the market interest rate used to discount the estimated future cash flows of the instrument. Such market rates are derived by calculating the appropriate spreads over comparable U.S. Treasury securities, based on the credit quality, industry and structure of the asset. See Notes 11A. and 12 to the Consolidated Financial Statements for a discussion of our fair value measurements, the procedures performed by management to determine that the amounts represent appropriate estimates and our accounting policy regarding unrealized appreciation on debt securities. | If the derived interest rates used to calculate fair value increased by 100 basis points, the fair value of the total debt security portfolio of $17 billion would decrease by approximately $1.3 billion, resulting in an after-tax decrease to shareholders' equity of approximately $0.7 billion as of December 31, 2021. | ||||
66
SEGMENT REPORTING
The following section of this MD&A discusses the results of each of our segments.
Cigna entered into a definitive agreement in October 2021 to sell its life, accident and supplemental benefits businesses in seven countries to Chubb for $5.75 billion cash. In connection with the pending Chubb Transaction, we revised our business reporting structure. As such, we adjusted our segment reporting effective in the fourth quarter of 2021 so that the results previously reported in the International Markets segment are now reported as follows:
•The businesses to be retained by Cigna are now reported in the newly created International Health operating segment that will be aggregated with our existing U.S. Commercial and U.S. Government operating segments in the renamed Cigna Healthcare reporting segment (previously named U.S. Medical).
•The businesses to be sold pursuant to the Chubb Transaction are now reported in Other Operations.
See Note 1 to the Consolidated Financial Statements for further description of our segments.
In segment discussions, we present "adjusted revenues" and "pre-tax adjusted income (loss) from operations," defined as income (loss) before income taxes excluding net realized investment results, amortization of acquired intangible assets, results of transitioning clients prior to 2020 and special items. Cigna's share of certain realized investment results of its joint ventures reported in the Cigna Healthcare segment using the equity method of accounting are also excluded. Special items are matters that management believes are not representative of the underlying results of operations due to their nature or size. Ratios presented in this segment discussion exclude the same items as adjusted revenues and pre-tax adjusted income (loss) from operations. See Note 23 to the Consolidated Financial Statements for additional discussion of these metrics and a reconciliation of income before income taxes to pre-tax adjusted income from operations, as well as a reconciliation of total revenues to adjusted revenues. Note 23 to the Consolidated Financial Statements also explains that segment revenues include both external revenues and sales between segments that are eliminated in Corporate.
In these segment discussions, we also present "pre-tax adjusted margin," defined as pre-tax adjusted income (loss) from operations divided by adjusted revenues.
See the "Executive Overview" section of this MD&A for summarized financial results of each of our segments.
Evernorth Segment
Evernorth includes a broad range of coordinated and point solution health services and capabilities, as well as those from partners across the healthcare system, in pharmacy solutions, benefits management solutions, care delivery and care management solutions and intelligence solutions. As described in the introduction to Segment Reporting, Evernorth's performance is measured using adjusted revenues and pre-tax adjusted income from operations.
The key factors that impact Evernorth's pharmacy revenues and pharmacy and other service costs are volume, mix of claims and price. These key factors are discussed further below. See Note 2 to the Consolidated Financial Statements included in this Form 10-K for additional information on revenue and cost recognition policies for this segment.
•As our clients' claim volumes increase or decrease, our resulting revenues and cost of revenues correspondingly increase or decrease. Our gross profit could also increase or decrease as a result of changes in purchasing discounts.
•The mix of claims generally considers the type of drug and distribution method used for dispensing and fulfilling. Types of drugs can have an impact on our pharmacy revenues, pharmacy and other service costs and gross profit, including amounts payable under certain financial and performance guarantees with our clients. In addition to the types of drugs, the mix of generic claims (i.e., generic fill rate) also impacts our gross profit. Generally, higher generic fill rates reduce revenues, as generic drugs are typically priced lower than the branded drugs they replace. However, as ingredient cost paid to pharmacies on generic drugs is incrementally lower than the price charged to our clients, higher generic fill rates generally have a favorable impact on our gross profit. The home delivery generic fill rate is currently lower than the network generic fill rate as fewer generic substitutions are available among maintenance medications (such as therapies for chronic conditions) commonly dispensed from home delivery pharmacies as compared to acute medications that are primarily dispensed by pharmacies in our retail networks. Furthermore, our gross profit differs among network, home delivery and specialty distribution methods and can impact our profitability.
•Our client contract pricing is impacted by our ongoing ability to negotiate favorable contracts for pharmacy network, pharmaceutical and wholesaler purchasing and manufacturer rebates. As we seek to improve the effectiveness of our
67
integrated solutions for the benefit of our clients, we are continuously innovating and improving affordability. Our gross profit could also increase or decrease as a result of drug purchasing contract initiatives implemented. Inflation also impacts our pricing because most of our contracts provide that we bill clients and pay pharmacies based on a generally recognized price index for pharmaceuticals. Therefore, the rate of inflation for prescription drugs and our efforts to manage this inflation for our clients continues to be a significant driver of our revenues and cost of revenues in the current environment.
In this MD&A, we present revenues and gross profit, as well as adjusted revenues and adjusted gross profit, consistent with our segment reporting metrics, which exclude special items and, for periods prior to 2020, contributions from transitioning clients. As of December 31, 2019, the transition of these clients was substantially complete; therefore, beginning in 2020, we no longer exclude results of transitioning clients from our adjusted metrics. Additionally, for the year ended December 31, 2020, we recorded an adjustment related to a former client contract that was excluded from our adjusted metrics. See the "Key Transactions and Business Developments" section of this Form 10-K MD&A for further discussion of transitioning clients and why we present this information.
Results of Operations
| Financial Summary | For the Years Ended December 31, | Change Favorable (Unfavorable) | Change Favorable (Unfavorable) | ||||||||||||||||||||||||||||||||||||||||||||
| (Dollars in millions) | 2021 | 2020 | 2019 | 2021 vs. 2020 | 2020 vs. 2019 | ||||||||||||||||||||||||||||||||||||||||||
| Total revenues | $ | 131,912 | $ | 116,334 | $ | 109,794 | $ | 15,578 | 13 | % | $ | 6,540 | 6 | % | |||||||||||||||||||||||||||||||||
| Less: Transitioning clients | — | — | (13,347) | — | N/M | 13,347 | N/M | ||||||||||||||||||||||||||||||||||||||||
| Less: Contractual adjustment for a former client | — | (204) | — | 204 | N/M | (204) | N/M | ||||||||||||||||||||||||||||||||||||||||
Adjusted revenues (1) | $ | 131,912 | $ | 116,130 | $ | 96,447 | $ | 15,782 | 14 | % | $ | 19,683 | 20 | % | |||||||||||||||||||||||||||||||||
| Gross profit | $ | 8,408 | $ | 7,797 | $ | 8,908 | $ | 611 | 8 | % | $ | (1,111) | (12) | % | |||||||||||||||||||||||||||||||||
Adjusted gross profit (1) | $ | 8,408 | $ | 7,593 | $ | 6,984 | $ | 815 | 11 | % | $ | 609 | 9 | % | |||||||||||||||||||||||||||||||||
| Pre-tax adjusted income from operations | $ | 5,818 | $ | 5,363 | $ | 5,092 | $ | 455 | 8 | % | $ | 271 | 5 | % | |||||||||||||||||||||||||||||||||
| Pre-tax adjusted margin | 4.4 | % | 4.6 | % | 5.3 | % | (20) | bps | (70) | bps | |||||||||||||||||||||||||||||||||||||
Adjusted expense ratio (2) | 1.9 | % | 1.9 | % | 2.0 | % | – | bps | (10) | bps | |||||||||||||||||||||||||||||||||||||
| For the Years Ended December 31, | Change Favorable (Unfavorable) | Change Favorable (Unfavorable) | |||||||||||||||||||||||||||||||||
| (Dollars and adjusted scripts in millions) | 2021 | 2020 | 2019 | 2021 vs. 2020 | 2020 vs. 2019 | ||||||||||||||||||||||||||||||
Selected Financial Information (1) | |||||||||||||||||||||||||||||||||||
| Pharmacy revenue by distribution channel | |||||||||||||||||||||||||||||||||||
| Adjusted network revenues | $ | 64,992 | $ | 56,181 | $ | 41,483 | 16 | % | 35 | % | |||||||||||||||||||||||||
| Adjusted home delivery and specialty revenues | 54,391 | 49,886 | 45,836 | 9 | % | 9 | % | ||||||||||||||||||||||||||||
| Other pharmacy revenues | 6,428 | 5,403 | 4,900 | 19 | % | 10 | % | ||||||||||||||||||||||||||||
| Total adjusted pharmacy revenues | $ | 125,811 | $ | 111,470 | $ | 92,219 | 13 | % | 21 | % | |||||||||||||||||||||||||
| Adjusted fees and other revenues | 6,084 | 4,628 | 4,168 | 31 | % | 11 | % | ||||||||||||||||||||||||||||
| Net investment income | 17 | 32 | 60 | (47) | % | (47) | % | ||||||||||||||||||||||||||||
| Adjusted revenues | $ | 131,912 | $ | 116,130 | $ | 96,447 | 14 | % | 20 | % | |||||||||||||||||||||||||
| Pharmacy script volume | |||||||||||||||||||||||||||||||||||
Adjusted network scripts (3) | 1,355 | 1,206 | 941 | 12 | % | 28 | % | ||||||||||||||||||||||||||||
Adjusted home delivery and specialty scripts (3) | 283 | 287 | 283 | (1) | % | 1 | % | ||||||||||||||||||||||||||||
Total adjusted scripts (3) | 1,638 | 1,493 | 1,224 | 10 | % | 22 | % | ||||||||||||||||||||||||||||
Generic fill rate (4) | |||||||||||||||||||||||||||||||||||
| Network | 85.4 | % | 87.4 | % | 87.1 | % | (200) | bps | 30 | bps | |||||||||||||||||||||||||
| Home delivery | 85.9 | % | 85.2 | % | 84.3 | % | 70 | bps | 90 | bps | |||||||||||||||||||||||||
| Overall generic fill rate | 85.5 | % | 87.2 | % | 86.8 | % | (170) | bps | 40 | bps | |||||||||||||||||||||||||
(1)Amounts exclude special items and for periods prior to 2020, contributions from transition clients for the year ended December 31, 2019.
(2)Adjusted expense ratio is calculated as selling, general and administrative expense excluding contributions from transition clients for the year ended December 31, 2019 as a percentage of adjusted revenues.
(3)Non-specialty network scripts filled through 90-day programs and home delivery scripts are multiplied by three. All other network and specialty scripts are counted as one script.
(4)Generic fill rate is defined as the total number of generic scripts divided by the total overall scripts filled.
68
2021 versus 2020
Adjusted network revenues increased, reflecting increased prices, due to inflation on branded drugs and higher claims volume, primarily due to our collaboration with Prime Therapeutics. These increases were partially offset by claims mix due to an increase in the generic fill rate after excluding the impact of COVID-19 vaccines.
Adjusted home delivery and specialty revenues increased, reflecting higher specialty claims volume due in part to our collaboration with Prime Therapeutics, as well as increased prices, primarily due to inflation on branded drugs. These increases were partially offset by slightly lower home delivery claims volume.
Other pharmacy revenues increased, reflecting higher volume from our CuraScript Specialty Distribution business.
Adjusted fees and other revenues increased, reflecting customer growth from our services supporting benefits management solutions, including customer growth from certain fee based contractual arrangements and the acquisition of MDLIVE.
Adjusted gross profit and pre-tax adjusted income from operations increased, reflecting continued contract affordability improvements and business growth. Pre-tax adjusted income from operations increase was partially offset by strategic investments in expanding partnerships, new businesses and solutions, and digital technology.
The expense ratio was flat reflecting higher revenues as well as increased strategic investments in expanding partnerships, new businesses and solutions, and digital technology in the year ended December 31, 2021 offset by increased operating expenses due to client transitions in the year ended December 31, 2020.
2020 versus 2019
In the first quarter of 2020, U.S. Government operating segment customers transitioned to Express Scripts' retail pharmacy network. In the third quarter of 2019, U.S. Commercial operating segment customers transitioned to Express Scripts' retail pharmacy network.
Adjusted network revenues increased, reflecting the transition of Cigna Healthcare's customers, higher claims volume due to our collaboration with Prime Therapeutics and increased prices due to inflation on branded drugs. These favorable effects were partially offset by claims mix due to the increase in the generic fill rate.
Adjusted home delivery and specialty revenues increased, reflecting higher prices, due to inflation on branded drugs and higher home delivery and specialty claims volume. These increases were partially offset by claims mix due to an increase in the generic fill rate.
Adjusted gross profit and pre-tax adjusted income from operations increased, reflecting customer growth, higher adjusted pharmacy scripts volumes, continued contract affordability improvements and the favorable impact of claims mix as a result of the types of drugs dispensed, the distribution method used for dispensing and fulfilling and an increase in the generic fill rate. Pre-tax adjusted income from operations increase was partially offset by an increase in operating expenses due to client transitions.
The expense ratio was lower, reflecting higher revenues and increased operating expenses due to client transitions.
Cigna Healthcare Segment
Cigna Healthcare includes Cigna's U.S. Commercial, U.S. Government and International Health businesses, which provide comprehensive medical and coordinated solutions to clients and customers to support whole-person health needs. U.S. Commercial products and services include medical, pharmacy, behavioral health, dental, vision, health advocacy programs and other products and services for insured and self-insured customers. U.S. Government solutions include Medicare Advantage, Medicare Supplement and Medicare Part D plans for seniors and individual health insurance plans both on and off the public exchanges. International Health solutions include health care coverage in our international markets, as well as health care benefits for globally mobile individuals and employees of multinational organization. The Cigna Healthcare segment is comprised of the previously named U.S. Medical segment and the businesses to be retained from the previous International Markets segment. The addition of International Health to the Cigna Healthcare segment did not have a material impact on the business drivers which contributed to changes in results of operations when comparing 2020 to 2019. As described in the introduction to Segment Reporting, performance of the Cigna Healthcare segment is measured using adjusted revenues and pre-tax adjusted income from operations. Key factors affecting results for this segment include:
•customer growth;
•revenue growth;
•percentage of Medicare Advantage customers in plans eligible for quality bonus payments;
•medical costs as a percentage of premiums (medical care ratio or "MCR") for our insured businesses; and
69
•selling, general and administrative expense as a percentage of adjusted revenues (expense ratio).
Results of Operations
| Financial Summary | For the Years Ended December 31, | Change Favorable (Unfavorable) | Change Favorable (Unfavorable) | ||||||||||||||||||||||||||||||||||||||||||||
| (Dollars in millions) | 2021 | 2020 | 2019 | 2021 vs. 2020 | 2020 vs. 2019 | ||||||||||||||||||||||||||||||||||||||||||
| Adjusted revenues | $ | 44,652 | $ | 41,135 | $ | 39,089 | $ | 3,517 | 9 | % | $ | 2,046 | 5 | % | |||||||||||||||||||||||||||||||||
| Pre-tax adjusted income from operations | $ | 3,609 | $ | 4,031 | $ | 3,963 | $ | (422) | (10) | % | $ | 68 | 2 | % | |||||||||||||||||||||||||||||||||
| Pre-tax adjusted margin | 8.1 | % | 9.8 | % | 10.1 | % | (170) | bps | (30) | bps | |||||||||||||||||||||||||||||||||||||
| Medical care ratio | 84.0 | % | 78.3 | % | 80.0 | % | (570) | bps | 170 | bps | |||||||||||||||||||||||||||||||||||||
| Expense ratio | 21.0 | % | 23.5 | % | 23.4 | % | 250 | bps | (10) | bps | |||||||||||||||||||||||||||||||||||||
2021 versus 2020
Adjusted revenues increased, reflecting Medicare Advantage and Individual customer growth, higher premium rates due to anticipated underlying medical cost trend, higher net investment income and the absence of the 2020 premium relief programs for clients implemented in response to significantly lower than historical utilization as individuals deferred care due to the COVID-19 pandemic.
Pre-tax adjusted income from operations decreased due to increased utilization of health care services by our customers, including increased direct costs of COVID-19 testing, treatment and vaccines; partially offset by higher net investment income, increased specialty contributions, the absence of the premium relief programs and the repeal of the health insurance industry tax. The impacts of COVID-19 remain uncertain and could vary significantly as discussed in the "COVID-19 Update" section of this MD&A.
The medical care ratio increased due to increased utilization of health care services by our customers, including increased direct costs of COVID-19 testing, treatment and vaccines as well as the repeal of the health insurance industry tax; partially offset by the absence of the premium relief programs.
The expense ratio decreased, reflecting increased revenues, the repeal of the health insurance industry tax, favorable litigation developments and efficiencies from continued disciplined expense management.
2020 versus 2019
Adjusted revenues increased, reflecting Medicare Advantage and U.S. Commercial insured customer growth, as well as higher premium rates due to anticipated underlying medical cost trend and the resumption of the health insurance industry tax. These favorable effects were partially offset by the impact of 2020 premium relief programs for clients implemented in response to significantly lower than historical utilization as individuals deferred care due to the COVID-19 pandemic.
Pre-tax adjusted income from operations increased, reflecting net favorable COVID-19 related impacts as well as U.S. Commercial insured and Medicare Advantage customer growth; partially offset by the resumption of the health insurance industry tax and less favorable prior period development. COVID-19 related impacts include deferral of care by our customers; partially offset by direct COVID-19 costs, costs of actions we have taken to support customers, providers and employees, and increased disenrollment resulting from the economic impacts of the pandemic.
The medical care ratio decreased driven by COVID-19 related impacts and the pricing effect of the health insurance industry tax. COVID-19 related impacts include deferral of care by our customers; partially offset by direct COVID-19 costs and premium relief programs extended to employer clients.
The expense ratio was flat reflecting higher insured revenues as well as efficiencies from continued disciplined expense management and the resumption of the health insurance industry tax.
70
Medical Customers
A medical customer is defined as a person meeting any one of the following criteria:
•is covered under a medical insurance policy, managed care arrangement or service agreement issued by us;
•has access to our provider network for covered services under their medical plan; or
•has medical claims that are administered by us.
| As of December 31, | Change Favorable (Unfavorable) | Change Favorable (Unfavorable) | |||||||||||||||||||||||||||||||||||||||||||||
| (In thousands) | 2021 | 2020 | 2019 | 2021 vs. 2020 | 2020 vs. 2019 | ||||||||||||||||||||||||||||||||||||||||||
| Cigna Healthcare Medical Customers | |||||||||||||||||||||||||||||||||||||||||||||||
| Insured | 4,757 | 4,538 | 4,466 | 219 | 5 | % | 72 | 2 | % | ||||||||||||||||||||||||||||||||||||||
| U.S. Commercial | 2,166 | 2,141 | 2,114 | 25 | 1 | % | 27 | 1 | % | ||||||||||||||||||||||||||||||||||||||
| U.S. Government | 1,510 | 1,387 | 1,361 | 123 | 9 | % | 26 | 2 | % | ||||||||||||||||||||||||||||||||||||||
International Health (1) | 1,081 | 1,010 | 991 | 71 | 7 | % | 19 | 2 | % | ||||||||||||||||||||||||||||||||||||||
| Services only | 12,324 | 12,112 | 12,671 | 212 | 2 | % | (559) | (4) | % | ||||||||||||||||||||||||||||||||||||||
| U.S. Commercial | 11,688 | 11,485 | 12,073 | 203 | 2 | % | (588) | (5) | % | ||||||||||||||||||||||||||||||||||||||
International Health (1) | 636 | 627 | 598 | 9 | 1 | % | 29 | 5 | % | ||||||||||||||||||||||||||||||||||||||
| Total | 17,081 | 16,650 | 17,137 | 431 | 3 | % | (487) | (3) | % | ||||||||||||||||||||||||||||||||||||||
(1) International Health excludes medical customers served by less than 100% owned subsidiaries and customers that are part of the businesses to be sold pursuant to the Chubb Transaction.
2021 versus 2020
Our medical customer base increased at December 31, 2021 compared with December 31, 2020 reflecting a higher customer base in our Middle Market, Select and International Health segments as well as our Individual business and Medicare Advantage plans; partially offset by a lower customer base in our National segment.
2020 versus 2019
Our medical customer base decreased at December 31, 2020 compared with December 31, 2019, reflecting a lower customer base in our Middle Market and National Accounts segments and increased disenrollment resulting from the economic impacts of the COVID-19 pandemic; partially offset by growth in our Select segment, Medicare Advantage plans and International Health.
Unpaid Claims and Claim Expenses
| As of December 31, | Change Increase (Decrease) | Change Increase (Decrease) | |||||||||||||||||||||||||||||||||||||||||||||
| (In millions) | 2021 | 2020 | 2019 | 2021 vs. 2020 | 2020 vs. 2019 | ||||||||||||||||||||||||||||||||||||||||||
Unpaid claims and claim expenses – Cigna Healthcare | $ | 4,261 | $ | 3,695 | $ | 3,336 | $ | 566 | 15 | % | $ | 359 | 11 | % | |||||||||||||||||||||||||||||||||
2021 versus 2020
Our unpaid claims and claim expenses liability was higher as of December 31, 2021 compared with December 31, 2020, primarily due to Medicare Advantage and Individual customer growth and increased claim volumes.
2020 versus 2019
Our unpaid claims and claim expenses liability was higher as of December 21, 2020 compared with December 31, 2019, primarily due to Medicare Advantage and U.S. Commercial insured customer growth.
Other Operations
For 2021, 2020 and 2019, Other Operations includes International businesses to be sold, Corporate Owned Life Insurance ("COLI") and the Company's run-off operations. Prior to the sale of the Group Disability and Life business on December 31, 2020, Other Operations also included Cigna's Group Disability and Life business which offered group long-term and short-term disability and group life, accident, voluntary and specialty insurance products and services. Other Operations was previously named Group
71
Disability and Other. As described in the introduction of Segment Reporting, performance of Other Operations is measured using adjusted revenues and pre-tax adjusted income from operations.
Results of Operations
| Financial Summary | For the Years Ended December 31, | Change Favorable (Unfavorable) | Change Favorable (Unfavorable) | |||||||||||||||||||||||||||||||||||||||||
| (Dollars in millions) | 2021 | 2020 | 2019 | 2021 vs. 2020 | 2020 vs. 2019 | |||||||||||||||||||||||||||||||||||||||
| Adjusted revenues | $ | 3,989 | $ | 8,446 | $ | 8,215 | $ | (4,457) | (53) | % | $ | 231 | 3 | % | ||||||||||||||||||||||||||||||
| Pre-tax adjusted income from operations | $ | 889 | $ | 966 | $ | 1,131 | $ | (77) | (8) | % | $ | (165) | (15) | % | ||||||||||||||||||||||||||||||
| Pre-tax adjusted margin | 22.3 | % | 11.4 | % | 13.8 | % | 1,090 | bps | (240) | bps | ||||||||||||||||||||||||||||||||||
2021 versus 2020
Adjusted revenues decreased due to the sale of the Group Disability and Life business on December 31, 2020. Because the sold business constituted a significant portion of Other Operations, adjusted revenues substantially declined in 2021 compared to 2020.
Pre-tax adjusted income from operations also declined due to the sale of the Group Disability and Life Insurance business. That decrease was partially offset by an increase in earnings from the International businesses held for sale.
2020 versus 2019
Adjusted revenues increased, reflecting business growth in the International businesses held for sale and the sold Group Disability and Life business. Partially offsetting those favorable effects were lower net investment income in the sold Group Disability and Life business and unfavorable foreign currency movements in the International businesses held for sale.
Pre-tax adjusted income from operations decreased due to lower earnings in the sold Group Disability and Life business reflecting unfavorable life claims experience related to the COVID-19 pandemic, unfavorable disability claim experience and lower investment income, partially offset by favorable results in the voluntary products. Those unfavorable effects were partially offset by improved earnings in the International businesses held for sale reflecting improved margin and business growth.
Other Items Related to International Businesses Subject to Definitive Purchase Agreement
For the year ended, December 31, 2021, 86% of the segment's adjusted revenues and 89% of the segment's pre-tax adjusted income from operations was associated with International businesses held for sale.
Corporate
Corporate reflects amounts not allocated to operating segments, including net interest expense (defined as interest on corporate debt less net investment income on investments not supporting segment and other operations), certain litigation matters, expense associated with our frozen pension plans, charitable contributions, severance, certain overhead and enterprise-wide project costs and intersegment eliminations for products and services sold between segments.
| Financial Summary | For the Years Ended December 31, | Change Favorable (Unfavorable) | Change Favorable (Unfavorable) | ||||||||||||||||||||||||||||||||||||||||||||
| (In millions) | 2021 | 2020 | 2019 | 2021 vs. 2020 | 2020 vs. 2019 | ||||||||||||||||||||||||||||||||||||||||||
| Pre-tax adjusted (loss) from operations | $ | (1,339) | $ | (1,552) | $ | (1,824) | $ | 213 | 14 | % | $ | 272 | 15 | % | |||||||||||||||||||||||||||||||||
2021 versus 2020
Pre-tax adjusted loss from operations was lower, primarily reflecting lower interest expense due to a lower average interest rate and lower levels of outstanding debt resulting from debt repayments.
2020 versus 2019
Pre-tax adjusted loss from operations was lower, primarily reflecting lower interest expense due to lower levels of debt.
INVESTMENT ASSETS
The following table presents our investment asset portfolio excluding separate account assets as of December 31, 2021 and December 31, 2020. Additional information regarding our investment assets is included in Notes 11, 12, 13 and 14 to the Consolidated
72
Financial Statements. For comparisons of investment assets portfolio excluding separate account assets as of December 31, 2020 compared with December 31, 2019, please refer to the previously filed MD&A included in Part II, Item 7 of our Form 10-K for the year ended December 31, 2020.
| (In millions) | December 31, 2021 | December 31, 2020 | ||||||||||||
| Debt securities | $ | 16,958 | $ | 18,131 | ||||||||||
| Equity securities | 603 | 501 | ||||||||||||
| Commercial mortgage loans | 1,566 | 1,419 | ||||||||||||
| Policy loans | 1,338 | 1,351 | ||||||||||||
| Other long-term investments | 3,574 | 2,832 | ||||||||||||
| Short-term investments | 428 | 359 | ||||||||||||
| Total | 24,467 | |||||||||||||
Investments classified as assets of businesses held for sale (1) | (5,109) | |||||||||||||
| Investments per Consolidated Balance Sheets | $ | 19,358 | $ | 24,593 | ||||||||||
(1) Investments related to the international life, accident and supplemental benefits businesses that are held for sale. See Note 5 to the Consolidated Financial Statements for additional information.
Debt Securities
Investments in debt securities include publicly-traded and privately-placed bonds, mortgage and other asset-backed securities and preferred stocks redeemable by the investor. These investments are classified as available for sale and are carried at fair value on our balance sheet. Additional information regarding valuation methodologies, key inputs and controls is included in Note 12 to the Consolidated Financial Statements. More detailed information about debt securities by type of issuer and maturity dates is included in Note 11 to the Consolidated Financial Statements.
The following table reflects our portfolio of debt securities by type of issuer as of December 31, 2021 and December 31, 2020:
| (In millions) | December 31, 2021 | December 31, 2020 | ||||||||||||
| Federal government and agency | $ | 387 | $ | 456 | ||||||||||
| State and local government | 171 | 167 | ||||||||||||
| Foreign government | 2,616 | 2,511 | ||||||||||||
Corporate | 13,266 | 14,562 | ||||||||||||
| Mortgage and other asset-backed | 518 | 435 | ||||||||||||
| Total | $ | 16,958 | $ | 18,131 | ||||||||||
Our debt securities portfolio decreased during 2021, reflecting a decrease in valuations due to increasing yields and net sale activity.
As of December 31, 2021, $14.7 billion, or 87% of the debt securities in our investment portfolio were investment grade (Baa and above, or equivalent) and the remaining $2.3 billion were below investment grade. The majority of the bonds that are below investment grade are rated at the higher end of the non-investment grade spectrum. These quality characteristics have not materially changed since the prior year and remain consistent with our investment strategy.
Debt securities include private placement assets of $5.8 billion. These investments are generally less marketable than publicly-traded bonds; however, yields on these investments tend to be higher than yields on publicly-traded bonds with comparable credit risk. We perform a credit analysis of each issuer and require financial and other covenants that allow us to monitor issuers for deteriorating financial strength and pursue remedial actions, if warranted.
Investments in debt securities are diversified by issuer, geography and industry. On an aggregate basis, the debt securities portfolio continues to perform according to original investment expectations. However, due to the economic impacts of the COVID-19 pandemic, there are certain issuers, particularly within the aviation, energy and hospitality sectors, that have shown signs of distress, primarily in the form of requests for temporary covenant relief. There were no material unrealized losses in any of these sectors as of the reporting date. We continue to monitor the economic environment and its effect on our portfolio and consider the impact of various factors in determining the allowance for credit losses on debt securities, which is discussed in Note 11 to the Consolidated Financial Statements.
Foreign government obligations are concentrated in Asia, primarily South Korea and Taiwan, consistent with our risk management practice and local regulatory requirements of our international business operations. We expect the amount of these foreign government
73
obligations to decrease significantly during 2022 upon the close of our sale of certain international businesses as discussed in Note 5 to the Consolidated Financial Statements.
Commercial Mortgage Loans
As of December 31, 2021, the $1.6 billion commercial mortgage loan portfolio consisted of approximately 50 loans that are in good standing. Our commercial mortgage loans are fixed rate loans, diversified by property type, location and borrower. Given the quality and diversity of the underlying real estate, positive debt service coverage and significant borrower cash invested in the property generally ranging between 30 and 40%, we remain confident that the vast majority of borrowers will continue to perform as expected under their contract terms. For further discussion of the results and changes in key loan metrics, see Note 11 to the Consolidated Financial Statements.
Loans are secured by high quality commercial properties, located in strong institutional markets and are generally made at less than 65% of the property's value at origination of the loan. Property value, debt service coverage, quality, building tenancy and stability of cash flows are all important financial underwriting considerations. We hold no direct residential mortgage loans and do not originate or service securitized mortgage loans.
Our annual in-depth review of our commercial mortgage loan investments is the primary mechanism for monitoring the overall quality rating of the mortgage portfolio. We completed the annual in-depth review in the second quarter of 2021 which included an analysis of each underlying property's most recent annual financial statements, rent rolls and operating plans, as well as a physical inspection of the property and a review of applicable market reports. The results of this annual review confirmed that the overall credit quality of our portfolio remains strong and was generally in line with the previous year's results.
COVID-19 has negatively impacted commercial real estate fundamentals and capital market activity with concentrated weakness in hotels and regional malls. Our mortgage loan portfolio is well diversified by property type and geography with no material exposure to hotels and no exposure to regional shopping malls. We continue to monitor the long-term impacts surrounding the office sector fundamentals due to multiple headwinds that may impact future valuations: expanded work from home flexibility, shorter term leases, elevated tenant improvement allowances and corporate migration to lower cost states. Our mortgage loans secured by office properties are in good standing.
Other Long-term Investments
Other long-term investments of $3.6 billion as of December 31, 2021 included investments in securities limited partnerships and real estate limited partnerships, direct investments in real estate joint ventures and other deposit activity that is required to support various insurance and health services businesses. The increase in other long-term investments of $0.7 billion since December 31, 2020 is primarily driven by net additional funding activity and value creation in the underlying investments. These limited partnership entities typically invest in mezzanine debt or equity of privately-held companies and equity real estate. Given our subordinate position in the capital structure of these underlying entities, we assume a higher level of risk for higher expected returns. To mitigate risk, these investments are diversified across approximately 210 separate partnerships and approximately 110 general partners who manage one or more of these partnerships. Also, the underlying investments are diversified by industry sector or property type and geographic region. No single partnership investment exceeded 4% of our securities and real estate limited partnership portfolio.
Income from our limited partnership investments is generally reported on a one quarter lag due to the timing of when financial information is received from the general partner or manager of the investments. Our net investment income increased significantly versus 2020 driven by the strong performance of assets underlying our limited partnership investments. The broad recovery since the beginning of the outbreak of the COVID-19 pandemic has resulted in strong corporate earnings and higher public and private asset valuations. We expect continued volatility in private equity and real estate fund performance going forward as fair market valuations are adjusted to reflect market and portfolio transactions.
We participate in an insurance joint venture in China with a 50% ownership interest. We account for this joint venture under the equity method of accounting and report our share of the net assets of $1.0 billion in Other assets. Our 50% share of the investment portfolio supporting the joint venture's liabilities is approximately $8.4 billion as of December 31, 2021. These investments were comprised of approximately 75% debt securities, including government and corporate debt diversified by issuer, industry and geography; 15% equities, including mutual funds, equity securities and private equity partnerships; and 10% long-term deposits and policy loans. Approximately 1% of the joint venture's investment assets are exposed to private real estate property developers in the China market. We participate in the approval of the joint venture's investment strategy and continuously review its execution. There were no investments with a material unrealized loss as of December 31, 2021.
74
Investment Outlook
We continue to actively monitor the economic impact of the pandemic, including supply chain, labor market and inflation dynamics, as well as fiscal and monetary responses and their potential impact on the portfolio. Future realized and unrealized investment results will be driven largely by market conditions that exist when a transaction occurs or at the reporting date. These future conditions are not reasonably predictable; however, we believe that the vast majority of our investments will continue to perform under their contractual terms. Based on our strategy to match the duration of invested assets to the duration of insurance and contractholder liabilities, we expect to hold a significant portion of these assets for the long-term. Although future declines in investment fair values resulting from interest rate movements and credit deterioration due to both investment-specific and the global economic uncertainties discussed above remain possible, we do not expect these losses to have a material adverse effect on our financial condition or liquidity.
MARKET RISK
Financial Instruments
Our assets and liabilities include financial instruments subject to the risk of potential losses from adverse changes in market rates and prices. Consistent with disclosure requirements, the following items have been excluded from this consideration of market risk for financial instruments:
•changes in the fair values of insurance-related assets and liabilities because their primary risks are insurance rather than market risk;
•changes in the fair values of investments recorded using the equity method of accounting and liabilities for pension and other postretirement and postemployment benefit plans (and related assets); and
•changes in the fair values of other significant assets and liabilities, such as goodwill, deferred policy acquisition costs, taxes and various accrued liabilities. Because they are not financial instruments, their primary risks are other than market risk.
Excluding these items, our primary market risk exposures from financial instruments are:
•Interest-rate risk on fixed-rate, medium-term instruments. Changes in market interest rates affect the value of instruments that promise a fixed return.
•Foreign currency exchange rate risk of the U.S. dollar, net of derivatives used for hedging, is primarily to the Chinese yuan renminbi and South Korean won. An unfavorable change in exchange rates reduces the carrying value of net assets denominated in foreign currencies.
Our Management of Market Risks
We predominantly rely on three techniques to manage our exposure to market risk:
•Investment/liability matching. We generally select investment assets with characteristics (such as duration, yield, currency and liquidity) that correspond to the underlying characteristics of our related insurance and contractholder liabilities so that we can match the investments to our obligations. Shorter-term investments generally support shorter-term life and health liabilities. Medium-term, fixed-rate investments support interest-sensitive and health liabilities. Longer-term investments generally support products with longer payout periods such as annuities.
•Use of local currencies for foreign operations. We generally conduct our international business through foreign operating entities that maintain assets and liabilities in local currencies. This technique limits exchange rate risk to our net assets.
•Use of derivatives. We use derivative financial instruments to reduce our primary market risks. See Note 11 to the Consolidated Financial Statements for additional information about derivative financial instruments.
75
Effect of Market Fluctuations
Assuming a 100 basis point increase in interest rates and 10% strengthening in the U.S. dollar to foreign currencies, the effect of hypothetical changes in market rates or prices on the fair value of certain financial instruments, subject to the exclusions noted above (particularly insurance liabilities), would have been as follows as of December 31:
| Market scenario for certain non-insurance financial instruments | Loss in Fair Value | |||||||||||||
| (in billions) | 2021 | 2020 | ||||||||||||
| 100 basis point increase in interest rates (excluding long-term debt) | $ | 1.4 | $ | 1.4 | ||||||||||
| 10% strengthening in U.S. dollar to foreign currencies | $ | 0.3 | $ | 0.4 | ||||||||||
The effect of a hypothetical increase in interest rates, primarily on debt securities and commercial mortgage loans, was determined by estimating the present value of future cash flows using various models, primarily duration modeling.
In the event of a hypothetical 100 basis point increase in interest rates, the fair value of the Company's long-term debt would decrease approximately $2.9 billion at December 31, 2021 and $3.0 billion at December 31, 2020. Changes in the fair value of our long-term debt do not impact our financial position or operating results. See Note 7 to the Consolidated Financial Statements for additional information about the Company's debt.
The effect of a hypothetical strengthening of the U.S. dollar relative to the foreign currencies of certain financial instruments held by us was estimated to be 10% of the fair value of these instruments, translated to the U.S. dollar. Our foreign operations hold investment assets, such as debt securities, cash and cash equivalents that are generally invested in the currency of the related liabilities.
Item 7A. QUANTITATIVE AND QUALITATIVE DISCLOSURES ABOUT MARKET RISK
The information contained under the caption "Market Risk" in the MD&A section of this Form 10-K is incorporated by reference.
76
Item 8. FINANCIAL STATEMENTS AND SUPPLEMENTARY DATA
Report of Independent Registered Public Accounting Firm
To the Board of Directors and Shareholders of Cigna Corporation
Opinions on the Financial Statements and Internal Control over Financial Reporting
We have audited the accompanying consolidated balance sheets of Cigna Corporation and its subsidiaries (the "Company") as of December 31, 2021 and 2020, and the related consolidated statements of income, comprehensive income, changes in total equity and cash flows for each of the three years in the period ended December 31, 2021, including the related notes (collectively referred to as the "consolidated financial statements"). We also have audited the Company's internal control over financial reporting as of December 31, 2021, based on criteria established in Internal Control - Integrated Framework (2013) issued by the Committee of Sponsoring Organizations of the Treadway Commission (COSO).
In our opinion, the consolidated financial statements referred to above present fairly, in all material respects, the financial position of the Company as of December 31, 2021 and 2020, and the results of its operations and its cash flows for each of the three years in the period ended December 31, 2021 in conformity with accounting principles generally accepted in the United States of America. Also in our opinion, the Company maintained, in all material respects, effective internal control over financial reporting as of December 31, 2021, based on criteria established in Internal Control - Integrated Framework (2013) issued by the COSO.
Basis for Opinions
The Company's management is responsible for these consolidated financial statements, for maintaining effective internal control over financial reporting, and for its assessment of the effectiveness of internal control over financial reporting, included in Management's Annual Report on Internal Control over Financial Reporting appearing under Item 9A. Our responsibility is to express opinions on the Company's consolidated financial statements and on the Company's internal control over financial reporting based on our audits. We are a public accounting firm registered with the Public Company Accounting Oversight Board (United States) (PCAOB) and are required to be independent with respect to the Company in accordance with the U.S. federal securities laws and the applicable rules and regulations of the Securities and Exchange Commission and the PCAOB.
We conducted our audits in accordance with the standards of the PCAOB. Those standards require that we plan and perform the audits to obtain reasonable assurance about whether the consolidated financial statements are free of material misstatement, whether due to error or fraud, and whether effective internal control over financial reporting was maintained in all material respects.
Our audits of the consolidated financial statements included performing procedures to assess the risks of material misstatement of the consolidated financial statements, whether due to error or fraud, and performing procedures that respond to those risks. Such procedures included examining, on a test basis, evidence regarding the amounts and disclosures in the consolidated financial statements. Our audits also included evaluating the accounting principles used and significant estimates made by management, as well as evaluating the overall presentation of the consolidated financial statements. Our audit of internal control over financial reporting included obtaining an understanding of internal control over financial reporting, assessing the risk that a material weakness exists, and testing and evaluating the design and operating effectiveness of internal control based on the assessed risk. Our audits also included performing such other procedures as we considered necessary in the circumstances. We believe that our audits provide a reasonable basis for our opinions.
Definition and Limitations of Internal Control over Financial Reporting
A company's internal control over financial reporting is a process designed to provide reasonable assurance regarding the reliability of financial reporting and the preparation of financial statements for external purposes in accordance with generally accepted accounting principles. A company's internal control over financial reporting includes those policies and procedures that (i) pertain to the maintenance of records that, in reasonable detail, accurately and fairly reflect the transactions and dispositions of the assets of the company; (ii) provide reasonable assurance that transactions are recorded as necessary to permit preparation of financial statements in accordance with generally accepted accounting principles, and that receipts and expenditures of the company are being made only in accordance with authorizations of management and directors of the company; and (iii) provide reasonable assurance regarding prevention or timely detection of unauthorized acquisition, use, or disposition of the company's assets that could have a material effect on the financial statements.
77
Because of its inherent limitations, internal control over financial reporting may not prevent or detect misstatements. Also, projections of any evaluation of effectiveness to future periods are subject to the risk that controls may become inadequate because of changes in conditions, or that the degree of compliance with the policies or procedures may deteriorate.
Critical Audit Matters
The critical audit matter communicated below is a matter arising from the current period audit of the consolidated financial statements that was communicated or required to be communicated to the audit committee and that (i) relates to accounts or disclosures that are material to the consolidated financial statements and (ii) involved our especially challenging, subjective, or complex judgments. The communication of critical audit matters does not alter in any way our opinion on the consolidated financial statements, taken as a whole, and we are not, by communicating the critical audit matter below, providing a separate opinion on the critical audit matter or on the accounts or disclosures to which it relates.
Goodwill Impairment Assessment - Evernorth and U.S. Government Reporting Units
As described in Note 18 to the consolidated financial statements, as of December 31, 2021, goodwill is primarily reported in the Evernorth segment ($35.1 billion) and the Cigna Healthcare segment ($10.7 billion), of which a portion of the goodwill balance for the Cigna Healthcare segment relates to the U.S. Government reporting unit. Management conducts its annual quantitative evaluation for goodwill impairment during the third quarter at the reporting unit level and writes it down through shareholders' net income if impaired. On a quarterly basis, management performs a qualitative impairment assessment to determine if events or changes in circumstances indicate that it is more likely than not that the carrying value of a reporting unit exceeds its estimated fair value. Fair value of a reporting unit is generally estimated based on both a discounted cash flow analysis and a market approach using assumptions that management believes a hypothetical market participant would use to determine a current transaction price. The significant assumptions and estimates used in determining fair value primarily include the discount rate and future cash flows. A discount rate is selected to correspond with each reporting unit's weighted average cost of capital. Future cash flows for Evernorth are primarily driven by the forecasted gross margins of the business, as well as operating expenses and long-term growth rates. Future cash flows for the U.S. Government reporting unit is primarily driven by forecasted revenues, benefit expenses, operating expenses and long-term growth rates.
The principal considerations for our determination that performing procedures relating to the goodwill impairment assessment of the Evernorth and the U.S. Government reporting units is a critical audit matter are the significant judgment by management when estimating the fair value of the reporting units. This in turn led to a high degree of auditor judgment, subjectivity, and effort in performing procedures and evaluating management's estimate of the reporting units' fair value determined using significant assumptions related to the discount rate, forecasted gross margins, and long-term growth rates for the Evernorth reporting unit and the discount rate, forecasted revenues, benefit expenses, operating expenses, and long-term growth rates for the U.S. Government reporting unit (collectively referred to as the "significant assumptions"). In addition, the audit effort involved the use of professionals with specialized skill and knowledge.
Addressing the matter involved performing procedures and evaluating audit evidence in connection with forming our overall opinion on the consolidated financial statements. These procedures included testing the effectiveness of controls relating to management's goodwill impairment assessment, including controls over management's methodology, inputs and assumptions used in its goodwill impairment assessment of the Evernorth and the U.S. Government reporting units. These procedures also included, among others (i) testing management's process for determining the fair value estimate of the reporting units; (ii) evaluating the appropriateness of the discounted cash flow analysis and market approach; (iii) testing the completeness and accuracy of underlying data used in the discounted cash flow analysis and market approach and (iv) evaluating the reasonableness of the significant assumptions. Evaluating the reasonableness of the significant assumptions involved consideration of (i) the current and past performance of the reporting units; (ii) the consistency with external market and industry data; and (iii) whether these assumptions were consistent with evidence obtained in other areas of the audit, as applicable. Professionals with specialized skill and knowledge were used to assist in the evaluation of the reasonableness of the discount rate and long-term growth rate significant assumptions.
/s/ PricewaterhouseCoopers LLP
Hartford, Connecticut
February 24, 2022
We have served as the Company's auditor since 1983.
78
a
Cigna Corporation Consolidated Statements of Income | ||||||||||||||||||||
| For the Years Ended December 31, | ||||||||||||||||||||
| (In millions, except per share amounts) | 2021 | 2020 | 2019 | |||||||||||||||||
| Revenues | ||||||||||||||||||||
| Pharmacy revenues | $ | 121,413 | $ | 107,769 | $ | 103,099 | ||||||||||||||
| Premiums | 41,154 | 42,627 | 39,714 | |||||||||||||||||
| Fees and other revenues | 9,962 | 8,761 | 9,363 | |||||||||||||||||
| Net investment income | 1,549 | 1,244 | 1,390 | |||||||||||||||||
| TOTAL REVENUES | 174,078 | 160,401 | 153,566 | |||||||||||||||||
| Benefits and expenses | ||||||||||||||||||||
| Pharmacy and other service costs | 117,553 | 103,484 | 97,668 | |||||||||||||||||
| Medical costs and other benefit expenses | 33,562 | 32,710 | 30,819 | |||||||||||||||||
| Selling, general and administrative expenses | 13,030 | 14,072 | 14,053 | |||||||||||||||||
| Amortization of acquired intangible assets | 1,998 | 1,982 | 2,949 | |||||||||||||||||
| TOTAL BENEFITS AND EXPENSES | 166,143 | 152,248 | 145,489 | |||||||||||||||||
| Income from operations | 7,935 | 8,153 | 8,077 | |||||||||||||||||
| Interest expense and other | (1,208) | (1,438) | (1,682) | |||||||||||||||||
| Debt extinguishment costs | (141) | (199) | (2) | |||||||||||||||||
| Gain (loss) on sale of business | — | 4,203 | — | |||||||||||||||||
| Net realized investment gains (losses) | 196 | 149 | 177 | |||||||||||||||||
| Income before income taxes | 6,782 | 10,868 | 6,570 | |||||||||||||||||
| TOTAL INCOME TAXES | 1,367 | 2,379 | 1,450 | |||||||||||||||||
| Net income | 5,415 | 8,489 | 5,120 | |||||||||||||||||
| Less: Net income attributable to noncontrolling interests | 50 | 31 | 16 | |||||||||||||||||
| SHAREHOLDERS' NET INCOME | $ | 5,365 | $ | 8,458 | $ | 5,104 | ||||||||||||||
| Shareholders' net income per share | ||||||||||||||||||||
| Basic | $ | 15.87 | $ | 23.17 | $ | 13.58 | ||||||||||||||
| Diluted | $ | 15.73 | $ | 22.96 | $ | 13.44 | ||||||||||||||
The accompanying Notes to the Consolidated Financial Statements are an integral part of these statements.
79
Cigna Corporation Consolidated Statements of Comprehensive Income | ||||||||||||||||||||
| For the Years Ended December 31, | ||||||||||||||||||||
| (In millions) | 2021 | 2020 | 2019 | |||||||||||||||||
| Net income | $ | 5,415 | $ | 8,489 | $ | 5,120 | ||||||||||||||
| Other comprehensive income (loss), net of tax | ||||||||||||||||||||
| Net unrealized appreciation (depreciation) on securities and derivatives | (215) | (75) | 957 | |||||||||||||||||
| Net translation gains (losses) on foreign currencies | (232) | 252 | (59) | |||||||||||||||||
| Postretirement benefits liability adjustment | 410 | (105) | (133) | |||||||||||||||||
| Other comprehensive income (loss), net of tax | (37) | 72 | 765 | |||||||||||||||||
| Total comprehensive income | 5,378 | 8,561 | 5,885 | |||||||||||||||||
| Comprehensive income (loss) attributable to noncontrolling interests | ||||||||||||||||||||
| Net income attributable to redeemable noncontrolling interests | 19 | 14 | 11 | |||||||||||||||||
| Net income attributable to other noncontrolling interests | 31 | 17 | 5 | |||||||||||||||||
| Other comprehensive (loss) attributable to redeemable noncontrolling interests | (14) | (8) | (5) | |||||||||||||||||
| Total comprehensive income attributable to noncontrolling interests | 36 | 23 | 11 | |||||||||||||||||
| SHAREHOLDERS' COMPREHENSIVE INCOME | $ | 5,342 | $ | 8,538 | $ | 5,874 | ||||||||||||||
The accompanying Notes to the Consolidated Financial Statements are an integral part of these statements.
80
Cigna Corporation Consolidated Balance Sheets | |||||||||||
| As of December 31, | |||||||||||
| (In millions) | 2021 | 2020 | |||||||||
| Assets | |||||||||||
| Cash and cash equivalents | $ | 5,081 | $ | 10,182 | |||||||
| Investments | 920 | 1,331 | |||||||||
| Accounts receivable, net | 15,071 | 12,191 | |||||||||
| Inventories | 3,722 | 3,165 | |||||||||
| Other current assets | 1,283 | 930 | |||||||||
| Assets of businesses held for sale | 10,057 | — | |||||||||
| Total current assets | 36,134 | 27,799 | |||||||||
| Long-term investments | 18,438 | 23,262 | |||||||||
| Reinsurance recoverables | 4,970 | 5,200 | |||||||||
| Deferred policy acquisition costs | 677 | 3,385 | |||||||||
| Property and equipment | 3,692 | 4,205 | |||||||||
| Goodwill | 45,811 | 44,648 | |||||||||
| Other intangible assets | 34,102 | 35,179 | |||||||||
| Other assets | 2,728 | 2,687 | |||||||||
| Separate account assets | 8,337 | 9,086 | |||||||||
| TOTAL ASSETS | $ | 154,889 | $ | 155,451 | |||||||
| Liabilities | |||||||||||
| Current insurance and contractholder liabilities | $ | 5,318 | $ | 5,308 | |||||||
| Pharmacy and other service costs payable | 15,309 | 13,347 | |||||||||
| Accounts payable | 6,655 | 5,478 | |||||||||
| Accrued expenses and other liabilities | 7,322 | 8,515 | |||||||||
| Short-term debt | 2,545 | 3,374 | |||||||||
| Liabilities of businesses held for sale | 6,423 | — | |||||||||
| Total current liabilities | 43,572 | 36,022 | |||||||||
| Non-current insurance and contractholder liabilities | 12,563 | 16,844 | |||||||||
| Deferred tax liabilities, net | 8,346 | 8,939 | |||||||||
| Other non-current liabilities | 3,762 | 4,629 | |||||||||
| Long-term debt | 31,125 | 29,545 | |||||||||
| Separate account liabilities | 8,337 | 9,086 | |||||||||
| TOTAL LIABILITIES | 107,705 | 105,065 | |||||||||
Contingencies — Note 22 | |||||||||||
| Redeemable noncontrolling interests | 54 | 58 | |||||||||
| Shareholders' equity | |||||||||||
Common stock (1) | 4 | 4 | |||||||||
| Additional paid-in capital | 29,574 | 28,975 | |||||||||
| Accumulated other comprehensive loss | (884) | (861) | |||||||||
| Retained earnings | 32,593 | 28,575 | |||||||||
| Less: Treasury stock, at cost | (14,175) | (6,372) | |||||||||
| TOTAL SHAREHOLDERS' EQUITY | 47,112 | 50,321 | |||||||||
| Other noncontrolling interests | 18 | 7 | |||||||||
| Total equity | 47,130 | 50,328 | |||||||||
| Total liabilities and equity | $ | 154,889 | $ | 155,451 | |||||||
(1) Par value per share, $0.01; shares issued, 394 million as of December 31, 2021 and 390 million as of December 31, 2020; authorized shares, 600 million.
The accompanying Notes to the Consolidated Financial Statements are an integral part of these statements.
81
| Cigna Corporation | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Consolidated Statements of Changes in Total Equity | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| (In millions) | Common Stock | Additional Paid-in Capital | Accumulated Other Comprehensive (Loss) | Retained Earnings | Treasury Stock | Shareholders' Equity | Other Non- controlling Interests | Total Equity | Redeemable Noncontrolling Interests | |||||||||||||||||||||||||||||||||||||||||||||||
| Balance at December 31, 2018 | $ | 4 | $ | 27,751 | $ | (1,711) | $ | 15,088 | $ | (104) | $ | 41,028 | $ | 7 | $ | 41,035 | $ | 37 | ||||||||||||||||||||||||||||||||||||||
| (15) | (15) | (15) | ||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Effect of issuing stock for employee benefit plans | 555 | (104) | 451 | 451 | ||||||||||||||||||||||||||||||||||||||||||||||||||||
| Other comprehensive income (loss) | 770 | 770 | 770 | (5) | ||||||||||||||||||||||||||||||||||||||||||||||||||||
| Net income | 5,104 | 5,104 | 5 | 5,109 | 11 | |||||||||||||||||||||||||||||||||||||||||||||||||||
Common dividends declared (per share: $0.04) | (15) | (15) | (15) | |||||||||||||||||||||||||||||||||||||||||||||||||||||
| Repurchase of common stock | (1,985) | (1,985) | (1,985) | |||||||||||||||||||||||||||||||||||||||||||||||||||||
| Other transactions impacting noncontrolling interests | — | (6) | (6) | (8) | ||||||||||||||||||||||||||||||||||||||||||||||||||||
| Balance at December 31, 2019 | $ | 4 | $ | 28,306 | $ | (941) | $ | 20,162 | $ | (2,193) | $ | 45,338 | $ | 6 | $ | 45,344 | $ | 35 | ||||||||||||||||||||||||||||||||||||||
| (30) | (30) | (30) | ||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Effect of issuing stock for employee benefit plans | 672 | (90) | 582 | 582 | ||||||||||||||||||||||||||||||||||||||||||||||||||||
| Other comprehensive income (loss) | 80 | 80 | 80 | (8) | ||||||||||||||||||||||||||||||||||||||||||||||||||||
| Net income | 8,458 | 8,458 | 17 | 8,475 | 14 | |||||||||||||||||||||||||||||||||||||||||||||||||||
Common dividends declared (per share: $0.04) | (15) | (15) | (15) | |||||||||||||||||||||||||||||||||||||||||||||||||||||
| Repurchase of common stock | (4,089) | (4,089) | (4,089) | |||||||||||||||||||||||||||||||||||||||||||||||||||||
| Other transactions impacting noncontrolling interests | (3) | (3) | (16) | (19) | 17 | |||||||||||||||||||||||||||||||||||||||||||||||||||
| Balance at December 31, 2020 | $ | 4 | $ | 28,975 | $ | (861) | $ | 28,575 | $ | (6,372) | $ | 50,321 | $ | 7 | $ | 50,328 | $ | 58 | ||||||||||||||||||||||||||||||||||||||
| Effect of issuing stock for employee benefit plans | 604 | (93) | 511 | 511 | ||||||||||||||||||||||||||||||||||||||||||||||||||||
| Other comprehensive income (loss) | (23) | (23) | (23) | (14) | ||||||||||||||||||||||||||||||||||||||||||||||||||||
| Net income | 5,365 | 5,365 | 31 | 5,396 | 19 | |||||||||||||||||||||||||||||||||||||||||||||||||||
Common dividends declared (per share: $4.00) | (1,347) | (1,347) | (1,347) | |||||||||||||||||||||||||||||||||||||||||||||||||||||
| Repurchase of common stock | (7,710) | (7,710) | (7,710) | |||||||||||||||||||||||||||||||||||||||||||||||||||||
| Other transactions impacting noncontrolling interests | (5) | (5) | (20) | (25) | (9) | |||||||||||||||||||||||||||||||||||||||||||||||||||
| Balance at December 31, 2021 | $ | 4 | $ | 29,574 | $ | (884) | $ | 32,593 | $ | (14,175) | $ | 47,112 | $ | 18 | $ | 47,130 | $ | 54 | ||||||||||||||||||||||||||||||||||||||
The accompanying Notes to the Consolidated Financial Statements are an integral part of these statements.
82
Cigna Corporation
Consolidated Statements of Cash Flows
| For the Years Ended December 31, | ||||||||||||||||||||
| (In millions) | 2021 | 2020 | 2019 | |||||||||||||||||
| Cash Flows from Operating Activities | ||||||||||||||||||||
| Net income | $ | 5,415 | $ | 8,489 | $ | 5,120 | ||||||||||||||
| Adjustments to reconcile net income to net cash provided by operating activities: | ||||||||||||||||||||
| Depreciation and amortization | 2,923 | 2,802 | 3,651 | |||||||||||||||||
| Realized investment (gains) losses, net | (196) | (149) | (177) | |||||||||||||||||
| Deferred income tax (benefit) | (220) | (386) | (313) | |||||||||||||||||
| Gain on sale of business | — | (4,203) | — | |||||||||||||||||
| Debt extinguishment costs | 141 | 199 | 2 | |||||||||||||||||
| Net changes in assets and liabilities, net of non-operating effects: | ||||||||||||||||||||
| Accounts receivable | (2,843) | (1,496) | (713) | |||||||||||||||||
| Inventories | (557) | (504) | 149 | |||||||||||||||||
| Deferred policy acquisition costs | (267) | (307) | (242) | |||||||||||||||||
| Reinsurance recoverable and Other assets | (389) | 230 | (277) | |||||||||||||||||
| Insurance liabilities | 967 | 841 | 575 | |||||||||||||||||
| Pharmacy and other service costs payable | 1,961 | 2,891 | (192) | |||||||||||||||||
| Accounts payable and Accrued expenses and other liabilities | (77) | 1,346 | 1,343 | |||||||||||||||||
| Other, net | 333 | 597 | 559 | |||||||||||||||||
| NET CASH PROVIDED BY OPERATING ACTIVITIES | 7,191 | 10,350 | 9,485 | |||||||||||||||||
| Cash Flows from Investing Activities | ||||||||||||||||||||
| Proceeds from investments sold: | ||||||||||||||||||||
| Debt securities and equity securities | 2,030 | 2,283 | 3,487 | |||||||||||||||||
| Investment maturities and repayments: | ||||||||||||||||||||
| Debt securities and equity securities | 1,628 | 1,519 | 1,825 | |||||||||||||||||
| Commercial mortgage loans | 180 | 19 | 199 | |||||||||||||||||
| Other sales, maturities and repayments (primarily short-term and other long-term investments) | 1,936 | 1,575 | 1,311 | |||||||||||||||||
| Investments purchased or originated: | ||||||||||||||||||||
| Debt securities and equity securities | (3,553) | (4,765) | (4,282) | |||||||||||||||||
| Commercial mortgage loans | (327) | (113) | (307) | |||||||||||||||||
| Other (primarily short-term and other long-term investments) | (2,554) | (1,924) | (1,753) | |||||||||||||||||
| Property and equipment purchases, net | (1,154) | (1,094) | (1,050) | |||||||||||||||||
| Acquisitions, net of cash acquired | (1,833) | (139) | (153) | |||||||||||||||||
| Divestiture, net of cash sold | (61) | 5,592 | — | |||||||||||||||||
| Other, net | 97 | 23 | (11) | |||||||||||||||||
| NET CASH (USED IN) PROVIDED BY INVESTING ACTIVITIES | (3,611) | 2,976 | (734) | |||||||||||||||||
| Cash Flows from Financing Activities | ||||||||||||||||||||
| Deposits and interest credited to contractholder deposit funds | 153 | 1,023 | 955 | |||||||||||||||||
| Withdrawals and benefit payments from contractholder deposit funds | (168) | (979) | (1,097) | |||||||||||||||||
| Net change in short-term debt | 975 | 60 | (681) | |||||||||||||||||
| Net proceeds on issuance of term loan | — | 1,398 | — | |||||||||||||||||
| Repayment of term loan | — | (1,400) | — | |||||||||||||||||
| Payments for debt extinguishment | (136) | (212) | (3) | |||||||||||||||||
| Repayment of long-term debt | (4,578) | (8,047) | (4,491) | |||||||||||||||||
| Net proceeds on issuance of long-term debt | 4,260 | 3,465 | — | |||||||||||||||||
| Repurchase of common stock | (7,742) | (4,042) | (1,987) | |||||||||||||||||
| Issuance of common stock | 326 | 376 | 224 | |||||||||||||||||
| Common stock dividend paid | (1,341) | (15) | (15) | |||||||||||||||||
| Other, net | 39 | (160) | (92) | |||||||||||||||||
| NET CASH (USED IN) FINANCING ACTIVITIES | (8,212) | (8,533) | (7,187) | |||||||||||||||||
| Effect of foreign currency rate changes on cash, cash equivalents and restricted cash | (65) | 41 | (8) | |||||||||||||||||
| Net (decrease) increase in cash, cash equivalents and restricted cash | (4,697) | 4,834 | 1,556 | |||||||||||||||||
Cash, cash equivalents and restricted cash January 1, (1) | 10,245 | 5,411 | 3,855 | |||||||||||||||||
Cash, cash equivalents and restricted cash, December 31, | 5,548 | 10,245 | 5,411 | |||||||||||||||||
| Cash reclassified to assets of businesses held for sale | (425) | — | (743) | |||||||||||||||||
Cash, cash equivalents and restricted cash December 31, per Consolidated Balance Sheets (2) | $ | 5,123 | $ | 10,245 | $ | 4,668 | ||||||||||||||
| Supplemental Disclosure of Cash Information: | ||||||||||||||||||||
| Income taxes paid, net of refunds | $ | 2,240 | $ | 1,837 | $ | 1,776 | ||||||||||||||
| Interest paid | $ | 1,253 | $ | 1,439 | $ | 1,645 | ||||||||||||||
(1) Includes $743 million reported in Assets of businesses held for sale as of January 1, 2020.
(2) Restricted cash and cash equivalents were reported in Other long-term investments as of December 31, 2021 and December 31, 2020 and were reported in Other long-term investments and Other assets as of December 31, 2019.
The accompanying Notes to the Consolidated Financial Statements are an integral part of these statements.
83
CIGNA CORPORATION
NOTES TO THE CONSOLIDATED FINANCIAL STATEMENTS
TABLE OF CONTENTS
| Note Number | Footnote | Page | ||||||
BUSINESS AND CAPITAL STRUCTURE | ||||||||
INSURANCE INFORMATION | ||||||||
INVESTMENTS | ||||||||
WORKFORCE MANAGEMENT AND COMPENSATION | ||||||||
PROPERTY, LEASES AND OTHER ASSET BALANCES | ||||||||
COMPLIANCE, REGULATION AND CONTINGENCIES | ||||||||
RESULTS DETAILS | ||||||||
84
Note 1 – Description of Business
Cigna Corporation, together with its subsidiaries (either individually or collectively referred to as "Cigna," the "Company," "we," "our" or "us") is a global health services organization with a mission of helping those we serve improve their health, well-being and peace of mind by making health care affordable, predictable and simple. Our subsidiaries offer a differentiated set of pharmacy, medical, behavioral, dental and supplemental products and services.
The majority of these products are offered through employers and other groups such as governmental and non-governmental organizations, unions and associations. Cigna also offers commercial health and dental insurance and Medicare products to individuals in the United States and selected international markets. In addition to these ongoing operations, Cigna also has certain run-off operations.
Details of the Company's reporting segments and recent changes are provided below:
We entered into a definitive agreement in October 2021 to sell our life, accident and supplemental benefits businesses in seven countries to Chubb INA Holdings, Inc. ("Chubb") for $5.75 billion cash (the "Chubb Transaction"). See Note 5 for further information on the classification of these businesses as held for sale. In connection with the pending Chubb Transaction, we revised our business reporting structure. As such, we adjusted our segment reporting effective in the fourth quarter of 2021 so that the results previously reported in the International Markets segment are now reported as follows:
•The businesses to be retained by Cigna are now reported in the newly created International Health operating segment that will be aggregated with our existing U.S. Commercial and U.S. Government operating segments in the renamed Cigna Healthcare reporting segment (previously named U.S. Medical segment).
•The businesses to be sold pursuant to the Chubb Transaction are now reported in Other Operations.
Segment results for the years ended December 31, 2020 and 2019 have been restated to conform to the new segment presentation (see Note 23). A full description of our segments follows:
Evernorth includes a broad range of coordinated and point solution health services and capabilities, as well as those from partners across the health care system, in pharmacy solutions, benefits management solutions, care delivery and care management solutions and intelligence solutions, which are provided to health plans, employers, government organizations and health care providers.
Cigna Healthcare includes U.S. Commercial, U.S. Government and International Health operating segments that provide comprehensive medical and coordinated solutions to clients and customers. U.S. Commercial products and services include medical, pharmacy, behavioral health, dental, vision, health advocacy programs and other products and services for insured and self-insured customers. U.S. Government solutions include Medicare Advantage, Medicare Supplement and Medicare Part D plans for seniors and individual health insurance plans both on and off the public exchanges. International Health solutions include health care coverage in our international markets, as well as health care benefits for globally mobile individuals and employees of multinational organizations. The Cigna Healthcare segment is comprised of the previously named U.S. Medical segment and the businesses to be retained from the previous International Markets segment.
Other Operations contains the remainder of our business operations, consisting of the following:
•Ongoing business:
•Corporate-Owned Life Insurance ("COLI") offers permanent insurance contracts sold to corporations to provide coverage on the lives of certain employees for the purpose of financing employer-paid future benefit obligations.
•Exiting businesses:
•International Life, Accident and Supplemental Benefits Businesses in seven countries to be sold pursuant to the Chubb Transaction.
•Group Disability and Life. Prior to the sale of the U.S. Group Disability and Life business on December 31, 2020, this operating segment provided group long-term and short-term disability, group life, accident, voluntary and specialty insurance products and related services.
•Run-off businesses:
•Reinsurance: predominantly comprised of guaranteed minimum death benefit ("GMDB") and guaranteed minimum income benefit ("GMIB") business effectively exited through reinsurance with Berkshire Hathaway Life Insurance Company of Nebraska ("Berkshire") in 2013.
•Settlement Annuity business in run-off.
85
•Individual Life Insurance and Annuity and Retirement Benefits businesses: deferred gains from the sales of these businesses.
Other Operations was previously named Group Disability and Other.
Corporate reflects amounts not allocated to operating segments, including net interest expense (defined as interest on corporate debt less net investment income on investments not supporting segment and other operations), certain litigation matters, expense associated with our frozen pension plans, charitable contributions, severance, certain overhead and enterprise-wide project costs and intersegment eliminations for products and services sold between segments.
Note 2 – Summary of Significant Accounting Policies
Basis of Presentation
The Consolidated Financial Statements include the accounts of Cigna Corporation and its consolidated subsidiaries. Intercompany transactions and accounts have been eliminated in consolidation. These Consolidated Financial Statements were prepared in conformity with accounting principles generally accepted in the United States of America ("GAAP").
Amounts recorded in the Consolidated Financial Statements necessarily reflect management's estimates and assumptions about medical costs, investment and receivable valuations, interest rates and other factors. Significant estimates are discussed throughout these Notes; however, actual results could differ from those estimates. The impact of a change in estimate is generally included in earnings in the period of adjustment.
Recent Accounting Pronouncements
There were no new accounting standards adopted during the year ended December 31, 2021 that had a material impact on our consolidated financial statements.
Accounting Guidance Not Yet Adopted
Facilitation of the Effects of Reference Rate Reform on Financial Reporting (ASU 2020-04) and related amendments
•Permits optional expedients and exceptions to simplify the accounting for contract modifications, hedging arrangements and held-to-maturity investments, when certain changes are made to a contract or instrument to facilitate reference rate reform and the discontinuation of reference interbank offered rates, including LIBOR.
•An entity may elect to apply the amendments, by topic or subsection, at any point prospectively through December 31, 2022. When elected, the optional expedients must be applied consistently for all eligible contracts or transactions.
The Company has performed a comprehensive evaluation of our exposures and does not believe the cessation of LIBOR will materially impact our operations or financial results, primarily because many of the Company's contracts contain contractual fallback language for a new benchmark rate or the underlying exposure is minimal.
86
Targeted Improvements to the Accounting for Long-Duration Contracts (ASU 2018-12) and related amendments
Effective date of January 1, 2023 for Cigna (early adoption permitted) and requires the following key provisions (for insurance entities that issue long-duration contracts):
•Changes to the measurement of the future policy benefits liability for traditional and limited-pay insurance contracts:
•Assumptions used to measure cash flows (such as mortality, morbidity and lapse assumptions) to be updated at least annually with the effect of changes in those assumptions remeasured retrospectively and reflected in current period net income.
•Discount rate assumptions to be updated quarterly based on market level yields for low credit risk fixed income instruments ("upper-medium grade fixed-income instrument"), with any changes reflected in other comprehensive income. The upper-medium grade fixed-income instrument yield is interpreted to mean A-rated.
•Deferred policy acquisition costs ("DAC") related to long-duration insurance contracts to be amortized on a constant-level basis over the expected term of the related contracts. Other related deferred or capitalized balances (such as unearned revenue liability and value of business acquired) may use this simplified amortization method.
•Market risk benefits (defined as protecting the contractholder from other-than-nominal capital market risk and exposing the insurer to that risk) to be measured at fair value, with changes in fair value recognized in net income each period, except for the effect of changes in the insurance entity's credit risk to be recognized in other comprehensive income.
•Additional disclosures, including disaggregated rollforwards for the liability for future policy benefits, market risk benefits, separate account liabilities and DAC, as well as information about significant inputs, judgments, assumptions and methods used in measurement.
•Transition methods at adoption vary:
•Changes to the liability for future policy benefits to use a modified retrospective approach applied to all outstanding contracts on the basis of their existing carrying amounts as of the beginning of the earliest period presented, with an option to elect a full retrospective transition under certain criteria. Remeasuring the future policy benefits liability for the discount rate to be recorded through accumulated other comprehensive income at transition.
•DAC to follow the transition method used for future policyholder benefits.
•Market risk benefits to be transitioned retrospectively and measured at fair value at the beginning of the earliest period presented. The difference between this fair value and carrying value to be recognized in the opening balance of retained earnings, excluding the effect of credit risk changes that are to be recognized in accumulated other comprehensive income.
Expected effects:
•The new guidance will apply to our long-duration insurance products predominantly within the Other Operations and Cigna Healthcare segments.
•The Company developed a cross-functional implementation project plan and is executing on the necessary significant changes to our systems, processes and controls.
•The Company will adopt the standard on January 1, 2023, using the modified retrospective transition method for changes to the liability for future policy benefits and DAC. We currently do not expect the impact of adoption to be material to shareholder's equity.
•Although we continue to evaluate the new requirements of the standard and model their impacts across various products, we are unable to project or estimate the magnitude or frequency of expected changes to our financial results. However, it is possible that our income recognition pattern could change for several reasons:
•Applying periodic assumption updates, versus the current locked-in model, may change our timing of profit or loss recognition.
•DAC amortization will be on a constant level basis over the expected term of the related contracts and no longer tied to the emergence of profit on such contracts.
•Features, such as the Company's GMDB product, that provide market-risk benefits are not currently measured at fair value, so these liabilities and related reinsurance recoverables will become subject to market sensitivity, notably to interest rates.
87
Significant Accounting Policies
The Company's accounting policies are described either in this Note or in the applicable Notes to the Consolidated Financial Statements as listed in the table of contents.
A.Cash and Cash Equivalents
Cash and cash equivalents are carried at cost that approximates fair value. Cash equivalents consist of short-term investments with maturities of three months or less from the time of purchase. The Company reclassifies cash overdraft positions to liabilities when the legal right of offset does not exist.
B.Inventories
Inventories consist of prescription drugs and medical supplies and are stated at the lower of first-in-first-out cost or net realizable value.
C.Deferred Policy Acquisition Costs
Costs eligible for deferral include incremental, direct costs of acquiring new or renewal insurance and investment contracts and other costs directly related to successful contract acquisition. Examples of deferrable costs include commissions, sales compensation and benefits, policy issuance and underwriting costs. The Company records acquisition costs differently depending on the product line. Acquisition costs for:
•Supplemental health, life and accident insurance products (primarily individual products) that comprise the majority of the Company's deferred policy acquisition costs and group health and accident insurance products are deferred and amortized, generally in proportion to the ratio of periodic revenue to the estimated total revenues over the contract periods. See Note 5 for Deferred policy acquisition costs reclassified to Assets of businesses held for sale.
•Universal life products are deferred and amortized in proportion to the present value of total estimated gross profits over the expected lives of the contracts.
•Other products are expensed as incurred.
Deferred policy acquisition costs also include the value of business acquired ("VOBA") for certain acquisitions with material long-duration insurance contracts. The Company recorded amortization of deferred policy acquisition costs of $478 million in 2021, $502 million in 2020 and $483 million in 2019 primarily in Selling, general and administrative expenses.
Each year, deferred policy acquisition costs are tested for recoverability. For universal life and other individual products, management estimates the present value of future revenues less expected payments. For group health and accident insurance products, management estimates the sum of unearned premiums and anticipated net investment income less future expected claims and related costs. If management's estimates of these sums are less than the deferred costs, the Company reduces deferred policy acquisition costs and records an additional expense.
D.Other Assets (Current and Non-Current)
Other current assets consist primarily of prepaid expenses, accrued investment income, the current portion of reinsurance recoverables and income tax receivables. Other non-current assets consist primarily of GMIB assets, operating lease right-of-use assets and various other insurance-related assets. See Note 10 for the Company's accounting policy for GMIB assets and Note 19 for the Company's accounting policy related to leases. Additionally, other non-current assets include the carrying value of our equity-method investments in business-related joint ventures in China, India, the U.S. and other foreign jurisdictions. Earnings or losses from these equity-method investments in joint ventures are recorded in Fees and other revenues.
E.Redeemable Noncontrolling Interests
Redeemable noncontrolling interests on our Consolidated Balance Sheets represents the noncontrolling shareholders' preferred and common stock interests of the Company's consolidated less than fully owned subsidiaries. Those shareholders may choose to require the Company to purchase their redeemable noncontrolling interest. We also have the right to require those shareholders to sell their redeemable noncontrolling interest to us. The redeemable noncontrolling interest was recorded at fair value as of the date of purchase. When the estimated redemption value for a redeemable noncontrolling interest exceeds its carrying value, an adjustment to increase the redeemable noncontrolling interest is recorded with an offsetting reduction to retained earnings or additional paid-in capital in the
88
absence of retained earnings. When an adjustment is made to the carrying value of the redeemable noncontrolling interest, the calculation of shareholders' net income per share will be adjusted if the redemption value exceeds fair value.
F.Accrued Expenses and Other Current and Non-Current Liabilities
Accrued expenses (current) primarily includes financial and performance guarantee liabilities under pharmacy contracts (see section H), management compensation and various insurance-related liabilities, including experience-rated refunds, reinsurance contracts and the risk adjustment and minimum medical loss ratio rebate accruals under The Patient Protection and Affordable Care Act (the "ACA"). Other non-current liabilities primarily include obligations for pension (see Note 16), GMIB contract liabilities (see Note 10), lease liabilities (see Note 19), uncertain tax positions (see Note 21) and self-insured exposures not expected to be settled within one year.
The Company accrues for legal and regulatory matters when a loss contingency is both probable and estimable. The estimated loss is generally recorded in Selling, general and administrative expenses and represents the Company's best estimate of the loss contingency. If the loss estimate is a range, the Company accrues the minimum amount in the range if no amount is better than any other estimated amount in the range. Legal costs to defend the Company's litigation and arbitration matters are expensed as incurred in cases that the Company cannot reasonably estimate the ultimate cost to defend. If the Company can reasonably estimate the cost to defend, a liability for these costs is accrued when the claim is reported. Litigation and legal or regulatory matters that the Company has identified with a reasonable possibility of material loss are described in Note 22.
G.Translation of Foreign Currencies
The Company generally conducts its international business through foreign operating entities that maintain assets and liabilities in local currencies that are their functional currencies. The Company uses exchange rates as of the balance sheet date to translate assets and liabilities into U.S. dollars. Translation gains or losses on functional currencies, net of applicable taxes, are recorded in Accumulated other comprehensive income (loss). The Company uses average monthly exchange rates during the year to translate revenues and expenses into U.S. dollars.
H.Pharmacy Revenues and Costs
Pharmacy revenues. Pharmacy revenues are primarily derived from providing pharmacy benefit management services to clients and customers. Pharmacy revenues are recognized when control of the promised goods or services is transferred to clients and customers, in an amount that reflects the consideration the Company expects to receive for those goods or services.
The Company provides or makes available various services supporting benefit management and claims administration and is generally obligated to provide prescription drugs to clients' members using multiple distribution methods including retail networks, home delivery and specialty pharmacies. These goods and services are integrated into a single performance obligation to process claims, dispense prescription drugs and provide other services over the contract period (generally three years). This performance obligation is satisfied as the business stands ready to fulfill its obligation.
Revenues for dispensing prescription drugs through retail pharmacies are reported gross and consist of the prescription price (ingredient cost and dispensing fee) contracted with clients, including the customer copayment and any associated fees for services, because the Company acts as the principal in these arrangements. When a prescription is presented to a retail network pharmacy, the Company is solely responsible for customer eligibility, drug utilization review, drug-to-drug interaction review, any required clinical intervention, plan provision information, payment to the pharmacy and client billing. These revenues are recognized based on the full prescription price when the pharmacy claim is processed and approved for payment. The Company also provides benefit design and formulary consultation services to clients and negotiates separate contractual relationships with clients and network pharmacies. These factors indicate that the Company has control over these transactions until the prescription is processed. Revenues are billed, due and recognized at contract rates either on a periodic basis or as services are provided (such as based on volume of claims processed). This recognition pattern aligns with the benefits from services provided.
Home delivery and specialty pharmacy revenues are due and recognized as each prescription is shipped, net of reserves for discounts and contractual allowances estimated based on historical experience. Any differences between estimates and actual collections are reflected in operations when payments are received. Historically, adjustments to original estimates and returns have not been material. The Company has elected the practical expedient to account for shipping and handling as a fulfillment activity.
We may also provide certain financial and performance guarantees, including a minimum level of discounts a client may receive, generic utilization rates and various service levels. Clients may be entitled to receive compensation if we fail to meet the guarantees. Actual performance is compared to the contractual guarantee for each measure throughout the period and the Company defers revenue
89
for any estimated payouts within Accrued expenses and other liabilities (current). These estimates are adjusted at the end of the guarantee period. Historically, adjustments to original estimates have not been material. The performance guarantee liability was $1.1 billion as of December 31, 2021 and December 31, 2020.
The Company administers programs through which we may receive rebates and other vendor consideration from pharmaceutical manufacturers. The amounts of such rebates or other vendor consideration shared with pharmacy benefit management services clients vary based on the contractual arrangement with the client and in some cases the type of consideration received from the pharmaceutical manufacturer. Rebates and other vendor consideration payable to pharmacy benefit management services clients are recorded as a reduction of Pharmacy revenues. Estimated amounts payable to clients are based on contractual sharing arrangements between the Company and the client and these amounts are adjusted when amounts are collected from pharmaceutical manufacturers in accordance with the contractual arrangement between the Company and the client. Historically, these adjustments have not been material.
In retail, home delivery and specialty transactions, amounts may be collected from third-party payors. These are billed and collected subject to normal account receivable collections procedures.
Other pharmacy service revenues are earned by distributing specialty pharmaceuticals and medical supplies to providers, clinics and hospitals. These revenues are billed, due and recognized at contracted rates as prescriptions and supplies are shipped and services are provided.
Pharmacy costs. Pharmacy costs include the cost of prescriptions sold, network pharmacy claim costs and copayments. Also included are direct costs of dispensing prescriptions including supplies, shipping and handling and direct costs associated with clinical programs, such as drug utilization management and medication adherence counseling. Home delivery and specialty pharmacy costs are recognized when the drug is shipped and retail network costs are recognized when the drug is processed and approved for payment. Rebates and other vendor consideration received when providing pharmacy benefit management services are recorded as a reduction of pharmacy costs. Rebates are recognized as prescriptions are shipped or processed and approved for payment. Historically, the effect of adjustments resulting from the reconciliation of rebates recognized to the amounts billed and collected, net of contractual allowances, has not been material. The Company maintains reimbursement guarantees with certain retail network pharmacies. For each such guarantee, the Company records a pharmacy and other service costs payable or prepaid asset for applicable retail network claims based on our actual performance throughout the period against the contractual reimbursement rate. The Company's contracts with certain retail pharmacies give the Company the right to adjust reimbursement rates during the annual guarantee period.
Other. Incremental costs of obtaining service and pharmacy contracts for short-term arrangements are expensed as incurred.
I.Premiums and Related Expenses
Premiums for group life, accident and health insurance and managed care coverages are recognized as revenue on a pro rata basis over the contract period. Benefits and expenses are recognized when incurred and, for our Cigna Healthcare insured business, are presented net of pharmaceutical manufacturer rebates. For experience-rated contracts, premium revenue includes an adjustment for experience-rated refunds based on contract terms and calculated using the customer's experience (including estimates of incurred but not reported claims).
Premiums received for the Company's Medicare Advantage plans, Medicare Part D products and Individual and Family Plans from the Centers for Medicare and Medicaid Services ("CMS") and customers are recognized as revenue ratably over the contract period.
CMS provides risk-adjusted premium payments for Medicare Advantage Plans and Medicare Part D products based on our customer demographics and medical diagnoses, which may change from period to period based on the underlying health of our customers. The Company recognizes changes to risk-adjusted premiums as revenue when the amounts are determinable and collection is reasonably assured. Revenue adjustments are generally settled semi-annually with CMS. The final revenue adjustment is generally settled with CMS in the year following the contract year.
Medicare Part D premiums include payments from CMS for risk-sharing adjustments that are estimated quarterly based on claim experience by comparing actual incurred prescription drug costs to the estimated costs submitted in the original contracts. These adjustments may result in more or less revenue from CMS. Final revenue adjustments generally occur in the year following the contract year.
The ACA prescribed a risk-adjustment program to mitigate the risk for participating health insurance companies selling coverage on the public exchanges. The risk-adjustment program reallocates funds from insurers with lower risk populations to insurers with higher risk populations based on the relative risk scores of participants. We estimate our receivable or payable based on the risk of our
90
customers compared to the risk of other customers in the same state and market, considering data obtained from industry studies and the United States Department of Health and Human Services ("HHS"). Receivables or payables are recorded as adjustments to premium revenue based on our year-to-date experience when the amounts are reasonably estimable and collection is reasonably assured. Final revenue adjustments are determined by HHS in the year following the policy year.
Premium revenue may also include an adjustment to reflect the estimated effect of rebates due to customers under medical loss ratio provisions of the ACA. These rebate liabilities are settled in the subsequent year.
Premiums for individual life, accident and supplemental health insurance and annuity products, excluding universal life and investment-related products, are recognized as revenue when due. Benefits and expenses are matched with premiums.
Revenue for universal life products is recognized as follows:
•Investment income on assets supporting universal life products is recognized in Net investment income as earned.
•Charges for mortality, administration and policy surrender are recognized in Premiums as earned. Administrative fees are considered earned when services are provided.
Benefits and expenses for universal life products consist of benefit claims in excess of policyholder account balances and income earned by policyholders. Expenses are recognized when claims are incurred and income is credited to policyholders in accordance with contract provisions.
The unrecognized portion of premiums received is recorded as unearned premiums included in insurance and contractholder liabilities (see Note 9 for further information).
J.Fees and Related Expenses
The majority of the Company's service fees are derived from administrative services only ("ASO") arrangements, fee-for-service clinical solutions, administration of certain rebate arrangements, health benefit management services and administration of services to specialty pharmacy manufacturers.
ASO arrangements allow plan sponsors to self-fund claims and assume the risk of medical or other benefit costs. Most of the Company's ASO arrangements are for medical and specialty services, including pharmacy benefits. Generally, the Company's ASO arrangements are short-term. Contract modifications typically occur on renewal and are prospective in nature.
In return for fees from these clients, the Company provides access to our participating provider networks and other services supporting benefit management, including claims administration, behavioral health services, disease management, utilization management and cost containment programs. In general, the Company considers these services to be a combined performance obligation to provide cost effective administration of plan benefits over the contract period. Fees are billed, due and recognized monthly at contracted rates based on current membership or utilization. This recognition pattern aligns with the benefits from services provided to clients. These revenues are reported in Fees and other revenues in the Consolidated Statements of Income.
The Company may also provide performance guarantees that provide potential refunds to clients if certain service standards, clinical outcomes or financial metrics are not met. If these standards, outcomes and metrics are not met, the Company may be financially at risk up to a stated percentage of the contracted fee or a stated dollar amount. The Company defers revenue by recording a liability for estimated payouts associated with these guarantees within Accrued expenses and other liabilities. The amount of revenue deferred is estimated for each type of guarantee using either a most likely amount or expected value method depending on the nature of the guarantee and the information available to estimate refunds. Estimates are refined each reporting period as additional information on the Company's performance becomes available and upon final reconciliation and settlement following the guarantee period. Amounts accrued and paid for these performance guarantees during the reporting periods were not material.
Rebates from pharmaceutical manufacturers for ASO client purchases at retail pharmacies, net of amounts payable to ASO clients, were considered compensation for use of the manufacturer's products and recorded in Fees and other revenues prior to transitioning U.S. Commercial customers to Express Scripts' retail pharmacy network in the third quarter of 2019. After this transition, these rebates are reflected as a reduction to pharmacy costs (see "Pharmacy costs" above).
Expenses associated with administrative programs and services are recognized as incurred in Selling, general and administrative expenses.
91
The Company also earns revenue, as part of its integrated pharmacy benefits performance obligation, by offering fee-for-service clinical solutions to our clients, such as drug utilization management and medication adherence counseling. These clinical programs help clients to drive better health outcomes at a lower cost by identifying and addressing potentially unsafe or wasteful prescribing, dispensing and utilization of prescription drugs and communicating with, or supporting communications with physicians, pharmacies and patients. Fees are billed, due and recognized at contracted rates either on a periodic basis or as services are provided. This recognition pattern aligns with the benefits from services provided. These revenues are reported in Fees and other revenues in the Consolidated Statements of Income. Direct costs associated with these programs are recognized in Pharmacy and other service costs, and other related expenses are recorded as incurred in Selling, general and administrative expenses.
The Company earns fees from our Pharmacy Rebate Program services. These services include either our formulary rebate administrative service arrangements or our formulary processing arrangements. Formulary rebate administrative services may include formulary consultation, administration of rebate contracts, rebate submission, collection from drug manufacturers and the distribution of rebates to clients. Services may also include facilitating audits of data submissions and reporting of rebates to clients. Clients agree to pay administrative fees that are billed, due and recognized at contracted rates as services are performed. These revenues are reported gross in Fees and other revenues and associated costs are reported in Pharmacy and other service costs in the Consolidated Statements of Income. For certain other clients in our formulary processing arrangements, the Company does not control the right to retain rebates before they are transferred to the client for services performed. Clients agree to allow the Company to retain a portion of each rebate collected in exchange for formulary processing services provided. These rebate and administrative fee revenues are reported net in Fees and other revenues in the Consolidated Statements of Income. Revenue is recognized as rebates are processed.
The Company also earns fees by providing health benefit management solutions that drive cost reductions and improve quality outcomes. Clients are primarily sponsors of health benefit plans and fees may be stated as a per-member-per-month fee or as a per-claim fee. The Company considers the services to be a single performance obligation to stand ready to provide utilization management services over the contract period (generally three years). In certain arrangements, the Company assumes the financial obligation for third-party provider costs for medical services provided to the health plan's customers. Fees are recorded gross in Fees and other revenues in the Consolidated Statements of Income because the Company is acting as a principal in arranging for and controlling the services provided by third-party network providers. Contractual fees vary based on enrollment and provider costs and are billed, due and recognized monthly. Direct costs associated with these programs are recognized in Pharmacy and other service costs, and other related expenses are recorded in Selling, general and administrative expenses as incurred.
Certain health benefit management contracts require the Company to share the results of medical cost experience that differ from specified targets. This variable consideration is estimated at contract inception and adjusted through the contract period. The estimated profits and costs are recognized net in Fees and other revenues.
The Company also earns other service fees related to administrating services to specialty pharmacy manufacturers that are recorded in Fees and other revenues in the Consolidated Statements of Income. These revenues are billed, due and recognized at contracted rates as services are provided.
Note 3 – Accounts Receivable, Net
Accounting policy. The allowance for expected credit losses for current accounts receivable is based primarily on past collections experience relative to the length of time receivables are past due; however, when available evidence reasonably supports an assumption that counterparty credit risk over the expected payment period will differ from current and historical payment collections, a forecasting adjustment is reflected in the allowance for expected credit losses.
All other (non-credit) allowances are based on the current status of each customer's receivable balance, current economic and market conditions and a variety of other factors, including the length of time the receivables are past due, the financial health of customers and our past experience.
We bill pharmaceutical manufacturers based on management's interpretation of contractual terms and estimate a contractual allowance based on the best information available at the time a claim is processed. Contractual allowances for certain rebates receivable from pharmaceutical manufacturers are determined by reviewing payment experience and specific known items that could be adjusted under
92
contract terms. The Company's estimation process for contractual allowances for pharmaceutical manufacturer receivables generally results in an allowance for balances outstanding greater than 90 days.
Contractual allowances for certain receivables from third-party payors are based on their contractual terms and are estimates based on the Company's best information available at the time revenue is recognized.
Receivables and any associated allowance are written off only when all collection attempts have failed and such amounts are determined unrecoverable. We regularly review the adequacy of these allowances based on a variety of factors, including age of the outstanding receivable and collection history. When circumstances related to specific collection patterns change, estimates of the recoverability of receivables are adjusted.
The Company's accounts receivable include amounts due from clients, third-party payors, customers and pharmaceutical manufacturers, and are presented net of allowances. These balances include:
•Noninsurance customer receivables - amounts due from customers for noninsurance services, primarily pharmacy benefit management and ASO contracts.
•Pharmaceutical manufacturers receivable - amounts due from pharmaceutical manufacturers.
•Insurance customer receivables - amounts due from customers under insurance contracts, primarily premiums receivable and amounts due from CMS.
•Other receivables - all other accounts receivable not defined in the categories above.
The following amounts were included within Accounts receivable, net:
| (In millions) | December 31, 2021 | December 31, 2020 | |||||||||
| Noninsurance customer receivables | $ | 6,274 | $ | 5,534 | |||||||
| Pharmaceutical manufacturers receivable | 5,463 | 4,676 | |||||||||
| Insurance customer receivables | 2,932 | 1,789 | |||||||||
| Other receivables | 456 | 192 | |||||||||
| Total | 15,125 | ||||||||||
| Accounts receivable, net classified as Assets of businesses held for sale | (54) | ||||||||||
| Accounts receivable, net per Consolidated Balance Sheets | $ | 15,071 | $ | 12,191 | |||||||
These receivables are reported net of our allowances of $1.4 billion as of December 31, 2021 and $1.2 billion as of December 31, 2020 as follows:
•Included in our Pharmaceutical manufacturers receivable are contractual allowances for certain rebates receivable with pharmaceutical manufacturers of $926 million as of December 31, 2021 and $757 million as of December 31, 2020.
•Included in our Noninsurance customer receivables are contractual allowances from third-party payors of $321 million as of December 31, 2021 and $208 million as of December 31, 2020 based upon the contractual payment terms.
•The remaining allowances of $186 million as of December 31, 2021 and $224 million as of December 31, 2020 include allowances, discounts and claims adjustments issued to customers in the form of client credits, an allowance for current expected credit losses and other non-credit adjustments.
•The Company's allowance for current expected credit losses was $60 million as of December 31, 2021 and $65 million as of December 31, 2020.
93
Note 4 – Mergers, Acquisitions and Divestitures
A.Acquisition of MDLIVE
On April 19, 2021, Cigna acquired 97% of MDLIVE, Inc. ("MDLIVE"), a 24/7 virtual care platform. Combined with Cigna's previously held equity investment, Cigna now owns 100% of MDLIVE. The acquisition of MDLIVE will enable Cigna's Evernorth segment to continue expanding access to virtual care and delivering a more affordable, convenient and connected care experience for consumers.
The purchase price of $2.0 billion consisted of cash consideration. In accordance with GAAP, the total consideration transferred has been allocated to the tangible and intangible net assets acquired based on management's preliminary estimates of their fair values and may change as additional information becomes available over the next several months. As of December 31, 2021, the Company made immaterial measurement period adjustments to the purchase price allocation. The estimated fair values of assets acquired and liabilities assumed as of the closing date were as follows:
| (In millions) | |||||
| Goodwill | $ | 1,438 | |||
| Acquired intangible assets | 627 | ||||
| Tangible assets acquired net of liabilities assumed | 17 | ||||
| Total consideration transferred | 2,082 | ||||
| Less: Fair value to Cigna's previously held equity interest | (55) | ||||
| Total purchase price | $ | 2,027 | |||
Substantially all of the goodwill is assigned to the Evernorth segment ($1.3 billion). Goodwill is not deductible for federal income tax purposes. The acquired intangible assets primarily consist of customer relationships ($577 million) as well as internal-use software, provider networks and a trade name. The fair value of the customer relationships and the amortization period were determined using an income approach that relies heavily on projected future net cash flows including key assumptions for customer attrition, margins and discount rates. The customer relationship intangible asset is amortized over a period of 17 years in a pattern that reflects when Cigna expects to receive the benefits of the related cash flows.
The results of MDLIVE have been included in the Company's Consolidated Financial Statements from the date of the acquisition. Revenues from MDLIVE and their results of operations were not material to Cigna's consolidated results of operations for the year ended December 31, 2021. The pro forma effects of this acquisition for current and prior periods were not material to our consolidated results of operations.
B.Divestiture of U.S. Group Disability and Life business
On December 31, 2020, Cigna completed the sale of its U.S. Group Disability and Life business to New York Life Insurance Company for cash proceeds of $6.2 billion. The Company recognized a gain of $4.2 billion pre-tax ($3.2 billion after-tax), which included recognition of previously unrealized capital gains on investments sold (see Note 14 for further information).
C.Integration and Transaction-related Costs
In 2021, the Company incurred costs related to the acquisition of MDLIVE, the sale of the U.S. Group Disability and Life business, the terminated merger with Anthem, Inc. ("Anthem") and the pending Chubb Transaction (see Note 5 for further information on assets and liabilities of businesses held for sale). In 2020 and 2019, the Company incurred costs related to the acquisition and integration of Express Scripts Holding Company ("Express Scripts"), the terminated merger with Anthem, the sale of the U.S. Group Disability and Life insurance business and other transactions. These costs were $169 million pre-tax ($71 million after-tax) for the year ended December 31, 2021, compared with $527 million pre-tax ($404 million after-tax) for the year ended December 31, 2020 and $552 million pre-tax ($427 million after-tax) for the year ended December 31, 2019. These costs consisted primarily of certain projects to integrate or separate the Company's systems, products and services, fees for legal, advisory and other professional services and certain employment-related costs. After-tax costs for the year ended December 31, 2021 included a tax benefit from the resolution of a tax matter related to the sold Group Disability and Life business.
94
Note 5 – Assets and Liabilities of Businesses Held for Sale
Accounting Policy. The Company classifies assets and liabilities as held for sale ("disposal group") when management commits to a plan to sell the disposal group, the sale is probable within one year and the disposal group is available for immediate sale in its present condition. The Company considers various factors, particularly whether actions required to complete the plan indicate it is unlikely that significant changes to the plan will be made or the plan will be withdrawn. Assets held for sale are measured at the lower of carrying value or fair value less costs to sell. Any loss resulting from the measurement is recognized in the period the held-for-sale criteria are met. Conversely, gains are not recognized until the date of the sale. When the disposal group is classified as held for sale, depreciation and amortization for most long-lived assets ceases and the Company tests the assets for impairment. Deferred policy acquisition costs continue to be amortized.
Cigna entered into a definitive agreement in October 2021 to sell its life, accident and supplemental benefits businesses in seven countries to Chubb for $5.75 billion cash. Subject to applicable regulatory approvals and customary closing conditions, we expect to complete the sale of our life, accident and supplemental benefits businesses in Hong Kong, Indonesia, New Zealand, South Korea, Taiwan, Thailand and our interest in a joint venture in Turkey in the second quarter of 2022. The Company believes this sale is probable and has aggregated and classified the assets and liabilities directly associated with the pending sale as held for sale and has reported them separately on our Consolidated Balance Sheets as of December 31, 2021. The assets and liabilities of businesses held for sale were as follows:
| (In millions) | December 31, 2021 | ||||
| Cash and cash equivalents | $ | 406 | |||
| Investments | 5,109 | ||||
| Deferred policy acquisition costs | 2,755 | ||||
| Separate account assets | 878 | ||||
| Goodwill, other intangible assets and all other assets | 909 | ||||
| Total assets of business held for sale | 10,057 | ||||
| Insurance and contractholder liabilities | 4,644 | ||||
| Accounts payable, accrued expenses and other liabilities | 452 | ||||
| Deferred tax liabilities, net | 449 | ||||
| Separate account liabilities | 878 | ||||
| Total liabilities of business held for sale | $ | 6,423 | |||
The held for sale businesses reported Redeemable noncontrolling interests of $24 million, Gross unrealized appreciation on securities and derivatives of $137 million and Gross translation loss on foreign currencies of $209 million on our Consolidated Balance Sheets as of December 31, 2021.
95
Note 6 – Earnings Per Share ("EPS")
Accounting policy. The Company computes basic earnings per share using the weighted-average number of unrestricted common and deferred shares outstanding. Diluted earnings per share also includes the dilutive effect of outstanding employee stock options and restricted stock using the treasury stock method and the effect of strategic performance shares.
Basic and diluted earnings per share were computed as follows:
| 2021 | 2020 | 2019 | |||||||||||||||||||||||||||||||||||||||||||||||||||
| (Shares in thousands, dollars in millions, except per share amounts) | Basic | Effect of Dilution | Diluted | Basic | Effect of Dilution | Diluted | Basic | Effect of Dilution | Diluted | ||||||||||||||||||||||||||||||||||||||||||||
| Shareholders' net income | $ | 5,365 | $ | 5,365 | $ | 8,458 | $ | 8,458 | $ | 5,104 | $ | 5,104 | |||||||||||||||||||||||||||||||||||||||||
| Shares: | |||||||||||||||||||||||||||||||||||||||||||||||||||||
| Weighted average | 337,962 | 337,962 | 364,979 | 364,979 | 375,919 | 375,919 | |||||||||||||||||||||||||||||||||||||||||||||||
| Common stock equivalents | 3,004 | 3,004 | 3,410 | 3,410 | 3,898 | 3,898 | |||||||||||||||||||||||||||||||||||||||||||||||
| Total shares | 337,962 | 3,004 | 340,966 | 364,979 | 3,410 | 368,389 | 375,919 | 3,898 | 379,817 | ||||||||||||||||||||||||||||||||||||||||||||
| EPS | $ | 15.87 | $ | (0.14) | $ | 15.73 | $ | 23.17 | $ | (0.21) | $ | 22.96 | $ | 13.58 | $ | (0.14) | $ | 13.44 | |||||||||||||||||||||||||||||||||||
The following outstanding employee stock options were not included in the computation of diluted earnings per share because their effect was anti-dilutive:
| (In millions) | 2021 | 2020 | 2019 | |||||||||||||||||
| Anti-dilutive options | 1.5 | 4.1 | 3.5 | |||||||||||||||||
96
Note 7 – Debt
The outstanding amounts of debt and finance leases were as follows:
| (In millions) | December 31, 2021 | December 31, 2020 | ||||||||||||
| Short-term debt | ||||||||||||||
| Commercial paper | $ | 2,027 | $ | 1,030 | ||||||||||
$500 million, 3.05% Notes due 11/2022 | 495 | — | ||||||||||||
| Other, including finance leases | 23 | 18 | ||||||||||||
$78 million, 6.37% Notes due 6/2021 | — | 78 | ||||||||||||
$1,000 million, Floating Rate Notes due 9/2021 | — | 999 | ||||||||||||
$1,250 million, 3.4% Notes due 9/2021 | — | 1,249 | ||||||||||||
| Total short-term debt | $ | 2,545 | $ | 3,374 | ||||||||||
| Long-term debt | ||||||||||||||
$277 million, 4% Notes due 2022 | $ | — | $ | 276 | ||||||||||
$973 million, 3.9% Notes due 2022 | — | 972 | ||||||||||||
$500 million, 3.05% Notes due 2022 | — | 490 | ||||||||||||
$17 million, 8.3% Notes due 2023 | 17 | 17 | ||||||||||||
$63 million, 7.65% Notes due 2023 | 63 | 63 | ||||||||||||
$700 million, Floating Rate Notes due 2023 | 699 | 698 | ||||||||||||
$1,000 million, 3% Notes due 2023 | 985 | 975 | ||||||||||||
$1,187 million, 3.75% Notes due 2023 | 1,185 | 2,181 | ||||||||||||
$500 million, 0.613% Notes due 2024 | 498 | — | ||||||||||||
$1,000 million, 3.5% Notes due 2024 | 983 | 977 | ||||||||||||
$900 million, 3.25% Notes due 2025 | 897 | 896 | ||||||||||||
$2,200 million, 4.125% Notes due 2025 | 2,193 | 2,191 | ||||||||||||
$1,500 million, 4.5% Notes due 2026 | 1,504 | 1,505 | ||||||||||||
$800 million, 1.25% Notes due 2026 | 796 | — | ||||||||||||
$1,500 million, 3.4% Notes due 2027 | 1,423 | 1,410 | ||||||||||||
$259 million, 7.875% Debentures due 2027 | 259 | 259 | ||||||||||||
$600 million, 3.05% Notes due 2027 | 596 | 595 | ||||||||||||
$3,800 million, 4.375% Notes due 2028 | 3,782 | 3,780 | ||||||||||||
$1,500 million, 2.4% Notes due 2030 | 1,490 | 1,489 | ||||||||||||
$1,500 million, 2.375% Notes due 2031 (1) | 1,500 | — | ||||||||||||
$45 million, 8.3% Step Down Notes due 2033 | 45 | 45 | ||||||||||||
$190 million, 6.15% Notes due 2036 | 190 | 190 | ||||||||||||
$2,200 million, 4.8% Notes due 2038 | 2,192 | 2,180 | ||||||||||||
$750 million, 3.2% Notes due 2040 | 743 | 742 | ||||||||||||
$121 million, 5.875% Notes due 2041 | 119 | 119 | ||||||||||||
$448 million, 6.125% Notes due 2041 | 490 | 490 | ||||||||||||
$317 million, 5.375% Notes due 2042 | 315 | 315 | ||||||||||||
$1,500 million, 4.8% Notes due 2046 | 1,465 | 1,465 | ||||||||||||
$1,000 million, 3.875% Notes due 2047 | 988 | 988 | ||||||||||||
$3,000 million, 4.9% Notes due 2048 | 2,967 | 2,966 | ||||||||||||
$1,250 million, 3.4% Notes due 2050 | 1,236 | 1,235 | ||||||||||||
$1,500 million , 3.4% Notes due 2051 | 1,477 | — | ||||||||||||
| Other, including finance leases | 28 | 36 | ||||||||||||
| Total long-term debt | $ | 31,125 | $ | 29,545 | ||||||||||
(1) The Company has entered into interest rate swap contracts hedging a portion of these fixed-rate debt instruments. See Note 11 for further information about the Company's interest rate risk management and these derivative instruments.
97
Debt Issuance and Redemption. In order to decrease future interest expense, mitigate future refinancing risk and raise proceeds for general corporate purposes, the Company entered into the following transactions during 2021:
•Debt issuance: On March 3, 2021, the Company issued $4.3 billion of new senior notes. The proceeds of this issuance were mainly used to redeem outstanding debt securities. The remaining proceeds are available for general corporate purposes. Interest on this debt is paid semi-annually.
| Principal | Maturity Date | Interest Rate | Net Proceeds | |||||||||||||||||
$500 million (1) | March 15, 2024 | 0.613% | $499 million | |||||||||||||||||
$800 million (2) | March 15, 2026 | 1.250% | $797 million | |||||||||||||||||
$1,500 million (3) | March 15, 2031 | 2.375% | $1,492 million | |||||||||||||||||
$1,500 million (4) | March 15, 2051 | 3.400% | $1,479 million | |||||||||||||||||
(1) Redeemable at any time discounted at the U.S. Treasury rate plus 7.5 basis points. Redeemable at par on or after March 15, 2022.
(2) Redeemable at any time discounted at the U.S. Treasury rate plus 10 basis points. Redeemable at par on or after February 15, 2026.
(3) Redeemable at any time discounted at the U.S. Treasury rate plus 15 basis points. Redeemable at par on or after December 15, 2030.
(4) Redeemable at any time discounted at the U.S. Treasury rate plus 20 basis points. Redeemable at par on or after September 15, 2050.
•Debt redemption: During 2021, the Company completed the redemption of a total of $4.5 billion in aggregate principal amount of certain of its outstanding debt securities. The Company recorded a pre-tax loss of $141 million ($110 million after-tax), consisting primarily of premium payments.
Revolving Credit Agreements. Our revolving credit agreements provide us with the ability to borrow amounts for general corporate purposes, including for the purpose of providing liquidity support if necessary under our commercial paper program discussed below. As of December 31, 2021, there were no outstanding balances under these revolving credit agreements.
In April 2021, Cigna entered into a $3.0 billion five-year revolving credit and letter of credit agreement that matures in April 2026 and a $1.0 billion three-year revolving credit agreement that matures in April 2024, which are diversified among 23 banks and replaced the five-year revolving credit and letter of credit agreement that was scheduled to mature in April 2023. Under the current agreements, Cigna can borrow up to $3.0 billion and $1.0 billion, respectively, for general corporate purposes, with up to $500 million available under the five-year facility for issuance of letters of credit. The revolving credit agreements also include an option to extend the termination date for an additional one-year period, subject to consent of the banks.
Additionally, in April 2021, Cigna entered into a $1.0 billion 364-day revolving credit agreement that will mature in April 2022 and is diversified among 23 banks. This agreement replaced the prior $1.0 billion 364-day revolving credit agreement that was scheduled to expire in October 2021. Pursuant to this revolving credit agreement, Cigna can borrow up to $1.0 billion for general corporate purposes. The agreement includes the option to "term out" any revolving loans that are outstanding at maturity by converting them into a term loan maturing on the one-year anniversary of conversion.
Each of the five-year facility, the three-year facility and the 364-day facility include an option to increase commitments in an aggregate amount of up to $1.5 billion across all three facilities. Each of the three facilities also contain customary covenants and restrictions including a financial covenant that the Company's leverage ratio, as defined in the credit agreements, may not exceed 60%, subject to certain exceptions upon the consummation of an acquisition.
Commercial Paper. Under our commercial paper program we may issue short-term, unsecured commercial paper notes privately placed on a discounted basis through certain broker dealers at any time not to exceed an aggregate amount of $5.0 billion. Amounts available under the program may be borrowed, repaid and re-borrowed from time to time. The net proceeds of issuances have been and are expected to be used for general corporate purposes. The commercial paper average interest rate was 0.26% at December 31, 2021.
The Company was in compliance with its debt covenants as of December 31, 2021.
98
Maturities of outstanding long-term debt are as follows:
| (In millions) | Scheduled Maturities (1) | ||||
| 2022 | $ | 500 | |||
| 2023 | $ | 2,967 | |||
| 2024 | $ | 1,500 | |||
| 2025 | $ | 3,100 | |||
| 2026 | $ | 2,300 | |||
| Maturities after 2026 | $ | 21,481 | |||
(1) Long-term debt maturity amounts include current maturities of long-term debt.
Interest expense on long-term and short-term debt was $1.3 billion in 2021, $1.4 billion in 2020 and $1.6 billion in 2019.
Note 8 – Common and Preferred Stock
Cigna has a total of 25 million shares of $1 par value preferred stock authorized for issuance. No shares of preferred stock were outstanding at December 31, 2021, 2020 or 2019.
The following table presents the share activity of Cigna for the years ended December 31, 2021, 2020 and 2019:
| (Shares in thousands) | 2021 | 2020 | 2019 | ||||||||||||||
Common: Par value $0.01; 600,000 shares authorized | |||||||||||||||||
| Outstanding- January 1, | 354,771 | 372,531 | 380,924 | ||||||||||||||
| Net issued for stock option exercises and other benefit plans | 3,375 | 4,142 | 3,413 | ||||||||||||||
| Repurchased common stock | (35,198) | (21,902) | (11,806) | ||||||||||||||
| Outstanding- December 31, | 322,948 | 354,771 | 372,531 | ||||||||||||||
| Treasury stock | 71,246 | 35,505 | 13,012 | ||||||||||||||
| Issued- December 31, | 394,194 | 390,276 | 385,543 | ||||||||||||||
Dividends
In 2021, Cigna initiated and declared quarterly cash dividends of $1.00 per share of Cigna common stock. Cigna currently intends to pay regular quarterly dividends, with future declarations subject to approval by its Board of Directors and the Board's determination that the declaration of dividends remains in the best interests of Cigna and its shareholders. The decision of whether to pay future dividends and the amount of any such dividends will be based on the Company's financial position, results of operations, cash flows, capital requirements, the requirements of applicable law and any other factors the Board of Directors may deem relevant. On February 3, 2022, the Board of Directors declared a quarterly cash dividend of $1.12 per share of Cigna common stock to be paid on March 27, 2022 to shareholders of records on March 9, 2022.
The following table provides details of Cigna's dividend payments:
| Record Date | Payment Date | Amount per Share | Total Amount Paid (in millions) | ||||||||
| 2021 | |||||||||||
| March 10, 2021 | March 25, 2021 | $1.00 | $345 | ||||||||
| June 8, 2021 | June 23, 2021 | $1.00 | $342 | ||||||||
| September 8, 2021 | September 23, 2021 | $1.00 | $330 | ||||||||
| December 7, 2021 | December 22, 2021 | $1.00 | $324 | ||||||||
| 2020 | |||||||||||
| March 10, 2020 | April 9, 2020 | $0.04 | $15 | ||||||||
| 2019 | |||||||||||
| March 11, 2019 | April 10, 2019 | $0.04 | $15 | ||||||||
99
Accelerated Share Repurchase Agreements
On August 23, 2021, as part of our existing share repurchase program, we entered into separate accelerated share repurchase agreements ("ASR agreements") with Morgan Stanley & Co. LLC and JP Morgan Chase Bank, N.A. (collectively, the "Counterparties") to repurchase $2.0 billion of common stock in aggregate. On August 24, 2021, in accordance with the ASR agreements we remitted $2.0 billion to the Counterparties and received an initial delivery of 7.7 million shares of our common stock. We recorded the payments to the Counterparties as a reduction to stockholders' equity, consisting of a $1.6 billion increase in treasury stock, which reflects the value of the initial 7.7 million shares received upon initial settlement and a $400 million decrease in Additional paid-in capital, which reflects the value of the stock held back by the Counterparties pending final settlement of the agreements.
Upon final settlement of the ASR agreements on November 29, 2021 and December 1, 2021, we received an additional 1.8 million shares of our common stock for no additional consideration as the value of this stock was held back by the Counterparties pending final settlement of the agreements. The total number of shares of our common stock repurchased under the ASR agreements was 9.5 million based on an average daily volume weighted-average share price of our common stock during the term of the agreements, less a discount, of $209.53. In addition, we reclassified the $400 million recorded in Additional paid-in capital to Treasury stock upon settlement.
Note 9 – Insurance and Contractholder Liabilities
A.Account Balances – Insurance and Contractholder Liabilities
The Company's insurance and contractholder liabilities were comprised of the following:
| December 31, 2021 | December 31, 2020 | ||||||||||||||||||||||||||||||||||
| (In millions) | Current | Non-current | Total | Current | Non-current | Total | |||||||||||||||||||||||||||||
| Contractholder deposit funds | $ | 352 | $ | 6,702 | $ | 7,054 | $ | 350 | $ | 6,823 | $ | 7,173 | |||||||||||||||||||||||
| Future policy benefits | 312 | 9,194 | 9,506 | 327 | 9,317 | 9,644 | |||||||||||||||||||||||||||||
| Unearned premiums | 558 | 418 | 976 | 485 | 394 | 879 | |||||||||||||||||||||||||||||
| Unpaid claims and claim expenses | |||||||||||||||||||||||||||||||||||
Cigna Healthcare | 4,159 | 102 | 4,261 | 3,608 | 87 | 3,695 | |||||||||||||||||||||||||||||
| Other Operations | 548 | 180 | 728 | 538 | 223 | 761 | |||||||||||||||||||||||||||||
| Total | 5,929 | 16,596 | 22,525 | ||||||||||||||||||||||||||||||||
Insurance and contractholder liabilities classified as Liabilities of businesses held for sale (1) | (611) | (4,033) | (4,644) | ||||||||||||||||||||||||||||||||
| Total insurance and contractholder liabilities | $ | 5,318 | $ | 12,563 | $ | 17,881 | $ | 5,308 | $ | 16,844 | $ | 22,152 | |||||||||||||||||||||||
(1) Amounts classified as Liabilities of businesses held for sale primarily include $3.8 billion of Future policy benefits, $0.4 billion of Unpaid claims and $0.4 billion of Unearned premiums as of December 31, 2021.
Insurance and contractholder liabilities expected to be paid within one year are classified as current.
Accounting Policy - Contractholder Deposit Funds. Liabilities for contractholder deposit funds primarily include deposits received from customers for investment-related and universal life products and investment earnings on their fund balances. These liabilities are adjusted to reflect administrative charges and, for universal life fund balances, mortality charges. In addition, this caption includes: 1) premium stabilization reserves under group health insurance contracts representing experience refunds left with the Company to pay future premiums; 2) deposit administration funds used to fund non-pension retiree insurance programs; 3) retained asset accounts and 4) annuities or supplementary contracts without significant life contingencies. Interest credited on these funds is accrued ratably over the contract period.
Accounting Policy - Future Policy Benefits. Future policy benefits represent the present value of estimated future obligations under long-term life and supplemental health insurance policies and annuity products currently in force. These obligations are estimated using actuarial methods and consist primarily of reserves for annuity contracts, life insurance benefits, GMDB contracts (GMDB contracts are fully reinsured, see Note 10 for additional information) and certain life and accident insurance products of our international businesses to be sold.
Obligations for annuities represent specified periodic benefits to be paid to an individual or groups of individuals over their remaining lives. Obligations for life insurance policies and GMDB contracts represent benefits expected to be paid to policyholders, net of future premiums expected to be received. Management estimates these obligations based on assumptions as to premiums, interest rates, mortality or morbidity, future claim adjudication expenses and surrenders, allowing for adverse deviation as appropriate. Mortality, morbidity and surrender assumptions are based on the Company's own experience and published actuarial tables. Interest rate
100
assumptions are based on management's judgment considering the Company's experience and future expectations and range from 1% to 9%. Obligations for the direct and assumed run-off settlement annuity business include adjustments for realized and unrealized investment returns consistent with GAAP when a premium deficiency exists. As of December 31, 2021, approximately 18% of the liability for future policy benefits was supported by assets held in trust for the benefit of the ceding company under reinsurance agreements.
Accounting Policy - Unearned Premium. The unrecognized portion of premiums received is recorded as unearned premiums included in insurance and contractholder liabilities.
B.Unpaid Claims and Claim Expenses – Cigna Healthcare
This liability reflects estimates of the ultimate cost of claims that have been incurred but not reported, including expected development on reported claims, those that have been reported but not yet paid (reported claims in process) and other medical care expenses and services payable that are primarily comprised of accruals for incentives and other amounts payable to health care professionals and facilities. This liability includes amounts from the International Health businesses now reported in Cigna Healthcare following our change in segment reporting in 2021. Prior year rollforwards have been updated to reflect this segment change.
Accounting policy. The Company uses actuarial principles and assumptions that are consistently applied each reporting period and recognizes the actuarial best estimate of the ultimate liability along with a margin for adverse deviation. This approach is consistent with actuarial standards of practice that the liabilities be adequate under moderately adverse conditions.
The Company compares key assumptions used to establish the medical costs payable to actual experience for each reporting period. The unpaid claims liability is adjusted through current period shareholders' net income when actual experience differs from these assumptions. Additionally, the Company evaluates expected future developments and emerging trends that may impact key assumptions. The process used to determine this liability requires the Company to make critical accounting estimates that involve considerable judgment, reflecting the variability inherent in forecasting future claim payments. These estimates are highly sensitive to changes in the Company's key assumptions, specifically completion factors and medical cost trend.
The liability is primarily calculated using "completion factors" developed by comparing the claim incurral date to the date claims were paid. Completion factors are impacted by several key items including changes in: 1) electronic (auto-adjudication) versus manual claim processing; 2) frequency and timeliness of provider claims submissions; 3) number of customers and 4) the mix of products. The Company uses historical completion factors combined with an analysis of current trends and operational factors to develop current estimates of completion factors. The Company estimates the liability for claims incurred in each month by applying the current estimates of completion factors to the current paid claims data. This approach implicitly assumes that historical completion rates will be a useful indicator for the current period.
The Company relies more heavily on medical cost trend analysis that reflects expected claim payment patterns and other relevant operational considerations for more recent months. Medical cost trend is primarily impacted by medical service utilization and unit costs that are affected by changes in the level and mix of health benefits offered, including inpatient, outpatient and pharmacy, the impact of copays and deductibles, changes in provider practices and changes in consumer demographics and consumption behavior.
The total of incurred but not reported liabilities plus expected development on reported claims, including reported claims in process, was $4.0 billion at December 31, 2021 and $3.4 billion at December 31, 2020.
101
Activity, net of intercompany transactions, in the unpaid claims liability for the Cigna Healthcare segment for the years ended December 31 was as follows:
| (In millions) | 2021 | 2020 | 2019 | ||||||||||||||
| Beginning balance | $ | 3,695 | $ | 3,336 | $ | 3,090 | |||||||||||
| Less: Reinsurance and other amounts recoverable | 237 | 318 | 280 | ||||||||||||||
| Beginning balance, net | 3,458 | 3,018 | 2,810 | ||||||||||||||
| Incurred costs related to: | |||||||||||||||||
| Current year | 31,755 | 27,494 | 26,026 | ||||||||||||||
| Prior years | (219) | (144) | (180) | ||||||||||||||
| Total incurred | 31,536 | 27,350 | 25,846 | ||||||||||||||
| Paid costs related to: | |||||||||||||||||
| Current year | 27,929 | 24,187 | 23,176 | ||||||||||||||
| Prior years | 3,065 | 2,723 | 2,462 | ||||||||||||||
| Total paid | 30,994 | 26,910 | 25,638 | ||||||||||||||
| Ending balance, net | 4,000 | 3,458 | 3,018 | ||||||||||||||
| Add: Reinsurance and other amounts recoverable | 261 | 237 | 318 | ||||||||||||||
| Ending balance | $ | 4,261 | $ | 3,695 | $ | 3,336 | |||||||||||
Reinsurance and other amounts recoverable reflect amounts due from reinsurers and policyholders to cover incurred but not reported and pending claims of certain business for which the Company administers the plan benefits without any right of offset. See Note 10 for additional information on reinsurance.
Variances in incurred costs related to prior years' unpaid claims and claim expenses that resulted from the differences between actual experience and the Company's key assumptions for the years ended December 31 were as follows:
| (Dollars in millions) | 2021 | 2020 | ||||||||||||||||||||||||
| $ | % (1) | $ | % (2) | |||||||||||||||||||||||
| Actual completion factors | $ | 81 | 0.3 | % | $ | 57 | 0.2 | % | ||||||||||||||||||
| Medical cost trend | 138 | 0.5 | 87 | 0.4 | ||||||||||||||||||||||
| Total favorable variance | $ | 219 | 0.8 | % | $ | 144 | 0.6 | % | ||||||||||||||||||
(1) Percentage of current year incurred costs as reported for the year ended December 31, 2020.
(2) Percentage of current year incurred costs as reported for the year ended December 31, 2019.
Favorable prior year development in both years reflects lower than expected utilization of medical services as compared to our assumptions.
102
The following table depicts the incurred and paid claims development as of December 31, 2021 (net of reinsurance), claims frequency metrics and incurred but not reported liabilities reported in the Cigna Healthcare segment. The information about incurred and paid claims development for the year ended December 31, 2020 is presented as supplementary information and is unaudited.
| Incurred Costs | ||||||||||||||
| Incurral Year | 2020 (Unaudited) | 2021 | Unpaid Claims & Claim Expenses | Claims Frequency | ||||||||||
| (In millions) | ||||||||||||||
| 2020 | $ | 26,532 | $ | 26,332 | 156 | 4.7 | million | |||||||
| 2021 | 30,735 | 3,696 | 5.1 | million | ||||||||||
| Cumulative incurred costs for the periods presented | $ | 57,067 | ||||||||||||
| Cumulative Costs Paid | ||||||||||||||
| Incurral Year | 2020 (Unaudited) | 2021 | ||||||||||||
| (In millions) | ||||||||||||||
| 2020 | $ | 23,347 | $ | 26,176 | ||||||||||
| 2021 | 27,039 | |||||||||||||
| Cumulative paid costs for the periods presented | $ | 53,215 | ||||||||||||
| Outstanding liabilities for the periods presented, net of reinsurance | $ | 3,852 | ||||||||||||
| Other long-duration liabilities not included in development table above | 148 | |||||||||||||
Net unpaid claims and claims expenses - Cigna Healthcare | 4,000 | |||||||||||||
| Reinsurance and other amounts recoverable | 261 | |||||||||||||
Unpaid claims and claim expenses - Cigna Healthcare | $ | 4,261 | ||||||||||||
More than 95% of health claims incurred in a calendar year are paid within one year of their incurred date.
There is no single or common claim frequency metric used in the health care industry. The Company believes a relevant metric for its health insurance business is the number of customers for whom an insured medical claim was paid. Customers for whom no insured medical claim was paid are excluded from the calculation. Claims that did not result in a liability are not included in the frequency metric.
C.Unpaid Claims and Claim Expenses – Other Operations
Accounting policy. Liabilities for unpaid claims and claim expenses are established by book of business within Other Operations including the international businesses to be sold. Unpaid claims and claim expenses within the Other Operations consist of (1) case or claims reserves for reported claims that are unpaid as of the balance sheet date; (2) incurred but not reported reserves for claims when the insured event has occurred but has not been reported to the Company and (3) loss adjustment expense reserves for the expected costs of settling these claims. The Company consistently estimates incurred but not yet reported losses using actuarial principles and assumptions based on historical and projected claim incidence patterns, claim size and the expected payment period. The Company recognizes the actuarial best estimate of the ultimate liability within a level of confidence, consistent with actuarial standards of practice that the liabilities be adequate under moderately adverse conditions. The Company immediately records an adjustment in Medical costs and other benefit expenses when estimates of these liabilities change.
See Note 4 for a discussion of the divestiture of the Group Disability and Life business on December 31, 2020. Prior to the sale, the liabilities for unpaid claims and claim expenses in the Group Disability and Life business reflected reserves for long-term and short-term disability, life insurance and accident products. The majority of the unpaid claim liability related to disability claims that was measured as the present value of estimated future benefit payments, including expected development, for each reported claim that was receiving benefit payments over the expected disability period or pending a decision on eligibility for benefits.
103
Liability balance details. The liability details for unpaid claims and claim expenses are as follows. The liability no longer includes the International Health businesses now reported in Cigna Healthcare following our change in segment reporting. Prior year rollforwards have been updated to reflect the segment change.
| (In millions) | December 31, 2021 | December 31, 2020 | ||||||
Other Operations | ||||||||
| International businesses to be sold | $ | 447 | $ | 452 | ||||
| Other Operations | 281 | 309 | ||||||
Unpaid claims and claim expenses Other Operations | 728 | 761 | ||||||
Activity in the unpaid claims and claim expenses for international businesses held for sale and, prior to the sale, Group Disability and Life (see Note 4 for further information) is presented in the following table. Liabilities associated with Other Operations are excluded because they pertain to obligations for long-duration insurance contracts or, if short-duration, the liabilities have been largely reinsured.
| (In millions) | 2021 (1) | 2020 | 2019 | ||||||||||||||
| Beginning balance | $ | 452 | $ | 5,372 | $ | 5,039 | |||||||||||
| Less: Reinsurance | 45 | 169 | 140 | ||||||||||||||
| Beginning balance, net | 407 | 5,203 | 4,899 | ||||||||||||||
| Incurred claims related to: | |||||||||||||||||
| Current year | 982 | 4,205 | 3,958 | ||||||||||||||
| Prior years: | |||||||||||||||||
| Interest accretion | — | 154 | 152 | ||||||||||||||
| All other incurred | 11 | 48 | (25) | ||||||||||||||
| Total incurred | 993 | 4,407 | 4,085 | ||||||||||||||
| Paid claims related to: | |||||||||||||||||
| Current year | 738 | 2,392 | 2,163 | ||||||||||||||
| Prior years | 227 | 1,690 | 1,607 | ||||||||||||||
| Total paid | 965 | 4,082 | 3,770 | ||||||||||||||
| Foreign currency | (34) | 21 | (11) | ||||||||||||||
Divestiture of Group Disability and Life business (2) | — | (5,142) | — | ||||||||||||||
| Ending balance, net | 401 | 407 | 5,203 | ||||||||||||||
| Add: Reinsurance | 46 | 45 | 169 | ||||||||||||||
Ending balance | $ | 447 | $ | 452 | $ | 5,372 | |||||||||||
(1) Includes unpaid claims amounts classified as Liabilities of businesses held for sale.
(2) Includes Group Disability and Life reserves sold or reinsured to New York Life Insurance Company as part of the sale of the Group Disability and Life business and immaterial retained balances which are now excluded from this table.
Reinsurance in the table above reflects amounts due from reinsurers related to unpaid claims liabilities. See Note 10 for additional information on reinsurance.
Note 10 – Reinsurance
The Company's insurance subsidiaries enter into agreements with other insurance companies to limit losses from large exposures and to permit recovery of a portion of incurred losses. Reinsurance is ceded primarily in acquisition and disposition transactions when the underwriting company is not being acquired. Reinsurance does not relieve the originating insurer of liability. Therefore, reinsured liabilities must continue to be reported along with the related reinsurance recoverables. The Company regularly evaluates the financial condition of its reinsurers and monitors concentrations of its credit risk.
104
A.Reinsurance Recoverables
Accounting policy. Reinsurance recoverables represent amounts due from reinsurers for both paid and unpaid claims of the Company's insurance businesses. The Company bears the risk of loss if its reinsurers and retrocessionaires do not meet or are unable to meet their reinsurance obligations to the Company. Most reinsurance recoverables are classified as non-current assets. The current portion of reinsurance recoverables is reported in Other current assets and consists primarily of recoverables on paid claims expected to be settled within one year. Reinsurance recoverables are presented net of allowances, consisting primarily of an allowance for expected credit losses which is recognized on reinsurance recoverable balances each period and adjusted through benefits expense. Estimates of the allowance for expected credit losses are based on internal and external data used to develop expected loss rates over the anticipated duration of the recoverable asset that vary by external credit rating and collateral level.
The majority of the Company's reinsurance recoverables resulted from acquisition and disposition transactions in which the underwriting company was not acquired. Included in the table below are $129 million of current reinsurance recoverables that are reported in Other current assets as of December 31, 2021; as of December 31, 2020 there were $217 million of current reinsurance recoverables reported in Other current assets. The Company's reinsurance recoverables as of December 31, 2021 are presented in the following table by range of external credit rating and collateral level:
| (In millions) | Fair value of collateral contractually required to meet or exceed carrying value of recoverable | Collateral provisions exist that may mitigate risk of credit loss (2) | No collateral | Total | ||||||||||||||||||||||
| Ongoing Operations | ||||||||||||||||||||||||||
A-A A- equivalent and higher current ratings (1) | $ | — | $ | — | $ | 172 | $ | 172 | ||||||||||||||||||
BBB BBB- to BBB+ equivalent current credit ratings (1) | — | — | 61 | 61 | ||||||||||||||||||||||
| Not rated | 103 | 1 | 35 | 139 | ||||||||||||||||||||||
Total recoverables related to ongoing operations (3) | 103 | 1 | 268 | 372 | ||||||||||||||||||||||
| Acquisition, disposition or runoff activities | ||||||||||||||||||||||||||
A- equivalent and higher current ratings (1) | ||||||||||||||||||||||||||
| Lincoln National Life and Lincoln Life & Annuity of New York | — | 2,935 | — | 2,935 | ||||||||||||||||||||||
| Berkshire Hathaway Life Insurance Company of Nebraska | 276 | 370 | — | 646 | ||||||||||||||||||||||
| Prudential Retirement Insurance and Annuity | 565 | — | — | 565 | ||||||||||||||||||||||
| Life Insurance Company of North America | — | 437 | — | 437 | ||||||||||||||||||||||
| Other | 220 | 17 | 17 | 254 | ||||||||||||||||||||||
| Not rated | — | 12 | 3 | 15 | ||||||||||||||||||||||
| Total recoverables related to acquisition, disposition or runoff activities | 1,061 | 3,771 | 20 | 4,852 | ||||||||||||||||||||||
| Total | $ | 1,164 | $ | 3,772 | $ | 288 | $ | 5,224 | ||||||||||||||||||
| Allowance for uncollectible reinsurance | (30) | |||||||||||||||||||||||||
Total reinsurance recoverables (3) | $ | 5,194 | ||||||||||||||||||||||||
(1) Certified by a nationally recognized statistical rating organization ("NRSRO").
(2) Includes collateral provisions requiring the reinsurer to fully collateralize its obligation if its external credit rating is downgraded to a specified level.
(3) Includes $95 million of recoverables classified as Assets of businesses held for sale.
Collateral levels are defined internally based on the fair value of the collateral relative to the carrying amount of the reinsurance recoverable, the frequency at which collateral is required to be replenished and the potential for volatility in the collateral's fair value.
105
B.Effects of Reinsurance
The following table presents direct, assumed and ceded premiums for both short-duration and long-duration insurance contracts. It also presents reinsurance recoveries that have been netted against benefit expenses in the Company's Consolidated Statements of Income.
| (In millions) | 2021 | 2020 | 2019 | ||||||||||||||
| Premiums | |||||||||||||||||
| Short-duration contracts | |||||||||||||||||
| Direct | $ | 36,513 | $ | 38,425 | $ | 35,690 | |||||||||||
| Assumed | 335 | 85 | 64 | ||||||||||||||
| Ceded | (148) | (230) | (203) | ||||||||||||||
| Total short-duration contract premiums | 36,700 | 38,280 | 35,551 | ||||||||||||||
| Long-duration contracts | |||||||||||||||||
| Direct | 4,753 | 4,517 | 4,352 | ||||||||||||||
| Assumed | 99 | 99 | 105 | ||||||||||||||
| Ceded | (398) | (269) | (294) | ||||||||||||||
| Total long-duration contract premiums | 4,454 | 4,347 | 4,163 | ||||||||||||||
| Total premiums | $ | 41,154 | $ | 42,627 | $ | 39,714 | |||||||||||
| Total reinsurance recoveries | $ | 552 | $ | 431 | $ | 395 | |||||||||||
C.Effective Exit of GMDB and GMIB Business
The Company entered into an agreement with Berkshire to effectively exit the GMDB and GMIB business via a reinsurance transaction in 2013. Berkshire reinsured 100% of the Company's future claim payments in this business, net of other reinsurance arrangements existing at that time. The reinsurance agreement is subject to an overall limit with approximately $3.2 billion remaining at December 31, 2021.
GMDB is accounted for as assumed and ceded reinsurance and GMIB assets and liabilities are reported as derivatives at fair value as discussed below. GMIB assets are reported in Other current assets and Other assets and GMIB liabilities are reported in Accrued expenses and other liabilities and Other non-current liabilities.
GMDB
The GMDB exposure arises under annuities written by ceding companies that guarantee the benefit received at death. The Company's exposure arises when the guaranteed minimum death benefit exceeds the fair value of the related mutual fund investments at the time of a contractholder's death.
Accounting policy. The Company estimates the gross liability and reinsurance recoverable with an internal model based on the Company's experience and future expectations over an extended period, consistent with the long-term nature of this product. As a result of the reinsurance transaction, reserve increases have a corresponding increase in the recorded reinsurance recoverable, provided the increased recoverable remains within the overall Berkshire limit (including the GMIB asset presented below).
106
The following table presents the account value, net amount at risk and the number of contractholders for guarantees assumed by the Company in the event of death. The net amount at risk is the amount that the Company would have to pay if all contractholders died as of the specified date. The Company should be reimbursed in full for these payments unless the Berkshire reinsurance limit is exceeded.
| (Dollars in millions, excludes impact of reinsurance ceded) | December 31, 2021 | December 31, 2020 | |||||||||
| Account value | $ | 9,795 | $ | 9,523 | |||||||
| Net amount at risk | $ | 1,392 | $ | 1,570 | |||||||
| Average attained age of contractholders (weighted by exposure) | 77 | 77 | |||||||||
| Number of contractholders (estimated) | 170,000 | 185,000 | |||||||||
GMIB
The Company reinsured contracts with issuers of GMIB products. The Company's exposure represents the excess of a contractually guaranteed amount over the level of variable annuity account values. Payment by the Company depends on the actual account value in the related underlying mutual funds and the level of interest rates when the contractholders elect to receive minimum income payments that can only occur within 30 days of a policy anniversary after the appropriate waiting period. The Company has purchased retrocessional coverage ("GMIB assets") for these contracts including retrocessional coverage from Berkshire.
Accounting policy. The Company reports GMIB liabilities and assets as derivatives at fair value because cash flows of these liabilities and assets are affected by equity markets and interest rates, but are without significant life insurance risk and are settled in lump sum payments. The Company receives and pays fees periodically based on either contractholders' account values or deposits increased at a contractual rate. The Company will also pay and receive cash depending on changes in account values and interest rates when contractholders first elect to receive minimum income payments. Cash flows on these contracts are reported in operating activities.
Assumptions used in fair value measurement. GMIB assets and liabilities are established using capital market assumptions and assumptions related to future annuitant behavior (including mortality, lapse and annuity election rates). The Company classifies GMIB assets and liabilities in Level 3 of the fair value hierarchy described in Note 12 because assumptions related to future annuitant behavior are largely unobservable.
The only assumption expected to impact future shareholders' net income is non-performance risk. The non-performance risk adjustment reflects a market participant's view of nonpayment risk by adding an additional spread to the discount rate in the calculation of both (a) the GMIB liabilities to be paid by the Company and (b) the GMIB assets to be paid by the reinsurers, after considering collateral. The impact of non-performance risk was immaterial for the years ended December 31, 2021 and December 31, 2020.
GMIB liabilities totaling $572 million as of December 31, 2021 and $729 million as of December 31, 2020 are classified as Level 3 because fair value inputs are largely unobservable. The GMIB liabilities reflect the Company's credit risk, while the reinsurance recoverable reflects the credit risk of the reinsurers. There were three reinsurers covering 100% of the GMIB exposures as of December 31, 2021 and December 31, 2020 as follows:
| (In millions) | ||||||||||||||||||||||||||
| Line of Business | Reinsurer | December 31, 2021 | December 31, 2020 | Collateral and Other Terms at December 31, 2021 | ||||||||||||||||||||||
| GMIB | Berkshire | $ | 283 | $ | 353 | 100% were secured by assets in a trust. | ||||||||||||||||||||
| Sun Life Assurance Company of Canada | 167 | 215 | ||||||||||||||||||||||||
| Liberty Re (Bermuda) Ltd. | 151 | 190 | 100% were secured by assets in a trust. | |||||||||||||||||||||||
| Total GMIB recoverables reported in Other current assets and Other assets | $ | 601 | $ | 758 | ||||||||||||||||||||||
All reinsurers are rated A- equivalent and higher by an NRSRO.
107
Note 11 – Investments
Cigna's investment portfolio consists of a broad range of investments including debt securities, equity securities, commercial mortgage loans, policy loans, other long-term investments, short-term investments and derivative financial instruments. The sections below provide more detail regarding our investment balances and realized investment gains and losses. See Note 12 for information about the valuation of the Company's investment portfolio.
Debt securities, commercial mortgage loans, derivative financial instruments and short-term investments with contractual maturities during the next twelve months are classified on the balance sheet as current investments, unless they are held as statutory deposits or restricted for other purposes and then they are classified in Long-term investments. Equity securities may include funds that are used in our cash management strategy and are classified as current investments. All other investments are classified as Long-term investments.
The following table summarizes the Company's investments by category and current or long-term classification:
| December 31, 2021 | December 31, 2020 | |||||||||||||||||||||||||||||||||||||
| (In millions) | Current | Long-term | Total | Current | Long-term | Total | ||||||||||||||||||||||||||||||||
| Debt securities | $ | 796 | $ | 16,162 | $ | 16,958 | $ | 959 | $ | 17,172 | $ | 18,131 | ||||||||||||||||||||||||||
| Equity securities | — | 603 | 603 | — | 501 | 501 | ||||||||||||||||||||||||||||||||
| Commercial mortgage loans | 40 | 1,526 | 1,566 | 13 | 1,406 | 1,419 | ||||||||||||||||||||||||||||||||
| Policy loans | — | 1,338 | 1,338 | — | 1,351 | 1,351 | ||||||||||||||||||||||||||||||||
| Other long-term investments | — | 3,574 | 3,574 | — | 2,832 | 2,832 | ||||||||||||||||||||||||||||||||
| Short-term investments | 428 | — | 428 | 359 | — | 359 | ||||||||||||||||||||||||||||||||
| Total | 1,264 | 23,203 | 24,467 | |||||||||||||||||||||||||||||||||||
Investments classified as assets of businesses held for sale (1) | (344) | (4,765) | (5,109) | |||||||||||||||||||||||||||||||||||
| Investments per Consolidated Balance Sheets | $ | 920 | $ | 18,438 | $ | 19,358 | $ | 1,331 | $ | 23,262 | $ | 24,593 | ||||||||||||||||||||||||||
(1) Investments related to the international life, accident and supplemental benefits businesses that are held for sale. These investments are primarily comprised of debt securities and other long-term investments, and to a lesser extent, equity securities and short-term investments. See Note 5 to the Consolidated Financial Statements for additional information.
A.Investment Portfolio
Debt Securities
Accounting policy. Debt securities (including bonds, mortgage and other asset-backed securities and preferred stocks redeemable by the investor) are classified as available for sale and are carried at fair value with changes in fair value recorded either in Accumulated other comprehensive income (loss) within Shareholders' equity or in credit loss expense based on fluctuations in the allowance for credit losses, as further discussed below. Net unrealized appreciation on debt securities supporting the Company's run-off settlement annuity business is reported in Non-current insurance and contractholder liabilities rather than Accumulated other comprehensive income (loss). When the Company intends to sell or determines that it is more likely than not to be required to sell an impaired debt security, the excess of amortized cost over fair value is directly written down with a charge to Realized investment gains and losses. Certain asset-backed securities are considered variable interest entities, see Note 13 for additional information.
The Company reviews declines in fair value from a debt security's amortized cost basis to determine whether a credit loss exists, and when appropriate, recognizes a credit loss allowance with a corresponding charge to credit loss expense, presented in Realized investment gains and losses in the Company's Consolidated Statements of Income. The allowance for credit loss represents the excess of amortized cost over the greater of its fair value or the net present value of the debt security's projected future cash flows (based on qualitative and quantitative factors, including the probability of default and the estimated timing and amount of recovery). Each period, the allowance for credit loss is adjusted as needed through credit loss expense.
The Company does not measure an allowance for credit losses for accrued interest receivables. When interest payments are delinquent based on contractual terms or when certain terms (interest rate or maturity date) of the investment have been restructured, accrued interest, reported in Other current assets, is written off through a charge to Net investment income and interest income is recognized on a cash basis.
108
The amortized cost and fair value by contractual maturity periods for debt securities were as follows at December 31, 2021:
| (In millions) | Amortized Cost | Fair Value | ||||||||||||
| Due in one year or less | $ | 812 | $ | 816 | ||||||||||
| Due after one year through five years | 5,218 | 5,366 | ||||||||||||
| Due after five years through ten years | 5,173 | 5,453 | ||||||||||||
| Due after ten years | 4,067 | 4,805 | ||||||||||||
| Mortgage and other asset-backed securities | 505 | 518 | ||||||||||||
| Total | $ | 15,775 | $ | 16,958 | ||||||||||
Actual maturities of these securities could differ from their contractual maturities used in the table above because issuers may have the right to call or prepay obligations, with or without penalties.
Gross unrealized appreciation (depreciation) on debt securities by type of issuer is shown below:
| (In millions) | Amortized Cost | Allowance for Credit Loss | Unrealized Appreciation | Unrealized Depreciation | Fair Value | |||||||||||||||||||||||||||
| December 31, 2021 | ||||||||||||||||||||||||||||||||
| Federal government and agency | $ | 287 | $ | — | $ | 101 | $ | (1) | $ | 387 | ||||||||||||||||||||||
| State and local government | 154 | — | 17 | — | 171 | |||||||||||||||||||||||||||
| Foreign government | 2,468 | — | 194 | (46) | 2,616 | |||||||||||||||||||||||||||
| Corporate | 12,361 | (23) | 1,008 | (80) | 13,266 | |||||||||||||||||||||||||||
| Mortgage and other asset-backed | 505 | — | 17 | (4) | 518 | |||||||||||||||||||||||||||
| Total | $ | 15,775 | $ | (23) | $ | 1,337 | $ | (131) | $ | 16,958 | ||||||||||||||||||||||
Investments supporting liabilities of the Company's run-off settlement annuity business (included in total above) (1) | $ | 2,262 | $ | (5) | $ | 720 | $ | (10) | $ | 2,967 | ||||||||||||||||||||||
| December 31, 2020 | ||||||||||||||||||||||||||||||||
| Federal government and agency | $ | 334 | $ | — | $ | 122 | $ | — | $ | 456 | ||||||||||||||||||||||
| State and local government | 150 | — | 17 | — | 167 | |||||||||||||||||||||||||||
| Foreign government | 2,201 | — | 318 | (8) | 2,511 | |||||||||||||||||||||||||||
| Corporate | 13,108 | (19) | 1,506 | (33) | 14,562 | |||||||||||||||||||||||||||
| Mortgage and other asset-backed | 427 | (7) | 27 | (12) | 435 | |||||||||||||||||||||||||||
| Total | $ | 16,220 | $ | (26) | $ | 1,990 | $ | (53) | $ | 18,131 | ||||||||||||||||||||||
Investments supporting liabilities of the Company's run-off settlement annuity business (included in total above) (1) | $ | 2,282 | $ | (5) | $ | 838 | $ | (3) | $ | 3,112 | ||||||||||||||||||||||
(1) Net unrealized appreciation for these investments is excluded from accumulated other comprehensive income.
Review of declines in fair value. Management reviews impaired debt securities to determine whether a credit loss allowance is needed based on criteria that include:
•severity of decline;
•financial health and specific prospects of the issuer; and
•changes in the regulatory, economic or general market environment of the issuer's industry or geographic region.
109
The table below summarizes debt securities with a decline in fair value from amortized cost for which an allowance for credit losses has not been recorded, by investment grade and the length of time these securities have been in an unrealized loss position. These debt securities are primarily corporate securities with a decline in fair value that reflects an increase in market yields since purchase. Our allowance for credit losses on debt securities was not material as of December 31, 2021 and December 31, 2020.
| December 31, 2021 | December 31, 2020 | |||||||||||||||||||||||||||||||||||||||||||||||||
| (Dollars in millions) | Fair Value | Amortized Cost | Unrealized Depreciation | Number of Issues | Fair Value | Amortized Cost | Unrealized Depreciation | Number of Issues | ||||||||||||||||||||||||||||||||||||||||||
| One year or less | ||||||||||||||||||||||||||||||||||||||||||||||||||
| Investment grade | $ | 2,785 | $ | 2,861 | $ | (76) | 909 | $ | 1,026 | $ | 1,045 | $ | (19) | 300 | ||||||||||||||||||||||||||||||||||||
| Below investment grade | 561 | 578 | (17) | 781 | 381 | 405 | (24) | 232 | ||||||||||||||||||||||||||||||||||||||||||
| More than one year | ||||||||||||||||||||||||||||||||||||||||||||||||||
| Investment grade | 382 | 412 | (30) | 143 | 18 | 18 | — | 6 | ||||||||||||||||||||||||||||||||||||||||||
| Below investment grade | 162 | 170 | (8) | 53 | 90 | 100 | (10) | 33 | ||||||||||||||||||||||||||||||||||||||||||
| Total | $ | 3,890 | $ | 4,021 | $ | (131) | 1,886 | $ | 1,515 | $ | 1,568 | $ | (53) | 571 | ||||||||||||||||||||||||||||||||||||
Equity Securities
Accounting policy. Equity securities with a readily determinable fair value consist primarily of mutual funds that invest in fixed income debt securities while those without a readily determinable fair value consist of private equity investments. Changes in the fair values of equity securities that have a readily determinable fair value are reported in Net realized investment gains (losses). Equity securities without a readily determinable fair value are carried at cost minus impairment, if any, plus or minus changes resulting from observable price changes.
The following table provides the values of the Company's equity security investments as of December 31, 2021 and December 31, 2020. The amount of impairments or value changes resulting from observable price changes on equity securities still held was not material to the financial statements as of December 31, 2021 or 2020.
| December 31, 2021 | December 31, 2020 | |||||||||||||||||||||||||
| (In millions) | Cost | Carrying Value | Cost | Carrying Value | ||||||||||||||||||||||
| Equity securities with readily determinable fair values | $ | 257 | $ | 207 | $ | 238 | $ | 246 | ||||||||||||||||||
| Equity securities with no readily determinable fair value | 270 | 396 | 225 | 255 | ||||||||||||||||||||||
| Total | $ | 527 | $ | 603 | $ | 463 | $ | 501 | ||||||||||||||||||
As of December 31, 2021, the Company had a commitment to purchase $550 million of equity securities in Bright Health Group, Inc., a technology-enabled health insurance carrier. This transaction was completed in January 2022.
Commercial Mortgage Loans
Accounting policy. Commercial mortgage loans are carried at unpaid principal balances, net of an allowance for expected credit losses, and classified as either current or long-term investments based on their contractual maturities. Changes in the allowance for expected credit losses are recognized as credit loss expense and presented in Realized investment gains and losses in the Company's Consolidated Statements of Income.
Each period, the Company establishes (or adjusts) its allowance for expected credit losses for commercial mortgage loans. The allowance for expected credit losses is based on a credit risk category that is assigned to each loan at origination using key credit quality indicators, including debt service coverage and loan-to-value ratios. Credit risk categories are updated as key credit quality indicators change. An expected loss rate, assigned based on the credit risk category, is applied to each loan's unpaid principal balance to develop the aggregate allowance for expected credit losses. Commercial mortgage loans are considered impaired and written off against the allowance when it is probable that the Company will not collect all amounts due per the terms of the promissory note. In the event of a foreclosure, the allowance for credit losses is based on the excess of the carrying value of the mortgage loan over the fair value of its underlying collateral.
Mortgage loans held by the Company are made exclusively to commercial borrowers and are diversified by property type, location and borrower. Loans are generally issued at fixed rates of interest and are secured by high quality, primarily completed and substantially leased operating properties.
110
Credit quality. The Company regularly evaluates and monitors credit risk, beginning with the initial underwriting of a mortgage loan and continuing throughout the investment holding period. Mortgage origination professionals employ an internal credit quality rating system designed to evaluate the relative risk of the transaction at origination that is then updated each year as part of the annual portfolio loan review. The Company evaluates and monitors credit quality on a consistent and ongoing basis.
Quality ratings are based on our evaluation of a number of key inputs related to the loan, including real estate market-related factors such as rental rates and vacancies, and property-specific inputs such as growth rate assumptions and lease rollover statistics. However, the two most significant contributors to the credit quality rating are the debt service coverage and loan-to-value ratios. The debt service coverage ratio measures the amount of property cash flow available to meet annual interest and principal payments on debt, with a ratio below 1.0 indicating that there is not enough cash flow to cover the required loan payments. The loan-to-value ratio, commonly expressed as a percentage, compares the amount of the loan to the fair value of the underlying property collateralizing the loan.
The following table summarizes the credit risk profile of the Company's commercial mortgage loan portfolio as of December 31, 2021 and December 31, 2020:
| (Dollars in millions) | December 31, 2021 | December 31, 2020 | |||||||||||||||||||||||||||||||||||||||
| Loan-to-Value Ratio | Carrying Value | Average Debt Service Coverage Ratio | Average Loan-to-Value Ratio | Carrying Value | Average Debt Service Coverage Ratio | Average Loan-to-Value Ratio | |||||||||||||||||||||||||||||||||||
| Below 60% | $ | 560 | 2.18 | $ | 533 | 2.28 | |||||||||||||||||||||||||||||||||||
| 60% to 79% | 883 | 1.89 | 751 | 2.08 | |||||||||||||||||||||||||||||||||||||
| 80% to 100% | 129 | 1.47 | 141 | 1.33 | |||||||||||||||||||||||||||||||||||||
| Allowance for credit losses | (6) | (6) | |||||||||||||||||||||||||||||||||||||||
| Total | $ | 1,566 | 1.96 | 61 | % | $ | 1,419 | 2.08 | 61 | % | |||||||||||||||||||||||||||||||
All commercial mortgage loans in the Company's portfolio are current as of December 31, 2021 and December 31, 2020.
Policy Loans
Accounting policy. Policy loans, primarily associated with our corporate-owned life insurance business, are carried at unpaid principal balances plus accumulated interest, the total of which approximates fair value. These loans are collateralized by life insurance policy cash values and therefore have minimal exposure to credit loss. Interest rates are reset annually based on a rolling average of benchmark interest rates.
Other Long-Term Investments
Accounting policy. Other long-term investments include investments in unconsolidated entities, including certain limited partnerships and limited liability companies holding real estate, securities or loans and healthcare related investments. These investments are carried at cost plus the Company's ownership percentage of reporting income or loss, based on the financial statements of the underlying investments that are generally reported at fair value. Income or loss from these investments is reported on a one quarter lag due to the timing of when financial information is received from the general partner or manager of the investments.
Other long-term investments also include investment real estate carried at depreciated cost less any impairment write-downs to fair value when cash flows indicate that the carrying value may not be recoverable. Depreciation is generally recorded using the straight-line method based on the estimated useful life of each asset. Investment real estate as of December 31, 2021 and 2020 is expected to be held longer than one year and may include real estate acquired through the foreclosure of commercial mortgage loans.
Additionally, statutory and other restricted deposits and foreign currency swaps carried at fair value are reported in the table below as "Other." See discussion below for information on the Company's accounting policies for derivative financial instruments.
111
Other long-term investments and related commitments are diversified by issuer, property type and geographic regions. These investments are primarily unconsolidated variable interest entities, see Note 13 for additional information. The following table provides unfunded commitment and carrying value information for these investments. The Company expects to disburse approximately 35% of the committed amounts in 2022.
| Unfunded Commitments as of | ||||||||||||||||||||
| Carrying value as of December 31, | ||||||||||||||||||||
| (In millions) | 2021 | 2020 | December 31, 2021 | |||||||||||||||||
| Real estate investments | $ | 1,152 | $ | 951 | $ | 752 | ||||||||||||||
| Securities partnerships | 2,272 | 1,737 | 1,969 | |||||||||||||||||
| Other | 150 | 144 | — | |||||||||||||||||
| Total | $ | 3,574 | $ | 2,832 | $ | 2,721 | ||||||||||||||
Short-Term Investments and Cash Equivalents
Accounting policy. Security investments with maturities of greater than three months to one year from time of purchase are classified as short-term, available for sale and carried at fair value that approximates cost. Cash equivalents consist of short-term investments with maturities of three months or less from the time of purchase and are carried at cost that approximates fair value.
B.Derivative Financial Instruments
The Company uses derivative financial instruments to manage the characteristics of investment assets (such as duration, yield, currency and liquidity) to meet the varying demands of the related insurance and contractholder liabilities. The Company also uses derivative financial instruments to hedge the risk of changes in the net assets of certain of its foreign subsidiaries due to changes in foreign currency exchange rates and to hedge the interest rate risk of certain long-term debt. The Company has written and purchased GMIB reinsurance contracts in its run-off reinsurance business that are accounted for as freestanding derivatives as discussed in Note 10. Derivatives in the Company's separate accounts are excluded from the following discussion because associated gains and losses generally accrue directly to separate account policyholders.
Accounting policy. Derivatives are recorded on our Consolidated Balance Sheets at fair value and are classified as current or non-current according to their contractual maturities. Further information on our policies for determining fair value are discussed in Note 12. The Company applies hedge accounting when derivatives are designated, qualified and highly effective as hedges. Under hedge accounting, the changes in fair value of the derivative and the hedged risk are generally recognized together and offset each other when reported in Shareholders' net income. Various qualitative or quantitative methods appropriate for each hedge are used to formally assess and document hedge effectiveness at inception and each period throughout the life of a hedge.
The Company's derivative financial instruments are presented as follows:
•Fair value hedges of the foreign exchange-related changes in fair values of certain foreign-denominated bonds: Swap fair values are reported in Long-term investments or Other non-current liabilities. Offsetting changes in fair values attributable to the foreign exchange risk of the swap contracts and the hedged bonds are reported in Realized investment gains and losses. The portion of the swap contracts' changes in fair value excluded from the assessment of hedge effectiveness is recorded in Other comprehensive income and recognized in Net investment income as swap coupon payments are accrued, offsetting the foreign-denominated coupons received on the designated bonds. Net cash flows are reported in Operating activities, while exchanges of notional principal amounts are reported in Investing activities.
•Fair value hedges of the interest rate exposure on the Company's long-term debt: Using fair value hedge accounting, the fair values of the swap contracts are reported in Other assets or Other liabilities. The critical terms of these swaps match those of the long-term debt being hedged. As a result, the carrying value of the hedged debt is adjusted to reflect changes in its fair value driven by the Secured Overnight Financing Rate ("SOFR"). The effects of those adjustments on interest expense are offset by the effects of corresponding changes in the swaps' fair value. The net impact from the hedge reported in Interest expense and other reflects interest expense on the hedged debt at the variable interest rate. Cash flows relating to these contracts are reported in Operating activities.
•Net investment hedges of certain foreign subsidiaries that conduct their business principally in currencies other than the U.S. dollar: The fair values of the foreign currency swap and forward contracts are reported in Other assets or Other liabilities. The changes in fair values of these instruments are reported in Other comprehensive income, specifically in translation of foreign currencies. The portion of the change in fair values relating to foreign exchange spot rates will be recognized in earnings upon deconsolidation of the hedged foreign subsidiaries. The remaining changes in fair value of these instruments are
112
excluded from our effectiveness assessment and recognized in Interest expense and other over the term of the instrument. Cash flows relating to these contracts are reported in Investing activities.
•Economic hedges for derivatives not designated as accounting hedges: Fair values of forward contracts are reported in Current investments or Accrued expenses and other liabilities. The changes in fair values are reported in Realized investment gains and losses. Cash flows relating to these contracts are reported in Investing activities.
The gross fair values of our derivative financial instruments are presented in Note 12. As of December 31, 2021 and December 31, 2020, the effects of derivative financial instruments used in these individual hedging strategies were not material to the Consolidated Financial Statements, including gains or losses reclassified from Accumulated other comprehensive income into Shareholders' net income, amounts excluded from the assessment of hedge effectiveness and fair values of assets posted or held as collateral supporting the fair values of these derivative financial instruments. The following table summarizes the types and notional quantity of derivative instruments held by the Company:
| Notional Value as of | ||||||||||||||||||||
| (In millions) | December 31, 2021 | December 31, 2020 | ||||||||||||||||||
| Purpose | Type of Instrument | |||||||||||||||||||
Fair value hedge: To hedge the foreign exchange-related changes in fair values of certain foreign-denominated bonds. The notional value of these derivatives matches the amortized cost of the hedged bonds. A majority of these instruments are denominated in Euro, with the remaining instruments denominated in British Pound Sterling and Australian Dollars. | Foreign currency swap contracts | $ | 1,081 | $ | 925 | |||||||||||||||
Fair value hedge: To convert a portion of the interest rate exposure on the Company's long-term debt from fixed to variable rates. This more closely aligns the Company's interest expense with the interest income received on its cash equivalent and short-term investment balances. The variable rates are benchmarked to SOFR. | Interest rate swap contracts | $ | 750 | $ | — | |||||||||||||||
Net investment hedge: To reduce the risk of changes in net assets due to changes in foreign currency spot exchange rates for certain foreign subsidiaries that conduct their business principally in currencies other than the U.S. Dollar. The notional value of hedging instruments matches the hedged amount of subsidiary net assets. Foreign currency swap contracts are denominated in Euros, while foreign currency forward contracts are primarily denominated in Korean Won, with the remaining instruments denominated in New Zealand Dollar and Taiwan Dollar. | Foreign currency swap contracts | $ | 526 | $ | 526 | |||||||||||||||
Foreign currency forward contracts | $ | 1,380 | $ | 636 | ||||||||||||||||
Economic hedge: To hedge the foreign exchange-related changes in fair value of U.S. dollar-denominated investment assets to reflect the local currency for the Company's foreign subsidiary in South Korea. The notional value of hedging instruments generally aligns with the fair value of the hedged investments. | Foreign currency forward contracts | $ | 720 | $ | 538 | |||||||||||||||
Concentration of Risk
The Company did not have a concentration of investments in a single issuer or borrower exceeding 10% of shareholders' equity as of December 31, 2021 or 2020.
C.Net Investment Income
Accounting policy. When interest and principal payments on investments are current, the Company recognizes interest income when it is earned. The Company recognizes interest income on a cash basis when interest payments are delinquent based on contractual terms or when certain terms (interest rate or maturity date) of the investment have been restructured. For unconsolidated entities that are included in Other long-term investments, investment income is generally recognized according to the Company's share of the reported income or loss on the underlying investments. Investment income attributed to the Company's separate accounts is excluded from our earnings because associated gains and losses generally accrue directly to separate account policyholders.
113
The components of Net investment income for the years ended December 31 were as follows:
| (In millions) | 2021 | 2020 | 2019 | |||||||||||||||||
| Debt Securities | $ | 689 | $ | 962 | $ | 986 | ||||||||||||||
| Equity securities | 12 | 11 | 5 | |||||||||||||||||
| Commercial mortgage loans | 60 | 80 | 88 | |||||||||||||||||
| Policy loans | 63 | 64 | 66 | |||||||||||||||||
| Other long-term investments | 758 | 127 | 167 | |||||||||||||||||
| Short-term investments and cash | 26 | 52 | 131 | |||||||||||||||||
| Total investment income | 1,608 | 1,296 | 1,443 | |||||||||||||||||
| Less investment expenses | 59 | 52 | 53 | |||||||||||||||||
| Net investment income | $ | 1,549 | $ | 1,244 | $ | 1,390 | ||||||||||||||
Investment income for the year ended December 31, 2021 increased versus the year ended December 31, 2020 due to strong performance of assets underlying our limited partnership investments reported in Other long-term investments. The overall increase in investment income was partially offset by lower investment income from our debt securities as a result of lower invested asset levels following the divestiture of Cigna's U.S. Group Disability and Life business on December 31, 2020. The Company received income distributions of $568 million in 2021, $227 million in 2020 and $202 million in 2019 from its limited partnership investments reported in Other long-term investments.
D. Realized Investment Gains and Losses
Accounting policy. Realized investment gains and losses are based on specifically identified assets and result from sales, investment asset write-downs, change in the fair value of certain derivatives and equity securities and changes in allowances for credit losses on debt securities and commercial mortgage loan investments.
The following realized gains and losses on investments exclude amounts required to adjust future policy benefits for the run-off settlement annuity business (consistent with accounting for a premium deficiency), as well as realized gains and losses attributed to the Company's separate accounts because those gains and losses generally accrue directly to separate account policyholders:
| (In millions) | 2021 | 2020 | 2019 | |||||||||||||||||
| Net realized investment gains (losses), excluding credit loss expense and asset write-downs | $ | 194 | $ | 186 | $ | 189 | ||||||||||||||
| Credit loss (expense) recoveries | 2 | (27) | — | |||||||||||||||||
| Other investment asset write-downs | — | (10) | (12) | |||||||||||||||||
| Net realized investment gains (losses), before income taxes | $ | 196 | $ | 149 | $ | 177 | ||||||||||||||
Net realized investment gains, excluding credit loss expense and asset write-downs for the year ended December 31, 2021 was primarily driven by mark-to-market gains on equity securities and gains on the sales of real estate partnerships, partially offset by mark-to-market losses on derivatives. This activity for the year ended December 31, 2020 was primarily driven by mark-to-market on equity securities and sales of debt securities, while activity for the year ended December 31, 2019 was primarily driven by gains on the sales of real estate partnerships and debt securities. Credit loss (expense) recoveries on invested assets reflect credit losses incurred on debt securities primarily relating to issuers in certain industries that have been impacted by the global COVID-19 pandemic.
Note 12 – Fair Value Measurements
The Company carries certain financial instruments at fair value in the financial statements including debt securities, certain equity securities, short-term investments and derivatives. Other financial instruments are measured at fair value only under certain conditions, such as when impaired or when there are observable price changes for equity securities with no readily determinable fair value.
Fair value is defined as the price at which an asset could be exchanged in an orderly transaction between market participants at the balance sheet date. A liability's fair value is defined as the amount that would be paid to transfer the liability to a market participant, not the amount that would be paid to settle the liability with the creditor.
The Company's financial assets and liabilities carried at fair value have been classified based upon a hierarchy defined by GAAP. The hierarchy gives the highest ranking to fair values determined using unadjusted quoted prices in active markets for identical assets and liabilities (Level 1) and the lowest ranking to fair values determined using methodologies and models with unobservable inputs (Level 3). An asset's or a liability's classification is based on the lowest level of input that is significant to its measurement. For example, a financial asset or liability carried at fair value would be classified in Level 3 if unobservable inputs were significant to the instrument's
114
fair value, even though the measurement may be derived using inputs that are both observable (Levels 1 and 2) and unobservable (Level 3).
The Company estimates fair values using prices from third parties or internal pricing methods. Fair value estimates received from third-party pricing services are based on reported trade activity and quoted market prices when available and other market information that a market participant would use to estimate fair value. The internal pricing methods are performed by the Company's investment professionals and generally involve using discounted cash flow analyses, incorporating current market inputs for similar financial instruments with comparable terms and credit quality as well as other qualitative factors. In instances where there is little or no market activity for the same or similar instruments, fair value is estimated using methods, models and assumptions that the Company believes a hypothetical market participant would use to determine a current transaction price. These valuation techniques involve some level of estimation and judgment that becomes significant with increasingly complex instruments or pricing models.
The Company is responsible for determining fair value and for assigning the appropriate level within the fair value hierarchy based on the significance of unobservable inputs. The Company reviews methodologies, processes and controls of third-party pricing services and compares prices on a test basis to those obtained from other external pricing sources or internal estimates. The Company performs ongoing analyses of both prices received from third-party pricing services and those developed internally to determine that they represent appropriate estimates of fair value. The controls executed by the Company include evaluating changes in prices and monitoring for potentially stale valuations. The Company also performs sample testing of sales values to confirm the accuracy of prior fair value estimates. The minimal exceptions identified during these processes indicate that adjustments to prices are infrequent and do not significantly impact valuations. An annual due-diligence review of the most significant pricing service is conducted to review their processes, methodologies and controls. This review includes a walk-through of inputs for a sample of securities held across various asset types to validate the documented pricing process.
A.Financial Assets and Financial Liabilities Carried at Fair Value
The following table provides information as of December 31, 2021 and December 31, 2020 about the Company's financial assets and liabilities carried at fair value. Separate account assets are also recorded at fair value on the Company's Consolidated Balance Sheets and are reported separately in the Separate Accounts section below as gains and losses related to these assets generally accrue directly to policyholders.
| (In millions) | Quoted Prices in Active Markets for Identical Assets (Level 1) | Significant Other Observable Inputs (Level 2) | Significant Unobservable Inputs (Level 3) | Total | ||||||||||||||||||||||||||||||||||||||||||||||
| As of December 31, 2021 | As of December 31, 2020 | As of December 31, 2021 | As of December 31, 2020 | As of December 31, 2021 | As of December 31, 2020 | As of December 31, 2021 | As of December 31, 2020 | |||||||||||||||||||||||||||||||||||||||||||
| Financial assets at fair value | ||||||||||||||||||||||||||||||||||||||||||||||||||
| Debt securities | ||||||||||||||||||||||||||||||||||||||||||||||||||
| Federal government and agency | $ | 147 | $ | 207 | $ | 240 | $ | 249 | $ | — | $ | — | $ | 387 | $ | 456 | ||||||||||||||||||||||||||||||||||
| State and local government | — | — | 171 | 167 | — | — | 171 | 167 | ||||||||||||||||||||||||||||||||||||||||||
| Foreign government | — | — | 2,611 | 2,498 | 5 | 13 | 2,616 | 2,511 | ||||||||||||||||||||||||||||||||||||||||||
Corporate | — | — | 12,606 | 13,878 | 660 | 684 | 13,266 | 14,562 | ||||||||||||||||||||||||||||||||||||||||||
| Mortgage and other asset-backed | — | — | 418 | 309 | 100 | 126 | 518 | 435 | ||||||||||||||||||||||||||||||||||||||||||
| Total debt securities | 147 | 207 | 16,046 | 17,101 | 765 | 823 | 16,958 | 18,131 | ||||||||||||||||||||||||||||||||||||||||||
Equity securities (1) | 16 | 50 | 160 | 165 | 31 | 31 | 207 | 246 | ||||||||||||||||||||||||||||||||||||||||||
| Short-term investments | — | — | 428 | 325 | — | — | 428 | 325 | ||||||||||||||||||||||||||||||||||||||||||
Derivative assets (2) | — | — | 143 | 72 | — | — | 143 | 72 | ||||||||||||||||||||||||||||||||||||||||||
| Financial liabilities at fair value | ||||||||||||||||||||||||||||||||||||||||||||||||||
| Derivative liabilities | $ | — | $ | — | $ | 33 | $ | 108 | $ | — | $ | — | $ | 33 | $ | 108 | ||||||||||||||||||||||||||||||||||
(1) Excludes certain equity securities that have no readily determinable fair value.
(2) Derivative assets above include $34 million as of December 31, 2020 that are presented in the Short-term investments category disclosed in Note 11. See Note 11 for more information on our Derivative Financial Instruments.
115
Level 1 Financial Assets
Inputs for instruments classified in Level 1 include unadjusted quoted prices for identical assets in active markets accessible at the measurement date. Active markets provide pricing data for trades occurring at least weekly and include exchanges and dealer markets.
Assets in Level 1 include actively-traded U.S. government bonds and exchange-listed equity securities. A relatively small portion of the Company's investment assets are classified in this category given the narrow definition of Level 1 and the Company's investment asset strategy to maximize investment returns.
Level 2 Financial Assets and Financial Liabilities
Inputs for instruments classified in Level 2 include quoted prices for similar assets or liabilities in active markets, quoted prices from those willing to trade in markets that are not active or other inputs that are market observable or can be corroborated by market data for the term of the instrument. Such other inputs include market interest rates and volatilities, spreads and yield curves. An instrument is classified in Level 2 if the Company determines that unobservable inputs are insignificant.
Debt and equity securities. Approximately 94% of the Company's investments in debt and equity securities are classified in Level 2 including most public and private corporate debt and equity securities, federal agency and municipal bonds, non-government mortgage-backed securities and preferred stocks. Third-party pricing services and internal methods often use recent trades of securities with similar features and characteristics because many debt securities do not trade daily. Pricing models are used to determine these prices when recent trades are not available. These models calculate fair values by discounting future cash flows at estimated market interest rates. Such market rates are derived by calculating the appropriate spreads over comparable U.S. Treasury securities based on the credit quality, industry and structure of the asset. Typical inputs and assumptions to pricing models include, but are not limited to, a combination of benchmark yields, reported trades, issuer spreads, liquidity, benchmark securities, bids, offers, reference data and industry and economic events. For mortgage-backed securities, inputs and assumptions may also include characteristics of the issuer, collateral attributes, prepayment speeds and credit rating.
Nearly all of these instruments are valued using recent trades or pricing models. Less than 1% of the fair value of investments classified in Level 2 represents foreign bonds that are valued using a single, unadjusted market-observable input derived by averaging multiple broker-dealer quotes, consistent with local market practice.
Short-term investments are carried at fair value that approximates cost. The Company compares market prices for these securities to recorded amounts on a regular basis to validate that current carrying amounts approximate exit prices. The short-term nature of the investments and corroboration of the reported amounts over the holding period support their classification in Level 2.
Derivative assets and liabilities classified in Level 2 represent over-the-counter instruments such as foreign currency forward and swap contracts. Fair values for these instruments are determined using market observable inputs including forward currency and interest rate curves and widely published market observable indices. Credit risk related to the counterparty and the Company is considered when estimating the fair values of these derivatives. However, the Company is largely protected by collateral arrangements with counterparties and determined that no adjustments for credit risk were required as of December 31, 2021 or December 31, 2020. The nature and use of these derivative financial instruments are described in Note 11.
Level 3 Financial Assets and Financial Liabilities
Certain inputs for instruments classified in Level 3 are unobservable (supported by little or no market activity) and significant to their resulting fair value measurement. Unobservable inputs reflect the Company's best estimate of what hypothetical market participants would use to determine a transaction price for the asset or liability at the reporting date.
The Company classifies certain newly-issued, privately-placed, complex or illiquid securities in Level 3. Approximately 5% of debt and equity securities are priced using significant unobservable inputs and classified in this category.
Fair values of mortgage and other asset-backed securities, as well as corporate and government debt securities, are primarily determined using pricing models that incorporate the specific characteristics of each asset and related assumptions including the investment type and structure, credit quality, industry and maturity date in comparison to current market indices, spreads and liquidity of assets with similar characteristics. Inputs and assumptions for pricing may also include characteristics of the issuer, collateral attributes and prepayment speeds for mortgage and other asset-backed securities. Recent trades in the subject security or similar securities are assessed when available, and the Company may also review published research in its evaluation, as well as the issuer's financial statements.
116
Quantitative Information about Unobservable Inputs
The significant unobservable input used to value our corporate and government debt securities and mortgage and other asset-backed securities is an adjustment for liquidity. This adjustment is needed to reflect current market conditions and issuer circumstances when there is limited trading activity for the security.
The following table summarizes the fair value and significant unobservable inputs that were developed directly by the Company and used in pricing these debt securities as of December 31, 2021 and December 31, 2020. The range and weighted average basis point ("bps") amounts for liquidity reflect the Company's best estimates of the unobservable adjustments a market participant would make to calculate these fair values.
| Fair Value as of | Unobservable Adjustment Range (Weighted Average by Quantity) as of | ||||||||||||||||||||||||||||||||||
| (Fair value in millions ) | December 31, 2021 | December 31, 2020 | Unobservable input December 31, 2021 | December 31, 2021 | December 31, 2020 | ||||||||||||||||||||||||||||||
| Debt securities | |||||||||||||||||||||||||||||||||||
| Corporate and government debt securities | $ | 664 | $ | 696 | Liquidity | 60 - 1060 (410) | bps | 60 - 1370 (470) | bps | ||||||||||||||||||||||||||
| Mortgage and other asset-backed securities | 100 | 126 | Liquidity | 60 - 390 (100) | bps | 60 - 380 (80) | bps | ||||||||||||||||||||||||||||
Securities not priced by the Company (1) | 1 | 1 | |||||||||||||||||||||||||||||||||
| Total Level 3 debt securities | $ | 765 | $ | 823 | |||||||||||||||||||||||||||||||
(1) The fair values for these securities use single, unadjusted non-binding broker quotes not developed directly by the Company.
A significant increase in liquidity spread adjustments would result in a lower fair value measurement, while a decrease would result in a higher fair value measurement.
Changes in Level 3 Financial Assets and Financial Liabilities Carried at Fair Value
The following table summarizes the changes in financial assets and financial liabilities classified in Level 3 for the years ended December 31, 2021 and 2020. Gains and losses reported in the table may include net changes in fair value that are attributable to both observable and unobservable inputs.
| (In millions) | 2021 | 2020 | ||||||||||||
| Debt and Equity Securities | ||||||||||||||
| Beginning balance | $ | 854 | $ | 555 | ||||||||||
| Total gains (losses) included in shareholders' net income | (22) | (7) | ||||||||||||
| Gains (losses) included in other comprehensive income | (6) | (12) | ||||||||||||
Gains (losses) required to adjust future policy benefits for settlement annuities (1) | (8) | 7 | ||||||||||||
| Purchases, sales and settlements | ||||||||||||||
| Purchases | 138 | 107 | ||||||||||||
| Sales | (36) | (121) | ||||||||||||
| Settlements | (119) | (89) | ||||||||||||
| Total purchases, sales and settlements | (17) | (103) | ||||||||||||
| Transfers into/(out of) Level 3 | ||||||||||||||
| Transfers into Level 3 | 207 | 774 | ||||||||||||
| Transfers out of Level 3 | (212) | (360) | ||||||||||||
| Total transfers into/(out of) Level 3 | (5) | 414 | ||||||||||||
| Ending balance | $ | 796 | $ | 854 | ||||||||||
| Total gains (losses) included in Shareholders' net income attributable to instruments held at the reporting date | $ | (17) | $ | (17) | ||||||||||
| Change in unrealized gains or losses included in Other comprehensive income for assets held at the end of the reporting period | $ | (10) | $ | (6) | ||||||||||
(1) Amounts do not accrue to shareholders.
Total gains and losses included in Shareholders' net income in the tables above are reflected in the Consolidated Statements of Income as Net realized investment gains (losses) and Net investment income.
Gains and losses included in Other comprehensive income in the tables above are reflected in Net unrealized appreciation (depreciation) on securities and derivatives in the Consolidated Statements of Comprehensive Income.
117
Transfers into or out of the Level 3 category occur when unobservable inputs, such as the Company's best estimate of what a market participant would use to determine a current transaction price, become more or less significant to the fair value measurement. Market activity typically decreases during periods of economic uncertainty and this decrease in activity reduces the availability of market observable data. As a result, the level of unobservable judgment that must be applied to the pricing of certain instruments increases and is typically observed through the widening of liquidity spreads. Transfers between Level 2 and Level 3 during 2021 and 2020 primarily reflected changes in liquidity estimates for certain private placement issuers across several sectors. Transfers into and out of Level 3 were higher in 2020 due to significant fluctuations in unobservable inputs experienced as a result of the uncertainty over the economic impacts related to COVID-19. See discussion under Quantitative Information about Unobservable Inputs above for more information.
Separate Accounts
Accounting policy. Separate account assets and liabilities are contractholder funds maintained in accounts with specific investment objectives. The assets of these accounts are legally segregated and are not subject to claims that arise out of any of the Company's other businesses. These separate account assets are carried at fair value with equal amounts recorded for related separate account liabilities. The investment income and fair value gains and losses of separate account assets generally accrue directly to the contractholders and, together with their deposits and withdrawals, are excluded from the Company's Consolidated Statements of Income and Cash Flows. Fees and charges earned for mortality risks, asset management or administrative services are reported in either Premiums or Fees and other revenues. Investments that are measured using the practical expedient of net asset value ("NAV") are excluded from the fair value hierarchy.
Fair values of Separate account assets at December 31, 2021 and December 31, 2020 were as follows:
| (In millions) | Quoted Prices in Active Markets for Identical Assets (Level 1) | Significant Other Observable Inputs (Level 2) | Significant Unobservable Inputs (Level 3) | Total | ||||||||||||||||||||||||||||||||||||||||||||||
| December 31, 2021 | December 31, 2020 | December 31, 2021 | December 31, 2020 | December 31, 2021 | December 31, 2020 | December 31, 2021 | December 31, 2020 | |||||||||||||||||||||||||||||||||||||||||||
Guaranteed separate accounts (See Note 22) | $ | 227 | $ | 226 | $ | 276 | $ | 297 | $ | — | $ | — | $ | 503 | $ | 523 | ||||||||||||||||||||||||||||||||||
Non-guaranteed separate accounts (1) | 1,130 | 1,925 | 6,406 | 5,600 | 334 | 355 | 7,870 | 7,880 | ||||||||||||||||||||||||||||||||||||||||||
| Subtotal | $ | 1,357 | $ | 2,151 | $ | 6,682 | $ | 5,897 | $ | 334 | $ | 355 | 8,373 | 8,403 | ||||||||||||||||||||||||||||||||||||
Non-guaranteed separate accounts priced at NAV as a practical expedient (1) | 842 | 683 | ||||||||||||||||||||||||||||||||||||||||||||||||
| Total | 9,215 | |||||||||||||||||||||||||||||||||||||||||||||||||
Separate account assets of businesses classified as held for sale (2) | (878) | |||||||||||||||||||||||||||||||||||||||||||||||||
| Separate account assets per Consolidated Balance Sheets | $ | 8,337 | $ | 9,086 | ||||||||||||||||||||||||||||||||||||||||||||||
(1)Non-guaranteed separate accounts included $4.5 billion as of December 31, 2021 and $4.2 billion as of December 31, 2020 in assets supporting the Company's pension plans, including $0.3 billion classified in Level 3 as of December 31, 2021 and December 31, 2020.
(2)Investments related to the international life, accident and supplemental benefits businesses that are held for sale. See Note 5 to the Consolidated Financial Statements for additional information.
.
Separate account assets classified as Level 1 primarily include exchange-listed equity securities. Level 2 assets primarily include:
•corporate and structured bonds valued using recent trades of similar securities or pricing models that discount future cash flows at estimated market interest rates as described above; and
•actively-traded institutional and retail mutual fund investments.
Separate account assets classified in Level 3 primarily support Cigna's pension plans and include certain newly-issued, privately-placed, complex or illiquid securities that are priced using methods discussed above, as well as commercial mortgage loans. Activity, including transfers into and out of Level 3, was not material for the year ended December 31, 2021 or 2020.
118
Separate account investments in securities partnerships, real estate and hedge funds are generally valued based on the separate account's ownership share of the equity of the investee (NAV as a practical expedient) including changes in the fair values of its underlying investments. Substantially all of these assets support the Cigna Pension Plans. The following table provides additional information on these investments:
| Fair Value as of | Unfunded Commitment as of December 31, 2021 | Redemption Frequency (if currently eligible) | Redemption Notice Period | |||||||||||||||||||||||||||||
| (In millions) | December 31, 2021 | December 31, 2020 | ||||||||||||||||||||||||||||||
| Securities partnerships | $ | 513 | $ | 463 | $ | 275 | Not applicable | Not applicable | ||||||||||||||||||||||||
| Real estate funds | 325 | 215 | — | Quarterly | 30 - 90 days | |||||||||||||||||||||||||||
| Hedge funds | 4 | 5 | — | Up to annually, varying by fund | 30 - 90 days | |||||||||||||||||||||||||||
| Total | $ | 842 | $ | 683 | $ | 275 | ||||||||||||||||||||||||||
As of December 31, 2021, the Company does not have plans to sell any of these assets at less than fair value. These investments are structured to satisfy longer-term investment objectives. Securities partnerships are contractually non-redeemable and the underlying investment assets are expected to be liquidated by the fund managers within ten years after inception.
B.Assets and Liabilities Measured at Fair Value under Certain Conditions
Some financial assets and liabilities are not carried at fair value, such as commercial mortgage loans that are carried at unpaid principal, investment real estate that is carried at depreciated cost and equity securities with no readily determinable fair value when there are no observable market transactions. However, these financial assets and liabilities may be measured using fair value under certain conditions, such as when investments become impaired and are written down to their fair value, or when there are observable price changes from orderly market transactions of equity securities that otherwise had no readily determinable fair value.
For the years ended December 31, 2021 and 2020, no impairments were recognized requiring these assets to be measured at fair value. Realized investment gains and losses from these observable price changes for the years ended December 31, 2021 and December 31, 2020 were not material.
C.Fair Value Disclosures for Financial Instruments Not Carried at Fair Value
The following table includes the Company's financial instruments not recorded at fair value that are subject to fair value disclosure requirements at December 31, 2021 and December 31, 2020. In addition to universal life products and finance leases, financial instruments that are carried in the Company's Consolidated Financial Statements at amounts that approximate fair value are excluded from the following table:
| Classification in Fair Value Hierarchy | December 31, 2021 | December 31, 2020 | ||||||||||||||||||||||||||||||
| (In millions) | Fair Value | Carrying Value | Fair Value | Carrying Value | ||||||||||||||||||||||||||||
| Commercial mortgage loans | Level 3 | $ | 1,598 | $ | 1,566 | $ | 1,456 | $ | 1,419 | |||||||||||||||||||||||
| Long-term debt, including current maturities, excluding finance leases | Level 2 | $ | 35,621 | $ | 31,593 | $ | 37,676 | $ | 31,835 | |||||||||||||||||||||||
Note 13 – Variable Interest Entities
When the Company becomes involved with a variable interest entity and when there is a change in the Company's involvement with an entity, the Company must determine if it is the primary beneficiary and must consolidate the entity. The Company is considered the primary beneficiary if it has the power to direct the entity's most significant economic activities and has the right to receive benefits or obligation to absorb losses that could be significant to the entity. The Company evaluates the following criteria:
•the structure and purpose of the entity;
•the risks and rewards created by and shared through the entity; and
•the Company's ability to direct its activities, receive its benefits and absorb its losses relative to the other parties involved with the entity including its sponsors, equity holders, guarantors, creditors and servicers.
The Company determined it was not a primary beneficiary in any material variable interest entity as of December 31, 2021 or December 31, 2020.
119
The Company's involvement in variable interest entities for which it is not the primary beneficiary is described below.
Securities limited partnerships and real estate limited partnerships. The Company owns interests in securities limited partnerships and real estate limited partnerships that are defined as unconsolidated variable interest entities. These partnerships invest in the equity or mezzanine debt of privately-held companies and real estate properties. General partners unaffiliated with the Company control decisions that most significantly impact the partnership's operations and the limited partners do not have substantive kick-out or participating rights. The Company has invested in approximately 180 limited partnerships that have a carrying value of $2.6 billion as of December 31, 2021 reported in Other long-term investments. We have commitments to contribute an additional $2.2 billion to these entities. The Company's maximum exposure to loss from these investments is $4.8 billion, calculated as the sum of our carrying value and the additional funding commitments. Our noncontrolling interest in each of these limited partnerships is generally less than 15% of the partnership ownership interests. See Note 11 for further information on the Company's accounting policy for Other long-term investments.
Other variable interest entities. The Company is involved in other types of variable interest entities, including certain asset-backed and corporate securities, real estate joint ventures that develop properties for residential and commercial use, independent physician associations (IPAs) that provide care management services and international healthcare joint ventures. The Company's maximum exposure to loss is $0.6 billion from certain asset-backed and corporate securities and $0.4 billion from real estate joint ventures, which represents the sum of our carrying value and the additional funding commitments for these entities. The carrying values and maximum exposures for remaining unconsolidated variable interest entities was not material as of December 31, 2021.
The Company has not provided, and does not intend to provide, financial support to any of the variable interest entities in excess of its maximum exposure. We perform ongoing qualitative analyses of our involvement with these variable interest entities to determine if consolidation is required.
120
Note 14 – Accumulated Other Comprehensive Income (Loss) ("AOCI")
AOCI includes unrealized appreciation on securities and derivatives (excluding appreciation on investments supporting future policy benefit liabilities of the run-off settlement annuity business) (see Note 11), foreign currency translation and the net postretirement benefits liability adjustment. AOCI includes the Company's share from unconsolidated entities reported on the equity method. Generally, tax effects in AOCI are established at the currently enacted tax rate and reclassified to Shareholders' net income in the same period that the related pre-tax AOCI reclassifications are recognized. Changes in the components of AOCI were as follows:
| For the Years Ended December 31, | ||||||||||||||||||||
| (In millions) | 2021 | 2020 | 2019 | |||||||||||||||||
| Securities and Derivatives | ||||||||||||||||||||
| Beginning balance | $ | 900 | $ | 975 | $ | 18 | ||||||||||||||
| Appreciation (depreciation) on securities and derivatives | (230) | 776 | 1,266 | |||||||||||||||||
| Tax (expense) benefit | 31 | (150) | (270) | |||||||||||||||||
| Net appreciation (depreciation) on securities and derivatives | (199) | 626 | 996 | |||||||||||||||||
| Reclassification adjustment for (gains) losses included in Shareholders' net income ((Gain) loss on sale of business) | — | (862) | — | |||||||||||||||||
| Reclassification adjustment for (gains) losses included in Shareholders' net income (Net realized investment (gains) losses) | (21) | (26) | (49) | |||||||||||||||||
| Reclassification adjustment for tax expense included in Shareholders' net income | 5 | 187 | 10 | |||||||||||||||||
| Net (gains) losses reclassified from AOCI to Shareholders' net income | (16) | (701) | (39) | |||||||||||||||||
| Other comprehensive income (loss), net of tax | (215) | (75) | 957 | |||||||||||||||||
| Ending balance | $ | 685 | $ | 900 | $ | 975 | ||||||||||||||
| Translation of foreign currencies | ||||||||||||||||||||
| Beginning balance | $ | (15) | $ | (275) | $ | (221) | ||||||||||||||
| Translation of foreign currencies | (213) | 232 | (57) | |||||||||||||||||
| Tax (expense) benefit | (19) | 12 | (2) | |||||||||||||||||
| Net translation of foreign currencies | (232) | 244 | (59) | |||||||||||||||||
| Reclassification adjustment for (gains) losses included in Net income ((Gain) loss on sale of business) | — | 11 | — | |||||||||||||||||
| Reclassification adjustment for tax expense (benefit) included in Net income | — | (3) | — | |||||||||||||||||
| Net translation (gains) losses reclassified from AOCI to Net income | — | 8 | — | |||||||||||||||||
| Other comprehensive income (loss), net of tax | (232) | 252 | (59) | |||||||||||||||||
| Less: Net translation gain (loss) on foreign currencies attributable to noncontrolling interests | (14) | (8) | (5) | |||||||||||||||||
| Shareholders' other comprehensive income (loss), net of tax | (218) | 260 | (54) | |||||||||||||||||
| Ending balance | $ | (233) | $ | (15) | $ | (275) | ||||||||||||||
| Postretirement benefits liability | ||||||||||||||||||||
| Beginning balance | $ | (1,746) | $ | (1,641) | $ | (1,508) | ||||||||||||||
| Reclassification adjustment for amortization of net prior actuarial losses and prior service costs (Interest expense and other) | 85 | 70 | 62 | |||||||||||||||||
| Reclassification adjustment for settlement (Interest expense and other) | 4 | — | 10 | |||||||||||||||||
| Reclassification adjustment for tax (benefit) included in Shareholders' net income | (21) | (17) | (15) | |||||||||||||||||
| Net adjustments reclassified from AOCI to Shareholders' net income | 68 | 53 | 57 | |||||||||||||||||
| Valuation update | 448 | (206) | (249) | |||||||||||||||||
| Tax (expense) benefit | (106) | 48 | 59 | |||||||||||||||||
| Net change due to valuation update | 342 | (158) | (190) | |||||||||||||||||
| Other comprehensive income (loss), net of tax | 410 | (105) | (133) | |||||||||||||||||
| Ending balance | $ | (1,336) | $ | (1,746) | $ | (1,641) | ||||||||||||||
121
Note 15 – Organizational Efficiency Plan
During the fourth quarter of 2021, we approved a strategic plan to further leverage the Company's ongoing growth to drive operational efficiency through enhancements to organizational structure and increased use of automation and shared services. As a result we recognized a charge in Selling, general and administrative expenses of $168 million, pre-tax ($119 million, after-tax) in the fourth quarter of 2021. This charge included $59 million of one-time expenses related to abandonment of leased assets and impairment of property and equipment as well as $109 million of accrued expenses primarily for severance costs related to headcount reductions. We expect most of the severance to be paid by 2023.
The following table summarizes a rollforward of the accrued liability recorded in "Accrued expenses and other liabilities":
| (In millions) | |||||
| Fourth quarter 2021 charge | $ | 109 | |||
| 2021 payments | (6) | ||||
| Balance, December 31, 2021 | $ | 103 | |||
Note 16 – Pension
A.About Our Plans
The Company sponsors U.S. and non-U.S. defined benefit pension plans; future benefit accruals for the domestic plans are frozen.
Accounting policy. The Company measures the assets and liabilities of its domestic pension plans as of December 31. Benefit obligations are measured at the present value of estimated future payments based on actuarial assumptions. The Company uses the "corridor" method to account for changes in the benefit obligation when actual results differ from those assumed, or when assumptions change. These changes are called net unrecognized actuarial gains (losses). Under the corridor method, net unrecognized actuarial gains (losses) are initially recorded in Accumulated other comprehensive loss. When the unrecognized gain (loss) exceeds 10% of the benefit obligation, that excess is amortized to expense over the expected remaining lives of plan participants. The net plan expense is reported in Interest expense and other in the Consolidated Statements of Income.
For balance sheet purposes, we measure plan assets at fair value. When the actual return differs from the expected return, those differences are reflected in the net unrealized actuarial gain (loss) discussed above. However, to measure pension benefit costs, we use a "market-related" asset valuation that differs from the actual fair value for domestic pension plan assets invested in non-fixed income investments. The "market-related" value recognizes the difference between actual and expected long-term returns in the portfolio over five years, a method that reduces the short-term impact of market fluctuations on pension costs. The market-related asset value was approximately $4.4 billion, compared with a fair value of approximately $4.8 billion at December 31, 2021.
122
B.Funded Status and Amounts Included in Accumulated Other Comprehensive Income
The following table summarizes the projected benefit obligations and assets related to our U.S. and non-U.S. pension plans as of and for the years ended December 31:
| Pension Benefits | ||||||||||||||
| (In millions) | 2021 | 2020 | ||||||||||||
| Change in benefit obligation | ||||||||||||||
| Benefit obligation, January 1 | $ | 5,600 | $ | 5,314 | ||||||||||
| Service cost | 2 | 2 | ||||||||||||
| Interest cost | 132 | 168 | ||||||||||||
Actuarial (gains) losses, net (1) | (189) | 416 | ||||||||||||
| Benefits paid from plan assets | (304) | (285) | ||||||||||||
Benefits paid – other | (18) | (15) | ||||||||||||
| Benefit obligation, December 31 | 5,223 | 5,600 | ||||||||||||
| Change in plan assets | ||||||||||||||
| Fair value of plan assets, January 1 | 4,623 | 4,441 | ||||||||||||
| Actual return on plan assets | 522 | 449 | ||||||||||||
| Benefits paid | (304) | (285) | ||||||||||||
| Contributions | 5 | 18 | ||||||||||||
| Fair value of plan assets, December 31 | 4,846 | 4,623 | ||||||||||||
| Funded status | $ | (377) | $ | (977) | ||||||||||
| Liability in Consolidated Balance Sheets | ||||||||||||||
| Accrued expenses and other liabilities | $ | (14) | $ | (15) | ||||||||||
| Other non-current liabilities | $ | (363) | $ | (962) | ||||||||||
(1) 2021 gain reflects an increase in the discount rate; 2020 loss reflects a decrease in the discount rate, partially offset by a favorable change in the mortality assumption.
We fund our qualified pension plans at least at the minimum amount required by the Employee Retirement Income Security Act of 1974 and the Pension Protection Act of 2006. The Company made immaterial contributions to the qualified pension plans in 2021. For 2022, contributions to the qualified pension plans are expected to be immaterial. Future years' contributions will ultimately be based on a wide range of factors including but not limited to asset returns, discount rates and funding targets. Non-qualified pension and other postretirement benefit plans are generally funded on a pay-as-you-go basis as there are no plan assets for these plans.
123
Benefit payments. The following benefit payments are expected to be paid in:
| (In millions) | Pension Benefits | |||||||
| 2022 | $ | 317 | ||||||
| 2023 | $ | 318 | ||||||
| 2024 | $ | 317 | ||||||
| 2025 | $ | 315 | ||||||
| 2026 | $ | 316 | ||||||
| 2027-2031 | $ | 1,532 | ||||||
Amounts reflected in the pension liabilities shown above that have not yet been reported in net income and, therefore, have been included in Accumulated other comprehensive loss consisted of the following as of December 31:
| Pension Benefits | ||||||||||||||
| (In millions) | 2021 | 2020 | ||||||||||||
| Unrecognized net (losses) | $ | (1,753) | $ | (2,277) | ||||||||||
| Unrecognized prior service cost | (5) | (5) | ||||||||||||
| Postretirement benefits liability adjustment | $ | (1,758) | $ | (2,282) | ||||||||||
C.Cost of Our Plans
Net pension cost was as follows:
| Pension Benefits | ||||||||||||||||||||
| (In millions) | 2021 | 2020 | 2019 | |||||||||||||||||
| Service cost | $ | 2 | $ | 2 | $ | 2 | ||||||||||||||
| Interest cost | 132 | 168 | 194 | |||||||||||||||||
| Expected long-term return on plan assets | (269) | (260) | (245) | |||||||||||||||||
| Amortization of: | ||||||||||||||||||||
| Prior actuarial losses, net | 78 | 78 | 59 | |||||||||||||||||
| Litigation settlement – plan amendment | — | — | 142 | |||||||||||||||||
| Settlement loss | 4 | — | 10 | |||||||||||||||||
| Net (benefit) cost | $ | (53) | $ | (12) | $ | 162 | ||||||||||||||
The Cigna Pension Plan (the "Plan"), together with its Plan Sponsor, was a defendant in a class action lawsuit related to the Plan's conversion of certain employees from an annuity to a cash balance benefit in 1997. In the first quarter of 2019, the Plan implemented the court order resulting in an increase to the pension liability of $142 million. The Company reversed a litigation reserve for the expenses recognized for this matter in 2019 aggregating to the same amount resulting in no impact on net income.
D.Assumptions Used for Pension
| 2021 | 2020 | ||||||||||||||||
| Discount rate: | |||||||||||||||||
| Pension benefit obligation | 2.82% | 2.49% | |||||||||||||||
| Pension benefit cost | 2.49% | 3.30% | |||||||||||||||
| Expected long-term return on plan assets: | |||||||||||||||||
| Pension benefit cost | 6.75% | 6.75% | |||||||||||||||
| Mortality table for pension obligations | White Collar mortality table with MP 2021 projection scale | White Collar mortality table with MP 2020 projection scale | |||||||||||||||
The Company develops discount rates by applying actual annualized yields for high quality bonds by duration to the expected pension plan liability cash flows. The bond yields represent a diverse mix of actively traded high quality fixed-income securities that have an above average return at each duration as management believes this approach is representative of the yield achieved through plan asset investment strategy.
The expected long-term return on plan assets was developed considering historical long-term actual returns, expected long-term market conditions, plan asset mix and management's plan asset investment strategy.
124
E.Pension Plan Assets
As of December 31, 2021, pension assets included $4.5 billion invested in the separate accounts of Connecticut General Life Insurance Company, a subsidiary of the Company, as well as an additional $0.3 billion, primarily invested directly in funds offered by an unaffiliated insurance company.
The fair values of pension assets by category are as follows as of December 31, 2021 and 2020:
| (In millions) | 2021 | 2020 | ||||||||||||
| Debt securities: | ||||||||||||||
| Federal government and agency | $ | 9 | $ | 9 | ||||||||||
| Corporate | 1,653 | 1,680 | ||||||||||||
| Asset-backed | 108 | 53 | ||||||||||||
| Fund investments | 731 | 380 | ||||||||||||
| Total debt securities | 2,501 | 2,122 | ||||||||||||
| Equity securities: | ||||||||||||||
| Domestic | 789 | 978 | ||||||||||||
International, including funds and pooled separate accounts (1) | 358 | 471 | ||||||||||||
| Total equity securities | 1,147 | 1,449 | ||||||||||||
| Securities partnerships | 514 | 463 | ||||||||||||
Real estate funds, including pooled separate accounts (1) | 334 | 219 | ||||||||||||
| Commercial mortgage loans | 77 | 95 | ||||||||||||
| Hedge funds | — | 1 | ||||||||||||
| Guaranteed deposit account contract | 91 | 98 | ||||||||||||
| Cash equivalents and other current assets, net | 182 | 176 | ||||||||||||
| Total pension assets at fair value | $ | 4,846 | $ | 4,623 | ||||||||||
(1) A pooled separate account has several participating benefit plans and each owns a share of the total pool of investments.
The Company's current target investment allocation percentages (58% fixed income, 25% public equity securities and 17% in other investments, including private equity (securities partnerships) and real estate) are developed by management as guidelines, although the fair values of each asset category are expected to vary as a result of changes in market conditions. The Company will evaluate further allocation changes to equity securities, other investments and fixed income securities as funding levels change.
See Note 12 for further details regarding how fair value is determined, including the level within the fair value hierarchy and the procedures we use to validate fair value measurements. The Company classifies substantially all debt securities in Level 2 for pension plan assets. These assets are valued using recent trades of similar securities or are fund investments priced using their daily net asset value that is the exit price. A substantial portion of domestic equity securities within pension assets are classified as Level 1, while international equity funds within pension assets are predominantly classified in Level 2 using daily net asset value.
Securities partnerships, real estate and hedge funds are valued using net asset value as a practical expedient and are excluded from the fair value hierarchy. See Note 12 for additional disclosures related to these assets invested in the separate accounts of the Company's subsidiaries. Certain securities as described in Note 12, as well as commercial mortgage loans and guaranteed deposit account contracts, are classified in Level 3 because unobservable inputs used in their valuation are significant.
F.401(k) Plans
The Company sponsors a 401(k) plan in which the Company matches a portion of employees' pre-tax contributions. Participants in the plan may invest in various funds that invest in the Company's common stock, several diversified stock funds, a bond fund or a fixed-income fund.
The Company may elect to increase its matching contributions if the Company's annual performance meets certain targets. The Company's annual expense for these plans was as follows:
| (In millions) | 2021 | 2020 | 2019 | |||||||||||||||||
| Expense | $ | 268 | $ | 243 | $ | 256 | ||||||||||||||
125
Note 17 – Employee Incentive Plans
A.About Our Plans
The People Resources Committee (the "Committee") of the Board of Directors awards stock options, restricted stock grants, restricted stock units, deferred stock and strategic performance shares to certain employees. The Company issues original issue shares for these awards.
The Company records compensation expense for stock and option awards over their vesting periods primarily based on the estimated fair value at the grant date. Fair value is determined differently for each type of award as discussed below.
Shares of common stock available for award at December 31, were as follows:
| (In millions) | 2021 | 2020 | 2019 | |||||||||||||||||
| Common shares available for award | 19.1 | 20.6 | 23.2 | |||||||||||||||||
B.Stock Options
Accounting policy. The Company awards options to purchase Cigna common stock at the market price of the stock on the grant date. Options vest over periods ranging from one year to three years and expire no later than 10 years from grant date. Fair value is estimated using the Black-Scholes option-pricing model by applying the assumptions presented below. That fair value is reduced by options expected to be forfeited during the vesting period. The Company estimates forfeitures at the grant date based on our experience and adjusts the expense to reflect actual forfeitures over the vesting period. The fair value of options, net of forfeitures, is recognized in Selling, general and administrative expenses on a straight-line basis over the vesting period.
Black-Scholes option-pricing model assumptions and the resulting fair value of options are presented in the following table:
| 2021 | 2020 | 2019 | |||||||||||||||||||||
| Dividend yield | 1.85 | % | — | % | — | % | |||||||||||||||||
| Expected volatility | 30.0 | % | 30.0 | % | 30.0 | % | |||||||||||||||||
| Risk-free interest rate | 0.5 | % | 1.4 | % | 2.5 | % | |||||||||||||||||
| Expected option life | 4.5 years | 4.5 years | 4.4 years | ||||||||||||||||||||
| Weighted average fair value of options | $ | 44.84 | $ | 52.42 | $ | 53.10 | |||||||||||||||||
The dividend yield reflects expected future dividends. In 2021, the Company increased its dividend and expects to continue dividends at least at that level for the foreseeable future. The expected volatility reflects the past daily stock price volatility of Cigna stock. The Company does not consider volatility implied in the market prices of traded options to be a good indicator of future volatility because remaining traded options will expire within one year. The risk-free interest rate is derived using the four-year U.S. Treasury bond yield rate as of the award date for the primary annual grant. Expected option life reflects the Company's historical experience.
The following table shows the status of, and changes in, common stock options during the last three years:
| (Options in thousands) | 2021 | 2020 | 2019 | |||||||||||||||||||||||||||||||||||
| Options | Weighted Average Exercise Price | Options | Weighted Average Exercise Price | Options | Weighted Average Exercise Price | |||||||||||||||||||||||||||||||||
| Outstanding - January 1 | 9,742 | $ | 152.40 | 11,438 | $ | 136.19 | 12,370 | $ | 125.46 | |||||||||||||||||||||||||||||
| Granted | 1,524 | $ | 213.81 | 1,851 | $ | 191.86 | 1,569 | $ | 183.41 | |||||||||||||||||||||||||||||
| Exercised | (2,584) | $ | 129.08 | (3,289) | $ | 115.38 | (2,297) | $ | 106.75 | |||||||||||||||||||||||||||||
| Expired or canceled | (192) | $ | 199.10 | (258) | $ | 188.79 | (204) | $ | 180.08 | |||||||||||||||||||||||||||||
| Outstanding - December 31 | 8,490 | $ | 169.47 | 9,742 | $ | 152.40 | 11,438 | $ | 136.19 | |||||||||||||||||||||||||||||
| Options exercisable at year-end | 5,612 | $ | 152.92 | 6,837 | $ | 137.08 | 8,874 | $ | 123.87 | |||||||||||||||||||||||||||||
Compensation expense of $63 million related to unvested stock options at December 31, 2021 will be recognized over the next two years (weighted average period).
126
The table below summarizes information for stock options exercised during the last three years:
| (In millions) | 2021 | 2020 | 2019 | |||||||||||||||||
| Intrinsic value of options exercised | $ | 268 | $ | 304 | $ | 180 | ||||||||||||||
| Cash received for options exercised | $ | 326 | $ | 376 | $ | 224 | ||||||||||||||
| Tax benefit from options exercised | $ | 50 | $ | 57 | $ | 34 | ||||||||||||||
The following table summarizes information for outstanding common stock options at December 31, 2021:
| Options Outstanding | Options Exercisable | |||||||||||||
| Number (in thousands) | 8,490 | 5,612 | ||||||||||||
| Total intrinsic value (in millions) | $ | 511 | $ | 430 | ||||||||||
| Weighted average exercise price | $ | 169.47 | $ | 152.92 | ||||||||||
| Weighted average remaining contractual life | 6.0 years | 4.8 years | ||||||||||||
C.Restricted Stock
The Company awards restricted stock (grants and units) to the Company's employees that vest over periods ranging from to three years. Recipients of restricted stock awards accumulate dividends during the vesting period, but generally forfeit their awards and accumulated dividends if their employment terminates before the vesting date.
Accounting policy. Fair value of restricted stock awards is equal to the market price of Cigna's common stock on the date of grant. This fair value is reduced by awards that are expected to forfeit. At the grant date, the Company estimates forfeitures based on experience and adjusts the expense to reflect actual forfeitures over the vesting period. This fair value, net of forfeitures, is recognized in Selling, general and administrative expenses over the vesting period on a straight-line basis.
The following table shows the status of and changes in restricted stock awards during the last three years:
| (Awards in thousands) | 2021 | 2020 | 2019 | |||||||||||||||||||||||||||||||||||
| Grants/Units | Weighted Average Fair Value at Award Date | Grants/Units | Weighted Average Fair Value at Award Date | Grants/Units | Weighted Average Fair Value at Award Date | |||||||||||||||||||||||||||||||||
| Outstanding - January 1 | 1,600 | $ | 186.12 | 1,945 | $ | 178.78 | 2,138 | $ | 168.12 | |||||||||||||||||||||||||||||
| Awarded | 899 | $ | 213.82 | 791 | $ | 191.22 | 870 | $ | 183.86 | |||||||||||||||||||||||||||||
| Vested | (866) | $ | 184.07 | (1,026) | $ | 161.58 | (964) | $ | 160.74 | |||||||||||||||||||||||||||||
| Forfeited | (109) | $ | 197.01 | (110) | $ | 186.63 | (99) | $ | 168.68 | |||||||||||||||||||||||||||||
| Outstanding - December 31 | 1,524 | $ | 202.85 | 1,600 | $ | 186.12 | 1,945 | $ | 178.78 | |||||||||||||||||||||||||||||
The fair value of vested restricted stock at the vesting date for the years ended December 31 was as follows:
| (In millions) | 2021 | 2020 | 2019 | |||||||||||||||||
| Fair value of vested restricted stock | $ | 183 | $ | 190 | $ | 171 | ||||||||||||||
Approximately 10,300 employees held 1.5 million restricted stock awards at the end of 2021 with $168 million of related compensation expense to be recognized over the next two years (weighted average period).
D.Strategic Performance Shares ("SPS")
The Company awards SPSs to executives and certain other key employees generally with a performance period of three years. Half of these shares are subject to a market condition (total shareholder return relative to industry peer companies) and half are subject to a performance condition (cumulative adjusted net income). These targets are set by the Committee at the beginning of the performance period. Holders of these awards receive shares of Cigna common stock at the end of the performance period ranging anywhere from 0 to 200% of the original awards.
Accounting policy. Compensation expense for SPSs is recorded over the performance period. Fair value is determined at the grant date for "market condition" SPSs using a Monte Carlo simulation model and not subsequently adjusted regardless of the final outcome. Expense is initially accrued for "performance condition" SPSs based on the most likely outcome, but evaluated for adjustment each period for updates in the expected outcome. Expense is adjusted to the actual outcome (number of shares awarded times the share price at the grant date) at the end of the performance period.
127
The following table shows the status of and changes in SPSs during the last three years:
| 2021 | 2020 | 2019 | ||||||||||||||||||||||||||||||||||||
| (Awards in thousands) | Shares | Weighted Average Fair Value at Award Date | Shares | Weighted Average Fair Value at Award Date | Shares | Weighted Average Fair Value at Award Date | ||||||||||||||||||||||||||||||||
| Outstanding - January 1 | 808 | $ | 190.02 | 818 | $ | 177.94 | 707 | $ | 160.74 | |||||||||||||||||||||||||||||
| Awarded | 331 | $ | 213.90 | 362 | $ | 191.52 | 389 | $ | 184.72 | |||||||||||||||||||||||||||||
| Vested | (206) | $ | 196.29 | (309) | $ | 159.67 | (244) | $ | 139.27 | |||||||||||||||||||||||||||||
| Forfeited | (73) | $ | 197.38 | (63) | $ | 187.76 | (34) | $ | 178.98 | |||||||||||||||||||||||||||||
| Outstanding - December 31 | 860 | $ | 197.07 | 808 | $ | 190.02 | 818 | $ | 177.94 | |||||||||||||||||||||||||||||
The weighted average fair value per share of SPSs for expense purposes, including the Monte Carlo factor, at the award date for the years ended December 31, 2021, 2020 and 2019 was $239.57, $206.86 and $192.11, respectively.
The fair value of vested SPSs at the vesting date for the years ended December 31 was as follows:
| 2021 | 2020 | 2019 | ||||||||||||||||||||||||||||||||||||
| (Shares in thousands; $ in millions) | Shares | Fair Value | Shares | Fair Value | Shares | Fair Value | ||||||||||||||||||||||||||||||||
| Shares of Cigna common stock distributed upon SPS vesting | 243 | $ | 51 | 306 | $ | 55 | 254 | $ | 45 | |||||||||||||||||||||||||||||
Approximately 500 employees held 860,000 SPSs at the end of 2021 and $66 million of related compensation expense is expected to be recognized over the next two years. The amount of expense for "performance condition" SPSs will vary based on actual performance in 2022 and 2023.
E.Compensation Cost and Tax Effects of Share-based Compensation
The Company records tax benefits in Shareholders' net income during the vesting period based on the amount of expense being recognized. The difference between tax benefits based on the expense and the actual tax benefit realized are also recorded in Net income when stock options are exercised, or when restricted stock and SPSs vest.
| (In millions) | 2021 | 2020 | 2019 | |||||||||||||||||
| Total compensation cost for shared-based awards | $ | 268 | $ | 289 | $ | 299 | ||||||||||||||
| Tax benefits recognized | $ | 73 | $ | 63 | $ | 59 | ||||||||||||||
128
Note 18 – Goodwill, Other Intangibles and Property and Equipment
A.Goodwill
Accounting policy. Goodwill represents the excess of the cost of businesses acquired over the fair value of their net assets. The resulting goodwill is assigned to those reporting units expected to realize cash flows from the acquisition, based on those reporting units' relative fair values. As a result, goodwill is primarily reported in the Evernorth segment ($35.1 billion) and the Cigna Healthcare segment ($10.7 billion). The Company's reporting units are aligned with its operating segments as described in Note 1.
The Company conducts its annual quantitative evaluation for goodwill impairment during the third quarter at the reporting unit level and writes it down through shareholders' net income if impaired. On a quarterly basis, the Company performs a qualitative impairment assessment to determine if events or changes in circumstances indicate that it is more likely than not that the carrying value of a reporting unit exceeds its estimated fair value. Fair value of a reporting unit is generally estimated based on both a discounted cash flow analysis and a market approach using assumptions that the Company believes a hypothetical market participant would use to determine a current transaction price. The significant assumptions and estimates used in determining fair value primarily include the discount rate and future cash flows. A discount rate is selected to correspond with each reporting unit's weighted average cost of capital, consistent with that used for investment decisions considering the specific and detailed operating plans and strategies within that reporting unit. Projections of future cash flows differ by reporting unit and are consistent with our strategic projection processes. Future cash flows for Evernorth are primarily driven by the forecasted gross margins of the business, as well as operating expenses and long-term growth rates. Future cash flows for our other reporting units are primarily driven by forecasted revenues, benefit expenses, operating expenses and long-term growth rates.
Goodwill activity. Goodwill activity during 2021 and 2020 was as follows:
| (In millions) | 2021 | 2020 | ||||||||||||
| Balance at January 1, | $ | 44,648 | $ | 44,602 | ||||||||||
| Goodwill acquired, net | 1,428 | 29 | ||||||||||||
| Impact of foreign currency translation | (31) | 17 | ||||||||||||
| Total | 46,045 | |||||||||||||
| Goodwill classified as Assets of businesses held for sale | (234) | |||||||||||||
| Goodwill per Consolidated Balance Sheets at December 31, | $ | 45,811 | $ | 44,648 | ||||||||||
B.Other Intangibles
Accounting policy. The Company's other intangible assets primarily include purchased customer and producer relationships, provider networks and trademarks. The fair value of purchased customer relationships and the amortization method were determined as of the dates of purchase using an income approach that relies on projected future net cash flows including key assumptions for customer attrition and discount rates. The Company's definite-lived intangible assets are amortized on an accelerated or straight-line basis, reflecting their pattern of economic benefits, over periods from to 30 years. Management revises amortization periods if it believes there has been a change in the length of time that an intangible asset will continue to have value. Costs incurred to renew or extend the terms of these intangible assets are generally expensed as incurred.
The Company's amortized intangible assets are tested for impairment whenever events or changes in circumstances indicate that the carrying amount may not be recoverable. If the total of the expected future undiscounted cash flows generated by the underlying asset group is less than the carrying amount of the asset group, the Company recognizes an impairment charge equal to the difference between the carrying value of the asset group and its estimated fair value. The Company's indefinite-lived intangible assets are each reviewed for impairment at least annually by comparing their fair value with their carrying value. If the carrying value exceeds fair value, that excess is recognized as an impairment loss.
There were no material impairments in the years ended December 31, 2021, 2020 or 2019.
129
Components of other assets, including other intangibles. Other intangible assets were comprised of the following at December 31:
| (In millions) | Cost | Accumulated Amortization | Net Carrying Value | |||||||||||||||||
| 2021 | ||||||||||||||||||||
| Customer relationships | $ | 29,997 | 4,539 | 25,458 | ||||||||||||||||
| Trade Name - Express Scripts | 8,400 | 8,400 | ||||||||||||||||||
| Other | 447 | 81 | 366 | |||||||||||||||||
| Other intangible assets | 38,844 | 4,620 | 34,224 | |||||||||||||||||
| Value of business acquired ("VOBA" reported in Deferred policy acquisition costs) | 646 | 171 | 475 | |||||||||||||||||
Total (1) | $ | 39,490 | 4,791 | 34,699 | ||||||||||||||||
| 2020 | ||||||||||||||||||||
| Customer relationships | $ | 29,432 | 3,024 | 26,408 | ||||||||||||||||
| Trade Name - Express Scripts | 8,400 | 8,400 | ||||||||||||||||||
| Other | 475 | 104 | 371 | |||||||||||||||||
| Other intangible assets | 38,307 | 3,128 | 35,179 | |||||||||||||||||
| Value of business acquired (reported in Deferred policy acquisition costs) | 670 | 152 | 518 | |||||||||||||||||
| Total | $ | 38,977 | 3,280 | 35,697 | ||||||||||||||||
(1) Includes $386 million of VOBA and $122 million of Other intangible assets classified as Assets of businesses held for sale.
The Company has indefinite-lived intangible assets totaling $8.5 billion at December 31, 2021 and $8.5 billion at December 31, 2020, largely consisting of trade names and licenses.
C.Property and Equipment
Accounting policy. Property and equipment is carried at cost less accumulated depreciation. Cost includes interest, real estate taxes and other costs incurred during construction when applicable. Internal-use software that is acquired, developed or modified solely to meet the Company's internal needs, with no plan to market externally, is also included in this category. Costs directly related to acquiring, developing or modifying internal-use software are capitalized.
The Company calculates depreciation and amortization principally using the straight-line method generally based on the estimated useful life of each asset as follows: buildings and improvements, 10 to 40 years; purchased software, to five years; internally developed software, to seven years and furniture and equipment (including computer equipment), to 10 years. Improvements to leased facilities are depreciated over the lesser of the remaining lease term or the estimated life of the improvement. The Company considers events and circumstances that would indicate the carrying value of property, equipment or capitalized software might not be recoverable. An impairment charge is recorded if the Company determines the carrying value of any of these assets is not recoverable. The Company also reviews and shortens the estimated useful lives of these assets, if necessary.
Components of property and equipment. Property and equipment was comprised of the following as of December 31:
| (In millions) | Cost | Accumulated Amortization | Net Carrying Value | |||||||||||||||||
| 2021 | ||||||||||||||||||||
| Internal-use software | $ | 7,869 | $ | 5,060 | $ | 2,809 | ||||||||||||||
| Other property and equipment | 2,839 | 1,653 | 1,186 | |||||||||||||||||
| Total | 10,708 | 6,713 | 3,995 | |||||||||||||||||
| Property and equipment classified as Assets of businesses held for sale | (424) | (121) | (303) | |||||||||||||||||
| Total Property and equipment per Consolidated Balance Sheets | $ | 10,284 | $ | 6,592 | $ | 3,692 | ||||||||||||||
| 2020 | ||||||||||||||||||||
| Internal-use software | $ | 7,061 | $ | 4,048 | $ | 3,013 | ||||||||||||||
| Other property and equipment | 2,719 | 1,527 | 1,192 | |||||||||||||||||
| Total property and equipment | $ | 9,780 | $ | 5,575 | $ | 4,205 | ||||||||||||||
130
Components of depreciation and amortization. Depreciation and amortization expense was comprised of the following for the years ended December 31:
| (In millions) | 2021 | 2020 | 2019 | |||||||||||||||||
| Internal-use software | $ | 1,097 | $ | 971 | $ | 850 | ||||||||||||||
| Other property and equipment | 253 | 276 | 284 | |||||||||||||||||
| Value of business acquired (reported in Deferred policy acquisition costs) | 25 | 28 | 34 | |||||||||||||||||
| Other intangibles | 1,548 | 1,527 | 2,483 | |||||||||||||||||
| Total depreciation and amortization | $ | 2,923 | $ | 2,802 | $ | 3,651 | ||||||||||||||
The Company estimates annual pre-tax amortization for intangible assets, including internal-use software, over the next five calendar years to be as follows:
| (In millions) | Pre-tax Amortization | |||||||
| 2022 | $ | 2,651 | ||||||
| 2023 | $ | 2,293 | ||||||
| 2024 | $ | 1,961 | ||||||
| 2025 | $ | 1,792 | ||||||
| 2026 | $ | 1,543 | ||||||
131
Note 19 – Leases
The Company's leases are primarily for office space and certain computer and other equipment and have terms of up to 35 years.
Accounting policy. The Company determines if an arrangement is a lease and its lease classification (operating or finance) at inception. Both operating and finance leases result in (1) a right-of-use ("ROU") asset that represents our right to use the underlying asset for the lease term and (2) a lease liability that represents our obligation to make lease payments arising from the lease. ROU assets and lease liabilities are reflected in the following lines in the Company's Consolidated Balance Sheet:
| ROU Asset | Current Lease Liability | Non-Current Lease Liability | ||||||||||||||||||
| Operating lease | ||||||||||||||||||||
| Finance lease | ||||||||||||||||||||
These lease assets and liabilities are recognized at the lease commencement date based on the present value of the lease payments over the lease term. Most of the Company's leases do not provide an implicit rate, so the Company uses its incremental borrowing rate based on the information available at commencement date in determining the present value of lease payments. The ROU asset also includes any lease pre-payments made and excludes lease incentives for operating leases. The Company's expected life of a lease may consider options to extend or terminate a lease when it is reasonably certain that the Company will exercise that option.
The Company has lease agreements with lease and non-lease components that are accounted for as a single lease component. Operating lease ROU assets are amortized on a straight-line basis over the lease term, which is representative of the pattern in which benefit is expected to be derived from the right to use the underlying asset. Variable lease payments are expensed as incurred and represent amounts that are neither fixed in nature, such as maintenance and other services provided by the lessor, nor tied to an index or rate.
The components of lease expense were as follows:
| For the Years Ended December 31, | ||||||||||||||||||||
| (In millions) | 2021 | 2020 | 2019 | |||||||||||||||||
| Operating lease cost | $ | 170 | $ | 190 | $ | 188 | ||||||||||||||
| Finance lease cost: | ||||||||||||||||||||
| Amortization of ROU assets | 22 | 28 | 28 | |||||||||||||||||
| Interest on lease liabilities | 2 | 3 | 3 | |||||||||||||||||
| Total finance lease cost | 24 | 31 | 31 | |||||||||||||||||
| Variable lease cost | 39 | 48 | 50 | |||||||||||||||||
| Total lease cost | $ | 233 | $ | 269 | $ | 269 | ||||||||||||||
In addition, the Company recognized $33 million of one-time selling, general and administrative expenses related to abandonment of leased assets associated with the Organizational Efficiency Plan. See Note 15 for further information.
Supplemental cash flow information related to leases was as follows:
| For the Years Ended December 31, | ||||||||||||||||||||
| (In millions) | 2021 | 2020 | 2019 | |||||||||||||||||
| Cash paid for amounts included in the measurement of lease liabilities: | ||||||||||||||||||||
| Operating cash outflows from operating leases | $ | 167 | $ | 189 | $ | 173 | ||||||||||||||
| Operating cash outflows from finance leases | $ | 2 | $ | 3 | $ | 3 | ||||||||||||||
| Financing cash outflows from finance leases | $ | 22 | $ | 26 | $ | 25 | ||||||||||||||
| ROU assets obtained in exchange for lease obligations: | ||||||||||||||||||||
| Operating leases | $ | 122 | $ | 189 | $ | 89 | ||||||||||||||
| Finance leases | $ | 20 | $ | 9 | $ | 68 | ||||||||||||||
132
Operating and finance lease ROU assets and lease liabilities were as follows:
| (In millions) | December 31, 2021 | December 31, 2020 | ||||||||||||
Operating leases: (1) | ||||||||||||||
| Operating lease ROU assets | $ | 478 | $ | 552 | ||||||||||
| $ | 159 | $ | 152 | |||||||||||
| 436 | 491 | |||||||||||||
| Total operating lease liabilities | $ | 595 | $ | 643 | ||||||||||
| Finance leases: | ||||||||||||||
| Property and equipment, gross | $ | 101 | $ | 98 | ||||||||||
| Accumulated depreciation | (51) | (46) | ||||||||||||
| $ | 50 | $ | 52 | |||||||||||
| $ | 23 | $ | 18 | |||||||||||
| 28 | 36 | |||||||||||||
| Total finance lease liabilities | $ | 51 | $ | 54 | ||||||||||
(1) Operating leases include Assets of $27 million and Liabilities of $28 million in businesses held for sale.
As of December 31, 2021, the weighted average remaining lease term was 5 years for operating leases and 4 years for finance leases, and the weighted average discount rate was 2.81% for operating leases and 3.13% for finance leases.
Maturities of lease liabilities as of December 31, 2021 were as follows:
| (In millions) | Operating Leases | Finance Leases | ||||||||||||
| 2022 | $ | 152 | $ | 25 | ||||||||||
| 2023 | 132 | 12 | ||||||||||||
| 2024 | 107 | 6 | ||||||||||||
| 2025 | 70 | 3 | ||||||||||||
| 2026 | 66 | 3 | ||||||||||||
| Thereafter | 114 | 6 | ||||||||||||
| Total lease payments | 641 | 55 | ||||||||||||
| Less: imputed interest | 46 | 4 | ||||||||||||
Total (1) | $ | 595 | $ | 51 | ||||||||||
(1) Operating leases include Liabilities of $28 million in businesses held for sale.
Note 20 – Shareholders' Equity and Dividend Restrictions
State insurance departments and foreign jurisdictions that regulate certain of the Company's subsidiaries prescribe accounting practices (differing in some respects from GAAP) to determine statutory net income and surplus. The Company's life, accident and health insurance and Health Maintenance Organization ("HMO") subsidiaries are regulated by such statutory requirements. The statutory net income of the Company's life, accident and health insurance and HMO subsidiaries for the years ended, and their statutory surplus as of December 31, were as follows:
| (In billions) | 2021 | 2020 | 2019 | |||||||||||||||||
| Net income | $ | 3.4 | $ | 4.0 | $ | 3.8 | ||||||||||||||
| Surplus | $ | 13.3 | $ | 12.9 | $ | 13.8 | ||||||||||||||
133
The Company's HMO and life, accident and health insurance subsidiaries are also subject to minimum statutory surplus requirements and may be required to maintain investments on deposit with state departments of insurance or other regulatory bodies. Additionally, these subsidiaries may be subject to regulatory restrictions on the amount of annual dividends or other distributions (such as loans or cash advances) that insurance companies may extend to their parent companies without prior approval. As of December 31, 2021, these amounts, including restricted GAAP net assets of the Company's subsidiaries, were as follows:
| (In billions) | 2021 | |||||||
Minimum statutory surplus required by regulators (1),(2) | $ | 4.9 | ||||||
Investments on deposit with regulatory bodies (3) | $ | 0.3 | ||||||
Maximum dividend distributions permitted in 2022 without regulatory approval (4) | $ | 3.2 | ||||||
| Maximum loans to the parent company permitted without regulatory approval | $ | 0.8 | ||||||
Restricted GAAP net assets of Cigna Corporation's subsidiaries (5) | $ | 12.9 | ||||||
(1) Excludes amounts associated with foreign operated equity method joint ventures.
(2) Includes approximately $1 billion associated with businesses held for sale.
(3) Includes approximately $40 million associated with businesses held for sale.
(4) Includes approximately $200 million associated with businesses held for sale.
(5) Includes approximately $3.0 billion associated with businesses held for sale.
Permitted practices used by the Company's insurance subsidiaries in 2021 that differed from prescribed regulatory accounting had an immaterial impact on statutory surplus.
Undistributed earnings for equity method subsidiaries are $1.1 billion as of December 31, 2021.
Note 21 – Income Taxes
Accounting policy. Deferred income taxes are reflected in the Consolidated Balance Sheets for differences between the financial and income tax reporting bases of the Company's underlying assets and liabilities, and are established based upon enacted tax rates and laws. Deferred income tax assets are recognized when available evidence indicates that realization is more likely than not and a valuation allowance is established to the extent this standard is not met. The deferred income tax provision generally represents the net change in deferred income tax assets and liabilities during the reporting period excluding adjustments to accumulated other comprehensive income or amounts recorded in connection with a business combination. The current income tax provision generally represents estimated amounts due on income tax returns for the year reported to various jurisdictions plus the effect of any uncertain tax positions. The Company recognizes a liability for uncertain tax positions if management believes the probability that the positions will be sustained is 50% or less. For uncertain positions that management believes are more likely than not to be sustained, the Company recognizes a liability based upon management's estimate of the most likely settlement outcome with the taxing authority. The liabilities for uncertain tax positions are classified as current when the position is expected to be settled within 12 months or the statute of limitation expires within 12 months.
Income taxes attributable to the Company's foreign operations are generally provided using the respective foreign jurisdictions' tax rate.
134
A.Income Tax Expense
The components of income taxes for the years ended December 31 were as follows:
| (In millions) | 2021 | 2020 | 2019 | |||||||||||||||||
| Current taxes | ||||||||||||||||||||
| U.S. income taxes | $ | 1,268 | $ | 2,128 | $ | 1,476 | ||||||||||||||
| Foreign income taxes | 207 | 334 | 173 | |||||||||||||||||
| State income taxes | 112 | 303 | 114 | |||||||||||||||||
| Total current taxes | 1,587 | 2,765 | 1,763 | |||||||||||||||||
| Deferred taxes (benefits) | ||||||||||||||||||||
| U.S. income taxes (benefits) | (167) | (217) | (236) | |||||||||||||||||
| Foreign income taxes | 69 | 11 | 16 | |||||||||||||||||
| State income tax (benefits) | (122) | (180) | (93) | |||||||||||||||||
| Total deferred taxes (benefits) | (220) | (386) | (313) | |||||||||||||||||
| Total income taxes | $ | 1,367 | $ | 2,379 | $ | 1,450 | ||||||||||||||
Total income taxes for the years ended December 31 were different from the amount computed using the nominal federal income tax rate for the following reasons:
| 2021 | 2020 | 2019 | |||||||||||||||||||||||||||||||||||||||
| (In millions) | $ | % | $ | % | $ | % | |||||||||||||||||||||||||||||||||||
| Tax expense at nominal rate | $ | 1,424 | 21.0 | % | $ | 2,282 | 21.0 | % | $ | 1,380 | 21.0 | % | |||||||||||||||||||||||||||||
| Impact of sale of business | — | — | 104 | 1.0 | — | — | |||||||||||||||||||||||||||||||||||
| Effect of foreign earnings | (33) | (0.5) | (61) | (0.6) | 24 | 0.4 | |||||||||||||||||||||||||||||||||||
| Health insurance industry tax | — | — | 93 | 0.9 | — | — | |||||||||||||||||||||||||||||||||||
| State income tax (net of federal income tax benefit) | (9) | (0.1) | 24 | 0.2 | 32 | 0.5 | |||||||||||||||||||||||||||||||||||
| Other | (15) | (0.2) | (63) | (0.6) | 14 | 0.2 | |||||||||||||||||||||||||||||||||||
| Total income taxes | $ | 1,367 | 20.2 | % | $ | 2,379 | 21.9 | % | $ | 1,450 | 22.1 | % | |||||||||||||||||||||||||||||
Consolidated pre-tax income from the Company's foreign operations was approximately 26% of the Company's pre-tax income in 2021, 14% in 2020 and 12% in 2019.
135
B.Deferred Income Taxes
Deferred income tax assets and liabilities as of December 31, were as follows:
| (In millions) | 2021 | 2020 | ||||||||||||
Deferred tax assets | ||||||||||||||
| Employee and retiree benefit plans | $ | 304 | $ | 477 | ||||||||||
| Other insurance and contractholder liabilities | 263 | 278 | ||||||||||||
| Loss carryforwards | 278 | 177 | ||||||||||||
| Other accrued liabilities | 412 | 358 | ||||||||||||
| Other | 245 | 209 | ||||||||||||
| Deferred tax assets before valuation allowance | 1,503 | 1,499 | ||||||||||||
| Valuation allowance for deferred tax assets | (246) | (207) | ||||||||||||
| Deferred tax assets, net of valuation allowance | 1,257 | 1,292 | ||||||||||||
| Deferred tax liabilities | ||||||||||||||
| Depreciation and amortization | 698 | 660 | ||||||||||||
| Acquisition-related basis differences | 8,726 | 8,989 | ||||||||||||
| Policy acquisition expenses | 312 | 289 | ||||||||||||
| Unrealized appreciation on investments and foreign currency translation | 104 | 171 | ||||||||||||
| Other | 212 | 122 | ||||||||||||
| Total deferred tax liabilities | 10,052 | 10,231 | ||||||||||||
| Net deferred income tax (liabilities) | (8,795) | |||||||||||||
| Net deferred income tax (liabilities) assets classified as Liabilities of businesses held for sale | (449) | |||||||||||||
| Net deferred income tax (liabilities) assets per Consolidated Balance Sheets | $ | (8,346) | $ | (8,939) | ||||||||||
Management believes that future results will be sufficient to realize a majority of the Company's gross deferred tax assets. Valuation allowances are established against deferred tax assets when it is determined that it is more likely than not that the asset will not be recognized. Valuation allowances have been established against certain federal, state and foreign tax attributes. There are multiple expiration dates associated with these tax attributes.
C.Uncertain Tax Positions
Reconciliations of unrecognized tax benefits for the years ended December 31 were as follows:
| (In millions) | 2021 | 2020 | 2019 | |||||||||||||||||
| Balance at January 1, | $ | 1,210 | $ | 1,018 | $ | 928 | ||||||||||||||
| Increase due to prior year positions | 21 | 128 | 68 | |||||||||||||||||
| Increase due to current year positions | 31 | 88 | 29 | |||||||||||||||||
| Reduction related to settlements with taxing authorities | (15) | — | — | |||||||||||||||||
| Reduction related to lapse of applicable statute of limitations | (17) | (24) | (7) | |||||||||||||||||
| Balance at December 31, | $ | 1,230 | $ | 1,210 | $ | 1,018 | ||||||||||||||
Substantially all unrecognized tax benefits would impact shareholders' net income if recognized.
The Company classifies net interest expense on uncertain tax positions as a component of income tax expense and in Accrued expenses and other liabilities on the balance sheet. In addition to the amounts in the table above, the liability for net interest expense on uncertain tax positions was approximately $148 million as of December 31, 2021, $127 million as of December 31, 2020 and $100 million as of December 31, 2019.
D.Other Tax Matters
The statute of limitations for Cigna's consolidated federal income tax returns through 2016 have closed. However, Cigna filed amended returns for both the 2015 and 2016 tax years, which are under review by the Internal Revenue Service ("IRS"). Additionally, the IRS is examining Cigna's returns for 2017 and 2018. The statute of limitations for Express Scripts' consolidated federal income tax returns through 2012 has closed. However, for 2010 through 2012 tax years, there remains a significant disputed matter. The IRS is also examining Express Scripts' consolidated federal income tax returns for 2013 through 2018. The Company has established adequate reserves for these matters.
136
The Company conducts business in a number of state and foreign jurisdictions and may be engaged in multiple audit proceedings at any given time. Generally, no further state or foreign audit activity is expected for tax years prior to 2013 for Cigna's entities and 2006 for Express Scripts' entities.
Note 22 – Contingencies and Other Matters
The Company, through its subsidiaries, is contingently liable for various guarantees provided in the ordinary course of business.
A.Financial Guarantees: Retiree and Life Insurance Benefits
The Company guarantees that separate account assets will be sufficient to pay certain life insurance or retiree benefits. For the majority of these benefits, the sponsoring employers are primarily responsible for ensuring that assets are sufficient to pay these benefits and are required to maintain assets that exceed a certain percentage of benefit obligations. If employers fail to do so, the Company or an affiliate of the buyer of the retirement benefits business has the right to redirect the management of the related assets to provide for benefit payments. As of December 31, 2021, employers maintained assets that generally exceeded the benefit obligations under these arrangements of approximately $440 million. An additional liability is established if management believes that the Company will be required to make payments under the guarantees; there were no additional liabilities required for these guarantees, net of reinsurance, as of December 31, 2021. Separate account assets supporting these guarantees are classified in Levels 1 and 2 of the GAAP fair value hierarchy.
The Company does not expect that these financial guarantees will have a material effect on the Company's consolidated results of operations, liquidity or financial condition.
B.Certain Other Guarantees
The Company had indemnification obligations as of December 31, 2021 in connection with acquisition and disposition transactions. These indemnification obligations are triggered by the breach of representations or covenants provided by the Company, such as representations for the presentation of financial statements, filing of tax returns, compliance with law or identification of outstanding litigation. These obligations are typically subject to various time limitations, defined by the contract or by operation of law, such as statutes of limitation. In some cases, the maximum potential amount due is subject to contractual limitations based on a percentage of the transaction purchase price, while in other cases limitations are not specified or applicable. The Company does not believe that it is possible to determine the maximum potential amount due under these obligations because not all amounts due under these indemnification obligations are subject to limitation. There were no liabilities for these indemnification obligations as of December 31, 2021.
C.Guaranty Fund Assessments
The Company operates in a regulatory environment that may require its participation in assessments under state insurance guaranty association laws. The Company's exposure to assessments for certain obligations of insolvent insurance companies to policyholders and claimants is based on its share of business written in the relevant jurisdictions.
There were no material charges or credits resulting from existing or new guaranty fund assessments for the year ended December 31, 2021.
D.Legal and Regulatory Matters
The Company is routinely involved in numerous claims, lawsuits, regulatory inquiries and audits, government investigations, including under the federal False Claims Act and state false claims acts initiated by a government investigating body or by a qui tam relator's filing of a complaint under court seal and other legal matters arising, for the most part, in the ordinary course of managing a global health services business. Additionally, the Company has received and is cooperating with subpoenas or similar processes from various governmental agencies requesting information, all arising in the normal course of its business. Disputed tax matters arising from audits by the Internal Revenue Service or other state and foreign jurisdictions, including those resulting in litigation, are accounted for under GAAP guidance for uncertain tax positions. See Note 21 for additional information on tax matters.
Pending litigation and legal or regulatory matters that the Company has identified with a reasonably possible material loss and certain other material litigation matters are described below. For those matters that the Company has identified with a reasonably possible material loss, the Company provides disclosure in the aggregate of accruals and range of loss, or a statement that such information cannot be estimated. The Company's accruals for the matters discussed below under "Litigation Matters" and "Regulatory Matters" are not material. Due to numerous uncertain factors presented in these cases, it is not possible to estimate an aggregate range of loss (if
137
any) for these matters at this time. In light of the uncertainties involved in these matters, there is no assurance that their ultimate resolution will not exceed the amounts currently accrued by the Company. An adverse outcome in one or more of these matters could be material to the Company's results of operations, financial condition or liquidity for any particular period. The outcomes of lawsuits are inherently unpredictable and we may be unsuccessful in these ongoing litigation matters or any future claims or litigation.
Litigation Matters
Express Scripts Litigation with Anthem. In March 2016, Anthem filed a lawsuit in the United States District Court for the Southern District of New York alleging various breach of contract claims against Express Scripts relating to the parties' rights and obligations under the periodic pricing review section of the pharmacy benefit management agreement between the parties including allegations that Express Scripts failed to negotiate new pricing concessions in good faith, as well as various alleged service issues. Anthem also requested that the court enter declaratory judgment that Express Scripts is required to provide Anthem competitive benchmark pricing, that Anthem can terminate the agreement and that Express Scripts is required to provide Anthem with post-termination services at competitive benchmark pricing for one year following any termination by Anthem. Anthem claims it is entitled to $13 billion in additional pricing concessions over the remaining term of the agreement, as well as $1.8 billion for one year following any contract termination by Anthem and $150 million damages for service issues ("Anthem's Allegations"). On April 19, 2016, in response to Anthem's complaint, Express Scripts filed its answer denying Anthem's Allegations in their entirety and asserting affirmative defenses and counterclaims against Anthem. The court subsequently granted Anthem's motion to dismiss two of six counts of Express Scripts' amended counterclaims. Express Scripts filed its Motion for Summary Judgment on August 27, 2021. Anthem completed filing of its Response to Express Scripts' Motion for Summary Judgment on October 16, 2021. Express Scripts filed its Reply in Support of its Motion for Summary Judgment on November 19, 2021. There is no tentative trial date.
Medicare Advantage. A qui tam action that was filed by a relator in the United States District Court for the Southern District of New York in 2017 was unsealed on August 6, 2020. The action asserts claims related to risk adjustment practices arising from certain health exams conducted as part of the Company's Medicare Advantage business. In September 2021, the qui tam action was transferred to the United States District Court for the Middle District of Tennessee. On January 11, 2022, the U.S. Department of Justice ("DOJ") (U.S. Attorney's Offices for the Southern District of New York and the Middle District of Tennessee) filed a motion to partially intervene which is pending before the court. The Company has opposed the DOJ's motion to intervene and the government filed its reply brief on February 1, 2022. The motion has been fully briefed and is under the court's review.
Regulatory Matters
Civil Investigative Demand. The DOJ is conducting industry-wide investigations of Medicare Advantage organizations' risk adjustment practices. For certain Medicare Advantage organizations, including Cigna, those investigations have resulted in litigation (see above). The Company is currently responding to information requests (civil investigative demand) from the DOJ (U.S. Attorney's Office for the Eastern District of Pennsylvania). The Company is cooperating with the DOJ and has responded and continues to respond to its requests.
Note 23 – Segment Information
See Note 1 for a description of our segments, including the segment change effective in the fourth quarter of 2021. Prior year segment information has been adjusted to reflect the segment change and a description of our basis of reporting segment operating results is outlined below. Intersegment revenues primarily reflect pharmacy related transactions between the Evernorth and Cigna Healthcare segments.
The Company uses "pre-tax adjusted income (loss) from operations" and "adjusted revenues" as its principal financial measures of segment operating performance because management believes these metrics best reflect the underlying results of business operations and permit analysis of trends in underlying revenue, expenses and profitability. We define pre-tax adjusted income from operations as income before income taxes excluding net realized investment results, amortization of acquired intangible assets, results of transitioning clients prior to 2020, and special items. Cigna's share of certain realized investment results of its joint ventures reported in the Cigna Healthcare segment using the equity method of accounting are also excluded. Special items are matters that management believes are not representative of the underlying results of operations due to their nature or size. Adjusted income (loss) from operations is measured on an after-tax basis for consolidated results and on a pre-tax basis for segment results.
The Company defines adjusted revenues as total revenues excluding the following adjustments: special items, revenue contribution from transitioning clients prior to 2020, and Cigna's share of certain realized investment results of its joint ventures reported in the Cigna Healthcare segment using the equity method of accounting. Special items are matters that management believes are not representative of the underlying results of operations due to their nature or size. We exclude these items from this measure because management believes they are not indicative of past or future underlying performance of the business.
138
The Company does not report total assets by segment because this is not a metric used to allocate resources or evaluate segment performance.
The following tables present the special items recorded by the Company for the year ended December 31, 2021, 2020 and 2019:
| (In millions) | 2021 | 2020 | 2019 | ||||||||||||||||||||||||||||||||
| Description of Special Item Charges (Benefits) and Financial Statement Line Item(s) | After-tax | Before-tax | After-tax | Before-tax | After-tax | Before-tax | |||||||||||||||||||||||||||||
| Charge for organizational efficiency plan (Selling, general and administrative expenses) | $ | 119 | $ | 168 | $ | 24 | $ | 31 | $ | 162 | $ | 207 | |||||||||||||||||||||||
| Debt extinguishment costs | 110 | 141 | 151 | 199 | — | — | |||||||||||||||||||||||||||||
| Integration and transaction-related (benefits) costs (Selling, general and administrative expenses) | 71 | 169 | 404 | 527 | 427 | 552 | |||||||||||||||||||||||||||||
| (Benefits) charges associated with litigation matters (Selling, general and administrative expenses) | (21) | (27) | 19 | 25 | 41 | 51 | |||||||||||||||||||||||||||||
| Risk corridors recovery (Selling, general and administrative expenses) | — | — | (76) | (101) | — | — | |||||||||||||||||||||||||||||
| Contractual adjustment for a former client (Pharmacy revenues) | — | — | (155) | (204) | — | — | |||||||||||||||||||||||||||||
| (Gain) on sale of business | — | — | (3,217) | (4,203) | — | — | |||||||||||||||||||||||||||||
| Total impact from special items | $ | 279 | $ | 451 | $ | (2,850) | $ | (3,726) | $ | 630 | $ | 810 | |||||||||||||||||||||||
139
Summarized segment financial information was as follows:
| (In millions) | Evernorth | Cigna Healthcare | Other Operations | Corporate and Eliminations | Total | |||||||||||||||||||||||||||
| 2021 | ||||||||||||||||||||||||||||||||
| Revenues from external customers | $ | 127,692 | $ | 41,378 | $ | 3,459 | $ | — | $ | 172,529 | ||||||||||||||||||||||
| Inter-segment revenues | 4,203 | 2,271 | — | (6,474) | ||||||||||||||||||||||||||||
| Net investment income | 17 | 1,003 | 530 | (1) | 1,549 | |||||||||||||||||||||||||||
| Total revenues | 131,912 | 44,652 | 3,989 | (6,475) | 174,078 | |||||||||||||||||||||||||||
Net realized investment results from certain equity method investments | — | — | — | — | — | |||||||||||||||||||||||||||
| Adjusted revenues | $ | 131,912 | $ | 44,652 | $ | 3,989 | $ | (6,475) | $ | 174,078 | ||||||||||||||||||||||
| Depreciation and amortization | $ | 2,316 | $ | 551 | $ | 52 | $ | 4 | $ | 2,923 | ||||||||||||||||||||||
| Income (loss) before taxes | $ | 3,908 | $ | 3,812 | $ | 852 | $ | (1,790) | $ | 6,782 | ||||||||||||||||||||||
| Pre-tax adjustments to reconcile to adjusted income from operations | ||||||||||||||||||||||||||||||||
| (Income) attributable to noncontrolling interests | (31) | (3) | (24) | — | (58) | |||||||||||||||||||||||||||
Net realized investment (gains) losses (1) | 4 | (247) | 47 | — | (196) | |||||||||||||||||||||||||||
| Amortization of acquired intangible assets | 1,937 | 47 | 14 | — | 1,998 | |||||||||||||||||||||||||||
| Special items | ||||||||||||||||||||||||||||||||
| Charge for organizational efficiency plan | — | — | — | 168 | 168 | |||||||||||||||||||||||||||
| Debt extinguishment costs | — | — | — | 141 | 141 | |||||||||||||||||||||||||||
| Integration and transaction-related (benefits) costs | — | — | — | 169 | 169 | |||||||||||||||||||||||||||
| (Benefits) charges associated with litigation matters | — | — | — | (27) | (27) | |||||||||||||||||||||||||||
| Pre-tax adjusted income (loss) from operations | $ | 5,818 | $ | 3,609 | $ | 889 | $ | (1,339) | $ | 8,977 | ||||||||||||||||||||||
| (In millions) | Evernorth | Cigna Healthcare | Other Operations | Corporate and Eliminations | Total | |||||||||||||||||||||||||||
| 2020 | ||||||||||||||||||||||||||||||||
Revenues from external customers | $ | 112,647 | $ | 38,826 | $ | 7,684 | $ | — | $ | 159,157 | ||||||||||||||||||||||
| Inter-segment revenues | 3,655 | 1,966 | 23 | (5,644) | ||||||||||||||||||||||||||||
| Net investment income | 32 | 473 | 739 | — | 1,244 | |||||||||||||||||||||||||||
| Total revenues | 116,334 | 41,265 | 8,446 | (5,644) | 160,401 | |||||||||||||||||||||||||||
| Net realized investment results from certain equity method investments | — | (130) | — | — | (130) | |||||||||||||||||||||||||||
| Special item related to contractual adjustment for a former client | (204) | — | — | — | (204) | |||||||||||||||||||||||||||
| Adjusted revenues | $ | 116,130 | $ | 41,135 | $ | 8,446 | $ | (5,644) | $ | 160,067 | ||||||||||||||||||||||
| Depreciation and amortization | $ | 2,248 | $ | 458 | $ | 71 | $ | 25 | $ | 2,802 | ||||||||||||||||||||||
| Income (loss) before taxes | $ | 3,684 | $ | 4,291 | $ | 5,227 | $ | (2,334) | $ | 10,868 | ||||||||||||||||||||||
| Pre-tax adjustments to reconcile to adjusted income from operations | ||||||||||||||||||||||||||||||||
| (Income) attributable to noncontrolling interests | (17) | (1) | (19) | — | (37) | |||||||||||||||||||||||||||
Net realized investment (gains) losses (1) | (17) | (202) | (60) | — | (279) | |||||||||||||||||||||||||||
| Amortization of acquired intangible assets | 1,917 | 44 | 21 | — | 1,982 | |||||||||||||||||||||||||||
| Special items | ||||||||||||||||||||||||||||||||
| Charge for organizational efficiency plan | — | — | — | 31 | 31 | |||||||||||||||||||||||||||
| Debt extinguishment costs | — | — | — | 199 | 199 | |||||||||||||||||||||||||||
| Integration and transaction-related (benefits) costs | — | — | — | 527 | 527 | |||||||||||||||||||||||||||
| (Benefits) charges associated with litigation matters | — | — | — | 25 | 25 | |||||||||||||||||||||||||||
| Risk corridors recovery | — | (101) | — | — | (101) | |||||||||||||||||||||||||||
| Contractual adjustment for a former client | (204) | — | — | — | (204) | |||||||||||||||||||||||||||
| (Gain) on sale of business | — | — | (4,203) | — | (4,203) | |||||||||||||||||||||||||||
| Pre-tax adjusted income (loss) from operations | $ | 5,363 | $ | 4,031 | $ | 966 | $ | (1,552) | $ | 8,808 | ||||||||||||||||||||||
(1) Includes the Company's share of certain realized investment results of its joint ventures reported in the Cigna Healthcare segment using the equity method of accounting.
140
| (In millions) | Evernorth | Cigna Healthcare | Other Operations | Corporate and Eliminations | Total | |||||||||||||||||||||||||||
| 2019 | ||||||||||||||||||||||||||||||||
| Revenues from external customers | $ | 107,354 | $ | 37,455 | $ | 7,367 | $ | — | $ | 152,176 | ||||||||||||||||||||||
| Inter-segment revenues | 2,380 | 1,168 | 26 | (3,574) | ||||||||||||||||||||||||||||
| Net investment income (loss) | 60 | 510 | 822 | (2) | 1,390 | |||||||||||||||||||||||||||
| Total revenues | 109,794 | 39,133 | 8,215 | (3,576) | 153,566 | |||||||||||||||||||||||||||
| Revenue contributions from transitioning clients | (13,347) | — | — | — | (13,347) | |||||||||||||||||||||||||||
| Net realized investment results from certain equity method investments | — | (44) | — | — | (44) | |||||||||||||||||||||||||||
| Adjusted revenues | $ | 96,447 | $ | 39,089 | $ | 8,215 | $ | (3,576) | $ | 140,175 | ||||||||||||||||||||||
| Depreciation and amortization | $ | 3,071 | $ | 492 | $ | 85 | $ | 3 | $ | 3,651 | ||||||||||||||||||||||
| Income (loss) before taxes | $ | 3,983 | $ | 4,071 | $ | 1,180 | $ | (2,664) | $ | 6,570 | ||||||||||||||||||||||
| Pre-tax adjustments to reconcile to adjusted income from operations | ||||||||||||||||||||||||||||||||
| Adjustment for transitioning clients | (1,726) | — | — | — | (1,726) | |||||||||||||||||||||||||||
| (Income) attributable to noncontrolling interests | (4) | — | (16) | — | (20) | |||||||||||||||||||||||||||
Net realized investment (gains) losses (1) | — | (159) | (62) | — | (221) | |||||||||||||||||||||||||||
| Amortization of acquired intangible assets | 2,839 | 81 | 29 | — | 2,949 | |||||||||||||||||||||||||||
| Special items | ||||||||||||||||||||||||||||||||
| Charge for organizational efficiency plan | — | — | — | 207 | 207 | |||||||||||||||||||||||||||
| Integration and transaction-related (benefits) costs | — | — | — | 552 | 552 | |||||||||||||||||||||||||||
| (Benefits) charges associated with litigation matters | — | (30) | — | 81 | 51 | |||||||||||||||||||||||||||
| Pre-tax adjusted income (loss) from operations | $ | 5,092 | $ | 3,963 | $ | 1,131 | $ | (1,824) | $ | 8,362 | ||||||||||||||||||||||
(1) Includes the Company's share of certain realized investment gains (losses) of its joint ventures reported in the Cigna Healthcare segment using the equity method of accounting.
141
Revenue from external customers includes Pharmacy revenues, Premiums and Fees and other revenues. The following table presents these revenues by product, premium and service type for the year ended December 31:
| (In millions) | 2021 | 2020 | 2019 | |||||||||||||||||
| Products (Pharmacy revenues) (ASC 606) | ||||||||||||||||||||
| Network revenues | $ | 64,992 | $ | 56,365 | $ | 51,430 | ||||||||||||||
| Home delivery and specialty revenues | 54,391 | 49,906 | 49,226 | |||||||||||||||||
| Other | 6,428 | 5,403 | 4,900 | |||||||||||||||||
| Intercompany eliminations | (4,398) | (3,905) | (2,457) | |||||||||||||||||
| Total pharmacy revenues | 121,413 | 107,769 | 103,099 | |||||||||||||||||
| Insurance premiums (ASC 944) | ||||||||||||||||||||
| Cigna Healthcare | ||||||||||||||||||||
| U.S. Commercial | ||||||||||||||||||||
| Insured | 14,315 | 13,389 | 12,523 | |||||||||||||||||
| Stop loss | 4,868 | 4,614 | 4,328 | |||||||||||||||||
| Other | 1,290 | 1,135 | 1,040 | |||||||||||||||||
| U.S. Government | ||||||||||||||||||||
| Medicare Advantage | 8,362 | 7,565 | 6,314 | |||||||||||||||||
| Medicare Part D | 1,499 | 1,593 | 1,699 | |||||||||||||||||
| Other | 4,815 | 4,301 | 4,185 | |||||||||||||||||
| International Health | 2,588 | 2,472 | 2,382 | |||||||||||||||||
| Total Cigna Healthcare | 37,737 | 35,069 | 32,471 | |||||||||||||||||
| International businesses held for sale | 3,205 | 3,039 | 2,884 | |||||||||||||||||
| Domestic disability, life and accident | — | 4,423 | 4,225 | |||||||||||||||||
| Other | 221 | 124 | 147 | |||||||||||||||||
| Intercompany eliminations | (9) | (28) | (13) | |||||||||||||||||
| Total premiums | 41,154 | 42,627 | 39,714 | |||||||||||||||||
| Services (Fees) (ASC 606) | ||||||||||||||||||||
Evernorth | 6,070 | 4,611 | 4,165 | |||||||||||||||||
Cigna Healthcare | 5,743 | 5,491 | 6,022 | |||||||||||||||||
Other Operations | 19 | 116 | 123 | |||||||||||||||||
| Other revenues | 197 | 254 | 157 | |||||||||||||||||
| Intercompany eliminations | (2,067) | (1,711) | (1,104) | |||||||||||||||||
| Total fees and other revenues | 9,962 | 8,761 | 9,363 | |||||||||||||||||
| Total revenues from external customers | $ | 172,529 | $ | 159,157 | $ | 152,176 | ||||||||||||||
Foreign and U.S. revenues from external customers for the three years ended December 31 are shown below. The Company's foreign revenues are generated by its foreign operating entities. In the periods shown, no foreign country contributed more than 2% of consolidated revenues from external customers.
| (In millions) | 2021 | 2020 | 2019 | |||||||||||||||||
| United States | $ | 166,626 | $ | 154,042 | $ | 147,332 | ||||||||||||||
Foreign countries (1) | 5,903 | 5,115 | 4,844 | |||||||||||||||||
| Total | $ | 172,529 | $ | 159,157 | $ | 152,176 | ||||||||||||||
(1) International life, accident and supplemental benefits businesses in seven countries to be sold pursuant to the Chubb Transaction as described in Note 1 comprised of $3.2 billion, $3.1 billion and $2.9 billion in 2021, 2020 and 2019, respectively.
Revenues from U.S. Federal Government agencies, under a number of contracts, were 14% of consolidated revenues in 2021, 15% in 2020 and 14% in 2019. These amounts were reported in the Evernorth and Cigna Healthcare segments.
142
Item 9. CHANGES IN AND DISAGREEMENTS WITH ACCOUNTANTS ON ACCOUNTING AND FINANCIAL DISCLOSURE
None.
Item 9A. CONTROLS AND PROCEDURES
A.Disclosure Controls and Procedures
Based on an evaluation of the effectiveness of Cigna's disclosure controls and procedures conducted under the supervision and with the participation of Cigna's management (including Cigna's Chief Executive Officer and Chief Financial Officer), Cigna's Chief Executive Officer and Chief Financial Officer concluded that, as of the end of the period covered by this report, Cigna's disclosure controls and procedures are effective to ensure that information required to be disclosed by Cigna in the reports that it files or submits under the Exchange Act is recorded, processed, summarized and reported, within the time periods specified in the Securities and Exchange Commission's rules and forms and is accumulated and communicated to Cigna's management, including Cigna's Chief Executive Officer and Chief Financial Officer, as appropriate to allow timely decisions regarding required disclosure.
B.Internal Control Over Financial Reporting
Management's Annual Report on Internal Control over Financial Reporting
Management of Cigna Corporation is responsible for establishing and maintaining adequate internal control over financial reporting. The Company's internal controls were designed to provide reasonable assurance that the Company's consolidated published financial statements for external purposes were prepared in accordance with accounting principles generally accepted in the United States. The Company's internal control over financial reporting includes those policies and procedures that:
(i)pertain to the maintenance of records that, in reasonable detail, accurately and fairly reflect the transactions and dispositions of the assets of the Company;
(ii)provide reasonable assurance that transactions are recorded as necessary to permit preparation of financial statements in accordance with accounting principles generally accepted in the United States and that receipts and expenditures of the Company are being made only in accordance with authorization of management and directors of the Company; and
(iii)provide reasonable assurance regarding prevention or timely detection of unauthorized acquisitions, use or disposition of the Company's assets that could have a material effect on the financial statements.
Because of its inherent limitations, internal control over financial reporting may not prevent or detect misstatements.
Management assessed the effectiveness of the Company's internal control over financial reporting as of December 31, 2021. In making this assessment, management used the criteria set forth by the Committee of Sponsoring Organizations of the Treadway Commission ("COSO") in Internal Control-Integrated Framework (2013). Based on management's assessment and the criteria set forth by COSO, it was determined that the Company's internal control over financial reporting is effective as of December 31, 2021.
The Company's independent registered public accounting firm, PricewaterhouseCoopers LLP, has audited the effectiveness of the Company's internal control over financial reporting, as stated in their report located in Item 8 of this Form 10-K.
Change in Internal Control over Financial Reporting
There have been no changes in our internal control over financial reporting during the quarter ended December 31, 2021 that have materially affected, or are reasonably likely to materially affect, Cigna's internal control over financial reporting.
Item 9B. OTHER INFORMATION
Effective as of February 22, 2022, the Board of Directors of the Company adopted restated by-laws (the “By-Laws”) in order to make certain clarifications and ministerial changes relating to the responsibilities of the Chair of the Board.
The foregoing summary does not purport to be a complete description of the By-Laws and is qualified in its entirety by reference to the complete text of the By-Laws, a copy of which is filed herewith as Exhibit 3.2 to this Annual Report on Form 10-K and is incorporated by reference in this Item 9B.
143
Item 9C. DISCLOSURE REGARDING FOREIGN JURISDICTIONS THAT PREVENT INSPECTIONS
Not applicable.
144
PART III
Item 10. DIRECTORS, EXECUTIVE OFFICERS AND CORPORATE GOVERNANCE
A.Directors of the Registrant
The information under the captions "Corporate Governance Matters – Board of Directors' Nominees" and "– Board Meetings and Committees" (as it relates to Audit Committee disclosure) in Cigna's definitive proxy statement related to the 2022 annual meeting of shareholders is incorporated herein by reference.
B.Executive Officers of the Registrant
See Part I – "Information about our Executive Officers" in this Form 10-K.
C.Code of Ethics and Other Corporate Governance Disclosures
The information under the caption "Corporate Governance Matters – Codes of Ethics" in Cigna's definitive proxy statement related to the 2022 annual meeting of shareholders is incorporated herein by reference. We intend to promptly disclose on our website, in accordance with applicable rules, any required disclosure of changes to or waivers, if any, of our Code of Ethics or our Director Code of Business Conduct and Ethics.
D.Delinquent Section 16(a) Reports
The information under the caption "Ownership of Cigna Common Stock – Delinquent Section 16(a) Reports", if included in Cigna's definitive proxy statement related to the 2022 annual meeting of shareholders, is incorporated herein by reference.
Item 11. EXECUTIVE COMPENSATION
The information under the captions "Corporate Governance Matters – Non-Employee Director Compensation," "Certain Transactions – Compensation Committee Interlocks and Inside Participation," "Compensation Matters – Compensation Discussion and Analysis," "– Report of the People Resources Committee" and "– Executive Compensation Tables" in Cigna's definitive proxy statement related to the 2022 annual meeting of shareholders is incorporated herein by reference.
145
Item 12. SECURITY OWNERSHIP OF CERTAIN BENEFICIAL OWNERS AND MANAGEMENT AND RELATED STOCKHOLDER MATTERS
The following table presents information regarding Cigna's equity compensation plans as of December 31, 2021:
(a) (1) | (b) (2) | (c) (3) | ||||||||||||||||||
| Plan Category | Securities To Be Issued Upon Exercise Of Outstanding Options, Warrants And Rights | Weighted Average Exercise Price Of Outstanding Options, Warrants And Rights | Securities Remaining Available For Future Issuance Under Equity Compensation Plans (Excluding Securities Reflected In Column (a)) | |||||||||||||||||
| Equity Compensation Plans Approved by Security Holders | 10,348,718 | $ | 169.47 | 19,105,282 | ||||||||||||||||
| Equity Compensation Plans Not Approved by Security Holders | — | — | — | |||||||||||||||||
| Total | 10,348,718 | $ | 169.47 | 19,105,282 | ||||||||||||||||
(1)Includes, in addition to outstanding stock options:
(i) 78,070 restricted stock units, 61,201 deferred shares and 1,719,282 strategic performance shares that are reported at the maximum 200% payout rate granted under the Cigna Long-Term Incentive Plan, the Cigna Corporation Stock Plan and the Cigna Corporation Director Equity Plan; and
(ii) 545,035 shares of common stock underlying stock option awards granted under the Express Scripts Holding Company 2016 Long-Term Incentive Plan, 892,421 shares of common stock underlying stock option awards granted under the Express Scripts, Inc. 2011 Long-Term Incentive Plan, 530,092 shares of common stock underlying stock option awards granted under the Medco Health Solutions, Inc. 2002 Stock Incentive Plan and 13,798 shares of common stock underlying stock option awards granted under the Accredo Health, Incorporated 2002 Long-Term Incentive Plan that were all approved by the applicable company's shareholders before Cigna's acquisition of Express Scripts in December 2018.
(2)The weighted-average exercise price is based only on outstanding stock options. The outstanding stock options assumed due to Cigna's acquisition of Express Scripts, in aggregate, have a weighted-average exercise price of $148.00. Excluding the assumed options from this acquisition results in a weighted-average exercise price of $176.00.
(3)Represents 19,105,282 shares of common stock available as of the close of business December 31, 2021 for future issuance under the Cigna Long-Term Incentive Plan. No further grants may be made and no shares remain available for future issuance under any plan other than the Cigna Long-Term Incentive Plan.
The information under the captions "Ownership of Cigna Common Stock – Stock Held by Directors, Nominees and Executive Officers" and "Ownership of Cigna Common Stock – Stock Held by Certain Beneficial Owners" in Cigna's definitive proxy statement related to the 2022 annual meeting of shareholders is incorporated herein by reference.
Item 13. CERTAIN RELATIONSHIPS AND RELATED TRANSACTIONS, AND DIRECTOR INDEPENDENCE
The information under the captions "Corporate Governance Matters – Director Independence" and "– Certain Transactions" in Cigna's definitive proxy statement related to the 2022 annual meeting of shareholders is incorporated herein by reference.
Item 14. PRINCIPAL ACCOUNTANT FEES AND SERVICES
The information under the captions "Audit Matters – Policy for the Pre-Approval of Audit and Non-Audit Services" and "– Fees to Independent Registered Public Accounting Firm" in Cigna’s definitive proxy statement related to the 2022 annual meeting of shareholders is incorporated herein by reference.
146
PART IV
Item 15. EXHIBITS AND FINANCIAL STATEMENT SCHEDULES
(a)(1) The following Financial Statements can be found under Part II Item 8 of this Form 10-K:
Report of Independent Registered Public Accounting Firm. (Public Company Accounting Oversight Board ID: 238)
Consolidated Statements of Income for the years ended December 31, 2021, 2020 and 2019.
Consolidated Statements of Comprehensive Income for the years ended December 31, 2021, 2020 and 2019.
Consolidated Balance Sheets as of December 31, 2021 and 2020.
Consolidated Statements of Changes in Total Equity for the years ended December 31, 2021, 2020 and 2019.
Consolidated Statements of Cash Flows for the years ended December 31, 2021, 2020 and 2019.
Notes to the Consolidated Financial Statements.
(2)The financial statement schedules listed in the Index to Financial Statement Schedules on page FS-1 which list is incorporated herein.
(3)Set forth in this Item 15 is a list of exhibits filed or incorporated by reference as part of this Annual Report on Form 10-K.
(b)The exhibits listed in the accompanying "Index to Exhibits" in this Item 15 are filed or incorporated by reference as part of this Annual Report on Form 10-K.
(c)The financial statement schedules listed in the Index to Financial Statement Schedules on page FS-1 are filed as part of this Annual Report on Form 10-K.
147
INDEX TO EXHIBITS
| Number | Description | Method of Filing | ||||||
| 2.1(a) | Filed by Cigna Holding Company ("CHC") as Exhibit 2.1 to the Current Report on Form 8-K on March 13, 2018 and incorporated herein by reference. | |||||||
| 2.1(b) | Filed by CHC as Exhibit 2.1 to the Current Report on Form 8-K on July 2, 2018 and incorporated herein by reference. | |||||||
| 3.1 | Filed by the registrant as Exhibit 3.1 to the Current Report on Form 8-K on December 20, 2018 and incorporated herein by reference. | |||||||
| 3.2 | Filed herewith. | |||||||
| 4.1(a) | Filed by CHC as Exhibit 4.1 to the Current Report on Form 8-K on September 21, 2018 and incorporated herein by reference. | |||||||
| 4.1(b) | Filed by CHC as Exhibit 4.2 to the Current Report on Form 8-K on September 21, 2018 and incorporated herein by reference. | |||||||
| 4.1(c) | Filed by the registrant as Exhibit 4.7 to the Current Report on Form 8-K on December 20, 2018 and incorporated herein by reference. | |||||||
| 4.1(d) | Filed by the registrant as Exhibit 4.1 to the Current Report on Form 8-K on October 11, 2019 and incorporated herein by reference. | |||||||
| 4.1(e) | Filed by the registrant as Exhibit 4.1 to the Current Report on Form 8-K on March 16, 2020 and incorporated herein by reference. | |||||||
| 4.1(f) | Filed by the registrant as Exhibit 4.1 to the Current Report on Form 8-K on March 3, 2021 and incorporated herein by reference. | |||||||
| 4.2 | Filed by the registrant as Exhibit 4.2 to the Current Report on Form 8-K on October 11, 2019 and incorporated herein by reference. | |||||||
| 4.3(a) | Filed by CHC as Exhibit 4.1(a) to the Annual Report on Form 10-K for the year ended December 31, 2012 and incorporated herein by reference. | |||||||
| 4.3(b) | Filed by CHC as Exhibit 4.1(b) to the Annual Report on Form 10-K for the year ended December 31, 2012 and incorporated herein by reference. | |||||||
| 4.3(c) | Filed by CHC as Exhibit 4.1(c) to the Quarterly Report on Form 10-Q for the quarterly period ended March 31, 2011 and incorporated herein by reference. | |||||||
| 4.3(d) | Filed by CHC as Exhibit 4.1 to the Current Report on Form 8-K on March 10, 2008 and incorporated herein by reference. | |||||||
| 4.3(e) | Filed by CHC as Exhibit 99.2 to the Current Report on Form 8-K on May 28, 2010 and incorporated herein by reference. | |||||||
148
| 4.3(f) | Filed by CHC as Exhibit 99.2 to the Current Report on Form 8-K on December 9, 2010 and incorporated herein by reference. | |||||||
| 4.3(g) | Filed by CHC as Exhibit 99.2 to the Current Report on Form 8-K on March 8, 2011 and incorporated herein by reference. | |||||||
| 4.3(h) | Filed by CHC as Exhibit 4.1 to the Current Report on Form 8-K on November 14, 2011 and incorporated herein by reference. | |||||||
| 4.3(i) | Filed by CHC as Exhibit 4.1 to the Current Report on Form 8-K on March 26, 2015 and incorporated herein by reference. | |||||||
| 4.3(j) | Filed by CHC as Exhibit 4.1 to the Current Report on Form 8-K filed September 14, 2017 and incorporated herein by reference. | |||||||
| 4.3(k) | Filed by the registrant as Exhibit 4.1 to the Current Report on Form 8-K on December 20, 2018 and incorporated herein by reference. | |||||||
| 4.3(l) | Filed by the registrant as Exhibit 4.3 to the Current Report on Form 8-K on October 11, 2019 and incorporated herein by reference. | |||||||
| 4.4(a) | Filed by CHC as Exhibit 4.2 to the Annual Report on Form 10-K for the year ended December 31, 2009 and incorporated herein by reference. | |||||||
| 4.4(b) | Filed by the registrant as Exhibit 4.2 to the Current Report on Form 8-K on December 20, 2018 and incorporated herein by reference. | |||||||
| 4.4(c) | Filed by the registrant as Exhibit 4.4 to the Current Report on Form 8-K on October 11, 2019 and incorporated herein by reference. | |||||||
| 4.5(a) | Filed by CHC as Exhibit 4.3 to the Annual Report on Form 10-K for the year ended December 31, 2009 and incorporated herein by reference. | |||||||
| 4.5(b) | Filed by the registrant as Exhibit 4.3 to the Current Report on Form 8-K on December 20, 2018 and incorporated herein by reference. | |||||||
| 4.6(a) | Filed by Express Scripts, Inc. ("ESI") as Exhibit 4.1 to the Current Report on Form 8-K filed November 25, 2011 and incorporated herein by reference. | |||||||
| 4.6(b) | Filed by ESI as Exhibit 4.4 to the Current Report on Form 8-K on November 25, 2011 and incorporated herein by reference. | |||||||
| 4.6(c) | Filed by ESI as Exhibit 4.5 to the Current Report on Form 8-K on November 25, 2011 and incorporated herein by reference. | |||||||
| 4.6(d) | Seventh Supplemental Indenture, dated as of February 9, 2012, among Express Scripts, Inc., Express Scripts Holding Company, the other subsidiaries of Express Scripts Holding Company party thereto and Wells Fargo Bank, National Association, as trustee, related to Express Scripts Holding Company's 3.900% senior notes due 2022 | Filed by ESI as Exhibit 4.3 to the Current Report on Form 8-K filed February 10, 2012 and incorporated herein by reference. | ||||||
149
| 4.6(e) | Filed by Express Scripts Holding Company ("ESRX") as Exhibit 4.1 to the Current Report on Form 8-K on April 6, 2012 and incorporated herein by reference. | |||||||
| 4.6(f) | Filed by ESRX as Exhibit 4.1 to the Current Report on Form 8-K on June 5, 2014 and incorporated herein by reference. | |||||||
| 4.6(g) | Filed by ESRX as Exhibit 4.2 to the Current Report on Form 8-K on June 5, 2014 and incorporated herein by reference. | |||||||
| 4.6(h) | Filed by ESRX as Exhibit 4.3 to the Current Report on Form 8-K on June 5, 2014 and incorporated herein by reference. | |||||||
| 4.6(i) | Filed by ESRX as Exhibit 4.1 to the Current Report on Form 8-K on February 25, 2016 and incorporated herein by reference. | |||||||
| 4.6(j) | Filed by ESRX as Exhibit 4.2 to the Current Report on Form 8-K on February 25, 2016 and incorporated herein by reference. | |||||||
| 4.6(k) | Filed by ESRX as Exhibit 4.1 to the Current Report on Form 8-K on July 5, 2016 and incorporated herein by reference. | |||||||
| 4.6(l) | Filed by ESRX as Exhibit 4.2 to the Current Report on Form 8-K on July 5, 2016 and incorporated herein by reference. | |||||||
| 4.6(m) | Filed by ESRX as Exhibit 4.3 to the Current Report on Form 8-K on July 5, 2016 and incorporated herein by reference. | |||||||
| 4.6(n) | Filed by ESRX as Exhibit 4.1 to the Current Report on Form 8-K on November 30, 2017 and incorporated herein by reference. | |||||||
| 4.6(o) | Filed by ESRX as Exhibit 4.2 to the Current Report on Form 8-K on November 30, 2017 and incorporated herein by reference. | |||||||
| 4.6(p) | Filed by ESRX as Exhibit 4.3 to the Current Report on Form 8-K on November 30, 2017 and incorporated herein by reference. | |||||||
| 4.6(q) | Filed by the registrant as Exhibit 4.4 to the Current Report on Form 8-K on December 20, 2018 and incorporated herein by reference. | |||||||
| 4.6(r) | Filed by the registrant as Exhibit 4.5 to the Current Report on Form 8-K on October 11, 2019 and incorporated herein by reference. | |||||||
| 4.7(a) | Filed by ESI as Exhibit 4.1 to the Current Report on Form 8-K on June 10, 2009 and incorporated herein by reference. | |||||||
| 4.7(b) | Filed by ESI as Exhibit 4.4 to the Current Report on Form 8-K on June 10, 2009 and incorporated herein by reference. | |||||||
150
| 4.7(c) | Filed by ESI as Exhibit 4.6 to the Current Report on Form 8-K on November 25, 2011 and incorporated herein by reference. | |||||||
| 4.7(d) | Filed by ESRX as Exhibit 4.2 to the Current Report on Form 8-K on April 6, 2012 and incorporated herein by reference. | |||||||
| 4.7(e) | Filed by the registrant as Exhibit 4.5 to the Current Report on Form 8-K on December 20, 2018 and incorporated herein by reference. | |||||||
| 4.8 | Filed by the registrant as Exhibit 4.8 to the Annual Report on Form 10-K for the year ended December 31, 2020 and incorporated herein by reference. | |||||||
Exhibits 10.1 through 10.37 are identified as compensatory plans, management contracts or arrangements pursuant to Item 15 of Form 10-K.
| 10.1(a) | Filed by the registrant as Exhibit 10.1 to the Current Report on Form 8-K on May 3, 2021 and incorporated herein by reference. | |||||||
| 10.1(b) | Filed by CHC as Exhibit 10.21 to Form 10-K for the year ended December 31, 2011 and incorporated herein by reference. | |||||||
| 10.1(c) | Filed by CHC as Exhibit 10.2 to Form 10-Q for the period ended March 31, 2014 and incorporated herein by reference. | |||||||
| 10.1(d) | Filed by CHC as Exhibit 10.3 to Form 10-Q for the period ended March 31, 2015 and incorporated herein by reference. | |||||||
| 10.1(e) | Filed by CHC as Exhibit 10.3 to Form 10-Q for the period ended March 31, 2017 and incorporated herein by reference. | |||||||
| 10.1(f) | Filed by CHC as Exhibit 10.5 to Quarterly Report on Form 10-Q for the period ended March 31, 2018 and incorporated herein by reference. | |||||||
| 10.1(g) | Filed by the registrant as Exhibit 10.1 to Quarterly Report on Form 10-Q for the period ended March 31, 2019 and incorporated herein by reference. | |||||||
| 10.1(h) | Filed by the registrant as Exhibit 10.2 to Quarterly Report on Form 10-Q for the period ended March 31, 2019 and incorporated herein by reference. | |||||||
| 10.1(i) | Filed by the registrant as Exhibit 10.3 to Quarterly Report on Form 10-Q for the period ended March 31, 2019 and incorporated herein by reference. | |||||||
10.1(j) | Filed by the registrant as Exhibit 10.4 to Quarterly Report on Form 10-Q for the period ended March 31, 2019 and incorporated herein by reference. | |||||||
| 10.1(k) | Filed by the registrant as Exhibit 10.1 to Quarterly Report on Form 10-Q for the period ended March 31, 2020 and incorporated herein by reference. | |||||||
151
| 10.1(l) | Filed by the registrant as Exhibit 10.2 to Quarterly Report on Form 10-Q for the period ended March 31, 2020 and incorporated herein by reference. | |||||||
| 10.1(m) | Filed by the registrant as Exhibit 10.3 to Quarterly Report on Form 10-Q for the period ended March 31, 2020 and incorporated herein by reference. | |||||||
10.1(n) | Filed by the registrant as Exhibit 10.4 to Quarterly Report on Form 10-Q for the period ended March 31, 2020 and incorporated herein by reference. | |||||||
10.1(o) | Filed by the registrant as Exhibit 10.1 to Quarterly Report on Form 10-Q for the period ended March 31, 2021 and incorporated herein by reference. | |||||||
10.1(p) | Filed by the registrant as Exhibit 10.2 to Quarterly Report on Form 10-Q for the period ended March 31, 2021 and incorporated herein by reference. | |||||||
10.1(q) | Filed by the registrant as Exhibit 10.3 to Quarterly Report on Form 10-Q for the period ended March 31, 2021 and incorporated herein by reference. | |||||||
10.1(r) | Filed by the registrant as Exhibit 10.4 to Quarterly Report on Form 10-Q for the period ended March 31, 2021 and incorporated herein by reference. | |||||||
| 10.1(s) | Filed by the registrant as Exhibit 10.5 to Quarterly Report on Form 10-Q for the period ended March 31, 2020 and incorporated herein by reference. | |||||||
| 10.2 | Filed by CHC as Exhibit 10.7 to the Annual Report on Form 10-K for the year ended December 31, 2009 and incorporated herein by reference. | |||||||
| 10.3 | Filed by CHC as Exhibit 10.5 to the Quarterly Report on Form 10-Q for the quarterly period ended March 31, 2017 and incorporated herein by reference. | |||||||
| 10.4(a) | Filed by ESRX as Appendix A to ESRX's Definitive Proxy Statement on Schedule 14A for its 2016 Annual Meeting of Stockholders, filed March 21, 2016 and incorporated herein by reference. | |||||||
| 10.4(b) | Filed by ESRX as Exhibit 10.4 to the Current Report on Form 8-K on May 4, 2016 and incorporated herein by reference. | |||||||
| 10.4(c) | Filed by ESRX as Exhibit 10.7 to Current Report on Form 8-K on May 4, 2016 and incorporated herein by reference. | |||||||
| 10.5(a) | Filed by the registrant as Exhibit 4.10 to the Registration Statement on Form S-8 (No. 333-228930) on December 20, 2018 and incorporated herein by reference. | |||||||
152
| 10.5(b) | Filed by ESRX as Exhibit 10.6 to Quarterly Report on Form 10-Q for the quarter ended June 30, 2012 and incorporated herein by reference. | |||||||
| 10.5(c) | Filed by ESRX as Exhibit 10.14 to the Current Report on Form 8-K on April 2, 2012 and incorporated herein by reference. | |||||||
| 10.5(d) | Filed by ESRX as Exhibit 10.1 to the Quarterly Report on Form 10-Q for the quarter ended March 31, 2013 and incorporated herein by reference. | |||||||
| 10.6(a) | Filed by the registrant as Exhibit 4.11 to the Registration Statement on Form S-8 (No. 333-228930) on December 20, 2018 and incorporated herein by reference. | |||||||
| 10.6(b) | Filed by Medco Health Solutions, Inc. as Exhibit 10.2 to the Current Report on Form 8-K on February 8, 2005 and incorporated herein by reference. | |||||||
| 10.7 | Filed by the registrant as Exhibit 4.12 to the Registration Statement on Form S-8 (No. 333-228930) on December 20, 2018 and incorporated herein by reference. | |||||||
| 10.8 | Filed by CHC as Exhibit 10.1 to the Annual Report on Form 10-K for the year ended December 31, 2011 and incorporated herein by reference. | |||||||
| 10.9 | Filed by CHC as Exhibit 10.14 to the Annual Report on Form 10-K for the year ended December 31, 2011 and incorporated herein by reference. | |||||||
| 10.10 | Filed by the registrant as Exhibit 4.6 to the Registration Statement on Form S-8 (No. 333-228930) on December 20, 2018 and incorporated herein by reference. | |||||||
| 10.11 | Filed by ESI as Exhibit No. 10.1 to the Current Report on Form 8-K on May 25, 2007 and incorporated herein by reference. | |||||||
| 10.12(a) | Filed by the registrant as Exhibit 4.13 to the Registration Statement on Form S-8 (No. 333-228930) on December 20, 2018 and incorporated herein by reference. | |||||||
| 10.12(b) | Filed by the registrant as Exhibit 10.12(b) to the Annual Report on Form 10-K for the year ended December 31, 2019 and incorporated herein by reference. | |||||||
10.12(c) | Filed by the registrant as Exhibit 10.3 to Quarterly Report on Form 10-Q for the period ended June 30, 2021 and incorporated herein by reference. | |||||||
| 10.13(a) | Filed by CHC as Exhibit 10.15(a) to the Annual Report on Form 10-K for the year ended December 31, 2009 and incorporated herein by reference. | |||||||
| 10.13(b) | Filed by CHC as Exhibit 10.15(b) to the Annual Report on Form 10-K for the year ended December 31, 2009 and incorporated herein by reference. | |||||||
153
| 10.13(c) | Filed by CHC as Exhibit 10.16(c) to the Annual Report on Form 10-K for the year ended December 31, 2011 and incorporated herein by reference. | |||||||
| 10.14(a) | Filed by CHC as Exhibit 10.15 to the Annual Report on Form 10-K for the year ended December 31, 2007 and incorporated herein by reference. | |||||||
| 10.14(b) | Filed by CHC as Exhibit 10.1 to the Quarterly Report on Form 10-Q for the quarterly period ended June 30, 2009 and incorporated herein by reference. | |||||||
| 10.15(a) | Filed by the registrant as Exhibit 4.7 to the Registration Statement on Form S-8 (No. 333-228930) on December 20, 2018 and incorporated herein by reference. | |||||||
| 10.15(b) | Filed by the registrant as Exhibit 10.15(b) to the Annual Report on Form 10-K for the year ended December 31, 2019 and incorporated herein by reference. | |||||||
| 10.15(c) | Filed by the registrant as Exhibit 10.15(c) to the Annual Report on Form 10-K for the year ended December 31, 2019 and incorporated herein by reference. | |||||||
| 10.15(d) | Filed by the registrant as Exhibit 10.15(d) to the Annual Report on Form 10-K for the year ended December 31, 2019 and incorporated herein by reference. | |||||||
| 10.16 | Filed by CHC as Exhibit 10.1 to the Quarterly Report on Form 10-Q for the quarterly period ended March 31, 2014 and incorporated herein by reference. | |||||||
10.17(a) | Filed herewith. | |||||||
10.17(b) | Filed herewith. | |||||||
| 10.18 | Filed by the registrant as Exhibit 10.18 to the Annual Report on Form 10-K for the year ended December 31, 2020 and incorporated herein by reference. | |||||||
| 10.19 | Filed by CHC as Exhibit 10.4 to the Annual Report on Form 10-K for the year ended December 31, 2012 and incorporated herein by reference. | |||||||
| 10.20 | Filed by the registrant as Exhibit 4.8 to the Registration Statement on Form S-8 (No. 333-228930) on December 20, 2018 and incorporated herein by reference. | |||||||
| 10.21 | Filed by ESRX as Exhibit 10.1 to the Current Report on Form 8-K on March 5, 2014 and incorporated herein by reference. | |||||||
| 10.22 | Filed by the registrant as Exhibit 10.1 to the Current Report on Form 8-K on October 30, 2020 and incorporated herein by reference. | |||||||
| 10.23 | Filed by CHC as Exhibit 10.10 to the Annual Report on Form 10-K for the year ended December 31, 2009 and incorporated herein by reference. | |||||||
154
| 10.24 | Filed by CHC as Exhibit 10.1 to the Quarterly Report on Form 10-Q for the quarterly period ended March 31, 2012 and incorporated herein by reference. | |||||||
| 10.25 | Filed by CHC as Exhibit 10.18 to the Annual Report on Form 10-K for the year ended December 31, 2009 and incorporated herein by reference. | |||||||
| 10.26 | Filed by CHC as Exhibit 10.1 to the Current Report on Form 8-K on June 19, 2017 and incorporated herein by reference. | |||||||
| 10.27 | Filed by CHC as Exhibit 10.2 to the Quarterly Report on Form 10-Q for the period ended March 31, 2012 and incorporated herein by reference. | |||||||
| 10.28 | Filed by CHC as Exhibit 10.1(a) to the Quarterly Report on Form 10-Q for the period ended March 31, 2015 and incorporated herein by reference. | |||||||
| 10.29 | Filed by CHC as Exhibit 10.1(b) to the Quarterly Report on Form 10-Q for the period ended March 31, 2015 and incorporated herein by reference. | |||||||
10.30(a) | Filed by the registrant as Exhibit 10.1 to Amendment No. 1 to the Registration Statement on Form S-4 (No. 333-224960) on June 20, 2018 and incorporated herein by reference. | |||||||
10.30(b) | Filed herewith. | |||||||
10.30(c) | Filed herewith. | |||||||
| 10.31 | Filed by ESRX as Exhibit 10.1 to the Current Report on Form 8-K on May 4, 2016 and incorporated herein by reference. | |||||||
| 10.32 | Filed by CHC as Exhibit 10.20 to the Annual Report on Form 10-K for the year ended December 31, 2008 and incorporated herein by reference. | |||||||
| 10.33 | Filed by the registrant as Exhibit 10.34 to the Annual Report on Form 10-K for the year ended December 31, 2018 and incorporated herein by reference. | |||||||
| 10.34 | Filed by CHC as Exhibit 10.1 to the Current Report on Form 8-K on October 18, 2017 and incorporated herein by reference. | |||||||
| 10.35 | Filed by the registrant as Exhibit 10.35 to the Annual Report on Form 10-K for the year ended December 31, 2020 and incorporated herein by reference. | |||||||
10.36(a) | Filed by the registrant as Exhibit 10.36 to the Annual Report on Form 10-K for the year ended December 31, 2020 and incorporated herein by reference. | |||||||
10.36(b) | Filed herewith. | |||||||
| 10.36(c) | Filed herewith. | |||||||
155
| 10.37 | Filed by the registrant as Exhibit 10.37 to the Annual Report on Form 10-K for the year ended December 31, 2020 and incorporated herein by reference. | |||||||
| 10.38 | Filed by the registrant as Exhibit 10.1 to the Current Report on Form 8-K on April 30, 2021 and incorporated herein by reference. | |||||||
| 10.39 | Filed by CHC as Exhibit 10.29 to the Annual Report on Form 10-K for the year ended December 31, 2012 and incorporated herein by reference. | |||||||
| 21 | Filed herewith. | |||||||
| 23 | Filed herewith. | |||||||
| 31.1 | Filed herewith. | |||||||
| 31.2 | Filed herewith. | |||||||
| 32.1 | Furnished herewith. | |||||||
| 32.2 | Furnished herewith. | |||||||
| 101 | The following materials from Cigna Corporation's Annual Report on Form 10-K for the year ended December 31, 2021, formatted in inline XBRL (Extensible Business Reporting Language): (i) the Consolidated Balance Sheets; (ii) the Consolidated Statements of Income; (iii) the Consolidated Statements of Comprehensive Income; (iv) the Consolidated Statements of Cash Flows; (v) the Consolidated Statements of Changes in Total Equity; (vi) the Notes to Consolidated Financial Statements; and (vii) Financial Statement Schedules I and II. | Filed herewith. | ||||||
| 104 | Cover Page Interactive Data File (formatted as inline XBRL and contained in Exhibit 101) | Filed herewith. | ||||||
The agreements and other documents filed as exhibits to this report are not intended to provide factual information or other disclosure other than the terms of the agreements or other documents themselves and you should not rely on them for that purpose. In particular, any representations and warranties made by the Company in these agreements or other documents were made solely within the specific context of the relevant agreement or document and may not describe the actual state of affairs at the date they were made or at any other time.
Item 16. FORM 10-K SUMMARY
None.
156
SIGNATURES
Pursuant to the requirements of Section 13 or 15(d) of the Securities Exchange Act of 1934, the registrant has duly caused this report to be signed on its behalf by the undersigned, thereunto duly authorized.
Date: February 24, 2022
| CIGNA CORPORATION | |||||||||||
| | |||||||||||
| By: | /s/ Brian C. Evanko | ||||||||||
| Brian C. Evanko | |||||||||||
| Executive Vice President and Chief Financial Officer | |||||||||||
| (Principal Financial Officer) | |||||||||||
Pursuant to the requirements of the Securities Exchange Act of 1934, this report has been signed below by the following persons on behalf of the registrant and in the capacities indicated as of February 24, 2022.
| Signature | Title | |||||||
| /s/ David M. Cordani | ||||||||
| David M. Cordani | Chief Executive Officer and Chairman of the Board | |||||||
| (Principal Executive Officer) | ||||||||
| /s/ Brian C. Evanko | ||||||||
| Brian C. Evanko | Executive Vice President and Chief Financial Officer | |||||||
| (Principal Financial Officer) | ||||||||
| /s/ Mary T. Agoglia Hoeltzel | ||||||||
| Mary T. Agoglia Hoeltzel | Senior Vice President, Tax and Chief Accounting Officer | |||||||
| (Principal Accounting Officer) | ||||||||
| /s/ William J. DeLaney | ||||||||
| William J. DeLaney | Director | |||||||
| /s/ Eric J. Foss | ||||||||
| Eric J. Foss | Director | |||||||
| /s/ Elder Granger, M.D. | ||||||||
| Elder Granger, M.D. | Director | |||||||
| /s/ Neesha Hathi | ||||||||
| Neesha Hathi | Director | |||||||
157
| /s/ George Kurian | ||||||||
| George Kurian | Director | |||||||
| /s/ Kathleen M. Mazzarella | ||||||||
| Kathleen M. Mazzarella | Director | |||||||
| /s/ Mark McClellan, M.D. | ||||||||
| Mark McClellan, M.D. | Director | |||||||
| /s/ John M. Partridge | ||||||||
| John M. Partridge | Director | |||||||
| /s/ Kimberly A. Ross | ||||||||
| Kimberly A. Ross | Director | |||||||
| /s/ Eric C. Wiseman | ||||||||
| Eric C. Wiseman | Lead Independent Director | |||||||
| /s/ Donna F. Zarcone | ||||||||
| Donna F. Zarcone | Director | |||||||
158
CIGNA CORPORATION AND SUBSIDIARIES
INDEX TO FINANCIAL STATEMENT SCHEDULES
| PAGE | |||||||||||
| Report of Independent Registered Public Accounting Firm on Financial Statement Schedules | FS-2 | ||||||||||
| Schedules | |||||||||||
| I | Condensed Financial Information of Cigna Corporation (Registrant) | FS-3 | |||||||||
Statements of Income for the Years Ended December 31, 2021, 2020 and 2019 | FS-3 | ||||||||||
| Balance Sheets as of December 31, 2021 and 2020 | FS-4 | ||||||||||
Statements of Cash Flows for the Years Ended December 31, 2021, 2020 and 2019 | FS-5 | ||||||||||
| Notes to Condensed Financial Statements | FS-6 | ||||||||||
| II | Valuation and Qualifying Accounts for the Years Ended December 31, 2021, 2020 and 2019 | FS-8 | |||||||||
Schedules other than those listed above are omitted because they are not required or are not applicable, or the required information is shown in the financial statements or notes thereto.
FS-1
Report of Independent Registered Public Accounting Firm on
Financial Statement Schedules
To the Board of Directors and Shareholders of Cigna Corporation
Our audits of the consolidated financial statements referred to in our report dated February 24, 2022 appearing in the 2021 Annual Report to Shareholders of Cigna Corporation (which report and consolidated financial statements are included under Item 8 in this Annual Report on Form 10-K) also included an audit of the financial statement schedules listed in Item 15(a)(2) of this Form 10-K. In our opinion, these financial statement schedules present fairly, in all material respects, the information set forth therein when read in conjunction with the related consolidated financial statements.
/s/ PricewaterhouseCoopers LLP
Hartford, Connecticut
February 24, 2022
FS-2
CIGNA CORPORATION AND SUBSIDIARIES
SCHEDULE I
CONDENSED FINANCIAL INFORMATION OF CIGNA CORPORATION
(REGISTRANT)
STATEMENTS OF INCOME
| For the years ended | ||||||||||||||||||||
| December 31, | ||||||||||||||||||||
| (In millions) | 2021 | 2020 | 2019 | |||||||||||||||||
| Revenues | ||||||||||||||||||||
| Net investment income | $ | — | $ | 1 | $ | — | ||||||||||||||
| Intercompany interest income | 471 | 475 | 6 | |||||||||||||||||
| Total revenues | 471 | 476 | 6 | |||||||||||||||||
| Operating expenses | ||||||||||||||||||||
| Selling, general and administrative expenses | 8 | 4 | (85) | |||||||||||||||||
| Total operating expenses | 8 | 4 | (85) | |||||||||||||||||
| Income from operations | 463 | 472 | 91 | |||||||||||||||||
| Interest and other (expense) | (1,197) | (1,324) | (1,032) | |||||||||||||||||
| Intercompany interest (expense) | (13) | (48) | (127) | |||||||||||||||||
| Debt extinguishment costs | (131) | (171) | — | |||||||||||||||||
| Loss before income taxes | (878) | (1,071) | (1,068) | |||||||||||||||||
| Income tax (benefit) | (180) | (234) | (251) | |||||||||||||||||
| Loss of Parent Company | (698) | (837) | (817) | |||||||||||||||||
| Equity in income of subsidiaries | 6,063 | 9,295 | 5,921 | |||||||||||||||||
| Shareholders' net income | 5,365 | 8,458 | 5,104 | |||||||||||||||||
| Shareholders' other comprehensive income (loss), net of tax | ||||||||||||||||||||
| Net unrealized appreciation (depreciation) on securities and derivatives | (215) | (75) | 957 | |||||||||||||||||
| Net translation (losses) gains of foreign currencies | (218) | 260 | (54) | |||||||||||||||||
| Postretirement benefits liability adjustment | 410 | (105) | (133) | |||||||||||||||||
| Shareholders' other comprehensive income (loss), net of tax | (23) | 80 | 770 | |||||||||||||||||
| Shareholders' comprehensive income | $ | 5,342 | $ | 8,538 | $ | 5,874 | ||||||||||||||
See Notes to Financial Statements on the following pages.
FS-3
CIGNA CORPORATION AND SUBSIDIARIES
SCHEDULE I
CONDENSED FINANCIAL INFORMATION OF CIGNA CORPORATION
(REGISTRANT)
BALANCE SHEETS
| As of December 31, | ||||||||||||||
| (In millions) | 2021 | 2020 | ||||||||||||
| Assets | ||||||||||||||
| Cash and cash equivalents | $ | 33 | $ | 4,157 | ||||||||||
| Short-term investments | 99 | 49 | ||||||||||||
| Other current assets | 9 | 4 | ||||||||||||
| Total current assets | 141 | 4,210 | ||||||||||||
| Intercompany receivable | 8,962 | 1,666 | ||||||||||||
| Investments in subsidiaries | 70,896 | 76,040 | ||||||||||||
| Other noncurrent assets | 17 | 22 | ||||||||||||
| TOTAL ASSETS | $ | 80,016 | $ | 81,938 | ||||||||||
| Liabilities | ||||||||||||||
| Short-term debt | $ | 2,453 | $ | 3,278 | ||||||||||
| Other current liabilities | 775 | 616 | ||||||||||||
| Total current liabilities | 3,228 | 3,894 | ||||||||||||
| Intercompany payable | 5 | 5 | ||||||||||||
| Long-term debt | 29,671 | 27,718 | ||||||||||||
| TOTAL LIABILITIES | 32,904 | 31,617 | ||||||||||||
| Shareholders' Equity | ||||||||||||||
Common stock (shares issued, 394 and 390; authorized, 600) | 4 | 4 | ||||||||||||
| Additional paid-in capital | 29,574 | 28,975 | ||||||||||||
| Accumulated other comprehensive loss | (884) | (861) | ||||||||||||
| Retained earnings | 32,593 | 28,575 | ||||||||||||
| Less treasury stock, at cost | (14,175) | (6,372) | ||||||||||||
| TOTAL SHAREHOLDERS' EQUITY | 47,112 | 50,321 | ||||||||||||
| TOTAL LIABILITIES AND SHAREHOLDERS' EQUITY | $ | 80,016 | $ | 81,938 | ||||||||||
See Notes to Financial Statements on the following pages.
FS-4
CIGNA CORPORATION AND SUBSIDIARIES
SCHEDULE I
CONDENSED FINANCIAL INFORMATION OF CIGNA CORPORATION
(REGISTRANT)
STATEMENTS OF CASH FLOWS
| For the years ended | ||||||||||||||||||||
| December 31, | ||||||||||||||||||||
| (In millions) | 2021 | 2020 | 2019 | |||||||||||||||||
| Cash Flows from Operating Activities | ||||||||||||||||||||
| Shareholders' net income | $ | 5,365 | $ | 8,458 | $ | 5,104 | ||||||||||||||
| Adjustments to reconcile shareholders' net income | ||||||||||||||||||||
| to net cash provided by operating activities | ||||||||||||||||||||
| Equity in income of subsidiaries | (6,063) | (9,295) | (5,921) | |||||||||||||||||
| Debt extinguishment costs | 131 | 171 | — | |||||||||||||||||
| Dividends received from subsidiaries | 2,751 | 8,627 | 2,457 | |||||||||||||||||
| Other liabilities | 184 | 112 | 43 | |||||||||||||||||
| Other, net | 414 | 500 | 20 | |||||||||||||||||
| NET CASH PROVIDED BY OPERATING ACTIVITIES | 2,782 | 8,573 | 1,703 | |||||||||||||||||
| Cash Flows from Investing Activities | ||||||||||||||||||||
| Net change in loans due to (from) affiliates | (1,007) | (265) | — | |||||||||||||||||
| Short-term investment purchased, net | (50) | (19) | (30) | |||||||||||||||||
| NET CASH (USED IN) INVESTING ACTIVITIES | (1,057) | (284) | (30) | |||||||||||||||||
| Cash Flows from Financing Activities | ||||||||||||||||||||
| Net change in amounts due to affiliates | 2,062 | 2,262 | 2,015 | |||||||||||||||||
| Proceeds on issuance of commercial paper | 997 | 86 | 944 | |||||||||||||||||
| Payments for debt extinguishment | (126) | (181) | — | |||||||||||||||||
| Repayment of long-term debt | (4,199) | (5,996) | (3,002) | |||||||||||||||||
| Net proceeds on issuance of long-term debt | 4,260 | 3,465 | — | |||||||||||||||||
| Issuance of common stock | 326 | 376 | 224 | |||||||||||||||||
| Common dividends paid | (1,341) | (15) | (15) | |||||||||||||||||
| Repurchase of common stock | (7,742) | (4,042) | (1,987) | |||||||||||||||||
| Tax withholding on stock compensation and other | (86) | (87) | (82) | |||||||||||||||||
| Other | — | — | (13) | |||||||||||||||||
| NET CASH (USED IN) FINANCING ACTIVITIES | (5,849) | (4,132) | (1,916) | |||||||||||||||||
| Net (decrease) increase in cash and cash equivalents | (4,124) | 4,157 | (243) | |||||||||||||||||
| Cash and cash equivalents, beginning of year | 4,157 | — | 243 | |||||||||||||||||
| Cash and cash equivalents, end of year | $ | 33 | $ | 4,157 | $ | — | ||||||||||||||
See Notes to Financial Statements on the following pages.
FS-5
CIGNA CORPORATION AND SUBSIDIARIES
SCHEDULE I
CONDENSED FINANCIAL INFORMATION OF CIGNA CORPORATION
(REGISTRANT)
NOTES TO CONDENSED FINANCIAL STATEMENTS
The accompanying condensed financial statements should be read in conjunction with the Consolidated Financial Statements and the accompanying notes thereto contained in this Annual Report on Form 10-K ("Form 10-K").
Note 1 — For purposes of these condensed financial statements, Cigna Corporation's (the "Company") wholly-owned and majority-owned subsidiaries are recorded using the equity method of accounting.
Note 2 — See Note 7 – Debt included in Part II, Item 8 of this Form 10-K for a description of the short-term and long-term debt obligations of Cigna Corporation and its subsidiaries.
Debt Issuance and Redemption. In order to decrease future interest expense and reduce future refinancing risk, the Company entered into the following transactions during 2021:
•Debt issuance: On March 3, 2021, the Company issued $4.3 billion of new senior notes. The proceeds of this issuance were mainly used to redeem outstanding debt securities. The remaining proceeds are available for general corporate purposes. Interest on this debt is paid semi-annually.
| Principal | Maturity Date | Interest Rate | Net Proceeds | |||||||||||||||||
$500 million (1) | March 15, 2024 | 0.613% | $499 million | |||||||||||||||||
$800 million (2) | March 15, 2026 | 1.250% | $797 million | |||||||||||||||||
$1,500 million (3) | March 15, 2031 | 2.375% | $1,492 million | |||||||||||||||||
$1,500 million (4) | March 15, 2051 | 3.400% | $1,479 million | |||||||||||||||||
(1) Redeemable at any time discounted at the U.S. Treasury rate plus 7.5 basis points. Redeemable at par on or after March 15, 2022.
(2) Redeemable at any time discounted at the U.S. Treasury rate plus 10 basis points. Redeemable at par on or after February 15, 2026.
(3) Redeemable at any time discounted at the U.S. Treasury rate plus 15 basis points. Redeemable at par on or after December 15, 2030.
(4) Redeemable at any time discounted at the U.S. Treasury rate plus 20 basis points. Redeemable at par on or after September 15, 2050.
•Debt redemption: During 2021, the Company completed the redemption of a total of $4.2 billion in aggregate principal amount of certain of its outstanding debt securities. The Company recorded a pre-tax loss of $131 million ($101 million after-tax), consisting primarily of premium payments.
Revolving Credit Agreements. Our revolving credit agreements provide us with the ability to borrow amounts for general corporate purposes, including for the purpose of providing liquidity support if necessary under our commercial paper program discussed below. As of December 31, 2021, there were no outstanding balances under these revolving credit agreements.
In April 2021, Cigna entered into a $3.0 billion five-year revolving credit and letter of credit agreement that matures in April 2026 and a $1.0 billion three-year revolving credit agreement that matures in April 2024, which are diversified among 23 banks and replaced the five-year revolving credit and letter of credit agreement that was scheduled to mature in April 2023. Under the current agreements, Cigna can borrow up to $3.0 billion and $1.0 billion, respectively, for general corporate purposes, with up to $500 million available under the five-year facility for issuance of letters of credit. The revolving credit agreements also include an option to extend the termination date for an additional r period, subject to consent of the banks.
Additionally, in April 2021, Cigna entered into a $1.0 billion 364-day revolving credit agreement that will mature in April 2022 and is diversified among 23 banks. This agreement replaced the prior $1.0 billion 364-day revolving credit agreement that was scheduled to expire in October 2021. Pursuant to this revolving credit agreement, Cigna can borrow up to $1.0 billion for general corporate purposes. The agreement includes the option to "term out" any revolving loans that are outstanding at maturity by converting them into a term loan maturing on the one-year anniversary of conversion.
Each of the five-year facility, the three-year facility and the 364-day facility include an option to increase commitments in an aggregate amount of up to $1.5 billion across all three facilities. Each of the three facilities also contain customary covenants and restrictions including a financial covenant that the Company's leverage ratio, as defined in the credit agreements, may not exceed 60%, subject to certain exceptions upon the consummation of an acquisition.
FS-6
Commercial Paper. Under our commercial paper program we may issue short-term, unsecured commercial paper notes privately placed on a discounted basis through certain broker dealers at any time not to exceed an aggregate amount of $5.0 billion. Amounts available under the program may be borrowed, repaid and re-borrowed from time to time. The net proceeds of issuances have been and are expected to be used for general corporate purposes. The commercial paper average interest rate was 0.26% at December 31, 2021.
The Company was in compliance with its debt covenants as of December 31, 2021.
Maturity of the Company's long-term debt is as follows:
| (In millions) | ||||||||
| 2022 | $ | 430 | ||||||
| 2023 | $ | 2,754 | ||||||
| 2024 | $ | 1,214 | ||||||
| 2025 | $ | 2,957 | ||||||
| 2026 | $ | 2,034 | ||||||
| Maturities after 2026 | $ | 20,947 | ||||||
Note 3 — Intercompany receivables of the Company consist primarily of net amounts due from Express Scripts Holdings of $7.8 billion as of December 31, 2021 and $1.4 billion (consisting of an $8.2 billion receivable offset by a $6.8 billion payable) as of December 31, 2020. Interest income on the receivable was accrued at an annual fixed rate of 5.50%. Interest expense on the payable was accrued at an average rate of 0.20% in 2021.
Note 4 — The Company had guarantees of approximately $86 million as of December 31, 2021. These guarantees are primarily related to outstanding letters of credit. In 2021, no payments have been made on these guarantees.
FS-7
CIGNA CORPORATION AND SUBSIDIARIES
SCHEDULE II
VALUATION AND QUALIFYING ACCOUNTS AND RESERVES
| (In millions) | Balance at beginning of year | Charged (Credited) to costs and expenses | Charged (Credited) to other accounts | Other deductions | Balance at end of year | |||||||||||||||||||||||||||
| Description | ||||||||||||||||||||||||||||||||
| 2021 | ||||||||||||||||||||||||||||||||
| Investment asset valuation reserves | ||||||||||||||||||||||||||||||||
| Available-for-sale debt securities | $ | 26 | $ | 29 | $ | — | $ | (32) | $ | 23 | ||||||||||||||||||||||
| Commercial mortgage loans | $ | 6 | $ | — | $ | — | $ | — | $ | 6 | ||||||||||||||||||||||
| Accounts receivable, net | $ | 156 | $ | 54 | $ | — | $ | (84) | $ | 126 | ||||||||||||||||||||||
| Deferred tax asset valuation allowance | $ | 207 | $ | 23 | $ | 16 | $ | — | $ | 246 | ||||||||||||||||||||||
| Reinsurance recoverables | $ | 32 | $ | (2) | $ | — | $ | — | $ | 30 | ||||||||||||||||||||||
| 2020 | ||||||||||||||||||||||||||||||||
| Investment asset valuation reserves | ||||||||||||||||||||||||||||||||
| Available-for-sale debt securities | $ | — | $ | 82 | $ | — | $ | (56) | $ | 26 | ||||||||||||||||||||||
Commercial mortgage loans (1) | $ | — | $ | (1) | $ | 7 | $ | — | $ | 6 | ||||||||||||||||||||||
| Accounts receivable, net | $ | 252 | $ | (50) | $ | (12) | $ | (34) | $ | 156 | ||||||||||||||||||||||
| Deferred tax asset valuation allowance | $ | 196 | $ | 10 | $ | 1 | $ | — | $ | 207 | ||||||||||||||||||||||
Reinsurance recoverables (2) | $ | 2 | $ | (1) | $ | 31 | $ | — | $ | 32 | ||||||||||||||||||||||
| 2019 | ||||||||||||||||||||||||||||||||
| Accounts receivable, net | $ | 217 | $ | 51 | $ | — | $ | (16) | $ | 252 | ||||||||||||||||||||||
| Deferred tax asset valuation allowance | $ | 199 | $ | (6) | $ | 3 | $ | — | $ | 196 | ||||||||||||||||||||||
| Reinsurance recoverables | $ | 2 | $ | — | $ | — | $ | — | $ | 2 | ||||||||||||||||||||||
(1) The Company recorded an additional allowance of $7 million on January 1, 2020 upon the adoption of ASU 2016-13.
(2) The Company recorded an additional allowance of $31 million on January 1, 2020 upon the adoption of ASU 2016-13.
FS-8
Similar companies
See also UNITEDHEALTH GROUP INC - Annual report 2022 (10-K 2022-12-31) Annual report 2023 (10-Q 2023-09-30)See also HUMANA INC - Annual report 2022 (10-K 2022-12-31) Annual report 2023 (10-Q 2023-09-30)
See also CENTENE CORP - Annual report 2022 (10-K 2022-12-31) Annual report 2023 (10-Q 2023-09-30)
See also MOLINA HEALTHCARE, INC. - Annual report 2022 (10-K 2022-12-31) Annual report 2023 (10-Q 2023-09-30)
See also Alignment Healthcare, Inc. - Annual report 2022 (10-K 2022-12-31) Annual report 2023 (10-Q 2023-09-30)
