Alignment Healthcare, Inc. - Annual Report: 2021 (Form 10-K)
UNITED STATES
SECURITIES AND EXCHANGE COMMISSION
Washington, D.C. 20549
FORM 10-K
(Mark One)
☒ |
ANNUAL REPORT PURSUANT TO SECTION 13 OR 15(d) OF THE SECURITIES EXCHANGE ACT OF 1934 |
For the fiscal year ended December 31, 2021
OR
☐ |
TRANSITION REPORT PURSUANT TO SECTION 13 OR 15(d) OF THE SECURITIES EXCHANGE ACT OF 1934 FOR THE TRANSITION PERIOD FROM TO |
Commission File Number: 001-40295
ALIGNMENT HEALTHCARE, INC.
(Exact name of Registrant as specified in its Charter)
Delaware |
46-5596242 |
(State or other jurisdiction of incorporation or organization) |
(I.R.S. Employer Identification No.) |
1100 W. Town and Country Road, Suite 1600 Orange, California |
92868 |
(Address of principal executive offices) |
(Zip Code) |
Registrant’s telephone number, including area code: (844) 310-2247
Securities registered pursuant to Section 12(b) of the Act:
Title of each class |
|
Trading Symbol(s) |
|
Name of each exchange on which registered |
Common Stock, par value $0.001 per share |
|
ALHC |
|
The Nasdaq Stock Market LLC |
Securities registered pursuant to Section 12(g) of the Act: None
Indicate by check mark if the Registrant is a well-known seasoned issuer, as defined in Rule 405 of the Securities Act. Yes ☐ No ☒
Indicate by check mark if the Registrant is not required to file reports pursuant to Section 13 or 15(d) of the Act. Yes ☒ NO ☐
Indicate by check mark whether the Registrant: (1) has filed all reports required to be filed by Section 13 or 15(d) of the Securities Exchange Act of 1934 during the preceding 12 months (or for such shorter period that the Registrant was required to file such reports), and (2) has been subject to such filing requirements for the past 90 days. Yes ☒ NO ☐
Indicate by check mark whether the Registrant has submitted electronically every Interactive Data File required to be submitted pursuant to Rule 405 of Regulation S-T (§232.405 of this chapter) during the preceding 12 months (or for such shorter period that the Registrant was required to submit such files). Yes ☒ NO ☐
Indicate by check mark whether the registrant is a large accelerated filer, an accelerated filer, a non-accelerated filer, smaller reporting company, or an emerging growth company. See the definitions of “large accelerated filer,” “accelerated filer,” “smaller reporting company,” and “emerging growth company” in Rule 12b-2 of the Exchange Act.
Large accelerated filer |
|
☐ |
|
Accelerated filer |
|
☐ |
|
|
|
|
|||
Non-accelerated filer |
|
☒ |
|
Smaller reporting company |
|
☐ |
|
|
|
|
|
|
|
Emerging growth company |
|
☐ |
|
|
|
|
If an emerging growth company, indicate by check mark if the registrant has elected not to use the extended transition period for complying with any new or revised financial accounting standards provided pursuant to Section 13(a) of the Exchange Act. ☐
Indicate by check mark whether the registrant has filed a report on and attestation to its management’s assessment of the effectiveness of its internal control over financial reporting under Section 404(b) of the Sarbanes-Oxley Act (15 U.S.C. 7262(b)) by the registered public accounting firm that prepared or issued its audit report. ☐
Indicate by check mark whether the Registrant is a shell company (as defined in Rule 12b-2 of the Exchange Act). YES ☐ NO ☒
The aggregate market value of voting shares held by non-affiliates of the Registrant was $1,320,990,372 as of June 30, 2021, the last business day of the Registrant’s most recently completed second fiscal quarter (based on a closing price of $23.37 per share). Shares of common stock held by each executive officer, director, and holder of 5% or more of the outstanding common stock have been excluded in that such persons may be deemed to be affiliates. This determination of affiliate status is not necessarily a conclusive determination for other purposes.
As of February 28, 2022, the registrant had 187,067,046 shares of common stock, $0.001 par value per share, outstanding.
DOCUMENTS INCORPORATED BY REFERENCE
The information required by Part III of this Annual Report, to the extent not set forth herein, is incorporated herein by reference from the registrant’s definitive proxy statement relating to the Annual Meeting of Shareholders to be held in 2022, which definitive proxy statement shall be filed with the Securities and Exchange Commission within 120 days after the end of the fiscal year to which this Annual Report relates.
Table of Contents
|
|
Page |
PART I |
|
|
Item 1. |
4 |
|
Item 1A. |
27 |
|
Item 1B. |
64 |
|
Item 2. |
64 |
|
Item 3. |
64 |
|
Item 4. |
64 |
|
|
|
|
PART II |
|
|
Item 5. |
65 |
|
Item 6. |
66 |
|
Item 7. |
Management’s Discussion and Analysis of Financial Condition and Results of Operations |
67 |
Item 7A. |
81 |
|
Item 8. |
82 |
|
Item 9. |
Changes in and Disagreements With Accountants on Accounting and Financial Disclosure |
110 |
Item 9A. |
110 |
|
Item 9B. |
111 |
|
Item 9C. |
Disclosure Regarding Foreign Jurisdictions that Prevent Inspections |
111 |
|
|
|
PART III |
|
|
Item 10. |
112 |
|
Item 11. |
112 |
|
Item 12. |
Security Ownership of Certain Beneficial Owners and Management and Related Stockholder Matters |
112 |
Item 13. |
Certain Relationships and Related Transactions, and Director Independence |
112 |
Item 14. |
112 |
|
|
|
|
PART IV |
|
|
Item 15. |
113 |
|
Item 16. |
115 |
|
|
116 |
i
FORWARD-LOOKING STATEMENTS
Throughout this annual report on Form 10-K (this “Annual Report”), we make “forward-looking statements” within the meaning of the U.S. Private Securities Litigation Reform Act of 1995. All statements other than statements of historical fact included in this Annual Report are forward-looking statements. Forward-looking statements give our current expectations relating to our financial condition, results of operations, plans, objectives, future performance and business. You can identify forward-looking statements by the fact that they do not relate strictly to historical or current facts. These statements may include words such as “anticipate,” “estimate,” “expect,” “project,” “plan,” “intend,” “believe,” “may,” “will,” “should,” “can have,” “likely” and other words and terms of similar meaning. The forward-looking statements contained in this Annual Report are generally located in the material set forth under the heading “Management’s Discussion and Analysis of Financial Condition and Results of Operations” but may be found in other locations as well. These statements are based upon management’s current expectations, assumptions and estimates and are not guarantees of timing, future results or performance. All forward-looking statements are subject to risks and uncertainties that may cause actual results to differ materially from those that we expected, including:
1
We derive many of our forward-looking statements from our operating budgets and forecasts, which are based on many detailed assumptions. While we believe that our assumptions are reasonable, we caution that it is very difficult to predict the impact of known factors, and it is impossible for us to anticipate all factors that could affect our actual results. Important factors that could cause actual results to differ materially from our expectations, or cautionary statements, are disclosed under the sections entitled “Risk Factors” and “Management’s Discussion and Analysis of Financial Condition and Results of Operations” in this Annual Report.
All written and oral forward-looking statements attributable to us, or persons acting on our behalf, are expressly qualified in their entirety by these cautionary statements as well as other cautionary statements that are made from time to time in our other SEC filings and public communications. You should evaluate all forward-looking statements made in this Annual Report in the context of these risks and uncertainties.
We caution you that the important factors referenced above may not contain all of the factors that are important to you. In addition, we cannot assure you that we will realize the results or developments we expect or anticipate or, even if substantially realized, that they will result in the consequences or affect us or our operations in the way we expect. The forward-looking statements included in this Annual Report are made only as of the date hereof. We undertake no obligation to update or revise any forward-looking statement as a result of new information, future events or otherwise, except as otherwise required by law.
MARKET AND INDUSTRY DATA
Unless otherwise indicated, information in this Annual Report concerning economic conditions, our industry, our markets and our competitive position is based on a variety of sources, including information from independent industry analysts and publications, as well as our own estimates and research. This information involves a number of assumptions and limitations, and you are cautioned not to give undue weight to such estimates. While we believe the information presented in this Annual Report is generally reliable, forecasts, assumptions, expectations, beliefs, estimates and projects involve risk and uncertainties and are subject to change based on various factors, including those described under “Forward-Looking Statements” and “Risk Factors.”
Throughout this Annual Report, all references to “Net Promoter Score” or “NPS” are to a measure of satisfaction widely used in the healthcare industry. We calculate NPS based on responses to member surveys, conducted by a third-party administrator (either telephonically or online) that selects a random sample of members to participate. The surveys ask the consumer to rank, on a scale of one to 10, how likely the member would be to recommend Alignment to a friend or relative. We assign the designation of “Promoter” to respondents who provide a score of 9 or 10, the designation of “Neutral” to respondents who provide a score of 7 or 8, and the designation of “Detractor” to respondents who provide a score of 0 to 6. We then subtract the percentage of Detractors from Promoters to determine our overall Net Promoter Score. We believe that this method of calculation aligns with industry standards and that this metric is meaningful for investors because of the correlation between Net Promoter Score and consumer satisfaction.
2
Throughout this Annual Report, all references to the “Five-Star Rating System” or “Star rating” are to a measure used by the CMS to rate the performance of Medicare Advantage and Part D plans. Medicare Advantage Plans are rated on how well they perform in five different categories: (1) staying healthy: screenings, tests, and vaccines, (2) managing chronic (long-term) conditions, (3) plan responsiveness and care, (4) member complaints, problems getting services, and choosing to leave the plan, and (5) health plan customer service. Part D plans are rated on how well they perform in four different categories: (1) drug plan customer service, (2) member complaints, problems getting services, and choosing to leave the plan, (3) member experience with the drug plan, and (4) drug pricing and member safety. Ratings range from one to five stars, with five being the highest and one being the lowest. Plans are rated in each individual category. Medicare also assigns Medicare Advantage plans one overall star rating to summarize the plan’s performance as a whole.
BASIS OF PRESENTATION
We historically operated as a Delaware limited liability company under the name Alignment Healthcare Holdings, LLC. On March 17, 2021, Alignment Healthcare Holdings, LLC converted into a Delaware corporation pursuant to a statutory conversion and changed its name to Alignment Healthcare, Inc. As a result of this conversion, Alignment Healthcare Partners, LP, a Delaware limited partnership (“Alignment Partners”) and the sole unitholder of Alignment Healthcare Holdings, LLC, became the sole holder of shares of common stock of Alignment Healthcare, Inc. (the “Corporate Conversion”).
Prior to the closing of our initial public offering (“IPO”), (i) Alignment Healthcare, Inc. effected an approximately 1 for 260 split of its common stock (the “Stock Split”) and (ii) Alignment Partners merged with and into Alignment Healthcare, Inc., with Alignment Healthcare, Inc. surviving the merger (the “Company Merger”). Pursuant to the Company Merger, the partners of Alignment Partners received all of the then-outstanding shares of common stock of Alignment Healthcare, Inc. in exchange for their units in Alignment Partners. The Stock Split and Company Merger are collectively referred to herein as the “Corporate Reorganization.” Except as disclosed in this Annual Report, the consolidated financial statements and selected historical consolidated financial data and other financial information included in this Annual Report are those of Alignment Healthcare, Inc. and its subsidiaries and give effect to the Corporate Conversion and the Corporate Reorganization.
Unless the context otherwise requires, the terms “Alignment,” the “Company,” “our company,” “we,” “us” and “our” in this annual report refer to Alignment Healthcare Holdings, LLC, its consolidated subsidiaries and its affiliated medical groups, for all periods prior to the Corporate Conversion and to Alignment Healthcare, Inc., its consolidated subsidiaries and its affiliated medical groups, for all periods following the Corporate Conversion.
We are a holding company and our sole asset is the capital stock of our wholly owned subsidiaries, including Alignment Healthcare USA, LLC. Alignment Healthcare Holdings, LLC is the predecessor of the issuer for financial reporting purposes.
3
PART I
Item 1. Business.
Our Mission
Alignment Healthcare was founded in 2013 with one mission in mind: improving healthcare one senior at a time. We pursue this mission by relentlessly focusing on our core values:
We created Alignment based on the frustrating experiences we had when our parents and other loved ones needed healthcare. We saw firsthand the complexity they faced as seniors attempting to navigate care delivery and insurance without an advocate to create an integrated consumer experience that provides holistic and quality care at an affordable price. Our parents and seniors across the country are systemically and disproportionately impacted by the absence of care coordination, poor information transparency and misaligned incentives that characterize the healthcare system.
Our team of highly experienced healthcare leaders created the Alignment model to incorporate the lessons our management team has learned over decades collectively spent serving senior consumers. We believe that by combining our experienced, mission-driven team with purpose-built technology we have found a way to address the unmet needs of senior consumers and to “do well by doing good.” Our ultimate goal is to bring this differentiated, advocacy-driven healthcare experience to millions of senior consumers in the United States and to become the most trusted senior healthcare brand in the country.
How We are Revolutionizing Healthcare for Seniors
Alignment is a next generation, consumer-centric platform designed to revolutionize the healthcare experience for seniors. We deliver this experience through our Medicare Advantage plans, which are customized to meet the needs of a diverse array of seniors. Our platform was developed to align with the six core principles that we believe will be required to successfully deliver healthcare in the 21st century and that represent our key competitive strengths. Our platform enables us to:
Leverage Data, Technology and Analytics to Power All Aspects of Our Model
Healthcare organizations have long struggled to fully harness the utilization of data and technology to enhance business operations, improve clinical outcomes and drive consumer satisfaction. The industry produces an extraordinary amount of digitized data that is often unusable and siloed within organizations. This has created an opportunity for integrated end-to-end data management to be a significant competitive advantage.
Our proprietary technology platform, Alignment's Virtual Application ("AVA"), was designed specifically for senior care and provides end-to-end coordination of the healthcare ecosystem. AVA’s full suite of tools and services is built within a unified data architecture. Our technology capabilities and position in the healthcare ecosystem enables us to ingest and transform broad, longitudinal datasets into insights, analytics and custom-built applications designed to ensure consistent, high-quality care and service for Alignment’s members. We believe that AVA generates more timely, accurate and actionable insights than existing solutions, driving targeted member interventions and enabling internal care team workflows that result in superior clinical outcomes and consumer experiences.
4
The AVA platform is purpose-built to be used in all aspects of providing superior healthcare for Alignment’s senior members. AVA supports our own internally employed care teams, operations teams, marketing teams and concierge personnel, as well as local community-based healthcare providers and brokers. In addition, AVA’s scalability enables us to reliably produce replicable outcomes and experiences for our members as we scale in existing markets and expand to new ones.
Engage Consumers Directly and Develop Products to Address Their Needs
Traditional healthcare coverage and care delivery is complex and fails to consistently engage and satisfy consumers. Today, consumers have more purchasing power and exercise more control over their own healthcare decision-making than ever before. Medicare Advantage is marketed and sold direct-to-consumer, allowing seniors to select the manner in which they receive healthcare coverage and services on an annual basis.
At Alignment, we have designed our platform to be consumer-centric, to listen to and understand our members’ needs, and to delight our senior consumers. We believe that our primary role is to act as a trusted advocate on behalf of seniors and to design and offer healthcare plans that meet their unique healthcare and lifestyle needs. Our approach delivers outstanding service to our members and results in high-quality, convenient and accessible care that is affordable and represents superior value compared to existing solutions.
We recognize that seniors’ needs extend beyond traditional healthcare, which is why we provide additional services such as transportation, pet care, grocery benefits, companion care, fitness memberships, a 24/7 concierge and a clinical service hotline. Our member satisfaction is evidenced by our overall NPS score of greater than 60 which, based on data collected and made publicly available by Customer Guru, is significantly higher than the industry average NPS ranging from 30-40 and is comparable to celebrated consumer brands. See “Market and Industry Data” above for additional information regarding the calculation of NPS.
Proactively Manage and Coordinate Care for our Most Vulnerable Members
Seniors with complex, chronic conditions represent a small portion of the population, but account for a disproportionate amount of total healthcare spending. The complexity of the U.S. healthcare system results in uncoordinated care for this category of seniors, leading to poor outcomes, unnecessary spend and an unsatisfactory consumer experience.
Alignment identifies high-risk, chronically ill individuals and designs personalized care plans for those members. Our AVA platform stratifies our members based on their health status and social needs, allowing us to identify our most vulnerable members and deploy our Care Anywhere team to deliver timely, effective and coordinated care at the senior’s home, in a healthcare facility, or through a virtual channel. Our Care Anywhere program utilizes our own dedicated clinical teams to provide a combination of high-tech and high-touch care. These cross-disciplinary care teams, which include physicians, advanced practice clinicians, case managers, social workers and behavioral health coaches, work together to establish customized care plans and engage our high-risk seniors with ongoing care interventions that address their health and social needs.
Our high-risk, chronic, and complex care management capabilities, supported by the AVA platform, allow us to effectively manage risk, provide better clinical outcomes and improve our seniors’ experience.
Empower Providers and Employ Flexible Care Delivery Models
Despite being well-situated to influence outcomes for the seniors that they treat, providers often do not have the information and support required to optimize their patients’ outcomes. Many organizations have struggled to build a cohesive and flexible platform that can support and empower providers to delight senior consumers.
We engage with physicians and healthcare provider organizations by tailoring our care delivery tools, product designs and contract types to local market needs in a way that accommodates providers’ preferences and risk tolerance. Our provider engagement and training processes help generate consistent clinical outcomes across various markets with a diverse array of providers and varying degrees of value-based care sophistication. We currently have successful partnerships across a range of provider types, from health system-employed physicians to independent, community-based providers. We provide our partners with care performance metrics and actionable insights that enable them to continuously enhance quality of care, access relevant data to drive informed decision-making and improve the experience of members. This customized level of provider engagement, curated based on their particular needs and circumstances, helps them deliver the best possible clinical care.
Our flexible approach to local market care delivery enables us to attract key provider relationships in various markets and to scale more rapidly and with greater capital efficiency than we could if we were to rely entirely on our own clinical staff.
Design and Deploy Innovative Value–Based Payment Models
5
The legacy healthcare system relies on payment models that compensate healthcare providers based on the volume of services delivered rather than the quality of the care they provide. Despite the increasing focus of CMS on tying payments to health outcomes, we have yet to see widespread improvement in outcomes relative to overall healthcare spending.
Our company name, Alignment Healthcare, reflects one of our founding principles: to align all stakeholders in the healthcare ecosystem around doing what is best for the senior consumer. Our business model is value- based and our ultimate profitability is aligned with the healthcare outcomes of our seniors. We also enter into downstream contracts that are tailored to each providers’ capabilities and local market structure. These contracts employ various value-based payment models, such as shared risk or gainshare arrangements, which are designed to ensure that our provider partners are incentivized to improve the health outcomes of our seniors. In order to successfully manage the financial risk of delivering healthcare for our seniors, we utilize advanced tools, enable access to unified data, and maintain broad coverage and management over an ecosystem of healthcare professionals who are aligned to provide the best possible care.
Cultivate a Culture of Innovation
Traditional healthcare companies are burdened by their scale, administrative complexity and reliance on legacy technology solutions, resulting in their inability to adapt quickly and provide integrated services tailored to the dynamic needs of evolving healthcare consumers.
Given Alignment’s entrepreneurial heritage, a focus on continuous improvement and innovation is at the heart of our culture and DNA. We constantly solicit feedback from our members and seek opportunities to provide new solutions to meet their healthcare and lifestyle needs. We further believe our focus on innovation is a critical competitive advantage that enables our superior member experience, cost and health outcomes. Examples of our continued innovation include:
Built upon these six core principles, we believe Alignment is revolutionizing healthcare for seniors.
Industry Overview
The U.S. healthcare system has grown too complex and costly to meet the evolving needs of senior consumers who are increasingly exercising control over how they manage their overall health and wellness.
We are exclusively focused on serving the senior population, a significant and rapidly growing segment within the United States. As used in this annual report, “seniors” refer to Medicare-eligible persons, which are primarily people over the age of 65. Seniors are living longer than previous generations, with approximately 10,000 adults becoming eligible for Medicare each day, according to the U.S. Census Bureau. The population of U.S. seniors is expected to grow to 73.1 million by 2030, up from 56.1 million in 2020, and to increase as a percentage of the population from 17% to 21% over the same period. As our targeted population grows, so do their needs and demands.
Rising healthcare costs, particularly among the growing senior population, are uncoupled from outcomes
6
The growing senior population is putting additional pressure on an already strained healthcare system. According to the Kaiser Family Foundation, from 2010 to 2018, net Medicare spending increased from approximately $450 billion to more than $600 billion at an annual growth rate of 4%. The Congressional Budget Office projects net Medicare spending to be $683 billion in 2021 and expects that figure to exceed $1.3 trillion by 2030, representing an 8% compound annual growth rate. Despite increasing healthcare spending, U.S. seniors have poor health outcomes relative to other developed nations, exemplified through lower life expectancy, higher levels of hospital utilization and greater prevalence of chronic conditions. A significant portion of our nation’s unsustainably high healthcare costs are a direct result of the underserved senior population, especially high-risk and high-acuity seniors.
The fragmented U.S. healthcare system is complex and burdensome for seniors, particularly those with chronic, complex conditions driving a significant amount of the total spend
Navigating the U.S. healthcare system is particularly complex and burdensome for seniors, who often have more significant care needs and complex medical conditions. Seniors today experience a healthcare landscape that is fragmented across disparate point solutions and uncoordinated healthcare providers. According to the National Council on Aging, approximately 80% of the U.S. senior population suffers from at least one chronic illness, while nearly 70% of the senior population has been diagnosed with at least two chronic illnesses. Anyone who has cared for a senior understands the tremendous challenge this can represent. This dynamic results in a small percentage of the population representing a disproportionately high level of healthcare expenditures. According to a study by the American Hospital Association, the 36% percent of the Medicare population with four or more chronic conditions represents 75% of total Medicare spending. Many of these individuals have complex co-morbidities and would benefit from highly coordinated clinical care along with integrated social, psychological, pharmaceutical and functional support. Existing care models have failed to provide the level of coordination that these seniors need and deserve.
Traditional Medicare has struggled to incentivize high-quality, low-cost care, but Medicare Advantage is designed to employ value-based care to achieve better outcomes
Under the Medicare system, seniors have two primary choices for health insurance once they reach the age of 65. They can enroll in (i) traditional Medicare fee-for-service ("FFS") administered by CMS, or (ii) a Medicare Advantage plan administered by a managed care company. Traditional Medicare FFS offers members few network restrictions, but often leaves them exposed to catastrophic events with substantial out-of-pocket costs for care and drug coverage, and does not provide supplemental benefits. The Medicare Advantage system offers a greater value proposition to the senior in that it often provides enhanced pharmaceutical coverage, greater certainty of expected annual costs, out of pocket limits, holistic supplemental benefits and better catastrophic coverage relative to traditional Medicare.
The legacy healthcare delivery system of Medicare FFS results in reactive and often times costly care for acute events. By linking payments to the number of encounters and pricing to the complexity of the intervention, the fee-for-service model does not reward prevention, but rather incentivizes the treatment of acute care episodes with more costly and complex treatments. The Medicare Advantage system, on the other hand, has a value-based care economic construct whereby CMS shifts the responsibility for the outcomes, medical cost control and the administration of benefits to private health plans. Funding to Medicare Advantage plans is capped based on local Medicare FFS costs, which is designed to ensure that only those Medicare Advantage plans that are able to provide valuable, low-cost options on a consistent and long-term basis will succeed. By aligning profitability with overall patient outcomes and total medical expenditures rather than volume of services, the Medicare Advantage system allows managed care companies to adopt a high-touch, comprehensive and long-term approach to care.
Medicare Advantage incentivizes holistic care through supplemental benefit offerings that address social determinants of health and daily lifestyle needs, driving the consumerism of senior healthcare
The Medicare Advantage program incentivizes plans to develop innovative products that better respond to seniors’ needs beyond traditional medical care. CMS has adopted a broad definition of supplemental benefits that allows Medicare Advantage plans to proactively offer cross-disciplinary services specifically targeting social determinants of health that can have a significant impact on seniors’ health outcomes. This shift in the United States healthcare industry’s regulatory landscape has given rise to new market opportunities for Medicare Advantage plans to provide more holistic healthcare solutions and achieve superior clinical outcomes for their members. By allowing Medicare Advantage plans to provide access to healthcare via typical care delivery services combined with supplemental benefits, such as a monthly allowance for groceries, transportation, vision and dental services and other targeted product features, CMS has enabled Medicare Advantage plans to continue to increase their value proposition to seniors.
The concept of healthcare expanding into the senior’s daily life, combined with the increasing prevalence of, and seniors’ increasing familiarity with, digital solutions, have been cited as key drivers in the trend towards the consumerization of the senior healthcare industry. We believe that seniors’ desire and demand for change is driving the growth of the Medicare Advantage market and we intend to continuously innovate to offer products that address seniors’ unmet needs. The convergence of senior healthcare with senior consumerism has created a high-value market that we are well-positioned to serve.
7
The enhanced value-proposition of value-based care models, coupled with the aging senior population, are leading to significant growth in Medicare Advantage
A growing number of seniors are choosing Medicare Advantage plans over traditional Medicare FFS. In 2010, only 24% of the Medicare eligible population, or 11.1 million seniors, were enrolled in a Medicare Advantage plan. In 2021, this number had grown to 44% of the Medicare eligible population, or 28 million seniors. Industry projections have forecasted a continued increase in the Medicare Advantage penetration rate, such that the population using Medicare Advantage plans is expected to increase to 37 million in 2025 as Medicare Advantage penetration accelerates to approximately 47%.
Medicare Enrollment Trend

Source: L.E.K. Consulting.
Full potential of the Medicare Advantage health plan model remains unrealized
We believe that Medicare Advantage is unique in that it allows one entity to influence the entirety of a senior’s healthcare through a singular, direct-to-consumer product. Through the ability to drive comprehensive healthcare delivery and leverage robust data and analytics at the helm of the senior’s healthcare ecosystem, the health plan can develop a personalized, adaptive and reproducible approach to care delivery. However, traditional Medicare Advantage plans are not technology driven, lack delivery of care capabilities and often outsource key functions; as such, these traditional plans have been unable to offer a fully-integrated healthcare ecosystem. These plans frequently operate disparate and antiquated IT systems assembled from historical acquisitions that do not permit the real time sharing and analysis of medical data and history, which is often key to a senior receiving the right treatment at the right time. As a result, existing Medicare Advantage plans often fall short in their attempts to significantly improve the quality of care and consumer experience for seniors.
We created a consumer-centric and purpose-built Medicare Advantage model that addresses the limitations of Medicare FFS and traditional Medicare Advantage plans by seizing the opportunities provided by evolving senior preferences, the consumerization of healthcare and changes in the regulatory landscape. By leveraging our purpose-built technology platform, we are able to rethink, redesign and deploy solutions specifically tailored to meet the needs and improve the lives of our seniors.
Our Market Opportunity
We address a $683 billion market opportunity today that is expected to grow 8% annually over the next decade.
We built the Alignment Healthcare platform to bring tech-enabled, consumer-centric healthcare to all seniors in the United States. Seniors represent the highest proportion of healthcare spending in the United States on a per capita basis. There are approximately 7.0 million Medicare eligible seniors and approximately 3.7 million Medicare Advantage enrollees in our current markets, which we estimate represents a total addressable market of approximately $87 billion.
We believe there is tremendous opportunity to further scale our business and address the growing need for seniors to experience a better approach to healthcare. The Congressional Budget Office projects net Medicare spending to be $683 billion in 2021 and expects that figure to exceed $1.3 trillion by 2030, representing an 8% compound annual growth rate. Furthermore, with seniors increasingly choosing Medicare Advantage over traditional Medicare FFS, federal spending on payments to Medicare Advantage plans is projected to increase from $348 billion in 2021 to $491 billion in 2025, representing a 9% compound annual growth rate.
8
Ultimately, we believe our relentless pursuit of putting the senior first will allow us to capture market share in a sector with significant demographic tailwinds.
Alignment’s Virtuous Cycle
Our model is based on a flywheel concept, referred to as our “virtuous cycle”, which is designed to delight our senior consumers. We start by listening to and engaging with our seniors in order to provide a superior experience, in both their healthcare and daily living needs. Through our AVA technology platform, we utilize data and predictive algorithms that are specifically designed to ensure personalized care is delivered to each member. When our information-enabled care model is combined with our member engagement, we are able to improve healthcare outcomes by, for example, reducing unnecessary hospital admissions, which in turn lowers overall costs. Our unique ability to manage healthcare expenditures, while maintaining quality and member satisfaction, is a distinct and sustainable competitive advantage. The lower total healthcare expenditures allow us to reinvest our savings into richer coverage and benefits, which propels our growth in revenue and membership due to the enhanced consumer value proposition. As we grow, we continue to listen to and incorporate member feedback, and are able to further enhance benefits and produce strong clinical outcomes. Our virtuous cycle, based on the principle of doing well by doing good, is highly repeatable and a core tenet of our ability to continue to expand in existing and new markets in the future.
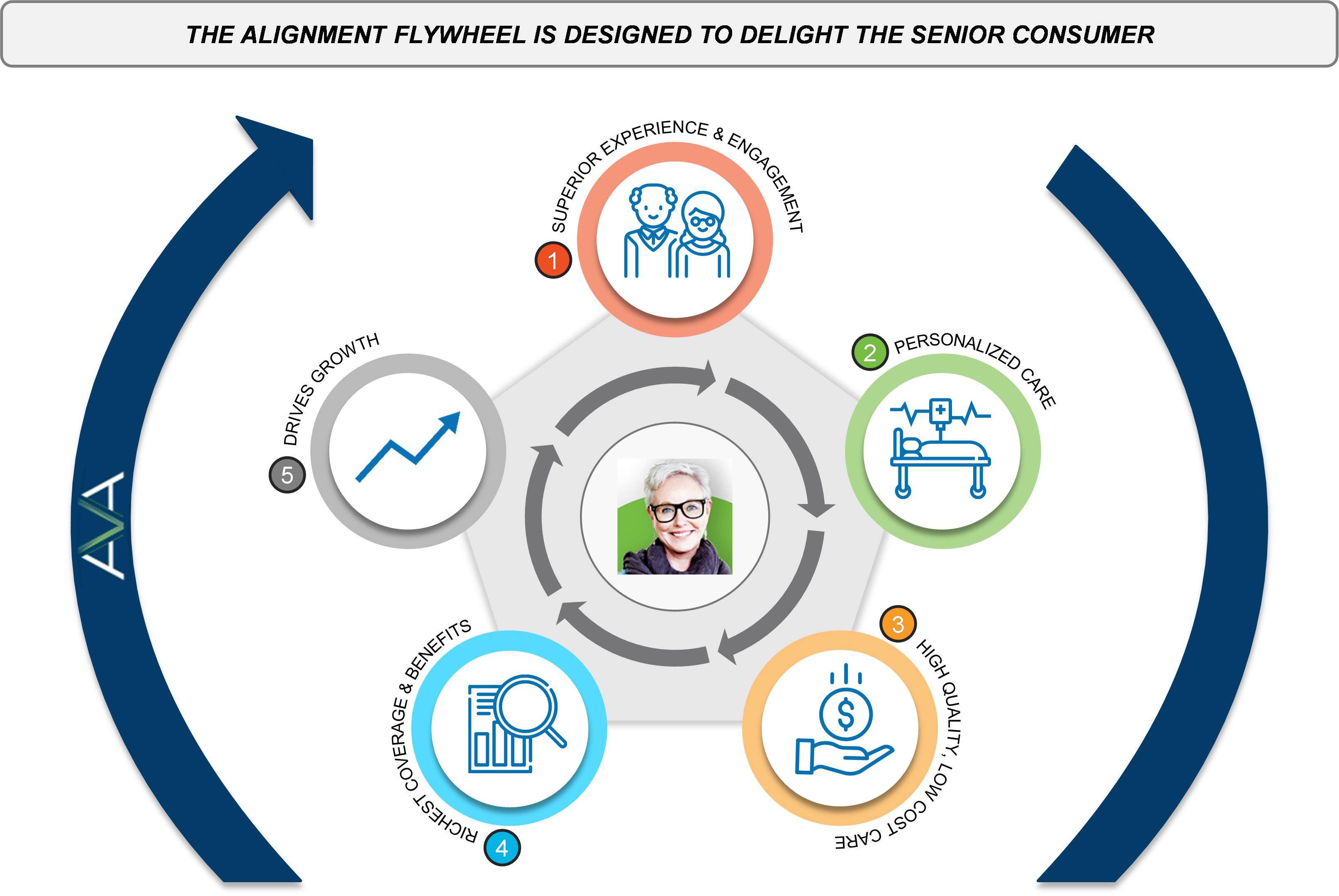
1) Superior experience and engagement: Our philosophy for serving seniors starts with our goal of treating each member as if they were our own mother, father or loved one. We have developed a variety of programs that are designed to address seniors’ healthcare and social needs. Our AVA platform provides care teams with actionable insights that help strengthen the quality and efficacy of our touch points with members. Additionally, our comprehensive benefit offerings establish us as fixtures in our members’ daily lives, which uniquely positions us to serve as an advocate when navigating the complexities of the healthcare system. Combined with consumer engagement activities, such as companion care (providing “grandkids on-demand”) and the delivery of meals and masks to members during the COVID-19 pandemic, we are able to build trusting, long-term relationships with our seniors.
2) Personalized care: AVA uses comprehensive data and predictive analytics to identify the needs of our members and create personalized experiences in every aspect of how we care for and serve them. We educate and provide timely information to our broader network of independent physicians to optimize health outcomes for our overall member population, and we deploy our internal clinical resources to care for our highest risk, most complex members. To manage our highest risk members, we rely on AVA to enable seamlessly integrated virtual and at-home healthcare delivery by utilizing direct “smart” interactions through the most effective engagement channels. For those of our members who are less vulnerable, we partner with local providers and support them with Alignment’s insights and resources to deliver high-quality, coordinated care. Members also have 24/7 access to a dedicated concierge team that can assist with medical needs, care navigation, transportation and other services that are important to the health of our members.
3) High-quality, low-cost care: The economic model underlying the Medicare Advantage value-based framework enables us to invest in preventative health and wellness activities, which reduce unnecessary medical events that can have lasting, negative consequences for our seniors. If a single nurse visit to a high-risk senior’s home prevents an avoidable hospitalization, then that visit represents a 30 to 1 return-on-investment, based on our internal calculations of the average cost of a nurse visit and hospitalization. Our ability to provide high- quality and low-cost care is critical to our ability to continue to offer a superior product offering and is a defining characteristic of our company relative to our competition.
9
4) Richest coverage and benefits: We leverage our improved clinical and operating results to proactively invest in more comprehensive coverage and richer benefits for our members, as well as in additional services that support the full spectrum of seniors’ daily healthcare and social needs. While we tailor our various products to meet the individual needs of our diverse consumers, we strive to consistently deliver the Alignment experience and enhanced value proposition across all offerings. For example, in 2022 we are offering $0 member premium products in 32 out of our 38 markets across California, North Carolina, Nevada, and Arizona.
5) Drives growth: Our next generation platform is designed to drive superior member experiences, differentiated clinical results and strong financial outcomes, which has led to a compound growth rate since inception through December 31, 2021, of 37% in revenue and 31% in the number of members enrolled in our HMO and PPO contracts ("Health Plan Membership"). See “—Our Results” below. As we continue to grow and increase density within existing markets, Alignment’s brand recognition with senior consumers, relationships with the broker community, and ability to influence provider behavior will continue to power our flywheel and drive sustained growth in our current and new markets.
Our Results
In order to achieve our mission of improving healthcare one senior at a time, we have developed a business model with a predictable, recurring revenue stream that provides significant visibility into our financial growth trajectory. We generally contract directly with CMS as a licensed Medicare Advantage plan and receive a recurring per member per month ("PMPM") payment in exchange for bearing the responsibility of our members’ healthcare outcomes and expenditures. These contractual arrangements, combined with the fact that the majority of our net membership growth occurs effective on January 1 of a calendar year after the annual enrollment period ("AEP"), provide a higher degree of visibility to our full year projected revenue early in the calendar year, subject to our ability to model for in-year member growth, as well as revenue PMPM, which in turn depends on member health and mortality trends.
We believe that Medicare Advantage is unique in that it allows one entity to influence the entirety of a senior’s healthcare through a single, direct-to-consumer product. Our platform is designed to maximize the benefits of Medicare Advantage, with all stakeholders being rewarded as we improve the clinical outcomes and experience for our consumers. We believe that the outcomes below clearly demonstrate the success of our unique consumer-centric platform by delivering on the promise of our virtuous cycle.

* Excludes the costs of our clinical model investments, which are comprised of the annual expenditures we incur to deploy our internal clinical resources, including the costs of employing doctors, nurses, case managers, social workers and medical supply costs, among others. We’ve been able to maintain a 70-78% MBR range (excluding the costs of our clinical model investments) for our year 5+ at-risk members throughout the COVID-19 pandemic despite the adverse impact COVID has had on our claims per member per month and revenue per member per month across cohorts.
10
Our ability to deliver lower healthcare costs while improving the consumer’s experience is a unique competitive advantage. This differentiation has led to our demonstrated ability to rapidly scale, as evidenced by the expansion of our model to 38 markets across four states covering approximately 92,700 Health Plan Members as of January 1, 2022. We believe we have proven that our model is highly predictable and repeatable across different markets and will enable strong growth on a national level as we pursue our vision of becoming the most trusted senior healthcare brand in the country.
We anticipate further investments in our business as we expand into new markets and continue to offer additional innovative product offerings and supplementary benefits in order to attract new members. Accordingly, in the near term we expect that as our business grows our costs related to this growth, such as expanding our operations, hiring additional employees and operating as a public company, also will increase. However, in the longer term we anticipate that these investments will positively impact our business and results.
Our Product Solutions
We leverage our control of the full healthcare dollar and plan design to rethink, redesign and deploy innovative products based on the needs and changing preferences of seniors
We deliver our healthcare platform through our Medicare Advantage plan offerings. Our plan offerings reflect CMS’s advocacy for improving seniors’ healthcare experience and addressing social determinants of health, and represent the convergence of quality healthcare, enhanced customer experience and lifestyle-focused features in a direct-to-consumer product. We recognize that no two seniors are alike and strive to meet the needs of a diverse array of consumers. We do this by offering various products that are designed with different populations in mind, all while providing personalized, easy to navigate healthcare with a great consumer experience at a superior value.
Our current product portfolio consists of Medicare Advantage products tailored to take into account factors such as health condition (ranging from plans for healthy members to chronic special needs plans), socioeconomic status (including Medicare and Medicaid dually-eligible special needs products), and ethnicity (including our new Harmony product, featuring benefits associated with Eastern medicine disciplines). Each product is carefully developed to create an offering that will suit the needs of the diverse senior population.
Our product offerings are described in the table below.
11
|
|
|
|
|
Product |
|
Consumer Target |
|
Product Description |
HMO |
|
Cost Conscious, Value Oriented |
|
Zero or low monthly premium, high value, more limited provider network |
|
|
|
||
Dually-Eligible |
|
Low Income, Complex Medical Conditions |
|
Product designed for |
|
|
|
||
Provider Sponsored Plan |
|
Provider Brand Conscious |
|
Co-branded or provider-aligned to jointly market the access of a specific provider with Alignment’s MA capabilities |
|
|
|
||
Chronic Special Needs |
|
Polychronic Conditions, Extra Care Support |
|
Specialized product design geared towards certain chronic conditions, such as Cardiovascular Disorders, Chronic Heart Failure, and/or Diabetes |
|
|
|
||
PPO |
|
Higher Income, Values More Choice |
|
Greater network flexibility, potentially higher monthly premium /out-of-pocket cost |
|
|
|
||
Virtual Care |
|
Tech-savvy; Telehealth Oriented |
|
Virtual-first primary care offering with rich and expansive supplemental benefits |
|
|
|
||
Ethnic Product Lines |
|
Traditionally Underserved Ethnic Communities |
|
Features products designed with the Asian and Hispanic communities in-mind |
|
|
|
||
Traditional Medicare/Direct Contracting Entity |
|
Original Medicare; Strong PCP Relationship |
|
Value-based arrangement with CMS for beneficiaries who want to remain in traditional Medicare |
In 2020, we launched Preferred Provider Organization (“PPO”) offerings in select markets, which we believe will be attractive to those seniors that prefer a more open network design. We have also continued to innovate by launching a unique virtual care plan, which will allow our members to select a virtual provider as their primary care physician, enjoy a rich array of benefits, and still access local, in-person healthcare resources when needed. These new and exciting product line expansions will still feature the same quality and experience that members have come to expect of other Alignment products, and our clinical team will continue to pursue proactive care management to ensure we can deliver innovative plans at an attractive price point to the consumer.
We believe that addressing the social determinants of health has a significant impact on the overall health of our seniors. As such, we have expanded our focus beyond traditional medical benefits to design products that provide seniors with a package of benefits and experiences that cover both healthcare and lifestyle needs. In addition to competitive pricing and coverage for primary care providers, specialists, inpatient and emergency room visits, vision, hearing, lab/x-ray services, pharmaceutical coverage and other similar benefits that many Medicare Advantage plans offer, we offer numerous additional features including:
12
While not every plan feature is available to all of our members and certain plan features entail additional costs, we have designed our existing portfolio of products to provide us with the flexibility to meet the distinctive needs of the communities we serve and our diverse membership. Our product solutions—supported by AVA and our integrated care delivery capabilities—are core to our mission of providing the highest-quality healthcare experience to all seniors.
Our Technology: Alignment’s Virtual Application
AVA empowers senior consumers and all the constituents in their health journey with relevant, timely and complete information as well as actionable insights to improve their health experience and outcomes.
Our position in the healthcare ecosystem as a Medicare Advantage plan and having our proprietary unified data platform provides us with differentiated access to large amounts of member data. With the benefit of this information, we are better able to effect change and positively impact our members’ healthcare experience. Since our founding, we have recognized that harnessing data and information had to be core tenants of our technology solution and care delivery model. As such, we leveraged our management team’s experience across healthcare and technology to build AVA—our proprietary technology platform designed to provide the best health outcomes and experiences for our members. AVA is a core system that was purpose-built from the ground up with the senior population and their ecosystem in mind. The benefits of AVA apply to our members, as well as everyone in their care ecosystem, including doctors, nurses, caregivers, health plan operational teams and health insurance brokers.
Key aspects of the AVA platform include:
13
Personalized Application Ecosystem: AVA offers a digital ecosystem with a personalized and customizable suite of applications for consumers, internal care teams, external provider partners, health plan operations and brokers/sales agents:
14
When paired with our operational expertise, we believe AVA is integral to our ability to drive our operations and business outcomes consistently across markets. AVA provides us with the flexibility to adapt our operating models to meet the needs of local communities and providers, while achieving high-quality, low-cost care in each market. We designed our technology tools and applications to result in a customized, yet consistent, experience for our members. From driving workflows to enabling smarter interventions, we believe AVA is a significant competitive advantage that allows us to deliver information-enabled healthcare at scale.
Our Clinical Model
We engage regularly with members as part of their daily lives and proactively manage their chronic conditions to improve outcomes and reduce cost.
Our clinical model is designed specifically for seniors and is managed across multiple disciplines (medical, social, psychological, pharmaceutical and functional) and sites of care (home, inpatient, outpatient, virtual and others). Our internal care teams and external providers use AVA to coordinate high-quality care for members and manage the complexity of the healthcare system. Given the prevalence of comorbidities within our chronically ill members, coordination across a multi-disciplinary care team is vital to providing a medical and behavioral care plan that drives improved outcomes.
Our care delivery model creates a highly personalized experience that is unique to each member depending on their personal health and circumstances. Our clinical continuum separates seniors into four categories in order to provide optimized care for every stage of a senior’s life: healthy, healthy utilizer, pre-chronic and chronic. We organize members into these care requirement categories using insights derived from AVA, which reflects detailed profiles of each members’ individual risks and gaps in care based on our longitudinal and comprehensive data sets. The data below represents a sample of our population stratification from 2021.

Healthy: The typical member in the “healthy” category requires low levels of medical care. Healthy members comprise approximately 74% of our membership base but account for only 4% of the institutional claims submitted.
Healthy Utilizer: The typical member in the “healthy utilizer” category is an otherwise healthy senior who has had isolated or unexpected health challenges requiring significant medical care. Healthy utilizers comprise approximately 8% of our membership base and account for 22% of the institutional claims submitted.
Pre-Chronic: The typical member in the “pre-chronic category” is identified as high-risk by AVA but has yet to incur significant healthcare expenditures. We also refer to these members as on the “launching pad”, and by deploying our targeted care programs towards this population we work to prevent or slow their increasing acuity levels. Pre-chronic members comprise approximately 8% of our membership but account for only 1% of the institutional claims submitted. Our active approach to monitoring gaps in care and acting before emerging health problems worsen is reflective of the culture of care embedded in our organization, and our focus on being a persistent advocate for our members.
15
Chronic: The typical member in the “chronic” category is generally a complex patient with multiple chronic conditions in need of significant, coordinated care. Chronic members comprise 10% of our membership but account for 73% of the institutional claims submitted.
Proactive, Coordinated Care Management
The majority of healthy and healthy utilizer members’ care needs are managed by our network of local community providers in conjunction with our support and oversight. We utilize continuous communication with our network of independent primary care providers to ensure that our members have access to preventative and ongoing care. We have also established a variety of tools and applications that provide us with insight into how our various providers are performing on key quality and cost metrics. We use this data to create a routine feedback loop with our external providers for the benefit of our broader senior population.
Our pre-chronic and chronic members are typically targeted for engagement through our Care Anywhere program. Care Anywhere is an advanced clinician-driven model of care that is staffed by Alignment-employed physicians, advanced practice clinicians, case managers, social workers and behavioral health coaches to assure execution of cross-functional care plans. Unlike many managed care plans, we have built these services in-house to provide valuable, high-quality care to members for free, which complements the care provided by our provider partners for their most challenging and resource-intensive patients. On average, a Care Anywhere patient is 77 years old, has five to six chronic conditions and monthly institutional healthcare expenditures in excess of $2,500 prior to their first Care Anywhere visit.
We structure our Care Anywhere program with a focus on prioritizing compassionate and effective care delivery and proactive health management. Key features of the Care Anywhere program include: proactive outreach; 24/7 access; highly detailed personalized care plans; and enhanced coordination of care and social needs. Standardized care programs are targeted to seniors based on their underlying conditions, such as Chronic Heart Failure or Chronic Obstructive Pulmonary Disorder, which are then personally tailored based on each individual’s underlying circumstances. We engage with this high-risk group of seniors based on their preferences for care delivery, which is typically in their homes or through telephonic and video consultations. During the initial months of the COVID-19 pandemic, we were able to rapidly pivot the modality of our clinical care to a virtual setting. In a period of 30 days, we went from approximately 97% of our care delivered in the home to 100% care delivered telephonically and virtually. Since the beginning of the COVID-19 pandemic in March 2020, approximately 74% of our Care Anywhere engagement has been telephonic or virtual. Our abrupt shift in modality of care exemplifies our adaptability and willingness to prioritize the safety and convenience of our members most in need of care.
We believe the combined capabilities of customized, coordinated care delivery with our health plan capabilities for this vulnerable population uniquely positions us in the marketplace and differentiates us from other healthcare companies. We believe, based on data gathered and analyzed using AVA, that our Care Anywhere program creates several benefits for our high-risk, complex members: improved quality of life, high patient satisfaction, reductions in unnecessary emergency room visits and inpatient care, and lower re-admission rates. This also allows us to establish a more direct relationship with seniors, building member loyalty and brand recognition. Our Care Anywhere program has an NPS score greater than 75, underscoring the positive impact it has on our most vulnerable members. These improved outcomes translate into financial savings that we can reinvest in our product offerings, which we believe is a significant competitive advantage.
The following real-life case studies demonstrate how we combine our technology with our cross-functional senior care programs in our pursuit of serving our seniors:
Case Study #1—Cross-Disciplinary Care Plans Tailored to the Needs of Our Members
The Issue: Mr. Smith suffers from multiple chronic conditions, including severe depression, schizophrenia, opioid dependence and estrangement from his three adult children. His PCP is not aware that the opioids he takes have rendered his psychiatric medications ineffective due to drug-to-drug interactions.
Typical Outcome: No intervention, which results in the continued use of an ineffective combination of medications, potentially leading to increased psychiatric issues, social isolation and hospitalizations.
AVA Response: AVA identifies Mr. Smith as a high-risk member based on his clinical profile. Additionally, AVA algorithms alert us to his recent history of multiple emergency room visits, hospitalizations (20+ in one year) and inpatient psychiatric admissions. Post-engagement, AVA continues to ingest diverse sources of raw data on his medication, treatments received, provider interactions and use of supplemental benefits (e.g., transportation) in order to support our Care Anywhere team’s high-touch management of Mr. Smith’s care.
Alignment Superior Solution: Once AVA identifies Mr. Smith’s issues, the Care Anywhere team devises a holistic, high-touch care plan which includes regular outreach, care coordination across his providers and pharmacy, and a support
16
system for him via family, neighbors and community service providers. Mr. Smith’s care team also identifies the medication regimen that works best for him and coordinates with transportation providers and a local pharmacy to ensure he has reliable access to the care and medications he needs.
Case Study #2—Preventing Unnecessary Hospitalizations by Addressing Social Factors
The Issue: Due to a lack of financial stability and low health literacy, Mr. Jones, a Type 1 diabetic since childhood, frequently visits the emergency room in response to low blood sugar because he cannot afford a balanced diet.
Typical Outcome: Mr. Jones continues visiting the emergency room and has a high likelihood of hospital readmission. The root cause of his frequent utilization goes unaddressed.
AVA Response: AVA’s AI algorithms leverage the social determinant and chronic illness diagnosis data to stratify the member as high-risk. Mr. Jones’ telehealth call for low blood sugar is automatically routed to the after-hours on-call physician at Alignment due to his status in AVA as a vulnerable member. AVA’s Patient 360 platform notifies the on-call physician of the member’s food needs, leading to an after-hours call and targeted intervention.
Alignment Superior Solution: Alignment’s on-call physician queries the member regarding his food instability, and after gaining an understanding of the significant barriers he faces has food delivered to Mr. Jones within 30 minutes to elevate his blood sugar. Mr. Jones is enrolled in the Care Anywhere program and seen by a nurse the next morning, who then enrolls him into Mom’s Meals food delivery program. Mr. Jones has regular check ins with the Alignment social worker and Care Anywhere provider which prevents further emergency room utilization for low blood sugar. Mr. Jones is a highly satisfied member given Alignment’s initial intervention and ongoing support.
Case Study #3—Clinical Interventions Leveraging Longitudinal Member Data
The Issue: Mrs. Johnson enters an emergency room at an out-of-network facility with shortness of breath and an undiagnosed pulmonary embolism (blood clot in her lung).
Typical Outcome: After a brief evaluation, the emergency room doctor sends Mrs. Johnson home without any communication with the patient’s health plan. The health plan may not know Mrs. Johnson was in the emergency room until a claim arrives 30 days later. Meanwhile, Mrs. Johnson’s pulmonary embolism remains undiagnosed and untreated, leaving Mrs. Johnson vulnerable to a catastrophic outcome.
AVA Response: AVA generates a notification of Mrs. Johnson’s emergency room visit through a centralized data feed. AVA, which contains Mrs. Johnson’s entire medical history, including information from unrelated specialists, indicates a high risk of blood clots based on a pharmacy alert triggered by a prescription for an anticoagulant medication in her medical records. The AVA Patient 360 platform shares the alert with Alignment’s on-call physician.
Alignment Superior Solution: Alignment is ready and equipped to provide consultation with emergency room doctors 24 hours a day. The Alignment on-call physician engages with the emergency room physician to discuss the AVA alert, causing the emergency room doctor to conduct a further assessment of Mrs. Johnson’s condition. Upon further evaluation, the emergency room doctor recognizes the significant risk at-hand and immediately has Mrs. Johnson admitted to the hospital instead of sending her home as previously planned. Mrs. Johnson then has her blood clot appropriately treated, potentially avoiding a catastrophic outcome.
Our collective investment in our care model and technology platform has produced strong clinical outcomes for our seniors. In 2021, we achieved a hospitalization rate of approximately 156 hospitalizations per every 1,000 at-risk members, which is approximately 38% better than the 2019 Medicare FFS performance in our markets. Further, we have achieved approximately 155-165 inpatient admissions per thousand on our at-risk membership for the last five years in a row, in spite of our significant membership growth over that period of time.
17

(1) FFS benchmark based on 2021 enrollment mix by market using 2019 Medicare FFS data. 2021 inpatient admits/k metric represents estimated full year 2021. Historical periods include estimated utilization where appropriate to account for billing settlements.
Our Growth Strategy
Accelerate our “virtuous cycle” flywheel to drive growth across markets while continuing to innovate and expand our product offerings.
The key elements of our growth strategy include:
Capitalize on the significant opportunity within our current markets
We currently operate in 38 markets, or counties, across California, North Carolina, Nevada and Arizona. We had approximately 92,700 Health Plan Members across these markets, as of January 1, 2022, representing approximately 3% of the overall market share among seniors that are in a Medicare Advantage plan in these counties; as such, we believe there is tremendous opportunity for growth in our existing geographical footprint. Meanwhile, we believe we have demonstrated an ability to compete with much larger competitors due to the significant value proposition of our product offerings:
We selected our initial markets due to their highly concentrated senior populations and favorable statewide demographic trends. For example, California has over 6.5 million Medicare eligible seniors, the highest of any state. According to CMS data, Los Angeles County alone has more seniors than 38 individual states. There are approximately 7.0 million Medicare eligible seniors and approximately 3.7 million Medicare Advantage enrollees in our current markets, which we estimate represents a total addressable market of approximately $87 billion. Additionally, Medicare Advantage penetration is rapidly increasing in our existing markets, reaching 52% across California, North Carolina, Nevada and Arizona, according to CMS as of January 2022.
18
We attract new members through both our internal and external sales channels. Our internal sales channel consists of Alignment representatives, both in the field and telephonically, who market and sell Alignment’s portfolio of products to prospective members. This channel also includes our new sales to members who sign up using Alignment’s direct online enrollment tools. Our external sales channel consists of partnerships with third party broker channels who sell Alignment products alongside competing products. These third-party organizations also employ in person, telephonic and online sales distribution channels. Our growth will depend on our continued success in marketing our products through these channels. We believe that we will continue to gain share in our current markets due to our strong track record of providing exceptional care, expanding our network with new contracts and innovative partnerships with a wide array of providers and offering a best-in-class member experience.
Expand into new markets
Given our track record of delivering exceptional results and delighting consumers in our existing markets, we recently launched our national expansion strategy guided by our disciplined approach to identifying new markets. In geographically adjacent markets, we have the benefit of leveraging our existing provider relationships and infrastructure to expand more rapidly in a less capital-intensive manner. In entirely new markets, we can reach scale quickly given our highly portable and adaptable AVA technology platform and our wealth of transferable care management expertise. We have identified additional markets for potential expansion in 2023 and beyond to continue to extend our growth runway.
Our model enables us to deliver high quality care and exceptional experience for our members across a diverse array of markets. We intend to focus on markets with significant senior populations where we expect to be able to replicate our model most effectively. An important component of our model is our ability to be flexible in our approach to contracting with provider partners and to tailor our applications and services. Since our founding in 2013, we have been successful in rural, urban and suburban markets, as well as markets with varying degrees of provider and health system competition and control. Additionally, our markets feature a diverse array of membership profiles across ethnicities, income levels and acuity. As a result, our model and platform are designed to scale and allow us to provide a predictable and replicable set of outcomes, regardless of the local market considerations.
Through our thoughtful and disciplined national expansion strategy, we believe we will be able to sustainably scale and reliably replicate our competitive advantages in new markets.
Partner with providers to accelerate growth and improve operational performance
We intend to grow in new and existing markets by leveraging the flexibility and adaptability of our model to contract with provider partners across a spectrum of risk sharing arrangements. Across our 38 existing markets, we have a wide variety of successful operating and financial arrangements with medical groups, shared risk providers, affiliate providers, providers employed by health systems and community-based, independent primary care physicians. These arrangements typically have multi-year terms across a number of contractual and financial frameworks. Our approach to contracting includes forms of capitation, including global, partial, or primary care risk, and fee-for-service payments. In addition to the basic form of the contract, and to further align ourselves with our provider partners, we often use upside-only incentive programs in an effort to engage our delivery network towards coordinating and supporting our members’ care delivery plans, including the provision of high-quality, cost-effective care. Within these relationships we can deploy different aspects of the existing Alignment toolkit depending on the level of risk and provider infrastructure. Our value-based approach to patient care and provider contracts, including profit and risk share programs, ensures that economic incentives are well-aligned so that providers can focus on delivering the best care. By enabling successful outcomes and offering an appealing value proposition to new provider partners, we are able to grow in new markets and rapidly build out robust provider networks that drive further growth for our platform.
We have also developed a track record of enabling mid-sized independent physician associations ("IPAs") and provider groups to thrive by providing them with access to a scaled platform that includes provider tools and support structures that enable them to effectively manage Medicare Advantage patients. As we grow and continue to partner with the physician community, we believe there will be increased opportunities to vertically integrate with providers. These opportunities could come in the form of minority investments, affiliate-relationships, joint ventures or acquisitions, and could generate growth and longer-term margin expansion opportunities by capturing additional channels of revenue outside of the Medicare Advantage business model. Vertical integration provides a true win-win scenario in which the member, physician and health plan benefit from better care coordination, enhanced product design and delivery, and superior data sharing and operational integration. These integrated benefits lead to an improved consumer experience and increased ability to invest in growth.
Expand services and product offerings
19
We see substantial opportunity to continue to build on our existing Medicare Advantage health plan offerings by providing an expanding portfolio of direct-to-consumer products. With the launch of our Medicare Advantage PPO products in 2020, we began to offer senior members additional choices while still relying on our sophisticated technology platform and member support model to provide proactive care to our members. Furthermore, the COVID-19 pandemic has accelerated a shift towards and increased preference for virtual care. As a result, we launched a virtual care plan in 2021, which allows our members to select a virtual provider as their primary care physician, enjoy a rich array of benefits, and still access local, in-person healthcare resources when needed. We will continue to tailor new Medicare Advantage product offerings to meet the distinct needs of our members in the future, such as potentially offering special needs plans tailored for niche populations.
We believe we can continue to drive our longer-term growth by insourcing certain product lines over time, such as vision, dental, specialty pharmacy, and others. We believe this “horizontal integration” of various product features can be further coupled with other forms of more “vertical integration”, such as hospice, home health or behavioral health, to directly serve a broader range of our members’ needs. Expanded offerings will continue to provide our healthcare consumers with more integrated services, which enhances their Alignment experience and contributes to improved quality of life and health.
Extending the Alignment model to broader senior populations
We will continue to innovate as regulatory changes expand our opportunities to deliver the Alignment experience to seniors in traditional Medicare and we are evaluating other opportunities to leverage our historical investments in our technology platform and our comprehensive clinical model across our existing and potentially new geographies. For example, we recently entered into CMS Innovation Center’s Direct Contracting program, which allows us to partner directly with physicians to help manage their Medicare FFS patient populations and participate in the upside and downside risk for caring for traditional Medicare members associated with managing the health of such patients. This program opens additional opportunities for us to deploy our technology platform and care management capabilities across a broader set of members and potentially new markets. As of December 31, 2021, we had approximately 5,400 members in our DCE arrangement with our physician partners in North Carolina, California and Nevada. While still early, we believe this DCE partnership is indicative of the value Alignment can potentially deliver to a broader set of seniors in traditional Medicare over time.
Grow through strategic acquisitions
We continually evaluate potential acquisition targets that would accelerate growth, enhance our care delivery model, and/or allow us to apply the Alignment model across broader populations. We will primarily focus on acquiring healthcare delivery groups in key geographies, standalone and provider-sponsored Medicare Advantage plans and other complementary risk bearing assets. We will also selectively explore additional opportunities that serve to enhance our technology platform and product offerings for our members and partners.
Regulation
Our operations and those of our affiliated entities are subject to extensive federal, state and local governmental laws and regulations. These laws and regulations require us to meet various standards relating to, among other things, reports to CMS, personnel qualifications, maintenance of proper records and quality assurance programs and patient care. The majority of our regulation and oversight comes from CMS, which regulates almost every aspect of our business, including our provider network, benefits, member enrollment, risk adjustment program, plan offerings, claims payments, quality improvement programs, and appeals and grievances. We have entered into standard form agreements with CMS pursuant to Sections 1851 through 1859 and Sections 1860D-1 through 1860D-43 of the SSA, pursuant to which we have agreed to operate our plans in accordance with applicable laws and regulations and CMS has agreed to make payments to us under the SSA. Each CMS contract has a one year term expiring on December 31 of the calendar year and is subject to annual one-year renewal terms. Under the contracts we are obligated to provide our members basic benefits and services covered by Part A and Part B of the original Medicare Program, any applicable supplemental benefits we elect to provide in our final benefit and price bid proposals approved by CMS, and prescription drugs. The CMS contracts further require us to develop our annual benefit and price bid proposals and submit to CMS all related information on premiums, benefits and cost sharing by no later than the first Monday in June prior to the commencement of the subsequent calendar year to which they apply, in accordance with the CMS regulations. Each CMS contract may be terminated by mutual consent or by CMS or by us for cause. We are required to accept new enrollments, make enrollments effective, process voluntary disenrollments and limit involuntary disenrollments in accordance with the CMS regulations. Generally, to enroll or remain enrolled in one of our Medicare Advantage plans, an individual must be a U.S. citizen or lawfully present in the U.S., be entitled to Medicare under Part A and enrolled in Part B, reside in the service area covered by the plan, complete and sign the required election forms to enroll and agree to abide by the rules of the Medicare Advantage plan into which he or she is enrolled or intends to enroll. Such agreements also provide for member and provider protections and marketing requirements, as well as recordkeeping and reporting requirements, all with reference to applicable laws and regulations. If any of our operations or those of our affiliated professional medical corporations are found to violate applicable laws or regulations, we could suffer severe consequences that would have a material adverse effect on our business, results of operations, financial condition, cash flows, reputation and stock price, including:
20
We expect that our industry will continue to be subject to substantial regulation, the scope and effect of which are difficult to predict. See “Risk Factors—Risks Related to Regulation.”
In addition to the SSA, CMS regulations, and our contractual obligations, we must also comply with a variety of other laws:
HIPPA, HITECH Act and Other Laws, Rules and Regulations Related to Data Privacy
We are subject to data privacy and protection and breach notification laws and regulations that apply to the collection, transmission, storage and use of PHI and other PII, which among other things, impose certain requirements relating to the privacy, security and transmission of PII. The legislative and regulatory landscape for privacy and data protection continues to evolve, and there has been an increasing focus on privacy and data protection issues with the potential to affect our business. Failure to comply with any of these laws and regulations could result in enforcement action against us, including fines, public censure, claims for damages by affected individuals, damage to our reputation and loss of goodwill, any of which could have a material adverse effect on our business, financial condition, results of operations or prospects. Ongoing efforts to comply with evolving laws and regulations may be costly and require ongoing modifications to our policies, procedures and systems.
The use of individually identifiable health data by our business is regulated at federal and state levels. These laws and rules are changed frequently by legislation or administrative interpretation. Various state laws address the use and maintenance of individually identifiable health information. Most are derived from the privacy and security regulations promulgated under HIPAA. HIPAA includes administrative provisions directed at simplifying electronic data interchange through standardizing transactions, establishing uniform healthcare provider, payer, and employer identifiers, and establishing regulations aimed at protecting confidentiality and security of patient and member data. The rules preempt all inconsistent state laws unless the state law is more privacy-protective. These regulations, in addition to other state laws, set standards for the security of electronic health information, including requirements that insurers provide customers with notice regarding how their individually identifiable health information is used.
21
HIPAA imposes mandatory penalties for certain violations. In 2022, penalties for violations of HIPAA and its implementing regulations start at $120 per violation and are not to exceed approximately $60,000 per violation, subject to a cap of approximately $1.8 million for violations of the same standard in a single calendar year. However, a single breach incident can result in violations of multiple standards. HIPAA also authorizes state attorneys general to file suit on behalf of their residents for statutory damages of up to $25,000. While HIPAA does not create a private right of action allowing individuals to sue in civil court for violations of HIPAA, its standards have been used as the basis for duty of care in state civil suits such as those for negligence or recklessness in the misuse or breach of PHI.
In addition, HIPAA mandates that the Secretary of the Department of Health and Human Services (“HHS”) conduct periodic compliance audits of HIPAA-covered entities and business associates for compliance with HIPAA’s privacy and security standards. It also tasks HHS with establishing a methodology whereby harmed individuals who were the victims of breaches of unsecured PHI may receive a percentage of any civil monetary penalty fine paid by the violator.
HIPAA further requires that members be notified of any unauthorized acquisition, access, use or disclosure of their unsecured PHI that compromises the privacy or security of such information, with certain exceptions related to unintentional or inadvertent use or disclosure by employees or authorized individuals. HIPAA specifies that such notifications must be made “without unreasonable delay and in no case later than 60 calendar days after discovery of the breach.” If a breach affects 500 patients or more, it must be reported to HHS without unreasonable delay, and HHS will post the name of the breaching entity on its public web site. Breaches affecting more than 500 patients in the same state or jurisdiction must also be reported to the local media. If a breach involves fewer than 500 people, the covered entity must record it in a log and notify HHS at least annually.
We also publish statements to our members and partners that describe how we handle and protect PHI. If federal or state regulatory authorities or private litigants consider any portion of these statements to be untrue, we may be subject to claims of deceptive practices, which could lead to significant liabilities and consequences, including, without limitation, costs of responding to investigations, defending against litigation, settling claims, and complying with regulatory or court orders.
Data privacy and security at the state level remains an evolving landscape. For example, California’s California Consumer Privacy Act of 2018 (“CCPA”), which came into effect on January 1, 2020, requires companies that process information on California residents to make new disclosures to consumers about their data collection, use and sharing practices, allow consumers to opt out of certain data sharing with third parties and provides a new cause of action for data breaches. In addition, on November 3, 2020, California voters approved a new privacy law, the California Privacy Rights Act (“CPRA”), which significantly modifies the CCPA, including by expanding consumers’ rights with respect to certain personal information and creating a new state agency to oversee implementation and enforcement efforts. This agency will be able to finance operations through penalties issued and with the CPRA’s removal of the mandatory cure period from CCPA, we will have less warning before compliance risk results in legal action. Many of the CPRA’s provisions will become effective on January 1, 2023. The CCPA and CPRA contain exemptions for medical information governed by the California Confidentiality of Medical Information Act, and for PHI collected by a covered entity or business associate governed by the privacy, security, and breach notification rule established pursuant to HIPAA, but the precise interpretation and application of this exemption by regulators is not yet clear.
The CCPA has prompted a number of proposals for new federal and state-level privacy legislation. Such proposed legislation, if enacted, may add additional complexity, variation in requirements, restrictions and potential legal risk, require additional investment of resources in compliance programs, impact strategies and the availability of previously useful data and could result in increased compliance costs and/or changes in business practices and policies. For example, the Virginia Consumer Data Protection Act, or the CDPA, signed by the Governor on March 2, 2021 and effective January 1, 2023, gives Virginia residents expanded rights to access and creates additional obligations on companies covered by the legislation.
While the CPRA/CCPA is an example of consumer privacy law, the NAIC’s Insurance Data Security Model Law (the “Model Law”) is a different type of law focused on securing insurance licensees’ information systems. Versions of this Model Law have been passed in many states and are expected to be passed in more states in the coming years. Similar to HIPAA, the Model Law requires technical, administrative, and procedural information security practices and procedures and includes reporting requirements for data breaches. These Model Laws are typically enforced by state insurance regulators.
It is possible that applicable laws may be interpreted and applied in a manner that is inconsistent with our practices and our efforts to comply with the evolving data protection rules may be unsuccessful. We must devote significant resources to understanding and complying with this changing landscape. Failure to comply with laws regarding privacy and security of PHI and other PII could expose us to penalties under such laws. Any such failure to comply with data protection and privacy laws could result in government-imposed fines or orders requiring that we change our practices, claims for damages or other liabilities, regulatory investigations and enforcement action, litigation and significant costs for remediation, any of which could adversely affect our business. Even if we are not determined to have violated these laws, government investigations into these issues typically require the expenditure of significant resources and generate negative publicity, which could have an adverse effect on our business, financial condition and results of operations.
22
As indicated above, there are numerous federal and state laws and regulations addressing patient and consumer privacy concerns, including notification requirements in the event of unauthorized access or theft of personal information. State statutes and regulations vary from state to state and could impose penalties. Substantially all of our relevant member data is maintained on our technology platform, AVA, which aggregates and provides us with access to extensive member datasets, including individually identifiable PHI. As a result, violations of HIPAA or applicable federal or state laws or regulations could subject us to significant criminal or civil penalties, including significant monetary penalties. Compliance with HIPAA and other privacy regulations requires significant and ongoing systems enhancements, training and administrative effort. See “Risk Factors—Security breaches, loss of data and other disruptions could compromise sensitive information related to our business or our members, or prevent us from accessing critical information and expose us to liability, which could adversely affect our business and our reputation.”
Our business and operations may also be subject to federal, state, and local consumer protection laws governing marketing communications, including the Telephone Consumer Protection Act (“TCPA”), which places restrictions on the use of automated tools and technologies to communicate with wireless telephone subscribers or communications services consumers generally and the CAN-SPAM Act, which regulates the transmission of marketing emails. In addition, certain of our businesses are also subject to the Payment Card Industry Data Security Standard (“PCI DSS”), which is a multifaceted security standard that is designed to protect credit card account data as mandated by payment brands and acquiring banks.
The Health Care Reform Law and Other Current or Future Legislative, Judicial or Regulatory Changes
The Patient Protection and Affordable Care Act and The Health Care and Education Reconciliation Act of 2010 (which we collectively refer to as the “Health Care Reform Law”) enacted significant reforms to various aspects of the U.S. health insurance industry. Certain significant provisions of the Health Care Reform Law include, among others, mandated coverage requirements, mandated benefits and guarantee issuance associated with commercial medical insurance, rebates to policyholders based on minimum benefit ratios, adjustments to Medicare Advantage premiums, the establishment of federally facilitated or state-based exchanges coupled with programs designed to spread risk among insurers, and the introduction of plan designs based on set actuarial values. Some of these changes impact us and other entities that offer Medicare Advantage plans. In addition, the Health Care Reform Law established insurance industry assessments, including an annual health insurance industry fee. In 2018, the fee levied on the health insurance industry was $14.3 billion. The health industry fee was permanently repealed beginning in calendar year 2021.
Corporate Practice of Medicine and Other Laws
As a corporate entity, we are not licensed to practice medicine. Many states in which we operate through our subsidiaries limit the practice of medicine to licensed individuals or professional organizations comprised of licensed individuals, and business corporations generally may not exercise control over the medical decisions of physicians. Statutes, regulations and court decisions relating to the practice of medicine, fee-splitting between physicians and referral sources, and similar issues vary widely from state to state. Under management agreements between certain of our subsidiaries and associated physician-owned professional groups, these groups retain sole responsibility for all medical decisions, as well as for hiring and managing physicians and other licensed healthcare providers, developing operating policies and procedures, implementing professional standards and controls, and maintaining malpractice insurance.
We, our in-house and externally engaged physicians and the facilities in which they operate are subject to various federal, state and local licensing and certification laws and regulations and accreditation standards and other laws, relating to, among other things, the adequacy of medical care, equipment, privacy of member information, physician relationships, personnel and operating policies and procedures. Failure to comply with these licensing, certification and accreditation laws, regulations and standards could result in prior payments being subject to recoupment, requirements to make significant changes to our operations and can give rise to civil or, in extreme cases, criminal penalties. We routinely take the steps we believe are necessary to retain or obtain all requisite licensure and operating authorities.
In markets where the corporate practice of medicine is prohibited, we have historically operated by maintaining long-term management and administrative services contracts with multiple associated professional medical entities that are wholly owned or primarily owned by physicians employed by us and, in turn, employ or contract with physicians to provide those professional medical services required by our members. Under these management agreements, Alignment Healthcare USA, LLC performs only non-medical administrative services, does not represent that it offers medical services and does not exercise influence or control over the practice of medicine by the physicians or the associated physician groups. In addition to the above management arrangements, we have certain contractual rights relating to the orderly transfer of equity interests in our physician practices through succession agreements and other arrangements with their physician equity holders. Such equity interests cannot, however, be transferred to or held by us or by any non-professional medical corporation. Accordingly, neither we nor our direct subsidiaries directly own any equity interests in any of our physician practices.
23
Anti-Kickback, Physician Self-Referral and Other Fraud and Abuse Laws
A federal law commonly referred to as the “Anti-Kickback Statute” prohibits the offer, payment, solicitation, or receipt of any form of remuneration to induce, or in return for, the referral of Medicare or other governmental health program patients or patient care opportunities, or in return for the purchase, lease or order of items or services that are covered by Medicare or other federal governmental health programs. Because the prohibitions contained in the Anti-Kickback Statute apply to the furnishing of items or services for which payment is made in “whole or in part,” the Anti-Kickback Statute could be implicated if any portion of an item or service we provide is covered by any of the state or federal health benefit programs described above. Violation of these provisions constitutes a felony criminal offense and applicable sanctions could include exclusion from the Medicare and Medicaid programs.
Section 1877 of the Social Security Act, commonly known as the “Stark Law,” prohibits physicians, subject to certain exceptions described below, from referring Medicare or Medicaid patients to an entity providing “designated health services” in which the physician, or an immediate family member, has an ownership or investment interest or with which the physician, or an immediate family member, has entered into a compensation arrangement. These prohibitions, contained in the Omnibus Budget Reconciliation Act of 1993, commonly known as “Stark II,” amended prior federal physician self-referral legislation known as “Stark I” by expanding the list of designated health services to a total of 11 categories. The professional groups with which we are contracted or affiliated provide one or more of these designated health services. Persons or entities found to be in violation of the Stark Law are subject to denial of payment for services furnished pursuant to an improper referral, civil monetary penalties, and exclusion from the Medicare and Medicaid programs.
A federal law commonly referred to as the “False Claims Act” prohibits the submission of a false or fraudulent claim to the government for payment or approval. Qui tam relators and/or the government may take the position that we submit certain data or information that could form the basis of a claim for payment, thus subjecting us to allegations under the False Claims Act. In such events, we could be subject to treble damages and per-claim penalties.
Many states also have enacted laws similar in scope and purpose to the Anti-Kickback Statute and, in more limited instances, the Stark Law, that are not limited to services for which Medicare or Medicaid payment is made. In addition, most states have statutes, regulations, or professional codes that restrict a physician from accepting various kinds of remuneration in exchange for making referrals. These laws vary from state to state and have seldom been interpreted by the courts or regulatory agencies. In states that have enacted these statutes, we believe that regulatory authorities and state courts interpreting these statutes may regard federal law under the Anti-Kickback Statute and the Stark Law as persuasive.
State Regulation of Insurance-Related Products
Laws in each of the states in which we operate our business license and regulate entities that offer health plans to residents of that state. The products we offer are sold under licenses issued by the applicable insurance regulators. However, for entities offering Medicare Advantage plans, federal law preempts all state laws and regulations except those relating to licensing and financial solvency.
Certain of our licensed insurance subsidiaries are also subject to regulation under state insurance holding company regulations. These regulations generally require, among other things, prior approval and/or notice of new products, rates, benefit changes, and certain material transactions, including dividend payments, purchases or sales of assets, intercompany agreements, and the filing of various financial and operational reports. The amount of dividends that may be paid to us by these insurance subsidiaries, without prior approval by state regulatory authorities, or ordinary dividends, is limited based on the entity’s level of statutory income and statutory capital and surplus. Actual dividends paid may vary due to consideration of excess statutory capital and surplus and expected future surplus requirements. We continue to maintain our levels of aggregate excess statutory capital and surplus in our state-regulated operating subsidiaries. Dividends from our non-insurance companies are generally not restricted by departments of insurance.
Intellectual Property
We believe that our intellectual property rights are valuable and critical to our business stability and growth. We rely on a combination of trademarks, copyrights, trade secrets, know-how license agreements and confidentiality procedures, non-disclosure agreements, employee disclosure and invention assignment agreements and other contractual rights to establish and protect our proprietary rights.
We do not have any issued patents and we are not currently pursuing any patent applications, including with respect to our AVA platform.
We intend to pursue additional intellectual property protection to the extent we believe it would be beneficial and cost effective.
24
Competition
The U.S. healthcare insurance industry is highly competitive. Our competitors vary by local market and include other managed care companies, national insurance companies, HMOs and PPOs. Many of our competitors have a larger membership base and/or greater financial resources than we do. In addition, other companies may enter our markets in the future, including emerging competitors in the Medicare Advantage program or competitors in the delivery of healthcare services. We believe that barriers to entry in our markets are not substantial, so the addition of new competitors can occur relatively easily, and customers enjoy significant flexibility in moving between competitors. Contracts for the sale of our products are generally tied to an annual bidding process with CMS. While health plans compete on the basis of many factors, including service and the quality and depth of provider networks, we expect that price and Star ratings will continue to be significant bases of competition. In addition to the challenge of controlling healthcare costs, we face intense competitive pressure to contain premium prices. Factors such as business consolidations, strategic alliances, legislative reform and marketing practices create pressure to contain premium price increases, despite being faced with increasing medical costs. The primary competitive factors for our industry include, but are not limited to, the following:
Employees and Human Capital Resources
We are focused on building a company that is transforming health care by putting seniors first with our on-demand care, and our employees are critical to our success. Our Human Capital strategy focuses on meeting business objectives by attracting, developing, engaging, and retaining a high-performing, diverse workforce. As of December 31, 2021, we had 847 full-time employees in addition to seasonal employees who assist with the Medicare AEP.
We believe that an engaged, innovative, and productive workforce is essential to supporting our company’s mission of changing healthcare one person at a time, as well as our values of putting our members first, supporting our physicians, applying technology to advance care, and having a serving heart. Each year, we conduct an employee survey that enables our leaders to develop action plans to further enhance employee engagement and productivity.
We recognize that Diversity, Equity, and Inclusion (“DEI”) is crucial as we scale and build our high-performing team. Our DEI strategy will be embedded in each aspect of our processes, programs, and structures that drive our talent lifecycle: attraction, recruitment, onboarding, development, and retention efforts. Our efforts to recruit for excellence are reflected in the composition of our current employee workforce and Board of Directors, which are comprised of a diverse group of highly qualified individuals that represent top talent in the industry. As of December 31, 2021, our workforce was made up of 68% female employees and 67% racially or ethnically diverse employees and our Board of Directors consisted of 36% female directors and 18% racially or ethnically diverse directors.
The future success of our company will depend, in part, on our continued ability to attract, develop and retain the best talent as we grow and scale the organization. Our talent acquisition and management strategies are designed to ensure that we create and develop a pipeline of outstanding physicians, clinical employees, and business leaders. A key component of our corporate sustainability and success is learning and development. We are intentional in our efforts to provide all employees opportunities to grow. Our training and development programs for employees focus on enhancing and developing talent within the company. All of our employees can access the training of their choice on-demand through our learning and development platform. We are currently designing additional training programs and resources for both new hires and longer-tenured employees.
25
Our compensation and incentive plans are designed to attract, retain, and reward employees by granting cash-based performance and stock-based awards. By motivating individuals to achieve business objectives and perform to the best of their abilities, they support the success of the company and the increase of stockholder value. We also provide comprehensive medical benefits, a positive work/life balance, generous paid time off, health and wellness programs, and learning and development opportunities. We regularly evaluate each aspect of compensation and benefits to ensure they align with the market and our peers.
We value the safety of our employees and have created a largely remote-work environment during the pandemic. We plan to implement a hybrid-remote workforce strategy to enhance our ability to attract the best talent nationally as we grow and continue to provide our employees with a healthy work-life balance.
Our board of directors believes that human capital management is an essential component of our continued growth and success. Management regularly reports to our board for input on important decisions related to human capital, including corporate culture, safety, compliance, talent management, organizational development, compensation, and benefits.
Corporate Information
We were originally formed as a Delaware limited liability company under the name Alignment Healthcare Holdings, LLC in 2013. In March 2021, we completed the Corporate Conversion and Corporate Reorganization and changed our name to Alignment Healthcare, Inc. During the same month, we completed our initial public offering and our common stock began trading on the Nasdaq Global Select Market under the symbol “ALHC.”
Our principal executive office is located at 1100 W. Town & Country Rd., Suite 1600, Orange, CA 92868 and our phone number is (844) 310-2247. Our website address is www.alignmenthealthcare.com. The information contained on, or that can be accessed through, our website is not incorporated by reference into this filing and you should not consider any information contained on, or that can be accessed through, our website as part of this filing. We are a holding company and all of our business operations are conducted through our subsidiaries and affiliated medical groups.
Our annual reports on Form 10-K, quarterly reports on Form 10-Q, current reports on Form 8-K and, if applicable, amendments to those reports filed or furnished pursuant to Section 13(a) of the Securities Exchange Act of 1934, as amended (the "Exchange Act"), are available free of charge on or through our website, http://www.alignmenthealthcare.com, as soon as reasonably practicable after we electronically file such material with, or furnish it to, the Securities and Exchange Commission, or the SEC. The SEC’s website, http://www.sec.gov, contains reports, proxy and information statements, and other information regarding issuers that file electronically with the SEC.
26
Item 1A. Risk Factors.
Our business involves a high degree of risk. You should carefully consider the risks and uncertainties described below, together with all of the other information contained in this Annual Report on Form 10-K, including our consolidated financial statements and the related notes thereto, before making a decision to invest in our common stock. The risks and uncertainties described below are not the only ones we face. Additional risks and uncertainties that we are unaware of, or that we currently believe are not material, may also become important factors that affect us. If any of the following risks occur, our business, financial condition, operating results and prospectus could be materially and adversely affected. In that event, the price of our common stock could decline, and you could lose all or part of your investment.
Risk Factors Summary
The following are the principal risks that are applicable to our business and the shares of our common stock. Such risks are discussed in more detail below, and you should read this Risk Factors section in its entirety before deciding whether to invest in our common stock.
27
Risks Related to Our Business
We have a history of net losses, we anticipate increasing expenses in the future, and we may not be able to achieve or maintain profitability.
28
We have incurred net losses on an annual basis since our inception, including a net loss of $195.3 million and $22.9 million for the years ended December 31, 2021 and December 31, 2020. As of December 31, 2021, we had an accumulated deficit of $574.9 million. We expect our aggregate costs will increase substantially in the foreseeable future as we expect to invest heavily in increasing our member base, growing our provider networks, expanding our operations geographically, engaging in expanded marketing and outreach efforts, enhancing our technology, hiring additional employees, operating as a public company and acquiring companies or assets complementary to our business. These efforts may prove more expensive than we currently anticipate, and we may not succeed in increasing our revenue sufficiently to offset these higher expenses. In addition, even if we are successful in increasing our membership and consequently increasing our total revenues from premiums earned, we may not successfully and effectively predict, price and manage the medical costs of our members. To date, we have financed our operations principally from the sale of our equity, revenue from the CMS and the incurrence of indebtedness. We may not generate positive cash flow from operations or profitability in the future.
We have encountered and will continue to encounter risks and difficulties frequently experienced by growing companies in rapidly changing industries, including increasing expenses as we continue to grow our business. In addition to the expected costs to grow our business, we also expect to incur additional legal, accounting and other expenses as a newly public company. Moreover, the investments we intend to make into growing our company may be more costly than we expect, and if we do not achieve the benefits anticipated from these investments, or if the realization of these benefits is delayed, they may not result in increased revenue or growth in our business. If our growth rate were to decline significantly or become negative, it could adversely affect our financial condition and results of operations. Furthermore, even if we achieve profitability in the future, we may not be able to sustain profitability in subsequent periods. If we are not able to maintain positive cash flow in the long term, we may require additional financing, which may not be available on favorable terms or at all and/or which would be dilutive to our stockholders. If we are unable to successfully address these risks and challenges as we encounter them, our business, results of operations and financial condition would be adversely affected. Our failure to achieve or maintain profitability could negatively impact the value of our common stock.
A pandemic, epidemic or outbreak of an infectious disease in the United States or worldwide, including the outbreak of the novel strain of coronavirus disease, COVID-19, could adversely affect our business.
If a pandemic, epidemic or outbreak of an infectious disease occurs in the United States or worldwide, our business may be adversely affected. The severity, magnitude and duration of the current COVID-19 pandemic is uncertain and rapidly changing. As of the date of this filing, the extent to which the COVID-19 pandemic may impact our business, results of operations and financial condition remains uncertain. Furthermore, because of our business model, the full impact of the COVID-19 pandemic may not be fully reflected in our results of operations and overall financial condition until future periods.
Adverse market conditions resulting from the spread of COVID-19 could materially adversely affect our business and the value of our common stock. Numerous state and local jurisdictions, including all markets where we operate, previously imposed, and others in the future may impose, “shelter-in-place” orders, quarantines, executive orders and similar government orders and restrictions for their residents to control the spread of COVID-19. Such orders or restrictions resulted in largely remote operations at our facilities, work stoppages or slowdowns among some clinical service providers, vendors and suppliers, travel restrictions and cancellation of events and restricted the ability of our members to obtain in-person medical care, among other effects, thereby adversely impacting our operations.
Other disruptions or potential disruptions include restrictions on the ability of our personnel to travel, delays in actions of regulatory bodies; diversion of or limitations on employee resources that would otherwise be focused on the operations of our business, including because of sickness of employees or their families or the desire of employees to avoid contact with groups of people; business adjustments or disruptions of certain third parties; and additional government requirements or other incremental mitigation efforts. The extent to which the COVID-19 pandemic impacts our business will depend on future developments, which are highly uncertain and cannot be predicted, including new information which may emerge concerning the severity and spread of COVID-19 and the actions to contain COVID-19 or treat its impact, among others. In addition, the COVID-19 virus disproportionately impacts our member base of seniors, especially those with chronic illnesses.
It is not currently possible to reliably project the direct impact of COVID-19 on our operating revenues and expenses. Key factors include the duration and extent of the outbreak in the markets in which we operate as well as societal and governmental responses. Members may continue to be reluctant to seek necessary care given the risks of the COVID-19 pandemic. This could have the effect of deferring healthcare expenses that we will need to incur to later periods and may also affect the longer-term health of members who defer preventative care or treatment, which may cause our costs to increase in the future. Additionally, as a result of the COVID-19 pandemic, we may experience slowed growth or a decline in our ability to market to potential members. We also may experience increased internal and third-party medical costs as we provide care, benefits and treatment coverage for members suffering from COVID-19. Beginning in the fourth quarter of 2020 and at certain times throughout 2021, we experienced increases in membership hospitalizations due to COVID-19. A sustained increase in membership hospitalizations due to COVID-19 could materially adversely impact our business, results of operations, and overall financial condition in future periods.
29
In response to the COVID-19 pandemic, we temporarily closed our corporate offices, and enabled most of our corporate work force to work remotely. As of December 31, 2021, we continued to maintain a reduced presence in our corporate offices. Beginning at the start of the pandemic, we also reduced staff at our clinics to minimize potential exposure to COVID-19. We have also implemented travel restrictions for non-essential business. If the COVID-19 pandemic worsens, especially in regions where we operate, our business activities originating from affected areas could be adversely affected. Disruptive activities could include business closures in impacted areas, further restrictions on our employees’ and service providers’ ability to travel, impacts to productivity if our employees or their family members experience health issues, and potential delays in hiring and onboarding of new employees. We may take further actions that alter our business operations as may be required by local, state, or federal authorities or that we determine are in the best interests of our employees. Such measures could negatively affect our sales and marketing efforts, sales cycles, employee productivity, or member retention, any of which could harm our financial condition and business operations.
Due to the COVID-19 pandemic, we and the providers in our networks have experienced increased challenges in documenting the health conditions of our members as completely or effectively as in the past. Medicare makes capitation payments using a “risk adjustment model,” which compensates plans based on the health status (acuity) of each individual member. Payors with higher acuity members receive more, and those with lower acuity members receive less, and we have corresponding arrangements with certain healthcare providers. Medicare requires that a patient’s health issues be documented annually regardless of the permanence of the underlying causes. Historically, this documentation was required to be completed during an in-person visit with a patient. As part of the Coronavirus Aid, Relief and Economic Security Act (the “CARES Act”), Medicare is allowing documentation for conditions identified during video visits with patients. However, given the disruption caused by COVID-19, it is unclear whether we and the providers in our networks will be able to document the health conditions of our members as comprehensively as we did prior to the pandemic, which may adversely impact our revenue in future periods. Such challenges, together with lower Medicare Risk Adjustment Factor (“RAF”) scores among new members due to COVID-19, had an adverse impact on per-member revenue in 2021 and may also impact future years.
The extent and continued impact of the COVID-19 pandemic on our business will depend on certain developments, including: the duration of the outbreak; the emergence of new variants and their infectiousness and severity; government responses to the pandemic; the impact on our members and our sales cycles; and the effect on our partners and our and their supply chains, all of which are uncertain and cannot be predicted. Because of our business model, the full impact of the COVID-19 pandemic may not be fully reflected in our results of operations and overall financial condition until future periods.
To the extent the COVID-19 pandemic adversely affects our business and financial results, it may also have the effect of heightening many of the other risks described in this “Risk Factors” section, including but not limited to those relating to cyber-attacks and security vulnerabilities, interruptions or delays due to third-parties, or our ability to raise additional capital or generate sufficient cash flows necessary to fulfill our obligations under our existing indebtedness or to expand our operations.
Our relatively limited operating history makes it difficult to evaluate our current business and future prospects and increases the risk of your investment.
Our relatively limited operating history makes it difficult to evaluate our current business and prospectus and plan for our future growth. We were founded in 2013, with most of our growth occurring in recent years. We have encountered and will continue to encounter significant risks and uncertainties frequently experienced by new and growing companies in heavily regulated and rapidly changing industries, such as determining appropriate investments for our limited resources, scaling our model and technology platform, attracting and retaining members, efficiently navigating and complying with evolving regulations, hiring, integrating, training and retaining skilled personnel, identifying and reaching agreements with reliable healthcare service providers, competing against more established competitors, unforeseen expenses and challenges in forecasting accuracy. Although we have successfully expanded our footprint outside of California and intend to continue to expand into new markets, new plans we provide or new markets we enter may not prove successful. If we are unable to increase our member enrollment, scale our platform, maintain a low cost structure, identify and reach agreements with reliable healthcare service providers, successfully manage our third-party medical costs or successfully expand the range of services and benefits we offer to members, our revenue and our ability to achieve and sustain profitability would be impaired. Additional risks include our ability to effectively manage growth, process, store, protect and use personal data in compliance with governmental regulation, contractual obligations and other legal obligations related to privacy and security and manage our obligations as a healthcare plan. If our assumptions regarding these and other similar risks and uncertainties, which we use to plan our business, are incorrect or change as we gain more experience operating our business or due to changes in our industry, or if we do not address these challenges successfully, our operating and financial results could differ materially from our expectations and our business could suffer.
Our growth strategy may not prove viable and we may not realize expected results.
Our business strategy is to grow rapidly by expanding our service offerings through an array of non-traditional benefits and continuing to build out and attract network relationships in our existing markets. We also intend to expand into new markets,
30
leveraging our AVA technology platform, which has been designed to scale and allow us to provide a predictable and replicable member experience across new markets. Our strategy hinges on our ability to satisfy our members in our existing markets, submit successful bids to CMS in new markets, attract new members, form alliances with primary care providers, and hire physicians, nurses and other medical support staff for our in-house care delivery programs. We also seek growth opportunities through strategic acquisitions and vertical integration. We cannot guarantee that we will be successful in pursuing our growth strategy. If we fail to evaluate and execute new business opportunities properly, we may not achieve anticipated benefits and may incur increased costs.
Our growth strategy involves a number of risks and uncertainties, including that:
Pursuing our growth strategy requires significant capital expenditures, the allocation of valuable management resources, and the hiring of additional personnel, and may strain our operations, and our financial and management controls and reporting systems and procedures. For a variety of reasons, we may not succeed in achieving scale, improving our operating efficiency or gaining operating leverage. Moreover, we have experienced and may in the future continue to experience attrition, which may further exacerbate these challenges. If we are unable to effectively execute our growth strategy and manage our growth, our results of operations and financial condition could be materially and adversely affected.
If we are unable to attract new members, our revenue growth will be adversely affected.
We currently derive substantially all of our revenue from CMS contracts related to our Medicare Advantage health plans. To increase our revenue, our business strategy is to grow organically by expanding the number of members under our plans in the markets in which we currently operate and in the new markets that we intend to enter. In order to support such growth, we must continue to enroll and retain a sufficient number of new members. We have experienced significant member growth since we commenced operations; however, we may not be able to maintain this growth, and our member base could decrease rapidly or shrink over time. Even if we are successful in achieving and maintaining growth, doing so may be more costly than we anticipate, and if we are not able to manage our costs, our results could be materially adversely affected.
We are focused on the Medicare-eligible population and face competition from other plans in the enrollment of Medicare-eligible potential members. If we are unable to obtain CMS contracts in new markets and convince the Medicare-eligible population of the benefits of our plans, or if potential or existing members prefer a plan offered by one of our competitors, we may not be able to effectively implement our growth strategy. Our ability to attract new members will depend on a variety of factors, including the following:
31
In addition, our growth strategy is partially dependent on beneficiaries electing to move from fee-for-service to one of our Medicare Advantage plans, or electing to move from their current Medicare Advantage plan, and selecting us as their Medicare Advantage plan. In some instances, original Medicare or other insurers’ MA plans may be more attractive to a consumer than our MA plans. For example, though our PPO members are enrolled in plans that enable them to visit any doctor participating in Medicare who will see them, our HMO plans have restrictions on the network of doctors that HMO members can see, and in some markets other providers participating in Medicare may choose to see no MA members or only MA members participating in specific plans. It is also possible that original Medicare or other insurers’ MA plans may offer broader physician networks in particular markets or highly competitive benefits, in which case those plans may be more attractive to some consumers than our MA plans. When the time to choose an MA plan comes, Medicare-eligible consumers may also choose to continue with their current insurer which was offered by their employer instead of transitioning to one of our plans.
For a majority of individuals, plan enrollment selections for Medicare Advantage are made during an annual enrollment period from October into December of each year; therefore, our ability to grow our member population is dependent in part on our ability to successfully enroll members during the annual enrollment period and to convince such individuals not to subsequently change that election. If our ability to market and sell our MA plans is constrained during an enrollment period for any reason, such as technology failures, reduced allocation of resources, any inability to timely employ, license, train, certify and retain employees and contractors and agents to sell plans, interruptions in the operation of our website or systems, or disruptions caused by other external factors, such as the COVID-19 pandemic, we could acquire fewer new members than expected or suffer a reduction in the number of our existing members.
Our inability to enroll new members and retain existing members would harm our ability to execute our growth strategy and may have a material adverse effect on our business operations and financial position.
If we do not design and price our products properly and competitively, if we are unable to develop new products and implement clinical initiatives to provide a better healthcare experience for our members, lower costs, and appropriately document the risk profile of our members, or if our estimates of benefits expense are inadequate, our profitability may be materially adversely affected.
We use a substantial portion of our revenues to pay the costs of healthcare services delivered to our members by third party providers. These costs include claims payments, capitation payments to providers (predetermined amounts paid to cover services), administrative costs and various other costs incurred to provide health insurance coverage to our members. These costs also include estimates of future payments to hospitals and other providers for medical care provided to our members. Generally, premiums in the healthcare business are fixed for one-year periods and we are required by federal law to spend a fixed amount of these premiums on healthcare services, covered benefits and quality improvement efforts. Accordingly, costs we incur in excess of our benefit cost projections generally are not recovered in the contract year through higher premiums and our ability to enhance the profitability of our plans depends in significant part on our ability to estimate the costs of our future benefit claims and other expenses. We make these estimates using actuarial methods and assumptions based upon claim payment patterns, medical inflation, historical developments, including claim inventory levels and claim receipt patterns, and other relevant factors. We also record benefits payable for future payments. We continually review estimates of future payments relating to benefit claims costs for services incurred in the current and prior periods and make necessary adjustments to our reserves, including premium deficiency reserves where appropriate. However, these estimates involve extensive judgment, and have considerable inherent variability that is sensitive to claim payment patterns and medical cost trends. Many factors may and often do cause actual healthcare costs to exceed what was estimated and used to set our premiums. These factors may include:
32
Key to our operational strategy is the implementation of clinical initiatives that we believe provide a better healthcare experience for our members, lower the cost of healthcare services delivered to our members, and appropriately document the risk profile of our members. Our profitability and competitiveness depend in large part on our ability to leverage our technology platform, AVA, to optimize and appropriately manage healthcare costs by, among other things, proactively managing member care.
Increases or decreases in staff and provider-related expenses, any costs associated with exiting products, additional investment in new products and in the expansion of clinical and technological capabilities as part of our integrated care delivery model, investments in health and well-being product offerings, acquisitions, new taxes and assessments, and implementation of regulatory requirements may increase our operating expenses. Any failure to adequately price our products or estimate sufficient benefits payable or effectively manage our operating expenses may result in a material adverse effect on our results of operations, financial position, and cash flows.
Premium increases, introduction of new product designs, and our relationships with our providers in various markets, among other issues, could also affect our membership levels. Other actions that could affect membership levels include our possible exit from or entrance into markets, or the termination of a large contract.
If we do not compete effectively in our markets, if we set rates too high or too low in highly competitive markets to keep or increase our market share, if membership does not increase as we expect, if membership declines, or if we lose membership with favorable medical cost experience while retaining or increasing membership with unfavorable medical cost experience, our results of operations, financial position, and cash flows may be materially adversely affected.
We may not be successful in maintaining or improving our Star ratings in future years, which may have a direct and substantial adverse impact on our revenue.
CMS measures the quality of Medicare Advantage plans through a Five Star Quality Rating System. The Star Rating system considers various measures adopted by CMS, including, among others, quality of care, preventative services, chronic illness management and member satisfaction. The achievement of Star ratings of 4-Star or higher qualifies Medicare Advantage plans for premium bonuses. The overall Star rating of our plans is 4.0 for the 2022 rating year / 2023 payment year. However, we may not be able to maintain or improve upon this Star rating in future years. Failure to maintain satisfactory quality and performance measures may negatively affect our premium rates, subject us to penalties, limit or reduce our membership, impede our ability to compete for new business in existing or new markets or result in the termination of our contracts, or affect our ability to establish new health plans or expand current health plans.
Various factors may make it difficult for us to maintain or increase our Star rating. For example, given that there are multiple providers that serve our plans, we may have limited ability to influence the overall quality rating of our plans. Additionally, our higher concentration of minority members and members residing in socioeconomically disadvantaged neighborhoods generally may make it more difficult for us to achieve and maintain high Star Ratings as compared to our competitors, given the well-documented health disparities among different minority and socioeconomic groups.
33
CMS updates and makes changes to the Star ratings annually. Changes implemented by CMS with respect to the Five Star Quality Rating System have, in the past, and could, in the future, negatively impact our Star ratings. For example, in 2020, unanticipated changes to the Star rating calculation methodology implemented by CMS in response to the COVID-19 pandemic resulted in a reduction in our Star rating that we believe may have been avoided had COVID-19 and CMS’s policy changes not occurred. Due to the impact of the COVID-19 pandemic and its effect on the ability of Medicare Advantage organizations to gather and submit data, CMS elected to revise the methodology and the measurement data for the 2021 rating year / 2022 payment year Star ratings. Among other changes, CMS adjusted the data used to calculate performance on measures based in Healthcare Effectiveness Data and Information Set data (“HEDIS data”) and Consumer Assessment of Healthcare Providers and Systems data (“CAHPS data”). We believe this adjusted measurement approach had a negative impact on our Star ratings.
In addition, audits of our performance for past or future periods may result in downgrades to our Star ratings. Accordingly, our plans may not be eligible for full level quality bonus payments, which could adversely affect the benefits we can offer, reduce membership and/or reduce profit margins. Low Star ratings may also reduce our membership, if members choose to enroll in higher-rated plans. Also, CMS has the authority to terminate plans that have had a rating of less than three Stars for three consecutive years, whereas Medicare Advantage plans with five Stars are permitted to conduct enrollment throughout almost the entire year. Because low quality ratings can potentially lead to the termination of one or more of our plans, we may not be able to prevent the potential termination of a plan or a shift of members to other plans based upon quality issues, which could, in turn, have a material adverse effect on our business, results of operations, financial condition and cash flows.
If we fail to develop and maintain satisfactory relationships with care providers to service our members, our business may be adversely affected.
Our success requires that we maintain and grow our provider networks and contract with providers and medical facilities in new markets in order to meet CMS requirements relating to network adequacy. We contract with a variety of physicians, nurses, hospitals, clinics and other third-party providers to deliver healthcare and related services to our members. Our plans encourage or require our customers to use these contracted providers. A key component of our integrated care delivery strategy is to increase the number of providers who share medical cost risk with us or have financial incentives to deliver high quality medical services in a cost-effective manner. In order to retain our members and attract additional membership, our provider networks, including those physicians participating in Medicare and willing to see our patients but with whom we have not contracted, must be not only adequate, but attractive, providing Medicare-eligible beneficiaries access to the providers and facilities that they want.
In any particular market, providers could refuse to contract with us, demand higher payments, or take other actions that could result in higher healthcare costs for us, less desirable outcomes for members or difficulty meeting regulatory or accreditation requirements, including network adequacy requirements. In some markets, certain providers, particularly hospitals, physician specialty groups, physician/hospital organizations, or multi-specialty physician groups, may have significant market positions and negotiating power. In addition, physician or practice management companies, which aggregate physician practices for administrative efficiency and marketing leverage, may compete with us in certain circumstances. If these providers refuse to contract with us, use their market position to negotiate unfavorable contracts with us or place us at a competitive disadvantage, or do not enter into contracts with us that encourage the delivery of quality medical services in a cost-effective manner, our ability to market products or to be profitable in those areas may be adversely affected.
In some situations, we have capitation contracts with individual or groups of primary care providers and specialists for an actuarially determined, fixed fee per month to provide a basket of required medical services to our members. The inability of providers to properly manage costs under these capitation arrangements could result in the financial instability of these providers and the termination of their relationship with us. In addition, payment or other disputes between a primary care provider and specialists with whom the primary care provider contracts could result in a disruption in the provision of services to our members or a reduction in the services available to our members. The financial instability or failure of a primary care provider to pay other providers for whom they have taken professional risk for services rendered could lead those other providers to demand payment from us even though we have made our regular fixed payments to the primary care provider. Providers with whom we contract may not properly manage the costs of services, maintain financial solvency or avoid disputes with other providers. Even if we contract with sufficient numbers of providers in our markets, we may be required, from time to time, to work with providers with whom we do not contract and who are not included in our networks. This can increase our medical costs, as there is no pre-negotiated rate that we pay the provider and no incentive for the provider to control costs.
34
Our ability to develop and maintain satisfactory relationships with providers and facilities may also be negatively impacted by factors not associated with us, such as changes in Medicare programs and other pressures on healthcare providers, including consolidation activity among hospitals, physician groups, and other healthcare providers. We may be unable to contract with new providers, facilities and other entities in our current markets or new markets in which we enter or renew any contracts we maintain with existing providers or facilities on favorable terms, if at all. If we are unable to enter into new contracts or maintain contracts with providers or facilities in certain markets, we may be unable to meet network adequacy requirements, which would prevent us from serving such markets and could have a material adverse effect on our business, financial condition and results of operations.
If we fail to manage our growth effectively, we may be unable to execute our business plan, maintain high levels of service and member satisfaction or adequately address competitive challenges.
We have experienced, and may continue to experience, rapid growth and organizational change, which has placed, and may continue to place, significant demands on our management and our operational and financial resources. Additionally, our organizational structure may become more complex as we improve our operational, financial and management controls, as well as our reporting systems and procedures. We may require significant capital expenditures and the allocation of valuable management resources to grow and change in these areas. We must rapidly scale our technology platform, effectively increase our headcount and expand our provider networks, and we must continue to effectively train and manage our employees and partners. We will be unable to manage our business effectively if we are unable to alleviate the strain on resources caused by growth in a timely and successful manner. If we fail to effectively manage our anticipated growth and change, the quality of our services may suffer, which could negatively affect our brand and reputation and harm our ability to attract and retain members and employees.
In addition, as we expand our business, it is important that we continue to maintain a high level of member service and satisfaction. As our member base continues to grow, we will need to expand our product and service offerings and our network of partners to provide personalized member service. If we are not able to continue to provide high quality products, benefits and medical care with high levels of member satisfaction, our reputation, as well as our business, results of operations and financial condition could be adversely affected.
The healthcare industry is highly competitive. There are many other healthcare plans and healthcare service providers, many of which have a longer operating history and substantially more resources, and there are few barriers to entry in the healthcare industry. This competition may have a material adverse effect on our business operations and financial position.
We compete directly with national, regional and local Medicare Advantage organizations for members and healthcare providers. Competition in our market involves rapidly changing technologies, evolving regulatory requirements and industry expectations, new product offerings and constantly evolving member and physician preferences and user requirements. We currently face competition from a range of companies, including other incumbent MA providers and health insurance companies. Many of the other companies currently providing health insurance coverage and healthcare services, particularly national insurers such as United Health, Aetna, Humana and Cigna, have been in business longer and/or have substantially more resources than we do. Other companies could enter the healthcare industry in the future and divert some or all of our business. We also face competition from traditional Medicare.
Our ability to compete successfully varies from location to location and depends on a number of factors, including the number of competing plans in the local market and the types of services available at local clinical facilities, the demographics of each market and our ability to generate offerings that meet the needs of that population, our local reputation for providing quality care to members, the commitment and expertise of the providers in our network and our in-house medical staff, our local service offerings and community programs and the cost of care in each locality. If we are unable to attract members, our revenue and profitability will be adversely affected. Some of our competitors may have greater recognition and may be more established in particular communities than we are, and may have greater financial and other resources than we have. Competing Medicare Advantage plans may also offer different programs or services than we do, which, combined with the foregoing factors, may result in our competitors being more attractive to our current members or potential members. While health plans compete on the basis of many factors, including service and the quality and depth of provider networks, we expect that price will continue to be a significant basis of competition. Furthermore, while we budget for improvements in our products and services to keep them competitive in their respective markets, to the extent that competitive forces cause related expenditures to increase in the future, our financial condition may be negatively affected. In addition, in certain instances our relationships with providers are not exclusive and our competitors have established or could seek to establish relationships with such providers. Additionally, as we expand into new geographies, we may encounter competitors with stronger relationships or recognition in the community in such new geography, which could give those competitors an advantage in retaining current members and obtaining new members, which may have a material adverse effect on our business operations and financial position.
Our failure to compete effectively may result in fewer plans being offered; a reduction in plan benefits; reduced services; a loss of existing members or inability to grow membership; fewer physician users; reduced revenues; lower gross margins; and loss of
35
market share. Any failure to meet and address these factors would harm our business, results of operations and financial condition.
We have entered into certain key contracts with large independent physician associations, hospitals and other provider networks to serve our membership base. The loss or renegotiation of any of these contracts could negatively impact our results.
Our provider network includes key contracts with certain large independent physician associations (“IPAs”), hospitals and other provider networks, which are critical to serving our membership base. Although we typically seek to enter into contracts spanning three or more years, after a specified period, certain of these contracts, including existing contracts with some of our largest IPA partners, hospitals or other providers, may terminate by their own terms or through notice of non-renewal. In the ordinary course of business, including in connection with renewals or extensions of these agreements, we engage in active discussions and renegotiations with these counterparties in respect of the solutions we provide and the terms of our agreements. The loss of any of our largest IPA partnerships, hospitals or other provider networks or the renegotiation of any of these contracts could adversely affect our results of operations, as this may alter the attractiveness of our provider network, result in more out-of-network claims costs and/or increase the payments we make to these counterparties.
Security breaches, loss of data and other disruptions could compromise sensitive information related to our business or our members, or prevent us from accessing critical information and expose us to liability, which could adversely affect our business and our reputation.
In the ordinary course of our business, we collect, store, process, transfer, disclose and otherwise use sensitive data, including protected health information (“PHI”), and other types of personal data or personally identifiable information (“PII”) relating to our employees, members and others. We also process and store, and use third-party service providers to process and store, substantial amounts of sensitive information, including intellectual property, confidential information and other proprietary business information. We manage and maintain such sensitive data and information utilizing a combination of on-site systems, managed data center systems and cloud-based computing center systems.
We are highly dependent on information technology networks and systems, including the internet, to securely process, transmit and store this sensitive data and information. Security breaches of this infrastructure, including physical or electronic break-ins, computer viruses, ransomware, attacks by hackers and other malicious actors and similar breaches, and employee or contractor error, negligence or malfeasance, can create system disruptions, shutdowns or unauthorized disclosure or modifications of such sensitive data or information, causing PHI or other PII to be accessed or acquired without authorization or to become publicly available. As our third-party service providers manage important aspects of the collection, storage, processing and transmission of employee, user and member information, and other confidential and sensitive information, we rely on them to perform functions that have material cybersecurity risks. Because of the sensitivity of the PHI, other PII and other sensitive information we and our service providers collect, store, transmit, and otherwise process and use, the security of our technology platform and other aspects of our services, including those provided or facilitated by our third-party service providers, are important to our operations and business strategy. Measures taken to protect our systems, those of our contractors or third-party service providers, or the PHI, other PII, or other sensitive information we or contractors or third-party service providers process or maintain (including our requirement that our third-party service providers enter into business associate agreements or other required security agreements, if applicable), may not adequately protect us from the risks associated with the collection, storage, processing and transmission of such sensitive data and information. For example, we may be required to expend significant capital and other resources, such as in the performance of ongoing risk assessments of our and our third-party service providers’ information systems, to protect against security breaches or to alleviate problems caused by security breaches. Because cyber-attacks are becoming more sophisticated and frequent and the techniques used to obtain unauthorized access or to sabotage systems change frequently and generally are not identified until they are launched against a target, despite the implementation of security measures, we or our third-party service providers may be unable to anticipate these techniques or to implement adequate protective measures.
A security breach or privacy violation that leads to disclosure or unauthorized use or modification of, or that prevents access to or otherwise impacts the confidentiality, security, or integrity of, member information, including PHI or other PII, or other sensitive information we or our contractors or third-party service providers maintain or otherwise process, could harm our reputation and brand, compel us to comply with breach notification laws, and cause us to incur significant costs for remediation, fines, penalties, providing notification to individuals. We would need to identify and implement measures intended to repair or replace systems or technology and to prevent future occurrences, and we could face potential increases in insurance premiums. This is of particular risk when considering tight integration with third-party service providers who manage or provide parts of our information systems. If we are unable to prevent or mitigate such security breaches or privacy violations or implement satisfactory remedial measures, or if it is perceived that we have been unable to do so, our operations could be disrupted, we may be unable to provide access to our systems, and we could suffer a loss of members. We may also suffer loss of reputation, adverse impacts on member and investor confidence and financial loss, and we would be exposed to the risk of governmental investigations or other actions, regulatory or contractual penalties, and other claims and liabilities, including liability under laws
36
and regulations that protect the privacy of member information or other personal information, such as the Health Insurance Portability and Accountability Act of 1996, as amended by the Health Information Technology for Economic and Clinical Health Act of 2009 (the “HITECH Act”), and their implementing regulations (collectively known as “HIPAA”). In addition, security breaches and other inappropriate access to, or acquisition or processing of, information can be difficult to detect, and any delay in identifying such incidents or in providing any notification of such incidents may lead to increased harm.
Any such breach or interruption of our systems or those of any of our third-party service providers could also compromise result in the compromise of our trade secrets and other proprietary information, which could adversely affect our business and competitive position. While we maintain insurance covering certain security and privacy damages and claim expenses, we may not carry insurance or maintain coverage sufficient to compensate for all liability and in any event, insurance coverage would not address the reputational damage that could result from a security incident.
Our service offering is driven by our core operating technology platform, AVA, allowing us to access and analyze comprehensive member data quickly, generating insights and alerts using such data and making recommendations to members and practitioners. AVA and the other systems or networks used in our business may experience an increase in attempted cyber-attacks, targeted intrusion, ransomware and phishing campaigns seeking to take advantage of shifts to employees and healthcare providers working remotely using their household or personal internet networks and to leverage fears promulgated by the COVID-19 pandemic.
A data breach could result in incorrect or delayed medical recommendations and prescriptions, missed alerts and missed opportunities to intervene for our members on a timely basis. Unauthorized access, loss or dissemination could also disrupt our operations, including our ability to perform our services, access member health information, collect, process, and prepare company financial information, provide information about our current and future services and engage in other member and clinician education and outreach efforts. Any of the foregoing could have a material adverse effect on our business, results of operations and financial condition.
Disruptions in our disaster recovery systems or management continuity planning could limit our ability to operate our business effectively and adequately care for our members.
Our information technology systems facilitate our ability to conduct our business. We rely on our core operating technology platform, AVA, to aggregate, organize and monitor health data, and to generate insights and recommendations to the care providers who serve our members. The functioning of our technology platform is critical to our ability to adequately care for our members and drive health outcomes. While we have disaster recovery systems and business continuity plans in place, any disruptions in our disaster recovery systems or the failure of these systems to operate as expected could, depending on the magnitude of the problem, adversely affect our operating results and the health of our members by limiting our capacity to effectively monitor and control our operations. Despite our implementation of a variety of security measures, our information technology systems could be subject to physical or electronic break-ins or disruptions from unauthorized tampering, fires, power loss, telecommunication failures or any weather-related disruptions where our headquarters is located or at locations that host portions of our technology platform. In addition, in the event that a significant number of our management personnel were unavailable in the event of a disaster, our ability to effectively conduct business and adequately care for our members could be adversely affected.
As a government contractor, we are exposed to risks that may materially adversely affect our business, including the potential loss of CMS contracts, potential suspension from participating in the Medicare Advantage program, changes to the risk-adjustment model used to determine the premiums paid to Medicare Advantage plans, changes to provisions for risk sharing under Medicare Part D and risks related to governmental audits and investigations, among others.
A significant portion of our revenue relates, directly or indirectly, to the Medicare Advantage program, which accounted for substantially all of our total revenue for the year ended December 31, 2021. Participating in the Medicare Advantage program exposes us to various risks, as described further below.
37
CMS has phased in a change in the process of calculating risk scores from the use of diagnoses data from the Risk Adjustment Processing System (“RAPS”), to diagnoses data from the Encounter Data System (“EDS”). The RAPS process requires Medicare Advantage organizations to apply a filter logic based on CMS guidelines and only submit diagnoses that satisfy those guidelines. For submissions through EDS, CMS requires Medicare Advantage organizations to submit all the encounter data and CMS will apply the risk adjustment filtering logic to determine the risk scores. The transition from RAPS to EDS was phased-in over several years, and CMS will rely solely on EDS submissions beginning in 2022. We will need to adjust our platform to account for this transition. The phase-in from RAPS to EDS could result in different risk scores from each dataset as a result of plan processing issues, CMS processing issues, or filtering logic differences between RAPS and EDS, and could have a material adverse effect on our results of operations, financial position, or cash flows.
CMS and the Office of the Inspector General of Health and Human Services (“HHS-OIG”), are continuing to perform audits of various companies’ selected Medicare Advantage contracts related to this risk adjustment diagnosis data. We refer to these audits as Risk-Adjustment Data Validation Audits (“RADV audits”). RADV audits review medical records in an attempt to validate provider medical record documentation and coding practices which influence the calculation of premium payments to Medicare Advantage organizations.
In 2012, CMS released a “Notice of Final Payment Error Calculation Methodology for Part C Medicare Advantage Risk Adjustment Data Validation (RADV) Contract-Level Audits.” The payment error calculation methodology provided that, in calculating the economic impact of audit results for a Medicare Advantage contract, if any, the results of the RADV audit sample would be extrapolated to the entire Medicare Advantage contract after a comparison of the audit results to a similar audit of the government’s traditional fee-for-service (“FFS”) Medicare program. We refer to the process of accounting for errors in fee-for-service claims as the “FFS Adjuster.” This comparison of RADV audit results to the FFS error rate is necessary to determine the economic impact, if any, of RADV audit results because the government used the
38
traditional fee-for-service Medicare program data set, including any attendant errors that are present in that data set, to estimate the costs of various health status conditions and to set the resulting adjustments to Medicare Advantage plans’ payment rates in order to establish actuarial equivalence in payment rates as required under the Medicare statute. CMS already makes other adjustments to payment rates based on a comparison of coding pattern differences between Medicare Advantage plans and traditional fee-for-service Medicare program data (such as for frequency of coding for certain diagnoses in Medicare Advantage plan data versus the traditional fee-for-service Medicare program dataset).
The final RADV extrapolation methodology, including the first application of extrapolated audit results to determine audit settlements, is expected to be applied to CMS RADV contract level audits conducted for contract year 2011 and subsequent years. CMS is currently conducting RADV contract level audits for certain of our Medicare Advantage plans.
On October 26, 2018, CMS issued a proposed rule and accompanying materials (the “Proposed Rule”) related to, among other things, the RADV audit methodology described above. If implemented, the Proposed Rule would use extrapolation in RADV audits applicable to payment year 2011 contract-level audits and all subsequent audits, without the application of an FFS Adjuster to audit findings. On October 21, 2021, CMS extended the standard three-year timeframe for finalizing the Proposed Rule until November 1, 2022. Whether, and to what extent, CMS finalizes the Proposed Rule, and any related regulatory, industry or company reactions, could have a material adverse effect on our results of operations, financial position, or cash flows.
In addition, as part of our internal compliance efforts, we routinely perform ordinary course reviews of our internal business processes related to, among other things, our risk coding and data submissions in connection with the risk-adjustment model. These reviews may also result in the identification of errors and the submission of corrections to CMS, that may, either individually or in the aggregate, be material. As such, the result of these reviews may have a material adverse effect on our results of operations, financial position, or cash flows. We will continue to work with CMS to ensure that Medicare Advantage plans are paid accurately and that payment model principles are in accordance with the requirements of the Social Security Act (“SSA”), which, if not implemented correctly could have a material adverse effect on our results of operations, financial position, or cash flows.
The premiums from CMS are subject to risk corridor provisions which compare costs targeted in our annual bids to actual prescription drug costs, limited to actual costs that would have been incurred under the standard coverage as defined by CMS. Variances exceeding certain thresholds may result in CMS making additional payments to us or require us to refund to CMS a portion of the premiums we received (known as a “risk corridor”). We estimate and recognize an adjustment to premiums revenue related to the risk corridor payment settlement based upon pharmacy claims experience. The estimate of the settlement associated with these risk corridor provisions requires
us to consider factors that may not be certain, including member eligibility differences with CMS.
Reinsurance and low-income cost subsidies represent payments from CMS in connection with the Medicare Part D program for which we assume no risk. Reinsurance subsidies represent payments for CMS’s portion of claims costs which exceed the member’s out-of-pocket threshold, or the catastrophic coverage level. Low-income cost subsidies represent payments from CMS for all or a portion of the deductible, the coinsurance and co-payment amounts above the out-of-pocket threshold for low-income beneficiaries. Monthly prospective payments from CMS for reinsurance and low-income cost subsidies are based on assumptions submitted with our annual bid. A reconciliation and settlement of CMS’s prospective subsidies against actual prescription drug costs we paid is made after the end of the applicable year.
Settlement of the reinsurance and low-income cost subsidies as well as the risk corridor payment is based on a reconciliation made approximately 9 months after the close of each calendar year. This reconciliation process requires us to submit claims data necessary for CMS to administer the program. Our claims data may not pass CMS’s claims edit processes due to various reasons, including discrepancies in eligibility or classification of low-income members. To the extent our data does not pass CMS’s claim edit processes, we may bear the risk for all or a portion of the claim which otherwise may have been subject to the risk corridor provision or payment which we would have otherwise received as a low-income subsidy or reinsurance claim. In addition, in the event the settlement represents an amount CMS owes us, there is a negative impact
39
on our cash flows and financial condition as a result of financing CMS’s share of the risk. The opposite is true in the event the settlement represents an amount we owe CMS.
We may be subject to legal proceedings and litigation, including intellectual property and privacy disputes, which are costly to defend and could materially harm our business and results of operations.
We may be party to lawsuits and legal proceedings in or outside of the normal course of business. These matters are often expensive and disruptive to normal business operations. We may face allegations, lawsuits and regulatory inquiries, audits and investigations regarding the denial of healthcare benefit payments, compensation or non-acceptance or termination of provider contracts, medical malpractice (based on our medical necessity decisions or brought against us on the theory that we are liable for providers’ alleged malpractice) or professional liability (in connection with the delivery of healthcare and related services to the public). We may also face qui tam allegations or lawsuits brought by individuals who seek to sue on behalf of the government including, among other allegations, resulting from coding and review practices under the Medicare Advantage risk-adjustment model.
We also may be subject to lawsuits under the FCA and comparable state laws for submitting allegedly fraudulent or otherwise inappropriate risk adjustment or Stars data. These lawsuits, which may be initiated by government authorities as well as private party relators, can involve significant monetary damages, fines, attorney fees and the award of bounties to private plaintiffs who successfully bring these suits, as well as to the government programs. In recent years, government oversight and law enforcement have become increasingly active and aggressive in investigating and taking legal action against potential fraud, waste and abuse. Fraud, waste, and abuse prohibitions encompass a wide range of activities, including kickbacks for referral of members, fraudulent coding practices, billing for unnecessary medical and/or other covered services, improper marketing and violations of patient privacy rights. The DOJ and the Department of Health and Human Services Office of Inspector General (“OIG”), have recently increased their scrutiny of healthcare payers and providers, and Medicare Advantage insurers, under the federal False Claims Act (“FCA”), in particular, and there have been a number of investigations, prosecutions, convictions and settlements in the healthcare industry. The FCA provides for treble damages and significant mandatory minimum penalties for each false claim or statement. Healthcare plans and providers thus often seek to resolve these types of allegations through settlement for significant and material amounts, including in circumstances where they do not acknowledge or admit liability, to avoid the uncertainty of treble damages that may be awarded in litigation proceedings. Such settlements often contain additional compliance and reporting requirements as part of a consent decree or settlement agreement, including, for example, corporate integrity agreements.
Additionally, we may face allegations, lawsuits and regulatory inquiries, audits and investigations regarding data privacy and security, labor and employment, consumer protection and intellectual property infringement, misappropriation or other violation, including claims related to patents, publicity, trademarks, copyrights and other intellectual property or proprietary rights. We may also face allegations or litigation related to our acquisitions, securities issuances or business practices, including public disclosures about our business.
40
Litigation and regulatory proceedings may be protracted and expensive, and the results are difficult to predict. Certain of these matters may include speculative claims for substantial or indeterminate amounts of damages and include claims for injunctive relief. Additionally, our litigation costs could be significant. Adverse outcomes with respect to litigation or any of these legal proceedings may result in significant settlement costs or judgments, penalties and fines, or require us to modify our services or require us to stop serving certain members or geographies, all of which could negatively impact our geographical expansion and revenue growth. We may also become subject to periodic audits, which would likely increase our regulatory compliance costs and may require us to change our business practices, which could negatively impact our revenue growth. Managing legal proceedings, litigation and audits, even if we achieve favorable outcomes, is time-consuming and diverts management’s attention from our business. Accordingly, such proceedings could harm our reputation, business, financial condition, results of operations and the market price of our common stock.
Although we maintain third-party professional liability insurance coverage and managed care errors and omissions policies, it is possible that claims against us may exceed the coverage limits of our insurance policies. Even if any professional liability loss is covered by an insurance policy, these policies typically have substantial deductibles for which we are responsible. Professional liability claims in excess of applicable insurance coverage could have a material adverse effect on our business, financial condition and results of operations. In addition, any professional liability claim brought against us, with or without merit, could result in an increase of our professional liability insurance premiums. Insurance coverage varies in cost and can be difficult to obtain, and we cannot guarantee that we will be able to obtain insurance coverage in the future on terms acceptable to us or at all. If our costs of insurance and claims increase, then our earnings could decline.
Our business may be adversely impacted if the healthcare services industry becomes more cyclical.
In the past, healthcare utilization generally has trended upward over time, regardless of minor fluctuations in the U.S. economy. We believe this trend may change, however, as consumers have been given more decision-making and spending responsibility. In turn, we believe members are making healthcare purchases on a more discretionary basis, especially for elective procedures. This could result in a more cyclical trend in healthcare utilization over the coming years and may cause short-term volatility in our operating results.
Any failure by us to manage acquisitions, divestitures and other significant transactions successfully may have a material adverse effect on our results of operations, financial position, and cash flows.
As part of our business strategy, we engage in discussions with third parties regarding possible investments, acquisitions, divestitures, strategic alliances, joint ventures, and outsourcing transactions and may enter into agreements relating to such transactions in order to further our business objectives. In order to pursue our acquisition strategy successfully, we must identify suitable candidates for and successfully complete transactions, some of which may be large and complex, and manage post-closing issues such as the integration of acquired companies or employees. Integration and other risks can be more pronounced for larger and more complicated transactions, transactions outside of our core business space, or if multiple transactions are pursued simultaneously. The failure to successfully integrate acquired entities and businesses or failure to produce results consistent with the financial model used in the analysis of our acquisitions, investments, joint ventures or strategic alliances may cause asset write-offs, restructuring costs or other expenses and may have a material adverse effect on our results of operations, financial position, and cash flows. If we fail to identify and successfully complete transactions that further our strategic objectives, we may be required to expend additional resources to expand our business organically.
If we are not able to maintain, enhance and protect our reputation and brand recognition, including through the maintenance and protection of trademarks, our business and results of operations will be harmed.
We believe that maintaining and enhancing our reputation and brand recognition is critical to our relationships with both members and providers and to our ability to attract new members. The promotion of our brand may require us to make substantial investments and we anticipate that, as our market becomes increasingly competitive, these marketing initiatives may become increasingly difficult and expensive. Moreover, our current marketing efforts to date have been limited to certain geographic regions and markets where our business operates to facilitate the efficient use of resources. If we grow nationally, we will need to spend additional resources to build strong national brand recognition and our efforts may not be effective. Our marketing activities may not be successful or yield increased revenue, and to the extent that these activities yield increased revenue, the increased revenue may not offset the expenses we incur and our results of operations could be harmed.
41
Any factor that diminishes our reputation or that of our management, including failing to meet the expectations of or provide quality medical care for our members, or any adverse publicity or litigation involving or surrounding us or our management, could make it substantially more difficult for us to attract new members. Similarly, because our existing members often act as references for us with prospective new members, any existing member that questions the quality of our care could impair our ability to secure additional new members. In addition, negative publicity resulting from any adverse government audit could injure our reputation. If we do not successfully maintain and enhance our reputation and brand recognition, our business may not grow and we could lose our relationships with members or providers, which would harm our business, results of operations and financial condition.
The registered or unregistered trademarks or trade names that we own may be challenged, infringed, circumvented, diluted, declared generic, lapsed or determined to be infringing on or dilutive of other marks. We may not be able to protect our rights in these trademarks and trade names, which we need in order to build name recognition with members, providers and other partners. In addition, third parties may in the future file for registration of trademarks similar or identical to our trademarks. If they succeed in registering or developing common law rights in such trademarks, and if we are not successful in challenging such third-party rights, we may not be able to use these trademarks to commercialize our technologies in certain relevant jurisdictions. If we are unable to establish name recognition based on our trademarks and trade names, we may not be able to compete effectively and our brand recognition, reputation and results of operations may be adversely affected.
Our business depends on our ability to effectively invest in, implement improvements to and properly maintain the uninterrupted operation and data integrity of our information technology platform and other business systems.
Our business is highly dependent on maintaining effective information systems, including our AVA platform, as well as the integrity and timeliness of the data we use to serve our members, support our in-house care teams and external providers and operate our business. Because of the large amount of data that we collect and manage, it is possible that hardware failures or errors in our systems could result in data loss or corruption or cause the information that we collect to be incomplete or contain inaccuracies that our in-house care teams, external providers and other partners regard as significant. If our data were found to be inaccurate or unreliable due to fraud or other error, or if we, or any of the providers we engage, were to fail to maintain information systems and data integrity effectively, we could experience operational disruptions that may impact our members, in-house care teams and external providers and other partners and hinder our ability to provide products and services, retain and attract members, manage our member risk profiles, report timely and accurate financial results and maintain regulatory compliance, among other things.
The COVID-19 pandemic could also cause our third-party data center hosting facilities and cloud computing platform providers, which are critical to our infrastructure, to shut down their business, experience security incidents that impact our business, delay or disrupt performance or delivery of services, or experience interference with the supply chain of hardware required by their systems and services, any of which could materially adversely affect our business. Limitations on access or disruptions to services provided by some of the external care providers upon which our platform and business operations rely could interrupt our ability to provide our platform, decrease the productivity of our workforce and provider networks, and significantly harm our business operations, financial condition and results of operations.
Our information technology strategy and execution are critical to our continued success because our technology platform is at the center of our business model. We must continue to invest in long-term solutions that will enable us to anticipate member needs and expectations, enhance the member experience, act as a differentiator in the market and protect against cybersecurity risks and threats. Our success is dependent, in large part, on maintaining the effectiveness of existing technology systems and continuing to deliver and enhance technology systems that support our business processes in a cost-efficient and resource-efficient manner. Increasing regulatory and legislative changes will place additional demands on our information technology infrastructure that could have a direct impact on resources available for other projects tied to our strategic initiatives. In addition, recent trends toward greater member engagement and increased regulatory scrutiny in healthcare require new and enhanced technologies. Connectivity among technologies is becoming increasingly important. We must also develop new systems to meet current market standards and keep pace with continuing changes in information processing technology, evolving industry and regulatory standards and member needs. Failure to do so may present compliance challenges and impede our ability to deliver products and services in a competitive manner. Further, because system development projects are long-term in nature, they may be more costly than expected to complete and may not deliver the expected benefits upon completion. Our failure to effectively invest in, implement improvements to and properly maintain the uninterrupted operation and data integrity of our information technology and other business systems could adversely affect our business, financial condition and results of operations.
If we are unable to obtain, maintain, protect and enforce intellectual property protection for our technology or if the scope of our intellectual property protection is not sufficiently broad, others may be able to develop and commercialize technology substantially similar to ours, and our ability to successfully commercialize our technology may be adversely affected.
42
Our business depends on internally developed technology and content, including software, databases, confidential information and know-how, such as the AVA platform, the protection of which is crucial to the success of our business. We rely on a combination of trademark, trade secret and copyright laws and confidentiality procedures and contractual provisions to protect our intellectual property rights in our internally developed technology and content. We may, over time, increase our investment in protecting our intellectual property through additional trademark, patent and other intellectual property filings that could be expensive and time-consuming. Effective trademark, trade secret, copyright and other intellectual property protection is expensive to develop and maintain, both in terms of initial and ongoing registration requirements and the costs of defending our rights. These measures, however, may not be sufficient to offer us meaningful protection. Additionally, we do not currently hold a patent or other registered or applied for intellectual property protection for AVA. If we are unable to protect our intellectual property and other proprietary rights, particularly with respect to AVA, our competitive position and our business could be harmed, as third parties may be able to commercialize and use technologies and software products that are substantially the same as ours without incurring the development and licensing costs that we have incurred. Any of our owned or licensed intellectual property rights could be challenged, invalidated, circumvented, infringed, misappropriated or otherwise violated, our trade secrets and other confidential information could be disclosed in an unauthorized manner to third parties, or our intellectual property rights may not be sufficient to permit us to take advantage of current market trends or otherwise to provide us with competitive advantages, which could result in costly redesign efforts, discontinuance of certain offerings or other competitive harm.
Monitoring unauthorized use of our intellectual property is difficult and costly. From time to time, we seek to analyze our competitors’ services, and may in the future seek to enforce our rights against potential infringement, misappropriation or other violation. However, the steps we have taken to protect our intellectual property rights may not be adequate to prevent infringement, misappropriation or other violation of our intellectual property. We may not be able to detect unauthorized use of, or take appropriate steps to enforce, our intellectual property rights. Any inability to meaningfully protect our intellectual property rights could result in harm to our ability to compete and reduce demand for our technology. Moreover, our failure to develop and properly manage new intellectual property could adversely affect our market positions and business opportunities. Also, some of our services rely on technologies and software developed by or licensed from third parties, and we may not be able to maintain our relationships with such third parties or enter into similar relationships in the future on reasonable terms or at all.
Uncertainty may result from changes to intellectual property legislation and from interpretations of intellectual property laws by applicable courts and agencies. Accordingly, despite our efforts, we may be unable to obtain, maintain, protect and enforce the intellectual property rights necessary to provide us with a competitive advantage. Our failure to obtain, maintain, protect and enforce our intellectual property rights could therefore have a material adverse effect on our business, financial condition and results of operations.
If we are unable to protect the confidentiality of our trade secrets, know-how and other proprietary and internally developed information, the value of our technology could be adversely affected.
We may not be able to protect our trade secrets, know-how and other internally developed proprietary information, including in relation to the AVA platform, adequately. Although we use reasonable efforts to protect this internally developed information and technology, our employees, consultants and other parties (including independent contractors and companies with which we conduct business) may unintentionally or willfully disclose our trade secrets or other proprietary information or technology to competitors. Enforcing a claim that a third party illegally disclosed or obtained and is using any of our internally developed information or technology is difficult, expensive and time-consuming, and the outcome is unpredictable. In addition, courts outside the United States are sometimes less willing to protect trade secrets, know-how and other proprietary information. We rely, in part, on non-disclosure, confidentiality and assignment-of-invention agreements with our employees, independent contractors, consultants and companies with which we conduct business to protect our trade secrets, know-how and other intellectual property and internally developed information. We may fail to enter into such agreements with all applicable parties, and such agreements may not be self-executing, or they may be breached and we may not have adequate remedies for such breach. Moreover, third parties may independently develop similar or equivalent proprietary information or reverse-engineer or otherwise gain access to our trade secrets, know-how and other internally developed information. Any of the foregoing could have a material adverse effect on our business, financial condition and results of operations.
Any restrictions on our use of, or ability to license, data, or our failure to license data and integrate third-party technologies, could have a material adverse effect on our business, financial condition and results of operations.
We depend upon licenses from third parties for some of the technology and data used in AVA, our core operating technology platform. We may be unsuccessful in maintaining those licenses, and in such event it is possible that alternative technology may not be available for license on favorable terms or at all. Moreover, we expect that we may need to obtain additional licenses from third parties in the future in connection with the development of our applications. In addition, we obtain a portion of the data that we use from government entities, public records, external healthcare providers and other partners. We believe that we have all rights necessary to use the data that is incorporated into our services. We cannot, however, assure you that our licenses for information will allow us to use that information for all potential or contemplated applications.
43
In addition, our ability to continue to offer an integrated healthcare experience to our members depends on maintaining AVA, which is partially populated with data disclosed to us by our members, the physicians in our network and our other partners with their consent. If these members, physicians and other partners revoke their consent for us to maintain, use, de-identify and share this data, consistent with applicable law, our data assets could be degraded.
In the future, data providers could withdraw their data from us or restrict our usage for any reason, including if there is a competitive reason to do so, if legislation is passed restricting the use of the data or if judicial interpretations are issued restricting use of the data that we currently use to support our services. In addition, data providers could fail to adhere to our quality control standards in the future, causing us to incur additional expense to appropriately utilize the data. If a substantial number of data providers were to withdraw or restrict their data, or if they fail to adhere to our quality control standards, and if we are unable to identify and contract with suitable alternative data suppliers and integrate these data sources into our service offerings, our ability to provide appropriate services to our members would be materially adversely impacted, which could have a material adverse effect on our business, financial condition and results of operations.
We also integrate into our internally developed applications and use third-party software to support our technology infrastructure. Some of this software is proprietary and some is open source software. These technologies may not be available to us in the future on commercially reasonable terms or at all and could be difficult to replace once integrated into our own internally developed applications. Most of these licenses can be renewed only by mutual consent and may be terminated if we breach the terms of the license and fail to cure the breach within a specified period of time. Our inability to obtain, maintain or comply with any of these licenses could delay development until equivalent technology can be identified, licensed and integrated, which would harm our business, financial condition and results of operations.
Our third-party licenses are generally non-exclusive and our competitors may obtain the right to use any of the data and technology covered by these licenses to compete directly with us. Our use of third-party technologies exposes us to increased risks, including, but not limited to, risks associated with the integration of new technology into our solutions, the diversion of our resources from development of our own internally developed technology and our inability to generate revenue from licensed technology sufficient to offset associated acquisition and maintenance costs. In addition, if our data suppliers choose to discontinue support of the licensed technology in the future, we might not be able to modify or adapt our own solutions.
Our use of “open source” software could adversely affect our ability to offer our products and services and subject us to possible litigation.
We may use open source software in connection with our services. Companies that incorporate open source software into their technologies have, from time to time, faced claims challenging the use of open source software and/or compliance with open source license terms. As a result, we could be subject to suits by parties claiming ownership of what we believe to be open source software or claiming noncompliance with open source licensing terms. Some open source software licenses require users who distribute software containing open source software to publicly disclose all or part of the source code to such software and/or make available any derivative works of the open source code, which could include valuable proprietary code of the user, on unfavorable terms or at no cost. While we monitor the use of open source software and try to ensure that none is used in a manner that would require us to disclose our internally developed source code, including that of our AVA platform, or that would otherwise breach the terms of an open source agreement, such use could inadvertently occur, in part because open source license terms are often ambiguous. In addition to risks related to license requirements, use of certain open source software can lead to greater risks than use of third-party commercial software, as open source licensors generally do not provide warranties or controls on the origin of software which, thus, may contain security vulnerabilities, such as the recent Log4j vulnerability, or infringing or broken code. Any requirement to publicly disclose our internally developed source code or pay damages for breach of contract could have a material adverse effect on our business, financial condition and results of operations and could help our competitors develop services that are similar to or better than ours.
We depend on our senior management team and other key employees, and the loss of one or more of these employees or an inability to attract and retain other highly skilled employees could harm our business.
Our success depends largely upon the continued services of our senior management team and other key employees. We rely on our leadership team in the areas of operations, product development, provision of medical services, information technology and security, marketing, and general and administrative functions. From time to time, there may be changes in our executive management team resulting from the hiring or departure of executives, which could disrupt our business. Our employment agreements with our executive officers and other key personnel do not require them to continue to work for us for any specified period and, therefore, they could terminate their employment with us at any time. Furthermore, volatility or lack of performance in our stock price may affect our ability to attract and retain replacements should key personnel depart. The loss of one or more of the members of our senior management team, or other key employees, could cause disruptions in or harm to our business, and replacing any such employees would entail significant time and cost. In particular, the loss of the services of our founder and Chief Executive Officer, John Kao, could significantly delay or prevent the achievement of our strategic objectives. We currently do not have “key person” insurance on any of our employees.
44
Competition for highly qualified personnel is intense, especially for technology specialists and for physicians, nurses and other medical professionals who are experienced in providing care services to older adults. We have, from time to time, experienced, and we expect to continue to experience, difficulty in hiring and retaining employees with appropriate qualifications. Many of the other Medicare Advantage plans and healthcare organizations with which we compete for experienced personnel have greater resources than we have. If we hire employees from competitors or other companies or healthcare providers, their former employees may attempt to assert that these employees or we have breached certain legal obligations, resulting in a diversion of our time and resources. If we fail to attract new personnel or fail to retain and motivate our current personnel, our business and future growth prospects could be harmed.
Our plans are concentrated in California, North Carolina, Nevada and Arizona, and so we are subject to risks associated with our geographic concentration, including unanticipated changes in population morbidity, which could significantly increase utilization rates and medical costs.
A substantial portion of our revenue is driven by CMS payments in connection with our health plans in California, North Carolina, Nevada and Arizona, with over 90% of our members concentrated in California as of December 31, 2021. As a result, our exposure to many of the risks described herein are not mitigated by a diversification of geographic focus. Unfavorable changes in healthcare or other benefit costs or reimbursement rates or increased competition in these areas or any other geographic area where our membership becomes concentrated in the future could therefore have a disproportionately adverse effect on our operating results. Furthermore, due to the concentration of our operations in these states and in California in particular, our business may be adversely affected by economic, health or other conditions that disproportionately affect these states as compared to other states or by natural disasters such as major earthquake, wildfire or hurricane. Any of these factors could have a significant impact on the health of a large number of our covered members, and regulatory changes undertaken in response to such events could require us to cover health care costs for members for which we would not typically be responsible.
Additionally, the geographic concentration and low-income status of a significant portion of our membership may make them more vulnerable to events such as the COVID-19 pandemic. In particular, a disproportionate number of our members may be affected by the COVID-19 pandemic, access to care may be more difficult, and proposed responses, including telehealth, may not be accessible. To continue to diversify our operations we will have to expand to other regions of the United States, which will require us to devote resources to identifying and exploring such perceived opportunities. We may not be able to continue to successfully expand our operations in any new geographic markets and so we may remain subject to the risks presented by our geographic concentration.
Our management team has limited experience managing a public company.
Most members of our management team have limited experience managing a publicly traded company, interacting with public company investors and complying with the increasingly complex laws pertaining to public companies. Our management team may not successfully or efficiently manage us as a public company that is subject to significant regulatory oversight and reporting obligations under the federal securities laws and the continuous scrutiny of securities analysts and investors. These new obligations and constituents require significant attention from our senior management and could divert their attention away from the day-to-day management of our business, which could adversely affect our business, results of operations and financial condition.
Competition for physicians and nurses, shortages of qualified personnel or other factors could increase our labor costs and adversely affect our revenue, profitability and cash flows.
Although we primarily contract with external providers for care delivery, we also employ physicians and other healthcare professionals to deliver in-house care, and our in-house care delivery operations are dependent on the efforts, abilities and experience of those employees. We compete with healthcare providers, hospitals, clinics, networks and other facilities in attracting physicians, nurses and medical staff to support our in-house care delivery capabilities and in recruiting and retaining qualified management and support personnel to be responsible for the daily operations of our clinics. In some markets, the lack of availability of clinical personnel, such as nurses, social workers and mental health professionals, is a significant operating issue facing all healthcare providers and others seeking to employ such personnel, and in certain markets the shortage has been exacerbated by the COVID-19 pandemic and its impacts, including governmental responses to the pandemic. This shortage may require us to continue to enhance wages and benefits to recruit and retain qualified personnel or to contract for more expensive temporary personnel. We also depend on the available labor pool of semi-skilled and unskilled workers in each of the markets in which we operate. Our failure to recruit and retain qualified management and medical personnel could have a material adverse effect on our business, financial condition and results of operations.
45
Any union activity that may occur among our clinical staff in the future could contribute to increased labor costs. Certain proposed changes in federal labor laws and the National Labor Relations Board’s modification of its election procedures could increase the likelihood of employee unionization attempts. Although none of our employees are currently represented by a collective bargaining agreement, to the extent a significant portion of our employee base unionizes, it is possible our labor costs could increase materially.
If our labor costs increase, we may not be able to offset these increased costs. Because a significant percentage of our revenue consists of fixed, prospective payments, our ability to pass along increased labor costs is limited. In particular, if labor costs rise at an annual rate greater than our net annual payments from CMS, our results of operations and cash flows will likely be adversely affected.
Our records, including those submitted to us by our external providers, may contain inaccurate or unsupportable information regarding risk adjustment scores of members, which could cause us to overstate or understate our revenue and subject us to various penalties.
The RAF scores attributable to our members determine, in part, the revenue to which we are entitled for the provision of medical care to our members. The data we submit to CMS is based, in part, on medical charts and diagnosis codes that our in-house clinical staff and our external providers prepare and submit to us. We generally rely on our in-house and externally engaged physicians to appropriately document and support such RAF data in our medical records. We also rely on our in-house and externally engaged physicians to appropriately code claims for medical services provided to members. If the providers do not provide us with accurate and supportable coding and diagnosis information, we may not be able to accurately estimate our revenue and medical costs associated with providing care to our members. If the data suggests the members are sicker than they actually are, we may overstate our revenue and overstate our costs. If the data suggests the members are healthier than they actually are, we may understate our revenue and underestimate our costs. Erroneous and/or unsupported submissions could result in a correction or retroactive adjustment in later periods. This corrected or adjusted information may be reflected in financial statements for periods subsequent to the period in which the revenue was recorded. We might also need to refund a portion of the revenue that we received, which refund, depending on its magnitude, could have a material adverse effect on our business, financial condition and results of operations.
Additionally, CMS audits Medicare Advantage organizations for documentation to support RAF-related payments for members. The Medicare Advantage organizations ask providers to submit the underlying documentation for members that they serve. It is possible that claims associated with members with higher RAF scores could be subject to more scrutiny in a CMS or plan audit. CMS may require us to make adjustments to our Medicare Advantage plan or impose other penalties as a result of its audits. In addition, we could be liable for penalties to the government under the FCA that range from $5,500 to $11,000 (adjusted for inflation) for each false claim, plus up to three times the amount of damages caused by each false claim, which can be as much as the amounts received directly or indirectly from the government for each such false claim. On January 29, 2018, the DOJ issued a final rule announcing adjustments to FCA penalties, under which the per claim penalty range was increased to a range from $11,181 to $22,363 for penalties assessed between January 29, 2018 and June 19, 2020, so long as the underlying conduct occurred after November 2, 2015. On June 19, 2020, the DOJ issued a final rule announcing further adjustments to FCA penalties, under which the per claim penalty range increases to a range from $11,665 to $23,331 for penalties assessed after June 19, 2020, so long as the underlying conduct occurred after November 2, 2015. CMS has indicated that, at least for some plan years, payment adjustments will not be limited to RAF scores for the specific Medicare Advantage enrollees for which errors are found but may also be extrapolated to the entire Medicare Advantage plan membership.
In addition to the provisions of the FCA, which provide for civil enforcement, the federal government can use several criminal statutes to prosecute persons who are alleged to have submitted false or fraudulent claims for payment to the federal government.
Our health plans may be randomly selected or targeted for review by CMS and the outcome of such a review may result in a material adjustment in our revenue and profitability, even if the information we submit to CMS is accurate and supportable.
A failure to accurately estimate incurred but not reported medical expense could adversely affect our results of operations.
Member care costs include estimates of future medical claims that have been incurred by the members but for which the provider has not yet billed. These claim estimates are made utilizing actuarial methods and are continually evaluated and adjusted by management, based upon our historical claims experience and other factors, including an independent assessment by a nationally recognized actuarial firm. Adjustments, if necessary, are made to medical claims expense and capitated revenues when the assumptions used to determine our claims liability change and when actual claim costs are ultimately determined.
46
Due to the inherent uncertainties associated with the factors used in these estimates and changes in the patterns and rates of medical utilization, materially different amounts could be reported in our financial statements for a particular period under different conditions or using different, but still reasonable, assumptions. It is possible that our estimates of this type of claim may be inadequate in the future. In such event, our results of operations could be adversely impacted. Further, the inability to estimate these claims accurately may also affect our ability to take timely corrective actions, further exacerbating the extent of any adverse effect on our results of operations.
Negative publicity regarding the managed healthcare industry generally could adversely affect our results of operations or business.
Negative publicity regarding the managed healthcare industry generally, or the Medicare Advantage program in particular, may result in increased regulation and legislative review of industry practices that further increase our costs of doing business and adversely affect our results of operations or business by:
Federal reductions in Medicare Advantage funding could adversely affect our financial condition and results of operations.
The majority of our revenues come from the government subsidized Medicare Advantage program. Medicare Advantage is a federally administered program financed in part by federal funds. The federal government has recently instituted measures aimed at controlling the growth of and/or reducing healthcare spending, including Medicare Advantage spending. We are exposed to financial risks associated with contracting with the federal government, including but not limited to our dependence upon Congress and CMS’ robustly funding the Medicare Advantage program and the impact that delays in government payments could have on our operating cash flow and liquidity. For example, future levels of funding for Medicare Advantage may be affected by continuing government efforts to contain healthcare costs and may further be affected by federal budgetary constraints. Congress periodically considers reducing or reallocating the amount of money the federal government spends on healthcare programs including the Medicare Advantage program, and CMS annually sets the rates and other financial factors that influence the amount of money Medicare Advantage organizations receive from the government. Furthermore, Medicare remains subject to the automatic spending reductions imposed by the Budget Control Act of 2011 and the American Taxpayer Relief Act of 2012 (“sequestration”), subject to a 2% cap, which has been extended several times, most recently by the Coronavirus Aid, Relief, and Economic Security Act of 2020, and is effective through 2030. Adverse economic conditions may put pressures on federal budgets as tax and other federal revenues decrease while the population that is eligible to participate in Medicare Advantage programs increases, creating more need for funding. This may require Congress and/or CMS to seek to reduce Medicare Advantage spending, which may result in reductions in funding for the Medicare Advantage program or contraction of covered benefits. A reduction (or less than expected increase), a protracted delay, or a change in allocation methodology in government funding for Medicare Advantage, as well as termination of one or more CMS contracts for the convenience of the government, may materially and adversely affect our results of operations, financial position and cash flows. In addition, if another federal government shutdown were to occur for a prolonged period of time, CMS payment obligations, including its obligations under the Medicare Advantage program, may be delayed. If CMS fails to make payments on a timely basis, our business could suffer, and our financial position, results of operations or cash flows may be materially affected. Payments from CMS may be delayed in the future, which, if extended for any significant period of time, could have a material adverse effect on our results of operations, financial position, cash flows or liquidity.
In addition, delays in obtaining, or failure to obtain or maintain, governmental approvals, or moratoria imposed by regulatory authorities, could adversely affect our revenues or membership, increase costs or adversely affect our ability to bring new products and services to market as forecasted.
Our clinics, the centers out of which our external providers operate, and the facilities that host our AVA platform may be negatively impacted by weather and other factors beyond our control.
47
Our results of operations may be adversely impacted by adverse conditions affecting our clinics, the centers out of which our external care providers operate, and the facilities that host our AVA platform, including severe weather events such as tornadoes and widespread winter storms, natural disasters such as earthquakes and fires, public health concerns such as contagious disease outbreaks, violence or threats of violence or other factors beyond our control that cause disruption of member scheduling, displacement of our members, employees and care teams, or force certain of our clinics, external providers’ centers, or facilities that host our AVA platform to close temporarily. In certain geographic areas, we have a large concentration of clinics, external provider facilities, and facilities that host our AVA platform that may be simultaneously affected by adverse weather conditions or other events. Our future operating results may be adversely affected by these and other factors that disrupt the operation of our clinics, the centers out of which our external providers operate and the facilities that host our AVA platform.
If we are unable to offer new and innovative products and services or our products and services fail to keep pace with advances in industry standards, technology and our members’ needs, our members may terminate or fail to renew their membership with us and our revenue and results of operations may suffer.
Our success depends on providing innovative, high-quality, customizable products and services that elevate our members’ healthcare experience and outcomes. If we cannot adapt to rapidly evolving industry standards, technology and increasingly sophisticated and varied members’ needs, our existing product and service offerings could become undesirable, obsolete or harm our reputation. In order to remain competitive, we must continue to invest significant resources in our personnel and technology in a timely and cost-effective manner in order to enhance our existing products and services and introduce new high-quality products and services that existing members and potential members will want. We are continually involved in a number of projects to develop new products and services, including the further refinement of our proprietary AVA platform. If our innovations are not responsive to the needs of our existing members or potential new members, are not appropriately timed with market opportunity, are not effectively brought to market or significantly increase our operating costs, we may lose existing members or be unable to enroll new members and our results of operations may suffer.
We are a holding company with no operations of our own, and we depend on our subsidiaries for cash.
Currently, we are a holding company and do not have any material assets or operations other than ownership of equity interests of our subsidiaries. Our operations are conducted almost entirely through our subsidiaries, and our ability to generate cash to meet our obligations or to pay dividends is highly dependent on the earnings of, and receipt of funds from, our subsidiaries through dividends, administrative expenses or intercompany loans. The ability of our subsidiaries to generate sufficient cash flow from future operations to allow us and them to make scheduled payments on our obligations will depend on their future financial performance, which will be affected by a range of economic, competitive and business factors, many of which are outside of our control. We cannot assure you that the cash flow and future earnings of our operating subsidiaries will be adequate for our subsidiaries to service their debt obligations. If our subsidiaries do not generate sufficient cash flow from future operations to satisfy corporate obligations, we may have to: undertake alternative financing plans (such as refinancing), restructure debt, sell assets, reduce or delay capital investments, or seek to raise additional capital. We cannot assure you that any such alternative refinancing would be possible, that any assets could be sold, or, if sold, of the timing of the sales and the amount of proceeds realized from those sales, that additional financing could be obtained on acceptable terms, if at all, or that additional financing would be permitted under the terms of our various debt instruments then in effect. Our inability to generate sufficient cash flow to satisfy our obligations, or to refinance our obligations on commercially reasonable terms, would have an adverse effect on our business, financial condition and results of operations. Furthermore, we and our subsidiaries may incur substantial additional indebtedness in the future that may severely restrict or prohibit our subsidiaries from making distributions, paying dividends or making loans to us.
Our ability to obtain funds from certain of our licensed subsidiaries is restricted by state insurance regulations.
Certain of our insurance subsidiaries operate in states that regulate the payment of dividends, loans, administrative expense reimbursements or other cash transfers to us, and require minimum levels of equity as well as limit investments to approved securities. The amount of dividends that may be paid to us by these insurance subsidiaries, without prior approval by state regulatory authorities, or ordinary dividends, is limited based on the entity’s level of statutory income and statutory capital and surplus. In some states, prior notification is provided before paying a dividend even if approval is not required. Actual dividends paid may vary due to consideration of excess statutory capital and surplus and expected future surplus requirements. We continue to maintain our levels of aggregate excess statutory capital and surplus in our state-regulated operating subsidiaries. Dividends from our non-insurance companies are generally not restricted by governmental departments of insurance. In the event that our subsidiaries are unable to provide sufficient capital to fund our obligations and allow us to pursue our objectives, our results of operations, financial position, and cash flows may be materially adversely affected.
We have limited experience serving as a Direct Contracting Entity with CMS and may not be able to realize the expected benefits thereof.
48
The CMS Center for Medicare and Medicaid Innovation recently announced a direct contracting model, which commenced in 2021, to create value-based payment arrangements directly with Direct Contracting Entities (“DCEs”), which is part of CMS’s strategy to drive broader healthcare reform and accelerate the shift from original Medicare toward value-based care models. A key aspect of direct contracting is providing new opportunities for a variety of different DCEs to participate in value-based care arrangements in Medicare fee-for-service. Our participation in the DCE program began on April 1, 2021 and, as of December 31, 2021, we had approximately 5,400 members in our DCE arrangement with our clinician partners in North Carolina, California and Nevada. Our participation in the DCE program is subject to annual CMS approval, and our contracts are not guaranteed to be renewed in future years. Prior to April 1, 2021, we had no experience serving as a DCE and may not be able to realize the expected benefits of these arrangements. In particular, we may be unable to achieve risk-like patient economics on original Medicare patients. Our participation in the direct contracting model may not be profitable to us initially or at all. In addition, our management team has and may further invest considerable time and resources in adapting to the direct contracting model. The direct contracting model may not be successful and may ultimately be discontinued, including as a result of decreased political support for value-based care or the direct contracting model, or may be unable to expand our total addressable market in the manner that we expect.
We are subject to risks associated with delegating services and functions to vendors.
We rely on a number of vendors and other third parties to perform various functions and fulfill our obligations to CMS and members. Our ability to operate our business depends on the performance of, and continued contracts with, these vendors. The functions performed by our major vendors include, but are not limited to, information technology support, claims processing, pharmaceutical benefit management, supplemental benefits (e.g., vision benefits) and other business process outsourcing. We also rely in part on third-party brokers for the marketing and sale of our insurance plans and on our IPAs, which perform certain functions on our behalf.
Our ability to operate our business depends on the performance of these third parties. Their performance may be compromised or interrupted for a variety of reasons, some of which are outside of our control. For example, if a vendor becomes disqualified by CMS from providing services in connection with a Medicare Advantage plan, we would be unable to continue to use their services. In the event that these third parties are unwilling or unable to perform services for us in accordance with our contract and legal requirements, we may face operational difficulties, penalties, fines, sanctions or litigation. Although we may be able to force the vendor to indemnify us for some or all of the financial penalties, our business and reputation may suffer nonetheless.
Additionally, in the event that one of our agreements with a key third party terminates, we may have a difficult time bringing the contracted services in-house or contracting with another vendor. Identifying a replacement vendor, negotiating an agreement with the vendor, and transitioning services to the vendor takes significant time and resources. We may be unable to enter into agreements with replacement vendors on favorable terms, or at all. Any loss of a key vendor relationship could result in a service disruption or unavailability and harm our ability to continue to develop, maintain, and improve our products.
Risks Related to Regulation
Our business activities are subject to substantial government regulation. New laws or regulations, or legislative, judicial, or regulatory changes in existing laws or regulations or their manner of application could increase our cost of doing business and may have a material adverse effect on our results of operations; our financial position; and our cash flows.
The Health Care Reform Law and Other Current or Future Legislative, Judicial or Regulatory Changes
The Patient Protection and Affordable Care Act and The Health Care and Education Reconciliation Act of 2010 (which we collectively refer to as the “Health Care Reform Law”) enacted significant reforms to various aspects of the U.S. health insurance industry. Certain significant provisions of the Health Care Reform Law include, among others, mandated coverage requirements, mandated benefits and guarantee issuance associated with commercial medical insurance, rebates to policyholders based on minimum benefit ratios, adjustments to Medicare Advantage premiums, the establishment of federally facilitated or state-based exchanges coupled with programs designed to spread risk among insurers, and the introduction of plan designs based on set actuarial values. Some of these changes impact us and other entities that offer Medicate Advantage plans. In addition, the Health Care Reform Law established insurance industry assessments, including an annual health insurance industry fee. In 2018, the fee levied on the health insurance industry was $14.3 billion. The health industry fee was permanently repealed beginning in calendar year 2021.
It is reasonably possible that the Health Care Reform Law and related regulations, as well as other current or future legislative, judicial or regulatory changes, including restrictions on our ability to manage our provider network or otherwise operate our business, or restrictions on profitability, including reviews by regulatory bodies that may compare the profitability of various products within our Medicare Advantage business and require that they remain within certain ranges of each other, increases in member benefits or changes to member eligibility criteria without corresponding increases in premium payments to us, may have
49
a material adverse effect on our results of operations (including restricting revenue, enrollment and premium growth in certain products and market segments, restricting our ability to expand into new markets, increasing our medical and operating costs, further lowering our payment rates and increasing our expenses associated with assessments), our financial position and our cash flows.
Additionally, potential legislative changes or judicial determinations, including activities to repeal or replace the Health Care Reform Law or declare all or certain portions of the Health Care Reform Law unconstitutional, creates uncertainty for our business, and we cannot predict when, or in what form, such legislative changes or judicial determinations may occur.
Health Insurance Portability and Accountability Act, the Health Information Technology for Economic and Clinical Health Act and Other Laws, Rules and Regulations Related to Data Privacy
We are subject to data privacy and protection laws and regulations that apply to the collection, transmission, storage and use of PHI and other PII, which among other things, impose certain requirements relating to the privacy, security and transmission of PII. The legislative and regulatory landscape for privacy and data protection continues to evolve, and there has been an increasing focus on privacy and data protection issues with the potential to affect our business. Failure to comply with any of these laws and regulations could result in enforcement action against us, including fines, public censure, claims for damages by affected individuals, damage to our reputation and loss of goodwill, any of which could have a material adverse effect on our business, financial condition, results of operations or prospects. Ongoing efforts to comply with evolving laws and regulations may be costly and require ongoing modifications to our policies, procedures and systems.
The use of individually identifiable health data by our business is regulated at federal and state levels. These laws and rules are changed frequently by legislation or administrative interpretation. Various state laws address the use and maintenance of individually identifiable health information. Most are derived from the privacy and security regulations promulgated under HIPAA. HIPAA includes administrative provisions directed at simplifying electronic data interchange through standardizing transactions, establishing uniform healthcare provider, payer, and employer identifiers, and establishing regulations aimed at protecting confidentiality and security of patient and member data. The rules preempt all inconsistent state laws unless the state law is more privacy-protective.
These regulations, in addition to other state laws, set standards for the security of electronic health information, including requirements that insurers provide customers with notice regarding how their individually identifiable health information is used. Compliance with HIPAA regulations requires us to regularly monitor security risk, implement and regularly review administrative, technical and physical safeguards to protect electronic health information, and provide workforce training, among other administrative efforts. HIPAA can also expose us to additional liability for violations by our business associates (e.g., entities that provide services to health plans and providers).
HIPAA imposes mandatory penalties for certain violations. In 2022, penalties for violations of HIPAA and its implementing regulations start at $120 per violation and are not to exceed approximately $60,000 per violation, subject to a cap of approximately $1.8 million for violations of the same standard in a single calendar year. However, a single breach incident can result in violations of multiple standards. HIPAA also authorizes state attorneys general to file suit on behalf of their residents for statutory damages of up to $25,000. While HIPAA does not create a private right of action allowing individuals to sue in civil court for violations of HIPAA, its standards have been used as the basis for duty of care in state civil suits such as those for negligence or recklessness in the misuse or breach of PHI.
HIPAA further requires that members be notified of any unauthorized acquisition, access, use or disclosure of their unsecured PHI that compromises the privacy or security of such information, with certain exceptions related to unintentional or inadvertent use or disclosure by employees or authorized individuals. HIPAA specifies that such notifications must be made “without unreasonable delay and in no case later than 60 calendar days after discovery of the breach.” If a breach affects 500 patients or more, it must be reported to HHS without unreasonable delay, and HHS will post the name of the breaching entity on its public web site. Breaches affecting more than 500 patients in the same state or jurisdiction must also be reported to the local media. If a breach involves fewer than 500 people, the covered entity must record it in a log and notify HHS at least annually.
We also publish statements to our members and partners that describe how we handle and protect PHI. If federal or state regulatory authorities or private litigants consider any portion of these statements to be untrue, we may be subject to claims of deceptive practices, which could lead to significant liabilities and consequences, including, without limitation, costs of responding to investigations, defending against litigation, settling claims, and complying with regulatory or court orders. Any of the foregoing consequences could have a material adverse impact on our business and our financial results
Data privacy and security at the state level remains an evolving landscape. For example, California’s California Consumer Privacy Act of 2018 ( “CCPA”), which came into effect on January 1, 2020, requires companies that process information on California residents to make new disclosures to consumers about their data collection, use and sharing practices, allow consumers to opt out of certain data sharing with third parties and provides a new cause of action for data breaches. In addition, on
50
November 3, 2020, California voters approved a new privacy law, the California Privacy Rights Act ( “CPRA”), which significantly modifies the CCPA, including by expanding consumers’ rights with respect to certain personal information and creating a new state agency to oversee implementation and enforcement efforts. This agency will be able to finance operations through penalties issued and with the CPRA’s removal of the mandatory cure period from CCPA, we will have less warning before compliance risk results in legal action. Many of the CPRA’s provisions will become effective on January 1, 2023. The CCPA and CPRA contain exemptions for medical information governed by the California Confidentiality of Medical Information Act, and for PHI collected by a covered entity or business associate governed by the privacy, security, and breach notification rule established pursuant to HIPAA, but the precise interpretation and application of this exemption by regulators is not yet clear.
The CCPA has prompted a number of proposals for new federal and state-level privacy legislation. Such proposed legislation, if enacted, may add additional complexity, variation in requirements, restrictions and potential legal risk, require additional investment of resources in compliance programs, impact strategies and the availability of previously useful data and could result in increased compliance costs and/or changes in business practices and policies. For example, the Virginia Consumer Data Protection Act, or the CDPA, signed by the Governor on March 2, 2021 and effective January 1, 2023, gives Virginia residents expanded rights to access and creates additional obligations on companies covered by the legislation.
It is possible that applicable laws may be interpreted and applied in a manner that is inconsistent with our practices and our efforts to comply with the evolving data protection rules may be unsuccessful. We must devote significant resources to understanding and complying with this changing landscape. Failure to comply with laws regarding privacy and security of PHI and other PII could expose us to penalties under such laws. Any such failure to comply with data protection and privacy laws could result in government-imposed fines or orders requiring that we change our practices, claims for damages or other liabilities, regulatory investigations and enforcement action, litigation and significant costs for remediation, any of which could adversely affect our business. Even if we are not determined to have violated these laws, government investigations into these issues typically require the expenditure of significant resources and generate negative publicity, which could have an adverse effect on our business, financial condition and results of operations.
As indicated above, there are numerous federal and state laws and regulations addressing patient and consumer privacy concerns, including notification requirements in the event of unauthorized access or theft of personal information. State statutes and regulations vary from state to state and could impose penalties. Violations of HIPAA or applicable federal or state laws or regulations could subject us to significant criminal or civil penalties, including significant monetary penalties. We cannot yet fully determine the impact these or future laws, rules, regulations and industry standards may have on our business or operations. Any such laws, rules, regulations and industry standards may be inconsistent among different jurisdictions, subject to differing interpretations or may conflict with our current or future practices. Additionally, our customers may be subject to differing privacy laws, rules and legislation, which may mean that they require us to be bound by varying contractual requirements applicable to certain other jurisdictions. Adherence to such contractual requirements may impact our collection, use, processing, storage, sharing and disclosure of various types of information and may mean we become bound by, or voluntarily comply with, self-regulatory or other industry standards relating to these matters that may further change as laws, rules and regulations evolve. Complying with these requirements and changing our policies and practices may be onerous and costly, and we may not be able to respond quickly or effectively to regulatory, legislative and other developments. These changes may in turn impair our ability to offer our existing or planned features, products and services and/or increase our cost of doing business. As we expand our customer base, these requirements may vary from customer to customer, further increasing the cost of compliance and doing business.
Our business and operations may also be subject to federal, state, and local consumer protection laws governing marketing communications, including the Telephone Consumer Protection Act, or TCPA, which places restrictions on the use of automated tools and technologies to communicate with wireless telephone subscribers or communications services consumers generally and the CAN-SPAM Act, which regulates the transmission of marketing emails. Under the TCPA, entities using an automatic dialing system to send communications must obtain prior express consent for non-marketing communications and prior express written consent for marketing communications. The TCPA has a private right of action, allowing individuals who have received unsolicited communications (phone calls, text messages or faxes) made using an “automatic dialing system” to seek statutory damages of $500 per violation, or $1500 if the violation was made willfully or knowingly. Despite our compliance efforts, we could nevertheless be forced to defend private class actions or government enforcement based on the communications we send to members.
In addition, certain of our businesses are also subject to the PCI DSS, which is a multifaceted security standard that is designed to protect credit card account data as mandated by payment brands and acquiring banks. We rely on vendors to assist us with PCI matters and to ensure PCI compliance. Despite our compliance efforts, we may become subject to claims that we have violated the PCI DSS or other requirements of the payment card brands, based on past, present, or future business practices, which could have an adverse impact on our business and reputation, subject us to fines and/or have a negative impact on our ability to accept credit card payments.
51
As described above, substantially all of our relevant member data is maintained on our technology platform, AVA, which aggregates and provides us with access to extensive member datasets, including individually identifiable PHI. As a result, any breach of our technology platform could expose us to substantial liability under HIPAA, the HITECH Act and other applicable laws, regulations or rules. See “Risk Factors—Security breaches, loss of data and other disruptions could compromise sensitive information related to our business or our members, or prevent us from accessing critical information and expose us to liability, which could adversely affect our business and our reputation.”
Corporate Practice of Medicine and Other Laws
As a corporate entity, we are not licensed to practice medicine. Many states in which we operate through our subsidiaries limit the practice of medicine to licensed individuals or professional organizations comprised of licensed individuals, and business corporations generally may not exercise control over the medical decisions of physicians. Statutes, regulations and court decisions relating to the practice of medicine, fee-splitting between physicians and referral sources, and similar issues vary widely from state to state. While we endeavor to comply with state corporate practice of medicine laws and regulations as we interpret them, the laws and regulations in these areas are complex, changing, and often subject to varying interpretations. The interpretation and enforcement of these laws vary significantly from state to state.
Under management agreements between certain of our subsidiaries and affiliated physician-owned professional groups, these groups retain sole responsibility for all medical decisions, as well as for hiring and managing physicians and other licensed healthcare providers, developing operating policies and procedures, implementing professional standards and controls, and maintaining malpractice insurance. Regulatory authorities and other parties may assert that, despite the management and administrative services agreements and other arrangements through which we operate, we are engaged in the prohibited corporate practice of medicine or that our arrangements constitute unlawful fee-splitting. Penalties for violations of the corporate practice of medicine or fee-splitting laws vary by state and may result in physicians being subject to disciplinary action, as well as to forfeiture of revenue from payors for services rendered. For business entities such as us, violations may also bring both civil and, in more extreme cases, criminal liability for engaging in medical practice without a license, our agreements could be found legally invalid and unenforceable (in whole or in part) or we could be required to restructure our contractual arrangements.
We, our in-house and externally engaged physicians and the facilities in which they operate are subject to various federal, state and local licensing and certification laws and regulations and accreditation standards and other laws, relating to, among other things, the adequacy of medical care, equipment, privacy of member information, physician relationships, personnel and operating policies and procedures. Failure to comply with these licensing, certification and accreditation laws, regulations and standards could result in prior payments being subject to recoupment, requirements to make significant changes to our operations and can give rise to civil or, in extreme cases, criminal penalties. We routinely take the steps we believe are necessary to retain or obtain all requisite licensure and operating authorities. While we have made reasonable efforts to substantially comply with federal, state and local licensing and certification laws and regulations and standards as we interpret them, the agencies that administer these programs may find that we have failed to comply in some material respects. If this were to occur, we could be subject to civil and/or criminal penalties, or we could be required to close or limit our operations at relevant sites.
In markets where the corporate practice of medicine is prohibited, we have historically operated by maintaining long-term management and administrative services contracts with multiple associated professional medical entities that are wholly owned or primarily owned by physicians employed by us and, in turn, employ or contract with physicians to provide those professional medical services required by our members. Under these management agreements, Alignment Healthcare USA, LLC performs only non-medical administrative services, does not represent that it offers medical services and does not exercise influence or control over the practice of medicine by the physicians or the associated physician groups. In addition to the above management arrangements, we have certain contractual rights relating to the orderly transfer of equity interests in our physician practices through succession agreements and other arrangements with their physician equity holders. Such equity interests cannot, however, be transferred to or held by us or by any non-professional medical corporation. Accordingly, neither we nor our direct subsidiaries directly own any equity interests in any of our physician practices. In the event that any of the physician owners of our practices fail to comply with the management arrangement, if any management arrangement is terminated and/or we are unable to enforce our contractual rights over the orderly transfer of equity interests in any of our physician practices, such events could have a material adverse effect on our business, results of operations, financial condition and cash flows.
It is possible that a state regulatory agency or a court could determine that our agreements with physician equity holders of practices and the way we carry out these arrangements as described above, either independently or coupled with the management services agreements with such associated physician practices, are in violation of prohibitions on the corporate practice of medicine. As a result, these arrangements could be deemed invalid. Such a determination could force a restructuring of our management arrangements with the affected practices, which might include revisions of the management services agreements, including a modification of the management fee and/or establishing an alternative structure that would permit us to contract with a physician network without violating prohibitions on the corporate practice of medicine. Such a restructuring may not be feasible, or it may not be possible to accomplish it within a reasonable time frame without a material adverse effect on our business, results of operations, financial condition and cash flows.
52
Anti-Kickback, Physician Self-Referral and Other Fraud and Abuse Laws
A federal law commonly referred to as the “Anti-Kickback Statute” prohibits the offer, payment, solicitation, or receipt of any form of remuneration to induce, or in return for, the referral of Medicare or other governmental health program patients or patient care opportunities, or in return for the purchase, lease or order of items or services that are covered by Medicare or other federal governmental health programs. Because the prohibitions contained in the Anti-Kickback Statute apply to the furnishing of items or services for which payment is made in “whole or in part,” the Anti-Kickback Statute could be implicated if any portion of an item or service we provide is covered by any of the state or federal health benefit programs described above. Violation of these provisions constitutes a felony criminal offense and applicable sanctions could include exclusion from the Medicare and Medicaid programs.
Section 1877 of the Social Security Act, commonly known as the “Stark Law,” prohibits physicians, subject to certain exceptions described below, from referring Medicare or Medicaid patients to an entity providing “designated health services” in which the physician, or an immediate family member, has an ownership or investment interest or with which the physician, or an immediate family member, has entered into a compensation arrangement. These prohibitions, contained in the Omnibus Budget Reconciliation Act of 1993, commonly known as “Stark II,” amended prior federal physician self-referral legislation known as “Stark I” by expanding the list of designated health services to a total of 11 categories. The professional groups with which we are contracted or affiliated provide one or more of these designated health services. Persons or entities found to be in violation of the Stark Law are subject to denial of payment for services furnished pursuant to an improper referral, civil monetary penalties, and exclusion from the Medicare and Medicaid programs.
A federal law commonly referred to as the “False Claims Act” prohibits the submission of a false or fraudulent claim to the government for payment or approval. Qui tam relators and/or the government may take the position that we submit certain data or information that could form the basis of a claim for payment, thus subjecting us to allegations under the False Claims Act. In such events, we could be subject to treble damages and per-claim penalties.
Many states also have enacted laws similar in scope and purpose to the Anti-Kickback Statute and, in more limited instances, the Stark Law, that are not limited to services for which Medicare or Medicaid payment is made. In addition, most states have statutes, regulations, or professional codes that restrict a physician from accepting various kinds of remuneration in exchange for making referrals. These laws vary from state to state and have seldom been interpreted by the courts or regulatory agencies. In states that have enacted these statutes, we believe that regulatory authorities and state courts interpreting these statutes may regard federal law under the Anti-Kickback Statute and the Stark Law as persuasive.
In addition, these laws are subject to modification and changes in interpretation, and are enforced by authorities vested with broad discretion. We continually monitor developments in this area. If we or our third parties with which we contract fail to comply with these laws, or if these laws are interpreted in a manner contrary to our interpretation or are reinterpreted or amended, or if new legislation is enacted with respect to healthcare fraud and abuse, illegal remuneration, or similar issues, we may be required to restructure our affected operations to maintain compliance with applicable law and/or be subject to liability. Such restructuring may not be possible or, if possible, may have a material adverse effect on our results of operations, financial position, or cash flows.
Environmental
We are subject to various federal, state, and local laws and regulations relating to the protection of human health and the environment. If an environmental regulatory agency finds any of our facilities to be in violation of environmental laws, penalties and fines may be imposed for each day of violation and the affected facility could be forced to cease operations. We could also incur other significant costs, such as cleanup costs or claims by third parties, as a result of releases of hazardous substances or violations of, or other liabilities under, environmental laws. Although we believe that our environmental practices, including waste handling and disposal practices, are in material compliance with applicable laws, future claims or violations, or changes in environmental laws, could have a material adverse effect on our results of operations, financial position or cash flows.
State Regulation of Insurance-Related Products
Laws in each of the states in which we operate our business license and regulate entities that offer health plans to residents of that state. The products we offer are sold under licenses issued by the applicable insurance regulators. However, for entities offering Medicare Advantage plans, federal law preempts all state laws and regulations except those relating to licensing and financial solvency.
53
With respect to state regulation of financial solvency, certain of our licensed insurance subsidiaries are subject to regulation under state insurance holding company regulations. These regulations generally require, among other things, prior approval and/or notice of certain material transactions, including dividend payments, purchases or sales of assets, intercompany agreements, and the filing of various financial and operational reports. The amount of dividends that may be paid to us by these insurance subsidiaries, without prior approval by state regulatory authorities, or ordinary dividends, is limited based on the entity’s level of statutory income and statutory capital and surplus. Actual dividends paid may vary due to consideration of excess statutory capital and surplus and expected future surplus requirements. We continue to maintain our levels of aggregate excess statutory capital and surplus in our state-regulated operating subsidiaries. Dividends from our non-insurance companies are generally not restricted by departments of insurance.
If any of our plans or operations are found to violate these or other government laws or regulations, we could suffer severe consequences that would have a material adverse effect on our business, results of operations, financial condition, cash flows, reputation and stock price, including:
If we are unable to effectively adapt to changes in the healthcare industry, including changes to laws and regulations regarding or affecting the U.S. healthcare reform, our business may be harmed.
Due to the importance of the healthcare industry in the lives of all Americans, federal, state, and local legislative bodies frequently pass legislation and promulgate regulations relating to healthcare reform or that affect the healthcare industry. As has been the trend in recent years, it is reasonable to assume that there will continue to be increased government oversight and regulation of the healthcare industry in the future. We cannot predict the ultimate content, timing or effect of any new healthcare legislation or regulations, nor is it possible at this time to estimate the impact of potential new legislation or regulations on our business. It is possible that future legislation enacted by Congress or state legislatures, or regulations promulgated by regulatory authorities at the federal or state level, could adversely affect our business or could change the operating environment of our clinical staff and external providers. It is possible that the changes in Medicare, Medicaid or other governmental healthcare program reimbursements may serve as precedent to possible changes in other payors’ reimbursement policies in a manner adverse to us. Similarly, changes in the private payor reimbursements could lead to adverse changes to Medicare, Medicaid and other governmental healthcare programs, which could have a material adverse effect on our business, financial condition and results of operations.
54
The policies and decisions of the federal and state governments regarding the Medicare Advantage program in which we participate have a substantial impact on our profitability. These governmental policies and decisions, which we cannot predict with certainty, directly shape the revenues given to us under the Medicare Advantage program, the eligibility and enrollment of our members, the services we provide to our members, and our administrative, healthcare services, and other costs associated with the Medicare Advantage program. Legislative or regulatory actions, such as changes to the Medicare Advantage program, those resulting in a reduction in payments to us, an increase in our cost of administrative and healthcare services, or additional fees, taxes or assessments, may have a material adverse effect on our results of operations, financial position, and cash flows.
While we believe that we have structured our agreements and operations in material compliance with applicable healthcare laws and regulations, we may be unable successfully address changes in the current regulatory environment. In addition, some of the healthcare laws and regulations applicable to us are subject to limited or evolving interpretations, and a review of our business or operations by a court, law enforcement or a regulatory authority might result in a determination that could have a material adverse effect on us. Furthermore, the healthcare laws and regulations applicable to us may be amended or interpreted in a manner that could have a material adverse effect on our business, prospects, results of operations and financial condition.
New federal restrictions on plans that CMS believes resemble dual-eligible special needs plans and new state-level restrictions on actual dual-eligible special needs plans may restrict the types and number of plans that we can offer, thus potentially adversely impacting our membership, revenue and/or profitability.
Medicare Advantage organizations may offer dual-eligible special needs plans (“D-SNPs”), which are plans that may only enroll beneficiaries who are eligible for both Medicare and Medicaid. D-SNPs must meet additional statutory and regulatory requirements that are intended to address certain challenges faced by the dually eligible population. According to CMS, some Medicare Advantage organizations offer plans that are not D-SNPs but that are designed to attract primarily dual-eligible beneficiaries (“D-SNP look-alike plans”). CMS recently issued a final rule to restrict the offering of D-SNP look-alike plans. Specifically, beginning in 2022, CMS will not enter into a contract for a new Medicare Advantage plan that is not a special needs plan (“SNP”) and is projected to enroll more than 80% dual-eligible members. Beginning in 2023, CMS will not renew a contract for such plans unless the plan has been active for less than a year and enrolls 200 or fewer members. Members enrolled in a non-renewed plan may be transitioned to another plan offered by the Medicare Advantage organization, if that plan meets certain criteria. Although the new rules did not materially impact our operations with respect to the 2022 plan year, they have the potential to do so with respect to 2023, as we have approximately 17,000 members that could require transfer from a D-SNP look-alike plan to another Alignment benefit plan with at least 20% non-dual eligible members (an “Alternative Alignment Plan”).
We are exploring various options that could allow us to avoid the need to transition our dually eligible members to an Alternative Alignment Plan and/or expand the range of plan options we can make available to these members, but we may not be successful in these efforts. In the event we are not successful, in certain of our markets we may work to transfer these members into D-SNPs, while in California, due to recent regulatory changes limiting the availability of D-SNP contracts, we would work to transfer these members into one or more Alternative Alignment Plans that are not D-SNPs but have benefits that are substantially similar or more attractive compared to our current D-SNP look-alike plans. Without offering these benefits enhancements, we may risk membership loss of the dually eligible population. However, because we will likely extend these benefits enhancements to an incrementally larger percentage of members, these product changes, benefit enhancements and other plan design decisions we make to the Alternative Alignment Plans to retain these members and incentivize growth may have a correspondingly incremental but potentially adverse impact on our financial condition, results of operations and cash flows.
If we lost the services of the licensed physicians who own our associated physician practices for any reason, the contractual arrangements with our associated physician practices could be in jeopardy.
As described above, because of regulations preventing the corporate practice of medicine, certain of our associated physician practice groups that operate our clinics are wholly owned or primarily owned by physicians employed by us. Although we retain certain rights regarding the succession of ownership of the associated practices through succession agreements and other arrangements with their physician equity holders, if current owners died, were incapacitated or otherwise were no longer affiliated with us, there could be a material adverse effect on the relationship between us and the associated physician practices and, therefore, our business operations could be adversely affected.
The contractual arrangements we have with our associated physician practices are not as secure as direct ownership of such entities. If we were to hold such groups directly, we would be able to exercise our rights as an equity holder directly to effect changes in the boards of directors of those entities, which could effect changes at the management and operational level. In contrast, under our current contractual arrangements with our physician groups, we may not be able to directly change the members of the boards of directors of these entities and would have to rely on the entities and the entities’ equity holders to perform their obligations in order to exercise our control over the entities. If any of these affiliated entities or their equity holders fail to perform their respective obligations under the contractual arrangements, we may have to incur substantial costs and expend additional resources to enforce such arrangements.
55
Changes in tax laws may adversely affect us, and the Internal Revenue Service or a court may disagree with tax positions taken by us, which may result in adverse effects on our financial condition or the value of our common stock.
The Tax Cuts and Jobs Act (the “TCJA”), enacted on December 22, 2017, significantly affected U.S. tax law, including by changing how the U.S. imposes tax on certain types of income of corporations and by reducing the U.S. federal corporate income tax rate to 21%. It also imposed new limitations on a number of tax benefits, including deductions for business interest, use of net operating loss carry forwards, taxation of foreign income and the foreign tax credit, among others.
The CARES Act, enacted on March 27, 2020, in response to the COVID-19 pandemic, further amended the U.S. federal tax code, including in respect of certain changes that were made by the TCJA, generally on a temporary basis. There can be no assurance that future tax law changes will not increase the rate of the corporate income tax significantly, impose new limitations on deductions, credits or other tax benefits, or make other changes that may adversely affect our business, cash flows or financial performance. In addition, the Internal Revenue Service (the "Service") has yet to issue guidance on a number of important issues regarding the changes made by the TCJA and the CARES Act. In the absence of such guidance, we will take positions with respect to a number of unsettled issues. There is no assurance that the Service or a court will agree with the positions taken by us, in which case tax penalties and interest may be imposed that could adversely affect our business, cash flows or financial performance.
Risks Related to Our Indebtedness and our Capital Requirements
Our existing indebtedness could adversely affect our business and growth prospects.
As of December 31, 2021, we had $154.1 million in principal amount (including the payment-in-kind balance and commitment fees) outstanding under our term loan maturing in June 2023 (the “Term Loan”). Our indebtedness under the Term Loan, or any additional indebtedness we may incur, could require us to divert funds identified for other purposes for debt service and impair our liquidity position. If we cannot generate sufficient cash flow from operations to service our debt, we may need to refinance our debt, dispose of assets or issue equity to obtain necessary funds. We do not know whether we will be able to take any of these actions on a timely basis, on terms satisfactory to us or at all.
Our indebtedness and the cash flow needed to satisfy our debt have important consequences, including:
Our level of indebtedness may place us at a competitive disadvantage to our competitors that are not as highly leveraged. Fluctuations in interest rates can increase borrowing costs. Increases in interest rates may directly impact the amount of interest we are required to pay and reduce earnings accordingly. In addition, developments in tax policy, such as the disallowance of tax deductions for interest paid on outstanding indebtedness, could have an adverse effect on our liquidity and our business, financial conditions and results of operations.
We expect to use cash flow from operations to meet current and future financial obligations, including funding our operations, debt service requirements and capital expenditures. The ability to make these payments depends on our financial and operating performance, which is subject to prevailing economic, industry and competitive conditions and to certain financial, business, economic and other factors beyond our control.
We may not be able to generate sufficient cash flow to service all of our indebtedness, and may be forced to take other actions to satisfy our obligations under such indebtedness, including refinancing such indebtedness, which may not be successful.
Our ability to make scheduled payments or to refinance outstanding debt obligations depends on our financial and operating performance, which will be affected by prevailing economic, industry and competitive conditions and by financial, business and other factors beyond our control. We may not be able to maintain a sufficient level of cash flow from operating activities to permit us to pay the principal, premium, if any, and interest on our indebtedness. Any failure to make payments of interest and principal on our outstanding indebtedness on a timely basis would likely result in penalties or defaults, which would also harm our ability to incur additional indebtedness.
56
If our cash flows and capital resources are insufficient to fund our debt service obligations, we may be forced to reduce or delay capital expenditures, sell assets, seek additional capital or seek to restructure or refinance our indebtedness. Any refinancing of our indebtedness could be at higher interest rates and may require us to comply with more onerous covenants. These alternative measures may not be successful and may not permit us to meet our scheduled debt service obligations. In the absence of such cash flows and resources, we could face substantial liquidity problems and might be required to sell material assets or operations to attempt to meet our debt service obligations. If we cannot meet our debt service obligations, the holders of our indebtedness may accelerate such indebtedness and, to the extent such indebtedness is secured, foreclose on our assets. In such an event, we may not have sufficient assets to repay all of our indebtedness.
We may need to refinance all or a portion of our indebtedness before maturity. We cannot assure you that we will be able to refinance any of our indebtedness on commercially reasonable terms or at all. We may not be able to obtain sufficient funds to enable us to repay or refinance our debt obligations on commercially reasonable terms, or at all.
The terms and conditions of our Term Loan restrict our current and future operations, particularly our ability to respond to changes or to take certain actions.
Our Term Loan contains a number of restrictive covenants that impose significant operating and financial restrictions on us and may limit our ability to engage in acts that may be in our long-term best interests, including restrictions on our ability to:
The restrictive covenants in our Term Loan require us to satisfy certain financial condition tests, including to maintain: a minimum liquidity of $6 million of unencumbered cash and permitted cash equivalent investments, as defined, on a consolidated basis, at least $10 million in consolidated accounts at the end of each calendar day and minimum consolidated revenue amounts. Our ability to satisfy those tests can be affected by events beyond our control. As December 31, 2021, we were in compliance with the financial covenants.
A breach of the covenants or restrictions under the Term Loan could result in an event of default under such document. Such a default may allow the creditors to accelerate the related debt. In the event the holders of our indebtedness accelerates the repayment, we may not have sufficient assets to repay that indebtedness or be able to borrow sufficient funds to refinance it. Even if we are able to obtain new financing, it may not be on commercially reasonable terms or on terms acceptable to us. As a result of these restrictions, we may be:
These restrictions, along with restrictions that may be contained in agreements evidencing or governing other future indebtedness, may affect our ability to grow in accordance with our growth strategy.
Our failure to raise additional capital or generate cash flows necessary to expand our operations and invest in new technologies in the future could reduce our ability to compete successfully and harm our results of operations.
57
We may need to raise additional funds, and we may not be able to obtain additional debt or equity financing on favorable terms or at all. Our need for additional capital will depend on our business needs, requirements and opportunities, including to develop and enhance new and existing products and services, enter new markets, further develop our infrastructure, and comply with any statutory, regulatory or contractual capital and liquidity requirements. In addition, we intend assess strategic acquisitions as the opportunities arise, some of which may be material to our operations. Our ability to obtain additional capital will depend on our development efforts, business plans, investor demand, operating performance, the condition of the capital markets, and other factors. If we raise additional equity financing, our security holders may experience significant dilution of their ownership interests. The equity securities we issue may also have rights, preferences, or privileges senior to the rights of existing stockholders. If we engage in additional debt financing, we may be required to accept terms that restrict our ability to incur additional indebtedness, force us to maintain specified liquidity or other ratios or restrict our ability to pay dividends or make acquisitions. In addition, the covenants in our Term Loan may limit our ability to obtain additional debt, and any failure to adhere to these covenants could result in penalties or defaults that could further restrict our liquidity or limit our ability to obtain financing.
If we need additional capital and cannot raise it on acceptable terms, or at all, we may not be able to, among other things:
If we are unable to obtain adequate financing or financing on terms satisfactory to us when we require it, our ability to continue to support our business growth and to respond to business challenges could be significantly limited or impaired.
Risks Related to Our Common Stock
Our operating results and stock price may be volatile, and the market price of our common stock may drop below the price you pay.
Our quarterly operating results are likely to fluctuate in the future. In addition, securities markets worldwide, and newly public companies in the healthcare and technology industry in particular, have experienced, and are likely to continue to experience, significant price and volume fluctuations. This market volatility, as well as general economic, market or political conditions, could subject the market price of our shares to wide price fluctuations regardless of our operating performance. Our operating results and the trading price of our shares may fluctuate in response to various factors, including:
58
These and other factors, many of which are beyond our control, may cause our operating results and the market price and demand for our shares to fluctuate substantially. Fluctuations in our quarterly or annual operating results could limit or prevent investors from readily selling their shares and may otherwise negatively affect the market price and liquidity of our shares. In addition, in the past, when the market price of a stock has been volatile, holders of that stock have sometimes instituted securities class action litigation against the company that issued the stock. If any of our shareholders brought a lawsuit against us, we could incur substantial costs defending the lawsuit. Such a lawsuit could also divert the time and attention of our management from our business, which could significantly harm our profitability and reputation. Further, we provide indemnification for our officers and directors for certain claims in connection with such litigation. Large indemnity payments would adversely affect our business, results of operations, and financial condition.
Our actual operating results may not meet or exceed our guidance and investor expectations, which would likely cause our stock price to decline.
From time to time, we may release guidance in our earnings releases, earnings conference calls or otherwise, regarding our future performance that represent our management’s estimates as of the date of release. If given, this guidance, which will include forward-looking statements, will be based on projections prepared by our management. Projections are based upon a number of assumptions and estimates that, while presented with numerical specificity, are inherently subject to significant business, economic and competitive uncertainties and contingencies, many of which are beyond our control. Our actual results could differ materially from such projections. Factors that could cause or contribute to such differences include, but are not limited to, those identified in this “Risk Factors” section. The principal reason that we expect to release guidance is to provide a basis for our management to discuss our business outlook with analysts and investors. With or without our guidance, analysts and other investors may publish expectations regarding our business, financial performance and results of operations. Guidance is necessarily speculative in nature, and it can be expected that some or all of the assumptions of the guidance furnished by us will not materialize or will vary significantly from actual results. If our actual performance does not meet or exceed our guidance or investor expectations, the trading price of our ordinary shares may decline.
An active, liquid trading market for our common stock may not be sustained.
Although our common stock is currently listed on the Nasdaq under the symbol “ALHC,” an active trading market for our shares may not be sustained. Accordingly, if an active trading market for our common is not maintained, the liquidity of our common stock, your ability to sell your shares of our common stock when desired and the prices that you may obtain for your shares of common stock will be adversely affected. An inactive market may also impair our ability to raise capital to continue to fund operations by issuing shares and may impair our ability to acquire other companies or technologies by using our shares as consideration.
The Lead Sponsors hold a substantial percentage of our outstanding common stock and have the ability to significantly influence our management, business plans and policies and the election of our directors, and their interests may conflict with ours or the holders of our common stock in the future.
As of December 31, 2021, funds managed by General Atlantic, L.P. (“General Atlantic”) and Warburg Pincus LLC (“Warburg Pincus” and, together with General Atlantic, the “Lead Sponsors”) beneficially owned approximately 49.6% of our common stock, which means that, based on their combined percentage voting power held after the offering, the Lead Sponsors together will effectively control the vote of all matters submitted to a vote of our shareholders, which will effectively enable them to control the election of the members of our board of directors (the “Board”) and all other corporate decisions. Accordingly, the Lead Sponsors have significant influence with respect to our management, business plans and policies, including the appointment and removal of our officers, decisions on whether to raise future capital and amending our charter and bylaws, which govern the rights attached to our common stock. In particular, for so long as the Lead Sponsors continue to own a significant percentage of our stock, the Lead Sponsors will be able to cause or prevent a change of control of us or a change in the composition of our Board and could preclude any unsolicited acquisition of us. The concentration of ownership could deprive holders of an opportunity to receive a premium for their shares of common stock as part of a sale of us and ultimately might affect the market price of our common stock.
In addition, in connection with our IPO, we entered into a Stockholders Agreement with the Lead Sponsors that provides (x) General Atlantic the right to designate: (i) four of the nominees for election to our Board for so long as General Atlantic beneficially owns at least 35% of our common stock then outstanding; (ii) three of the nominees for election to our Board for so long as General Atlantic beneficially owns less than 35% but at least 25% of our common stock then outstanding; (iii) two of the nominees for election to our Board for so long as General Atlantic beneficially owns less than 25% but at least 15% of our common stock then outstanding; and (iv) one of the nominees for election to our Board for so long as General Atlantic
59
beneficially owns less than 15% but at least 5% of our common stock then outstanding and (y) Warburg Pincus the right to designate one of the nominees for election to our Board for so long as Warburg Pincus beneficially owns at least 5% of our common stock then outstanding. The Lead Sponsors may also assign such right to their affiliates.
The Lead Sponsors and their affiliates engage in a broad spectrum of activities, including investments in the healthcare industry generally. In the ordinary course of their business activities, the Lead Sponsors and their affiliates may engage in activities where their interests conflict with our interests or those of our other shareholders, such as investing in or advising businesses that directly or indirectly compete with certain portions of our business or are suppliers or customers of ours. Our certificate of incorporation provides that none of the Lead Sponsors, any of their affiliates or any director who is not employed by us (including any non-employee director who serves as one of our officers in both his director and officer capacities) or its affiliates will have any duty to refrain from engaging, directly or indirectly, in the same business activities or similar business activities or lines of business in which we operate. The Lead Sponsors also may pursue acquisition opportunities that may be complementary to our business and, as a result, those acquisition opportunities may not be available to us. In addition, each of the Lead Sponsors may have an interest in pursuing acquisitions, divestitures and other transactions that, in its judgment, could enhance its investment, even though such transactions might involve risks to holders of our common stock.
Future sales and issuances by us of our common stock could result in additional dilution to you and could cause the price of our common stock to drop significantly. Additionally, a significant portion of our total outstanding shares may be sold into the market in the future. This could also cause the market price of our common stock to drop significantly, even if our business is doing well.
From time to time in the future, we may also issue additional shares of our common stock or securities convertible into our common stock pursuant to a variety of transactions, including acquisitions. Additionally, we have registered shares of common stock that we may issue under our equity compensation plans. Subject to the satisfaction of vesting conditions, such shares can be freely sold in the public market upon issuance. The issuance by us of additional shares of our common stock or securities convertible into our common stock would dilute your ownership of us and may cause the price of our common stock to drop significantly.
Moreover, sales of a substantial number of shares of our common stock in the public market by the holders thereof could occur at any time. These sales, or the perception in the market that the holders of a large number of shares intend to sell shares, could reduce the market price of our common stock. As of December 31, 2021, we had 187,193,613 outstanding shares of common stock. All of the shares of common stock sold in our IPO are freely tradable without restriction or further registration under the Securities Act of 1933, as amended (the "Securities Act"), except that any shares held by our affiliates, as that term is defined under Rule 144 of the Securities Act, may be sold only in compliance with certain limitations. Contractual lock-up restrictions imposed in connection with the IPO have now lapsed. The market price of our stock could decline if the holders of such shares sell them or are perceived by the market as intending to sell them. These factors could also make it more difficult for us to raise additional funds through future offerings of our shares of common stock or other securities.
If securities or industry analysts do not publish research or reports about our business, if they adversely change their recommendations regarding our shares or if our results of operations do not meet their expectations, our stock price and trading volume could decline.
The trading market for our shares is influenced by the research and reports that industry or securities analysts publish about us or our business. We do not have any control over these analysts. If one or more of these analysts cease coverage of us or fail to publish reports on us regularly, we could lose visibility in the financial markets, which in turn could cause our stock price or trading volume to decline. Moreover, if one or more of the analysts who cover us downgrade our stock, or if our results of operations do not meet their expectations, our stock price could decline.
We may issue shares of preferred stock in the future, which could make it difficult for another company to acquire us or could otherwise adversely affect holders of our common stock, which could depress the price of our common stock.
Our certificate of incorporation authorizes us to issue one or more series of preferred stock. Our Board has the authority to determine the preferences, limitations and relative rights of the shares of preferred stock and to fix the number of shares constituting any series and the designation of such series, without any further vote or action by our shareholders. Our preferred stock could be issued with voting, liquidation, dividend and other rights superior to the rights of our common stock. The potential issuance of preferred stock may delay or prevent a change in control of us, discouraging bids for our common stock at a premium to the market price, and materially adversely affect the market price and the voting and other rights of the holders of our common stock.
Because we have no current plans to pay regular cash dividends on our common stock for the foreseeable future, you may not receive any return on investment unless you sell your common stock for a price greater than that which you paid for it.
60
We do not anticipate paying any regular cash dividends on our common stock for the foreseeable future. Any decision to declare and pay dividends in the future will be made at the discretion of our Board and will depend on, among other things, our results of operations, financial condition, cash requirements, contractual restrictions and other factors that our Board may deem relevant. In addition, our ability to pay dividends is, and may be, limited by covenants of existing and any future outstanding indebtedness we or our subsidiaries incur. Therefore, any return on investment in our common stock is solely dependent upon the appreciation of the price of our common stock on the open market, which may not occur.
Provisions of our corporate governance documents could make an acquisition of us more difficult and may prevent attempts by our shareholders to replace or remove our current management, even if beneficial to our shareholders.
In addition to the Lead Sponsors’ beneficial ownership of a combined 49.6% of our common stock, our certificate of incorporation and bylaws and the Delaware General Corporation Law (the “DGCL”) contain provisions that could make it more difficult for a third party to acquire us, even if doing so might be beneficial to our shareholders. Among other things, these provisions:
Our certificate of incorporation contains a provision that provides us with protections similar to Section 203 of the DGCL, and prevents us from engaging in a business combination with a person who acquires at least 15% of our common stock for a period of three years from the date such person (excluding the Lead Sponsors and any of their direct or indirect transferees and any group as to which such persons are a party) acquired such common stock, unless Board or shareholder approval is obtained prior to the acquisition. These provisions could discourage, delay or prevent a transaction involving a change in control of our company. These provisions could also discourage proxy contests and make it more difficult for you and other shareholders to elect directors of your choosing and cause us to take other corporate actions you desire, including actions that you may deem advantageous, or negatively affect the trading price of our common stock. In addition, because our Board is responsible for appointing the members of our management team, these provisions could in turn affect any attempt by our shareholders to replace current members of our management team.
These and other provisions in our certificate of incorporation, bylaws and Delaware law could make it more difficult for shareholders or potential acquirers to obtain control of our Board or initiate actions that are opposed by our then-current Board, including delay or impede a merger, tender offer or proxy contest involving our company. The existence of these provisions could negatively affect the price of our common stock and limit opportunities for you
to realize value in a corporate transaction.
The provision of our certificate of incorporation requiring exclusive forum in the Court of Chancery of the State of Delaware or the federal district courts of the United States for certain types of lawsuits may have the effect of discouraging lawsuits against our directors and officers.
61
Pursuant to our certificate of incorporation, unless we consent in writing to the selection of an alternative forum, the Court of Chancery of the State of Delaware will be the sole and exclusive forum for (1) any derivative action or proceeding brought on our behalf, (2) any action asserting a claim of breach of a fiduciary duty owed by any of our directors, officers or other employees to us or our shareholders, (3) any action asserting a claim against us arising pursuant to any provision of the DGCL, our certificate of incorporation or our bylaws or (4) any other action asserting a claim against us that is governed by the internal affairs doctrine; provided that for the avoidance of doubt, the forum selection provision that identifies the Court of Chancery of the State of Delaware as the exclusive forum for certain litigation, including any “derivative action”, will not apply to suits to enforce a duty or liability created by the Securities Act, the Exchange Act or any other claim for which there is exclusive federal or concurrent federal and state jurisdiction. Additionally, unless we consent in writing to the selection of an alternative forum, the federal district courts of the United States of America shall be the exclusive forum for the resolution of any complaint asserting a cause of action arising under the Securities Act. Although we believe these exclusive forum provisions benefit us by providing increased consistency in the application of Delaware law and federal securities laws in the types of lawsuits to which each applies, the exclusive forum provisions may limit a stockholder’s ability to bring a claim in a judicial forum that it finds favorable for disputes with us or any of our directors, officers or stockholders, which may discourage lawsuits with respect to such claims. Our stockholders will not be deemed to have waived our compliance with the federal securities laws and the rules and regulations thereunder as a result of our exclusive forum provisions. Further, in the event a court finds any such exclusive forum provision contained in our certificate of incorporation to be unenforceable or inapplicable in an action, we may incur additional costs associated with resolving such action in other jurisdictions, which could harm our business, operating results and financial condition. Our certificate of incorporation further provides that any person or entity purchasing or otherwise acquiring any interest in shares of our capital stock is deemed to have notice of and consented to the provisions of our certificate of incorporation described above. The forum selection clauses in our certificate of incorporation may have the effect of discouraging lawsuits against us or our directors and officers and may limit our shareholders’ ability to obtain a favorable judicial forum for disputes with us.
General Risk Factors
Our overall business results may suffer from an economic downturn.
During periods of high unemployment, governmental entities often experience budget deficits as a result of increased costs and lower than expected tax collections. Moreover, the COVID-19 pandemic has created additional budgetary pressure on governmental entities. These budget deficits at federal, state and local government entities have decreased, and may continue to decrease, spending for health and human service programs, including Medicare and similar programs, which represents the most significant revenue source for us.
Our corporate culture has contributed to our success, and if we cannot maintain this culture as we grow, we could lose the innovation, creativity and teamwork fostered by our culture and our business may be harmed.
We believe that our culture has been and will continue to be a critical contributor to our success. We expect to continue to hire aggressively as we expand, and we believe our corporate culture has been crucial in our success and our ability to attract highly skilled personnel. If we do not continue to develop our corporate culture or maintain and preserve our core values of always putting the senior first, supporting doctors, using data and technology to revolutionize healthcare and acting with a serving heart, as we grow and evolve, we may be unable to foster the innovation, curiosity, creativity, focus on execution, teamwork and the facilitation of critical knowledge transfer and knowledge sharing we believe we need to support our growth. Our anticipated headcount growth and our transition from a private company to a public company may result in a change to our corporate culture, which could harm our business.
The requirements of being a public company may strain our resources and distract our management, which could make it difficult to manage our business.
As a public company, we incur legal, accounting and other expenses that we did not previously incur. We are subject to the reporting requirements of the Exchange Act and the Sarbanes-Oxley Act of 2002 (the "Sarbanes-Oxley Act"), the listing requirements of and other applicable securities rules and regulations. Compliance with these rules and regulations will continue to increase our legal and financial compliance costs, make some activities more difficult, time-consuming or costly and increase demand on our systems and resources. The Exchange Act requires that we file annual, quarterly and current reports with respect to our business, financial condition and results of operations. The Sarbanes-Oxley Act requires, among other things, that we establish and maintain effective internal controls and procedures for financial reporting, as discussed further below. Furthermore, the need to establish the corporate infrastructure demanded of a public company may divert our management’s attention from implementing our growth strategy, which could prevent us from improving our business, financial condition and results of operations. We have made, and will continue to make, changes to our internal controls and procedures for financial reporting and accounting systems to meet our reporting obligations as a public company. However, the measures we take may not be sufficient to satisfy our obligations as a public company. In addition, these rules and regulations increase our legal and financial compliance costs and make some activities more time-consuming and costly. For example, these rules and regulations make it more difficult
62
and more expensive for us to obtain director and officer liability insurance, and we may be required to incur substantial costs to maintain the same or similar coverage. These additional obligations could have a material adverse effect on our business, financial condition and results of operations.
In addition, changing laws, regulations and standards relating to corporate governance and public disclosure are creating uncertainty for public companies, increasing legal and financial compliance costs and making some activities more time consuming. These laws, regulations and standards are subject to varying interpretations, in many cases due to their lack of specificity and, as a result, their application in practice may evolve over time as new guidance is provided by regulatory and governing bodies. This could result in continuing uncertainty regarding compliance matters and higher costs necessitated by ongoing revisions to disclosure and governance practices. We have invested, and will continue to invest, resources to comply with evolving laws, regulations and standards, and this investment may result in increased general and administrative expenses and a diversion of our management’s time and attention from revenue-generating activities to compliance activities. If our efforts to comply with new laws, regulations and standards differ from the activities intended by regulatory or governing bodies due to ambiguities related to their application and practice, regulatory authorities may initiate legal proceedings against us and there could be a material adverse effect on our business, financial condition and results of operations.
As a result of becoming a public company, we are obligated to develop and maintain proper and effective internal control over financial reporting in order to comply with Section 404 of the Sarbanes-Oxley Act. These internal controls may not be determined to be effective, which may adversely affect investor confidence in us and, as a result, the value of our common stock. In addition, due to a transition period established by the SEC, we are not required to include a report of management’s assessment regarding internal control over financial reporting or an attestation report of our registered public accounting firm in our annual reports until the year following our first annual report filed with the SEC.
We became a public company following our IPO, and we will be required by Section 404 of the Sarbanes-Oxley Act to furnish a report by management on, among other things, the effectiveness of our internal control over financial reporting as of the year ended December 31, 2022. The process of designing and implementing internal control over financial reporting required to comply with this requirement will be time-consuming, costly and complicated. If during the evaluation and testing process we identify one or more material weaknesses or significant deficiencies in our internal control over financial reporting, our management may be unable to assert that our internal control over financial reporting is effective. In addition, if we fail to achieve and maintain the adequacy of our internal controls, as such standards are modified, supplemented or amended from time to time, we may not be able to ensure that we can conclude on an ongoing basis that we have effective internal controls over financial reporting in accordance with Section 404 of the Sarbanes-Oxley Act.
Even if our management concludes that our internal control over financial reporting is effective, our independent registered public accounting firm may issue a report that is qualified if it is not satisfied with our controls or the level at which our controls are documented, designed, operated or reviewed.
We cannot be certain as to the timing of completion of our evaluation, testing and any remediation actions or the impact of the same on our operations. If we are not able to implement the requirements of Section 404 of the Sarbanes-Oxley Act in a timely manner or with adequate compliance, our independent registered public accounting firm may issue an adverse opinion due to ineffective internal controls over financial reporting, and we may be subject to sanctions or investigation by regulatory authorities, such as the SEC. As a result, there could be a negative reaction in the financial markets due to a loss of confidence in the reliability of our financial statements. In addition, we may be required to incur costs in improving our internal control system and the hiring of additional personnel. Any such action could negatively affect our results of operations and cash flows.
Third parties may initiate legal proceedings alleging that we are infringing, misappropriating or otherwise violating their intellectual property rights, the outcome of which would be uncertain and could have a material adverse effect on our business, financial condition and results of operations.
Our commercial success depends on our ability to develop and commercialize our products and services and use our internally developed technology without infringing the intellectual property or proprietary rights of third parties. Intellectual property disputes can be costly to defend and may cause our business, operating results and financial condition to suffer. As the market for healthcare in the United States expands and more patents are issued, the risk increases that there may be patents issued to third parties that relate to our technology of which we are not aware or that we must challenge in order to continue our operations as currently or in the future contemplated. Whether merited or not, we may face allegations that we, our partners or parties indemnified by us have infringed, misappropriated or otherwise violated the patents, trademarks, copyrights, trade secrets or other intellectual property rights of third parties. Such claims may be made by competitors seeking to obtain a competitive advantage or by other parties. Additionally, in recent years, individuals and groups have begun purchasing intellectual property assets for the purpose of making such claims and attempting to extract settlements from companies like ours. We may also face allegations that our employees have misappropriated the trade secrets or other intellectual property or proprietary rights of their former employers or other third parties.
63
It may be necessary for us to initiate litigation to defend ourselves in order to determine the scope, enforceability, validity or ownership of third-party intellectual property or proprietary rights, or to establish our respective rights. We may not be able to successfully settle or otherwise resolve such adversarial proceedings or litigation. If we are unable to successfully settle future claims on terms acceptable to us we may be required to engage in or to continue claims, regardless of whether such claims have merit, that can be time-consuming, divert management’s attention and financial resources and be costly to evaluate and defend. Results of any such litigation are difficult to predict and may require us to stop commercializing or using our technology, obtain licenses, modify our services and technology while we develop non-infringing substitutes or incur substantial damages, settlement costs or face a temporary or permanent injunction prohibiting us from marketing or providing the affected products and services. If we require a third-party license, it may not be available on reasonable terms or at all, and we may have to pay substantial royalties and upfront or ongoing fees, or grant cross-licenses to our own intellectual property rights. Such licenses may also be non-exclusive, which could allow competitors and other parties to use the subject technology in competition with us. We may also have to redesign our services so they do not infringe, misappropriate or otherwise violate third-party intellectual property rights, which may not be possible or may require substantial monetary expenditures and time, during which our technology may not be available for commercialization or use. Even if we have an agreement to indemnify us against such costs, the indemnifying party may be unable to uphold its contractual obligations. If we cannot or do not obtain a third-party license to the infringed technology at all, license the technology on reasonable terms or obtain similar technology from another source, our revenue and earnings could be adversely impacted.
From time to time, we may be subject to legal proceedings and claims in the ordinary course of business with respect to intellectual property. Some third parties may be able to sustain the costs of complex litigation more effectively than we can because they have substantially greater resources. Even if resolved in our favor, litigation or other legal proceedings relating to intellectual property claims may cause us to incur significant expenses, and could distract our technical and management personnel from their normal responsibilities. In addition, there could be public announcements of the results of hearings, motions or other interim proceedings or developments, and if securities analysts or investors perceive these results to be negative, it could have a material adverse effect on the price of our common stock. Moreover, any uncertainties resulting from the initiation and continuation of any legal proceedings could have a material adverse effect on our ability to raise the funds necessary to continue our operations. Any of the foregoing could have a material adverse effect on our business, financial condition and results of operations.
Item 1B. Unresolved Staff Comments.
None.
Item 2. Properties.
Our corporate office is located in Orange, California at 1100 W. Town and Country Rd, Suite 1600, where we lease approximately 89,000 square feet of office space under a lease that terminates in 2024. We also have offices located in Cary and Raleigh, North Carolina and Las Vegas, Nevada, and small clinics located in Los Angeles, Milpitas, Modesto and Stockton, California, and Cary and Raleigh, North Carolina. We believe that our properties are generally suitable to meet our needs for the foreseeable future. In addition, to the extent we require additional space in the future, we believe that it would be readily available on commercially reasonable terms.
Item 3. Legal Proceedings.
We are from time to time subject to, and are presently involved in, litigation and other legal proceedings. We believe that there are no pending lawsuits or claims that, individually or in the aggregate, may have a material effect on our business, financial condition or operating results. The results of any future claims or proceedings cannot be predicted with certainty, and regardless of the outcome, litigation can have an adverse impact on us because of defense and litigation costs, diversion of management resources, and other factors.
Item 4. Mine Safety Disclosures.
Not applicable.
64
PART II
Item 5. Market for Registrant’s Common Equity, Related Stockholder Matters and Issuer Purchases of Equity Securities.
Market Information
Our common stock has been traded under the symbol “ALHC” on the NASDAQ Global Select Market since our initial public offering on March 26, 2021. Prior to that time, there was no public market for our common stock. As of February 28, 2022, there were approximately 67 holders of record of our common stock.
Dividend Policy
We currently intend to retain all available funds and any future earnings to fund the development and growth of our business and to potentially repay any indebtedness and, therefore, we do not anticipate paying any cash dividends in the foreseeable future. Additionally, because we are a holding company, our ability to pay dividends on our common stock may be limited by restrictions on the ability of our subsidiaries to pay dividends or make distributions to us. Any future determination to pay dividends will be at the discretion of our Board, subject to compliance with covenants in current and future agreements governing our and our subsidiaries’ indebtedness, and will depend on our results of operations, financial condition, capital requirements and other factors that our Board may deem relevant.
Securities Authorized for Issuance Under Equity Compensation Plans
For information regarding securities authorized for issuance under our equity compensation plans, see Part III, Item 12, “Security Ownership of Certain Beneficial Owners and Management and Related Stockholder Matters.”
Performance Graph
This performance graph below shall not be deemed “soliciting material” or to be “filed” with the SEC for purposes of Section 18 of the Exchange Act, or otherwise subject to the liabilities under that Section, and shall not be deemed to be incorporated by reference into this Annual Report on Form 10-K or any other filing of Alignment Healthcare, Inc. under the Exchange Act or the Securities Act, whether made before or after the date hereof and irrespective of any general incorporation language in any such filing, except to the extent that we specifically incorporate this information by reference therein.
The graph set forth below compares the cumulative total stockholder return on our common stock between March 26, 2021 (the date our common stock commenced trading on the Nasdaq Global Select Market) and December 31, 2021, with the cumulative total return of (a) the Nasdaq Healthcare Index and (b) the S&P 500, over the same period. This graph assumes the investment of $100 on March 26, 2021 in our common stock, the Nasdaq Healthcare Index, and the Nasdaq S&P 500 and assumes the reinvestment of dividends, if any. The graph assumes our closing sales price on March 26, 2021 of $17.31 per share as the initial value of our common stock and not the initial offering price to the public of $18.00 per share.
The comparisons shown in the graph below are based upon historical data. We caution that the stock price performance shown in the graph below is not necessarily indicative of, nor is it intended to forecast, the potential future performance of our common stock.
COMPARISON OF CUMULATIVE TOTAL RETURN
Among Alignment Healthcare, Inc., the NASDAQ Healthcare Index and the S&P 500
65

|
3/26/2021 |
|
|
4/30/2021 |
|
|
5/31/2021 |
|
|
6/30/2021 |
|
|
7/31/2021 |
|
|
8/31/2021 |
|
|
9/30/2021 |
|
|
10/31/2021 |
|
|
11/30/2021 |
|
|
12/31/2021 |
|
||||||||||
Alignment Healthcare, Inc. (ALHC) |
$ |
100.00 |
|
|
$ |
153.32 |
|
|
$ |
145.75 |
|
|
$ |
135.01 |
|
|
$ |
120.34 |
|
|
$ |
102.08 |
|
|
$ |
92.32 |
|
|
$ |
114.73 |
|
|
$ |
93.65 |
|
|
$ |
81.22 |
|
Nasdaq Healthcare Index |
|
100.00 |
|
|
|
105.13 |
|
|
|
102.33 |
|
|
|
109.16 |
|
|
|
108.55 |
|
|
|
112.06 |
|
|
|
105.84 |
|
|
|
105.20 |
|
|
|
98.68 |
|
|
|
98.09 |
|
S&P 500 |
|
100.00 |
|
|
|
105.31 |
|
|
|
106.05 |
|
|
|
108.52 |
|
|
|
111.10 |
|
|
|
114.48 |
|
|
|
109.15 |
|
|
|
116.80 |
|
|
|
115.99 |
|
|
|
121.18 |
|
Recent Sales of Unregistered Securities
None.
Use of Proceeds from Public Offering of Common Stock
On March 25, 2021, our Registration Statement on Form S-1 (SEC File No. 333-253824) for the initial public offering of 27,200,000 shares of common stock was declared effective by the Securities and Exchange Commission. Our common stock began trading on March 26, 2021 on Nasdaq under the ticker symbol “ALHC.” The IPO closed on March 30, 2021, with us selling 21,700,000 shares of common stock and certain selling stockholders selling 5,500,000 shares of common stock, in each case at a price to the public of $18.00 per share. On April 6, 2021, pursuant to a partial exercise of the underwriters’ over-allotment option, certain selling stockholders sold an additional 3,314,216 shares of common stock at the IPO price. In the aggregate, the IPO generated approximately $361.6 million in net proceeds for the Company, which amount is net of approximately $24.4 million in underwriters’ discounts and commissions and offering costs of approximately $4.6 million. The IPO commenced on March 25, 2021 and terminated upon the partial exercise of the underwriters’ over-allotment options as described above. The representatives of the several underwriters of the IPO were Goldman Sachs & Co. LLC and Morgan Stanley & Co. LLC.
There has been no material change in the use of proceeds described in the final IPO prospectus filed with the SEC on March 29, 2021. We may use a portion of our net proceeds to acquire or invest in complementary businesses, products, services or technologies.
Purchase of Equity Securities by the Issuer and Affiliated Purchasers
None.
Item 6. [Reserved]
66
Item 7. Management’s Discussion and Analysis of Financial Condition and Results of Operations.
The following discussion should be read in conjunction with the consolidated financial statements and accompanying notes, which appear elsewhere in this Annual Report on Form 10-K. This discussion contains forward-looking statements that involve risks and uncertainties. Our actual results could differ materially from those anticipated in these forward-looking statements as a result of various factors, including those discussed below and elsewhere in this Annual Report on Form 10-K. See Part I. Item 1A. Risk Factors and Cautionary Note Regarding Forward-Looking Statements. For discussion of 2019 items and year-over-year comparisons between 2020 and 2019 that are not included in this 2021 Form 10-K, refer to "Management's Discussion and Analysis of Financial Condition and Results of Operations" found in our Form S-1 that was originally filed with the Securities and Exchange Commission on March 3, 2021 and our Form S-1 filed with the Securities and Exchange Commission on November 16, 2021.
Overview
Alignment is a next generation, consumer-centric platform designed to revolutionize the healthcare experience for seniors. We deliver this experience through our Medicare Advantage plans, which are customized to meet the needs of a diverse array of seniors. Our innovative model of consumer-centric healthcare is purpose-built to provide seniors with care as it should be: high quality, low cost and accompanied by a vastly improved consumer experience. We combine a proprietary technology platform and a high-touch clinical model that enhances our members’ lifestyles and health outcomes while simultaneously controlling costs, which allows us to reinvest savings back into our platform and products to directly benefit the senior consumer. We have grown Health Plan Membership, which we define as members enrolled in our HMO and PPO contracts, from approximately 13,000 at inception to over 86,000 as of December 31, 2021, representing a 31% compound annual growth rate across 38 markets and 4 states. We had approximately 92,700 Health Plan Members across these markets as of January 1, 2022. Our ultimate goal is to bring this differentiated, advocacy-driven healthcare experience to millions of senior consumers in the United States and to become the most trusted senior healthcare brand in the country.
Our model is based on a flywheel concept, referred to as our “virtuous cycle”, which is designed to delight our senior consumers. We start by listening to and engaging with our seniors in order to provide a superior experience in both their healthcare and daily living needs. Through our proprietary technology platform, Alignment's Virtual Application ("AVA"), we utilize data and predictive algorithms that are specifically designed to ensure personalized care is delivered to each member. When our information-enabled care model is combined with our member engagement, we are able to improve healthcare outcomes by, for example, reducing unnecessary hospital admissions, which in turn lowers overall costs. Our ability to manage healthcare expenditures while maintaining quality and member satisfaction is a distinct and sustainable competitive advantage. Our lower total healthcare expenditures allow us to reinvest our savings into richer coverage and benefits, which propels our growth in revenue and membership due to the enhanced consumer value proposition. As we grow, we continue to listen to and incorporate member feedback, and we are able to further enhance benefits and produce strong clinical outcomes. Our virtuous cycle, based on the principle of doing well by doing good, is highly repeatable and a core tenet of our ability to continue to expand in existing and new markets in the future.
It is this virtuous cycle, underpinned by continuous expansion and improvement in our technology platform, that has enabled us to achieve revenues of $1,167.8 million for the year ended December 31, 2021 and $959.2 million for the year ended December 31, 2020, representing a revenue compound annual growth rate of 37% from our founding in 2013 through the fourth quarter of 2021.
Medicare Advantage Background
Today, seniors are confronted with a healthcare landscape that is fragmented across disparate point solutions, tools and vendors, without an accessible, coordinated approach to comprehensive care delivery. Under the traditional Medicare fee-for-service ("FFS") model, seniors receive access to hospital insurance benefits (“Part A”) and outpatient services (“Part B”) directly from CMS. Original Medicare (Part A and B) does not include prescription drug coverage (“Part D”), and most seniors enrolled in original Medicare opt to obtain Part D and other protection for gaps in their coverage by purchasing costly Medicare supplement insurance plans. In contrast, Medicare Advantage plans are direct-to-consumer and provide a single point of care delivery for Part A, Part B and often Part D coverage. Medicare Advantage penetration of the Medicare market is rapidly increasing given the enhanced benefits and coverage that Medicare Advantage plans offer relative to traditional Medicare FFS. Industry projections have forecasted a continued increase in the Medicare Advantage penetration rate, such that the population using Medicare Advantage plans is expected to increase from 28 million in 2021 to 37 million in 2025 as Medicare Advantage penetration accelerates from 44% to approximately 47%.
67
Medicare Advantage allows one entity to influence the entirety of a senior’s healthcare through a singular, direct-to-consumer product. We contract with CMS under the Medicare Advantage program to provide health insurance coverage to Medicare eligible persons under HMO and PPO plans in exchange for a payment per member per month ("PMPM"). The PMPM payment varies based on geography, CMS Star ratings and certain population-specific risk factors. Under these value-based contracts, we assume the economic risk of funding our members’ healthcare, supplemental benefits and related administration costs. By transferring the economic risk to managed care companies like Alignment, CMS has enabled us to focus on proactive, cross-disciplinary care targeted at improving health outcomes and lowering unnecessary healthcare expenditures.
The Medicare Advantage regulatory framework is designed to reward plans that achieve the triple aim of high-quality care, low costs and better experience. CMS payments to Medicare Advantage plans are allocated in each county or region based on a bidding system. Each plan submits a bid based on its estimated costs per enrollee for services covered under Medicare Parts A and B. Plans that have a low enough cost structure to bid under the benchmark are entitled to rebates, which enable those plans to offer enhanced supplemental benefits and medical coverage to their members, which in turn boosts membership growth and therefore revenue. CMS further measures Medicare Advantage beneficiaries’ clinical outcomes and experience with their health plans and the healthcare system through a Five Star Quality Rating System. Medicare Advantage plans are eligible to receive additional economic incentives based on their Star rating. Due to the competitive nature of CMS’s bidding system, only those plans that are able to provide low cost and high-quality outcomes will be able to offer enhanced benefit options, which is critical to achieving sustainable membership and growth on a long-term basis.
Under the Medicare Advantage system, our members typically enroll with us for a one-year period that can be renewed on an annual basis, resulting in revenue that is principally based on a subscription-like PMPM recurring revenue model. This model provides us with significant visibility into our short-term financial performance, particularly given that the substantial majority of our members continue to choose Alignment after their initial selection year. Further, our HMO and PPO plans covered under Medicare Advantage contracts with CMS are generally renewed for a calendar year term, unless CMS notifies us of its decision not to renew by May 1 of the year in which the contract would end. When carefully managed, this annual renewal process provides a measure of stability and predictability to our short-term revenue streams, allowing us to focus on improving health quality outcomes and lowering healthcare expenditures for our population through enhanced member care on a long-term basis.
Factors Affecting Our Performance
Our proprietary technology platform, AVA, is a key element of our business with capabilities that we expect to impact our future performance. AVA enables us to personalize and manage our member relationships, care quality and experience, and to coordinate and manage risk with our provider partners. AVA’s unified platform, analytical tools and data across the healthcare ecosystem enable us to produce consistent outcomes, unit economics and support new member growth. Additionally, our historical financial performance has been, and we expect our financial performance in the future will be, driven by our ability to:
Capitalize on Our Existing Market Growth Opportunity
Our ability to attract and retain members to grow in our existing markets depends on our ability to offer a superior value proposition. Providing better care and richer benefits that lead to higher member satisfaction at a lower cost generates greater performance for us under the Medicare Advantage program, which we can then use to fund our growth. We have proven that we can compete against, and take market share from, large established players in highly competitive markets. According to CMS data, we were one of the top three Medicare Advantage Organizations in terms of HMO net members growth in our California counties between 2016 and 2022. Further, over 80% of our membership growth came from “plan switchers”, which are seniors who joined Alignment from other Medicare Advantage plans as opposed to joining a Medicare Advantage plan for the first time.
We attract new members through both our internal and external sales channels. Our internal sales channel consists of Alignment representatives, both in the field and telephonically, who market and sell Alignment’s portfolio of products to prospective members. This channel also includes our new sales to members who sign up using Alignment’s direct online enrollment tools. Our external sales channel consists of partnerships with third party broker channels who sell Alignment products alongside competing products. These third-party organizations also consist of in-person, telephonic and online sales distribution channels. Our growth will depend on our continued success in marketing our products through these channels.
We believe that significant growth opportunities remain in our current geographic footprint which includes markets with some of the largest senior populations in the country. There are approximately 3.7 million Medicare-eligible individuals enrolled in Medicare Advantage plans in our existing 38 counties, of which our approximately 92,700 Health Plan Members represents only 3% market share. In fact, California has the greatest number of Medicare eligibles of any state in the country, and has more Medicare eligibles than the smallest 19 states combined. We believe that there are still significant opportunities for future growth even in our most mature markets where we have a 10-20% market share. As we gain brand recognition, expand our membership base and grow market share in our existing markets, we are also generally able to lower our incremental member acquisition costs. These savings can then be reinvested into our business to continue to allow us to offer innovative product offerings. We believe that we are well placed to continue to gain share in our current markets due to our strong track record of reducing
68
healthcare costs, providing exceptional care and a superior experience, establishing innovative partnerships with a wide array of providers in order to expand our network and offering a best-in-class member experience.
Additionally, we are evaluating other opportunities to leverage our historical investments in our technology platform and our comprehensive clinical model across our existing and potentially new geographies. As an example, we recently entered into CMS Innovation Center’s Direct Contracting program, which allows us to partner directly with physicians to help manage their Medicare FFS patient populations and participate in the upside and downside risk associated with managing the health of such patients. As of December 31, 2021, we had approximately 5,400 members in our DCE arrangement with our clinician partners in North Carolina. While still early, we believe this DCE partnership is indicative of the value we can potentially deliver to a broader set of seniors in traditional Medicare over time.
Drive Growth and Consistent Outcomes Through New Market Expansion
Given our track record of delivering exceptional results and delighting consumers in our existing markets, we recently launched our national expansion strategy guided by our disciplined approach to identifying new markets. While our growth opportunity in our existing geographic footprint is robust, we believe that we can expand into new markets by utilizing our proven, replicable model of offering richer coverage and benefits at a lower cost, coupled with a superior consumer experience. Over the last three years we have expanded into approximately 10 new markets per year and have increased our Medicare eligible population opportunity by 2.3 million through geographic expansion in 2020-2022.
We enter new markets with the goal of building brand awareness across our key stakeholders to achieve meaningful market share over time. We intend to focus on markets with significant senior populations where we expect to be able to replicate our model most effectively. Our analytical framework for selecting new markets to enter evaluates a number of factors, including: the presence of aligned provider partners, our ability to compete effectively based on the richness of our products, and our ability to build and deploy local market care delivery teams efficiently. Our methodical approach to new market expansion requires long-term planning and investment, given the lead time required to develop each market opportunity. We typically begin targeting new markets 12-18 months prior to product launch, during which period we develop local provider and broker contracts and relationships, apply for new state licenses and/or obtain approvals, obtain CMS approval, and file our bids for the following calendar year. We then further invest in new market annual enrollment period ("AEP") sales and marketing, as well as our local provider and clinical teams to support our growth and operational efforts, all prior to enrolling any new members. Upon product launch in a new market, and depending upon the nature of our contracting entry strategy and the pace of our new member growth over the first two to three years, we may in some instances incur losses over the first several years as we establish ourselves and the Alignment model in the community.
We believe that investment in new market development is required to drive sustained long-term growth, and our willingness to make such investments is underpinned by our proven success in a diverse array of markets across our existing geographic footprint. Enabled by AVA, we have been successful in rural, urban and suburban markets, as well as markets with varying degrees of provider and health system competition and control. Our existing markets also feature a diverse array of membership profiles across ethnicities, income levels and acuity. In a wide variety of geographies, population mixes and local market conditions, we have demonstrated success in achieving strong medical benefit ratio ("MBR") performance and consistently high satisfaction among our members.
AVA gives us the analytics and tools to replicate this value creation across a variety of operating and contracting models with our provider partners, which we believe provides us with the capability to successfully grow and scale in new markets in a methodical and manageable way. We have already identified additional markets in the Western, Southern, Northeastern and Great Lakes regions of the United States for potential expansion in 2022 and beyond, with a focus on higher-density population centers and adjacent counties, and believe that expansion into new markets and new states will continue to extend our growth opportunities for the foreseeable future.
Provide Superior Service, Care and Consumer Satisfaction
We are highly focused on providing superior service and care to our members and on maintaining high levels of consumer satisfaction, which are key to our financial performance and growth. The CMS Five Star Quality Rating System provides economic incentives to Medicare Advantage plans that achieve higher Star ratings by (i) meeting certain care criteria (such as completing particular preventative screening procedures or ensuring proper follow-up care is provided for specific conditions or episodes) and (ii) receiving high member satisfaction ratings. These incentives impact financial performance in the year following the CMS Rating Year (for example, CMS’s announcement of the 2022 Ratings occurred in the second half of 2021, and will impact our financial performance in 2023). Historically, we have earned additional bonus payments from CMS based on our performance under CMS’s Five Star Quality Rating System. For the last five years (CMS Rating Years 2018-2022), over 98% of our California members have been in a CMS contract achieving at least a 4 Star overall rating (the remaining members were in a CMS contract that had too few members to be measured). This is important to our financial performance, as (i) earning a 4 Star rating generally allows us to receive a 5% bonus to our revenue benchmark rate in our bids (subject to certain county-level adjustments), and (ii) a 4.5 Star rating allows us to retain a larger portion of the savings our model creates relative to our
69
benchmark by increasing our rebate percentage from 65% to 70% of savings, both of which allow us to offer richer coverage and supplemental benefits.
We believe our dedication to serving our seniors and our relentless focus on delivering quality outcomes has been instrumental in our ability to deliver a 4 Star or better rating for the past five years. Our Medicare Advantage plans in California currently have a 4 Star rating, and our plans in Nevada, North Carolina and Arizona do not yet have independent Star ratings due to our limited operating history in those markets. As a result, payments in Nevada and North Carolina are expected to be based on our Star rating in California for the next several years. We have invested heavily in internal clinical and non-clinical resources focused on driving important workstreams such as preventative care, medication adherence and care coordination, which impact our ability to achieve higher ratings in the CMS Star system. We also work hand-in-hand with our external community of providers to remediate gaps in care, which has directly resulted in our ability to maintain strong Stars performance. Both our internal and external efforts are facilitated by AVA, which helps to ensure that members are getting the right care at the right time.
In addition, our ability to broadly achieve and maintain superior member satisfaction enables us to increase our member engagement and retention. Our success in achieving member satisfaction is evidenced by our NPS of greater than 60 overall and greater than 75 for our Care Anywhere members, compared to an industry average NPS ranging from 30-40, based on data collected and made publicly available by Customer Guru, a commercial provider of member satisfaction tracking services. Further, in CMS’s most recent annual member survey, which asks members to evaluate our products across a variety of criteria, our HMO contract with CMS in California, which represents 98% of our California membership, scored a 5.0 Star rating on members’ rating of the health plan. These results reflect our ongoing efforts to continuously delight our senior consumers. See “Risk Factors —We may not be successful in maintaining or improving our Star ratings in future years, which may have a direct and substantial adverse impact on our revenue.”
Effectively Manage the Quality of Care to Improve Member Outcomes
Our care delivery model is based on a clinical continuum through which we have created a highly personalized experience that is unique to each member depending on their personal health and circumstances. Utilizing data and predictive analytics generated by AVA, our clinical continuum separates seniors into four categories in order to provide optimized care for every stage of a senior’s life: healthy, healthy utilizer, pre-chronic and chronic. We partner with our broader network of community providers to service members in our non-chronic categories, and we have developed a Care Anywhere program implemented by our internal clinical teams to care for our higher risk and/or chronically ill members. In calendar year 2021, only approximately 10% of our members fell within the chronically ill category; however, they accounted for more than 73% of our institutional claims. Therefore, we believe that giving these members the best possible preventative care is not only essential for optimizing clinical outcomes, but is also key to building a successful clinical model that allows us to manage the financial risk of our population as a whole.
By investing in our members’ care proactively, our model has consistently reduced unnecessary and costly care while improving the quality of our members’ lifestyle and healthcare experience. In 2021, we achieved a hospitalization rate of approximately 156 hospitalizations per every 1,000 at-risk members, which is approximately 38% better than the 2019 Medicare FFS performance (based on data from CMS’s Geographic Variation Public Use File) in our markets. Further, we have achieved approximately 155-165 inpatient admissions per thousand on our at-risk membership for the last five years in a row in spite of our significant membership growth over that period of time. This performance is a critical indicator of not only quality of care but also our financial outcomes. By delivering superior care and preventing avoidable utilization of the healthcare system, we are able to reduce our claims expenditures in some of our largest medical expense categories, which translates to superior MBR financial performance and ultimately the ability to offer richer products in the market.
Achieve Superior Unit Economics
As our senior population ages their healthcare needs become more frequent and complex. To combat the healthcare cost increases that typically result, we proactively look to (i) connect with our population early in their enrollment with Alignment to assess their care needs, (ii) develop care plans and engage those members with more chronic, complex health challenges in our clinical model, and (iii) continue to monitor and evaluate our healthier members in a preventative fashion over time. Given the Medicare Advantage payment mechanism and the retention of the vast majority of our members who continue to choose Alignment after their initial selection year, we are able to focus our efforts on driving favorable long-term health outcomes for our entire population.
As a result, our clinical model efforts have demonstrated the ability to lower the MBRs of our returning members. For example, new members joining our plans for whom we retain at least a majority of claim risk typically average MBRs between 85-90%, whereas our longest tenured members, who have been members of our plans for 5+ years and for whom we retain at least a majority of claim risk, have MBRs that typically average in the 70-75% range, with corresponding improvement in gross profit PMPM performance for such members, in each case excluding the costs of our clinical model investments (which are comprised of the annual expenditures we incur to deploy our internal clinical resources, including the costs of employing doctors, nurses, case managers, social workers and medical supply costs, among others). Furthermore, we’ve been able to maintain a 70-78%
70
MBR range (excluding the costs of our clinical model investments) for our year 5+ at-risk members throughout the COVID-19 pandemic despite the adverse impact COVID has had on our claims per member per month and revenue per member per month across cohorts. We believe this is evidence of our ability to manage the financial risk of our members as they age, and that these favorable underlying unit economic trends translate directly to our ability to continue to deliver a richer product to the marketplace. With this dynamic in mind, our consolidated MBR may be impacted year-to-year based on our pace of new member growth and mix of members by cohort. However, we believe our ability to sustain MBR performance improvement over time positions us well to invest in new member growth to drive long-term financial performance.
Investments in our Platform and Growth
We plan to continue to invest in our business in order to further develop our AVA platform, pursue new expansion opportunities and create innovative product offerings. We have invested significant time, effort and capital into developing our proprietary technology platform. Our member and provider interactions, cost management and consumer engagement are supported by AVA, and we anticipate continuing to invest in our technology to incorporate new plan designs, benefits and care protocols to enrich the consumer experience. We believe that investing in AVA to continuously improve its capacity, functionality and effectiveness will ensure that AVA continues to provide us with the most advanced tools to anticipate and address the evolving needs of our growing membership.
In order to maintain a differentiated value proposition for our members, we continue to invest in innovative product offerings and supplementary benefits to meet the evolving needs of the senior consumer. Additionally, we anticipate further investments in our business as we expand into new markets and pursue strategic acquisitions, which we expect will primarily be focused on healthcare delivery groups in key geographies, standalone and provider-sponsored Medicare Advantage plans and other complementary risk bearing assets.
A key part of our growth strategy is to carefully balance the short-term costs of our investments against the long-term benefits that they can achieve for our business and our members. We plan to balance these investments in our platform and in future growth with a continued focus on managing our results of operations and investing judiciously. Accordingly, in the short term these activities may increase our net losses, but in the longer term we anticipate that these investments will positively impact our business and results.
Seasonality to our Business
Our operational and financial results will experience some variability depending upon the time of year in which they are measured. This variability is most notable in the following areas:
Member Growth
We experience the largest portion of member growth during the first quarter, when plan enrollment selections made during AEP from October 15th through December 7th of the prior year take effect. While we also add members throughout the year, including during CMS’s Open Enrollment Period and Special Enrollment Periods when certain eligible individuals can enroll in Medicare Advantage after January 1, we expect to see a majority of our member growth occur January 1 of a given calendar year.
Continued Investments in Growth
We expect to continue to focus on driving long-term growth and the scalability of our approach through investments in our provider network, care model, AVA technology platform, new market expansions and marketing efforts. Due to the timing of many of these investments, we typically incur a greater level of investment in the second half of the year relative to the first half of the year, causing the second half of the year to often be less profitable than the first half of the year. Although the investments we make may adversely affect our operating results in the near term, we believe that they will be important drivers of our long-term performance.
Per-Member Revenue
Our revenue per member is a function of the county in which our members reside, our CMS Star rating for a given payment year, and our ability to accurately and appropriately document the acuity of a member. In January of each year, CMS revises the risk adjustment factor for each member based upon health conditions documented in the prior year, leading to a change in per-member revenue. As the year progresses, our per-member revenue often declines as new members join us, typically with less complete or accurate documentation (and therefore lower risk-adjustment scores), and senior mortality disproportionately impacts our higher-acuity (and therefore greater revenue) members. Further, given that we are able to reasonably project what our final risk adjustment payment will be after 100% of encounter data is submitted to and accepted by CMS, we accrue for our projected final risk adjustment payment over the course of the year, which is subject to adjustment up or down during the year as encounter data continues to develop for the prior calendar year.
71
Medical Costs
Medical costs will vary seasonally depending on a number of factors, but most significantly the weather. Certain illnesses, such as the influenza virus, are far more prevalent during colder months of the year, which will result in an increase in medical expenses during these time periods. We therefore expect to see higher levels of per-member medical costs in the first and fourth quarters. We also expect to experience an impact should there be a pandemic such as COVID-19, which may result in increased or decreased total medical costs depending upon the severity of the infection, the duration of the infection and the impact to the supply and availability of healthcare services for our members. We develop estimates for medical expenses incurred but not yet paid (“IBNP”) using an actuarial process that is consistently applied and centrally controlled. Medical expenses payable includes claims reported but not yet paid, estimates for claims incurred but not reported, and estimates for the costs necessary to process unpaid claims at the end of each period. These actuarial methods consider factors such as historical data for payment patterns, cost trends, product mix, seasonality, utilization of healthcare services and other relevant factors.
Prescription Drug Coverage
The design of our prescription drug coverage (Medicare Part D) results in coverage that varies as a member’s cumulative out-of-pocket costs pass through successive stages of a member’s plan period, which begins annually on January 1 for renewals. These plan designs generally result in us sharing a greater portion of the responsibility for total prescription drug costs in the early stages of the year and less in the latter stages, which typically results in a higher MBR on our Part D program in the first half of the year relative to the second half of the year.
Key Business Metrics
In addition to our GAAP financial information, we review a number of operating and financial metrics, including the following key metrics, to evaluate our business, measure our performance, identify trends affecting our business, formulate business plans and make strategic decisions.
|
|
Year Ended December 31, |
|
|
|
|
||||||
(dollars in '000's, except percentages) |
|
2021 |
|
|
2020 |
|
|
% Change |
|
|||
Health plan membership |
|
|
86,100 |
|
|
|
68,323 |
|
|
|
26.0 |
% |
Medical benefits ratio |
|
|
87.6 |
% |
|
|
82.6 |
% |
|
|
5.0 |
% |
Revenues |
|
$ |
1,167,773 |
|
|
$ |
959,222 |
|
|
|
21.7 |
% |
Net loss attributable to Alignment Healthcare, Inc. |
|
$ |
(195,286 |
) |
|
$ |
(22,926 |
) |
|
NM(2) |
|
|
Adjusted EBITDA(1) |
|
$ |
(33,116 |
) |
|
$ |
11,852 |
|
|
NM(2) |
|
|
Adjusted gross profit (1) |
|
$ |
144,370 |
|
|
$ |
166,596 |
|
|
|
-13.3 |
% |
(1) See "Adjusted EBITDA" and "Adjusted Gross Profit" below for reconciliation to the most directly comparable financial measure calculated in accordance with GAAP and related disclosures.
(2) Not meaningful
Health Plan Membership
We define Health Plan Membership as the number of members enrolled in our HMO and PPO contracts (the “Alignment Health Plan”) as of the end of a reporting period. We believe this is an important metric to assess growth of our underlying business, which is indicative of our ability to consistently offer a superior value proposition to seniors. This metric excludes third party payor members with respect to which we are at-risk for managing their healthcare expenditures, which represented 600 members and 7,674 members as of December 31, 2021 and December 31, 2020, respectively. It also excludes the approximately 5,400 traditional Medicare seniors for which we are at-risk for managing their healthcare expenditures through our DCE contracts with CMS.
Adjusted Gross Profit and Medical Benefits Ratio, or MBR
Adjusted gross profit is a non-GAAP financial measure that we define as loss from operations before depreciation and amortization, clinical equity-based compensation expense, and selling, general, and administrative expenses. Adjusted gross profit is a key measure used by our management and Board to understand and evaluate our operating performance and trends before the impact of our consolidated selling, general and administrative expenses.
Adjusted gross profit should not be considered in isolation of, or as an alternative to, measures prepared in accordance with GAAP. There are a number of limitations related to the use of Adjusted gross profit in lieu of loss from operations, which is the most directly comparable financial measure calculated in accordance with GAAP.
Our use of the term Adjusted gross profit may vary from the use of similar terms by other companies in our industry and accordingly may not be comparable to similarly titled measures used by other companies.
72
Adjusted gross profit is reconciled as follows:
|
|
Year Ended December 31, |
|
|||||
|
|
2021 |
|
|
2020 |
|
||
(dollars in thousands) |
|
|
|
|
|
|
||
Loss from operations |
|
$ |
(178,072 |
) |
|
$ |
(5,263 |
) |
Add back: |
|
|
|
|
|
|
||
Equity-based compensation (medical expenses) |
|
|
15,418 |
|
|
|
— |
|
Depreciation (medical expenses) |
|
|
220 |
|
|
|
366 |
|
Depreciation and amortization |
|
|
15,813 |
|
|
|
15,095 |
|
Selling, general, and administrative expenses |
|
|
290,991 |
|
|
|
156,398 |
|
Total add back |
|
|
322,442 |
|
|
|
171,859 |
|
Adjusted gross profit |
|
$ |
144,370 |
|
|
$ |
166,596 |
|
Adjusted gross profit % |
|
|
12.4 |
% |
|
|
17.4 |
% |
We calculate our MBR by dividing total medical expenses, excluding depreciation and equity-based compensation, by total revenues in a given period. We believe our MBR is an indicator of our gross profit for our Medicare Advantage plans and demonstrates the ability of our clinical model to produce superior outcomes by identifying and providing targeted care to our high-risk members resulting in improved member health and reduced total population medical expenses. We expect that this metric may fluctuate over time due to a variety of factors, including our pace of new member growth given that new members typically join Alignment with higher MBRs, while our model has demonstrated an ability to improve MBR for a given cohort over time.
When we determine, on an annual basis, whether we have satisfied the CMS minimum Medical Loss Ratio (“MLR”) of 85%, adjustments are made to the MBR calculation to include certain additional expenses related to improving the quality of care provided, and to exclude certain taxes and fees, in each case as permitted or required by CMS and applicable regulatory requirements.
Adjusted EBITDA
Adjusted EBITDA is a non-GAAP financial measure that we define as net loss before interest expense, income taxes, depreciation and amortization expense, reorganization and transaction-related expenses and equity-based compensation expense. Adjusted EBITDA is a key measure used by our management and our Board to understand and evaluate our operating performance and trends, to prepare and approve our annual budget and to develop short and long-term operating plans. In particular, we believe that the exclusion of the amounts eliminated in calculating Adjusted EBITDA provides useful measures for period-to-period comparisons of our business. Given our intent to continue to invest in our platform and the scalability of our business in the short to medium-term, we believe Adjusted EBITDA over the long term will be an important indicator of value creation.
Adjusted EBITDA should not be considered in isolation of, or as an alternative to, measures prepared in accordance with GAAP. There are a number of limitations related to the use of Adjusted EBITDA in lieu of net loss, which is the most directly comparable financial measure calculated in accordance with GAAP.
Our use of the term Adjusted EBITDA may vary from the use of similar terms by other companies in our industry and accordingly may not be comparable to similarly titled measures used by other companies.
Adjusted EBITDA is reconciled as follows:
|
|
Year Ended |
|
|||||
|
|
2021 |
|
|
2020 |
|
||
(dollars in thousands) |
|
|
|
|
|
|
||
Net loss attributable to Alignment Healthcare, Inc. |
|
$ |
(195,286 |
) |
|
$ |
(22,926 |
) |
Add back: |
|
|
|
|
|
|
||
Interest expense |
|
|
17,443 |
|
|
|
16,931 |
|
Depreciation and amortization |
|
|
16,033 |
|
|
|
15,461 |
|
|
|
|
|
|
|
|
||
EBITDA |
|
|
(161,810 |
) |
|
|
9,466 |
|
Equity-based compensation(1) |
|
|
121,999 |
|
|
|
2,124 |
|
Reorganization and transaction-related expenses(2) |
|
|
4,585 |
|
|
|
262 |
|
Acquisition expenses(3) |
|
|
2,110 |
|
|
|
— |
|
Adjusted EBITDA |
|
$ |
(33,116 |
) |
|
$ |
11,852 |
|
73
(1) 2021 represents equity-based compensation related to the timing of the IPO, including the previously issued stock appreciation rights ("SARs") liability awards, modifications related to transaction vesting units, and new grants made in conjunction with the IPO. 2020 represents equity-based compensation related to the Incentive Units (as defined in Footnote 1 to our consolidated financial statements, included in this Annual Report).
(2) Represents legal, professional, accounting and other advisory fees related to the Corporate Reorganization and the IPO that are considered non-recurring and non-capitalizable.
(3) Represents acquisition-related fees, such as legal and advisory fees, that are non-capitalizable.
Results of Operations
We operate and manage our business as a single reporting and operating segment, which is to provide healthcare services to our seniors. The components of our results of operations are as follows:
Revenues
Our revenue is comprised of earned premiums and other revenue. We receive and record premium revenue on a monthly basis from the federal government based on our contract with CMS. In accordance with this arrangement, we assume the responsibility for the outcomes and the economic risk of funding our members’ healthcare, supplemental benefits and related administration costs. We recognize premium revenue in the month that members are entitled to receive healthcare services, and premiums collected in advance are deferred. The monthly premium that we receive under our contract with CMS includes a PMPM which is adjusted based on certain risk factors derived from medical diagnoses for our members. The adjustments are estimated by projecting the ultimate annual premium and are recognized ratably during the year, with adjustments in each period to the amount of revenue recognized to reflect changes in the estimated ultimate premium. Premiums are also recorded net of estimated uncollectible amounts and retroactive membership adjustments.
Our recognized premium revenue for the Alignment Health Plan is subject to a minimum annual MLR of 85%. The MLR represents medical costs as a percentage of premium revenue. The Code of Federal Regulations defines what specifically constitutes medical expenses and premium revenue for the MLR test, and if the minimum MLR is not met, we are required to remit a portion of the premiums back to the federal government. The amount remitted, if any, is recognized as an adjustment to premium revenues in the consolidated statement of operations. There were no amounts payable for the MLR test as of December 31, 2021 or 2020.
The premiums we receive from CMS for our members are based on the annual bid that we submit to CMS. These payments represent revenues for providing healthcare coverage, including Medicare Part D benefits. Under the Medicare Part D program, members receive standard drug benefits. We may also provide enhanced benefits at our own expense. We recognize revenue for providing this insurance coverage in the month that members are entitled to receive healthcare services. Our CMS payment related to Medicare Part D is subject to risk sharing through the Medicare Part D risk corridor provisions. See “—Critical Accounting Policies—Revenue” below.
Our capitation revenue consists primarily of capitated fees for medical care services provided by us under arrangements with our third-party payors and from CMS related to our Direct Contracting Entities ("DCE"). Under those arrangements, we receive a PMPM payment for a defined member population, and we are responsible to provide health care services to the member population over the contract period. We are solely responsible for the cost of health care services related to the member population and in some cases, providing supplemental benefits provided by us to the members. We act as a principal in arranging for and controlling the services provided by our provider network and we are at risk for arranging and providing health care services. Capitation revenue is recognized in the month that members are entitled to receive health care services and capitation revenue collected in advance is deferred. We report this capitation revenue as part of earned premiums.
Expenses
Medical Expenses. Medical expenses includes claim payments, capitation payments, pharmacy costs net of rebates, allocations of certain centralized expenses, supplemental benefits, internal care delivery expenses and various other costs incurred to provide health insurance coverage to members, as well as estimates of future payments to hospitals and others for medical care previously provided to our members.
We have contracts with a network of hospitals, physicians, and other providers and compensate those providers and ancillary organizations based on contractual arrangements or CMS Medicare compensation guidelines. We pay these contracting providers either through fee-for-service arrangements in which the provider is paid negotiated rates for specific services provided, or through capitation payments, which represent monthly contractual fees disbursed for each member regardless of medical services provided to the member. We are ultimately responsible for the entirety of the cost of healthcare services related to our member population, in addition to supplemental benefits that we provide to our seniors.
Capitation-related expenses are recorded on an accrual basis during the coverage period. Expenses related to fee-for-service contracts are recorded in the period in which the related services are dispensed.
74
Pharmacy costs represent payments for members’ prescription drug benefits, net of rebates from drug manufacturers. Receivables for such pharmacy rebates are included in accounts receivable in the consolidated balance sheet.
Selling, General and Administrative Expenses. Selling, general and administrative expenses consist of (i) personnel expenses including salaries, bonuses, equity-based compensation expense and benefits for non-clinical employees; (ii) all corporate technology, occupancy costs and allocated overhead costs; (iii) professional and outside services, including external vendors and professional services; (iv) costs associated with administering our contracts with CMS, including claims adjudication, member and concierge services, provider engagement, and other health plan functions; and (v) central and community-based advertising costs to generate greater awareness, engagement and retention among our current and prospective members, as well as the infrastructure required to support all of our marketing efforts and ongoing commission payments. These expenses also include certain growth expenditures, including business development and various new market expansion activities. Our investments in our sales, marketing and other growth activities are an important component of our SG&A in a typical year given our desire to continue to grow on an accelerated trajectory. We anticipate continuing to invest heavily in our growth efforts in the near future, which we believe will be an important driver of long-term value creation. We expect selling, general and administrative expenses to increase in absolute dollars as we incur costs associated with being a public company and growing our business.
Depreciation and Amortization. Depreciation and amortization expenses are primarily attributable to our capital investment and consist of fixed asset depreciation, amortization of intangibles considered to have definite lives and amortization of capitalized internal-use software costs.
Other Expense
Interest Expense. Interest expense consists primarily of interest payments on our outstanding borrowings under our Term Loan (as defined below). See “—Liquidity and Capital Resources—Term Loan.”
Other (Income) Expenses. Other (income) expenses consist primarily of gains or losses on the disposition of assets.
The following table sets forth our consolidated statements of operations data for the periods indicated:
|
|
Year Ended December 31, |
|
|||||
|
|
2021 |
|
|
2020 |
|
||
(dollars in thousands) |
|
|
|
|
|
|
||
Revenues: |
|
|
|
|
|
|
||
Earned premiums |
|
$ |
1,167,085 |
|
|
$ |
955,393 |
|
Other |
|
|
688 |
|
|
|
3,829 |
|
Total revenues |
|
|
1,167,773 |
|
|
|
959,222 |
|
Expenses: |
|
|
|
|
|
|
||
Medical expenses |
|
|
1,039,041 |
|
|
|
792,992 |
|
Selling, general and administrative expenses |
|
|
290,991 |
|
|
|
156,398 |
|
Depreciation and amortization |
|
|
15,813 |
|
|
|
15,095 |
|
Total expenses |
|
|
1,345,845 |
|
|
|
964,485 |
|
Loss from operations |
|
|
(178,072 |
) |
|
|
(5,263 |
) |
Other expenses: |
|
|
|
|
|
|
||
Interest expense |
|
|
17,443 |
|
|
|
16,931 |
|
Other (income) expenses |
|
|
(229 |
) |
|
|
732 |
|
Total other expenses |
|
|
17,214 |
|
|
|
17,663 |
|
Loss before income taxes |
|
|
(195,286 |
) |
|
|
(22,926 |
) |
Provision for income taxes |
|
|
— |
|
|
|
— |
|
Net loss attributable to Alignment Healthcare, Inc. |
|
$ |
(195,286 |
) |
|
$ |
(22,926 |
) |
The following table sets forth our consolidated statements of operations data expressed as a percentage of total revenues for the periods indicated:
75
|
|
Year Ended December 31, |
|
|||||
|
|
2021 |
|
|
2020 |
|
||
(% of revenue) |
|
|
|
|
|
|
||
Revenues: |
|
|
|
|
|
|
||
Earned premiums |
|
|
100 |
% |
|
|
100 |
% |
Other |
|
|
— |
|
|
|
— |
|
Total revenues |
|
|
100 |
|
|
|
100 |
|
Expenses: |
|
|
|
|
|
|
||
Medical expenses |
|
|
89 |
|
|
|
83 |
|
Selling, general and administrative expenses |
|
|
25 |
|
|
|
16 |
|
Depreciation and amortization |
|
|
1 |
|
|
|
2 |
|
Total expenses |
|
|
115 |
|
|
|
101 |
|
Loss from operations |
|
|
(15 |
) |
|
|
(1 |
) |
Other expenses: |
|
|
|
|
|
|
||
Interest expense |
|
|
2 |
|
|
|
2 |
|
Other (income) expenses |
|
|
— |
|
|
|
— |
|
Total other expenses |
|
|
2 |
|
|
|
2 |
|
Loss before income taxes |
|
|
(17 |
) |
|
|
(2 |
) |
Provision for income taxes |
|
|
— |
|
|
|
— |
|
Net loss attributable to Alignment Healthcare, Inc. |
|
|
(17 |
)% |
|
|
(2 |
)% |
Revenues
|
|
Year Ended |
|
|
Change |
|
||||||||||
|
|
2021 |
|
|
2020 |
|
|
$ |
|
|
% |
|
||||
(dollars in thousands) |
|
|
|
|
|
|
|
|
|
|
|
|
||||
Revenues: |
|
|
|
|
|
|
|
|
|
|
|
|
||||
Earned premiums |
|
$ |
1,167,085 |
|
|
$ |
955,393 |
|
|
$ |
211,692 |
|
|
|
22.2 |
% |
Other |
|
|
688 |
|
|
$ |
3,829 |
|
|
|
(3,141 |
) |
|
|
(82.0 |
)% |
Total revenues |
|
$ |
1,167,773 |
|
|
$ |
959,222 |
|
|
$ |
208,551 |
|
|
|
21.7 |
% |
Revenues. Revenues were $1,167.8 million and $959.2 million for the years ended December 31, 2021 and 2020, respectively, an increase of $208.6 million or 21.7%. The increase was driven primarily by growth in Alignment’s Health Plan membership in 2021 as compared to 2020, which resulted in Health Plan premium revenue growth of 28.4% year over year for the year ended December 31, 2021. Health Plan premium revenue growth was offset by a reduction in capitation revenue from third party payors due to a contract that terminated on December 31, 2020.
Expenses
|
|
Year Ended |
|
|
Change |
|
||||||||||
|
|
2021 |
|
|
2020 |
|
|
$ |
|
|
% |
|
||||
(dollars in thousands) |
|
|
|
|
|
|
|
|
|
|
|
|
||||
Expenses: |
|
|
|
|
|
|
|
|
|
|
|
|
||||
Medical expenses |
|
$ |
1,039,041 |
|
|
$ |
792,992 |
|
|
$ |
246,049 |
|
|
|
31.0 |
% |
Selling, general and administrative expenses |
|
|
290,991 |
|
|
|
156,398 |
|
|
|
134,593 |
|
|
|
86.1 |
% |
Depreciation and amortization |
|
|
15,813 |
|
|
|
15,095 |
|
|
|
718 |
|
|
|
4.8 |
% |
Total expenses |
|
$ |
1,345,845 |
|
|
$ |
964,485 |
|
|
$ |
381,360 |
|
|
|
39.5 |
% |
Medical Expenses. Medical expenses were $1,039.0 million and $793.0 million for the year ended December 31, 2021 and 2020, respectively, an increase of $246.0 million, or 31.0%. The increase was driven primarily by growth in Alignment’s Health Plan membership in 2021 as compared to 2020. In addition, the increase was partially due to $15.4 million of equity-based compensation recorded to medical expenses related to the IPO. Overall, medical expenses grew at a higher rate than total revenues due to a combination of mix shift of membership away from Alignment's third-party payor members from 2020 to 2021, and the impact of COVID-19 on utilization in 2021. For January and February 2021, we experienced an increase in inpatient admissions due to COVID-related hospitalizations. The ultimate impact of COVID-19 to us and our financial condition is presently unknown and we continue to monitor the impact of COVID-19 on our claims reserve estimate.
76
Selling, General and Administrative Expenses. Selling, general and administrative expenses were $291.0 million and $156.4 million for the years ended December 31, 2021 and 2020, respectively, an increase of $134.6 million, or 86.1%. The increase was primarily due to equity-based compensation of $106.6 million. Excluding equity-based compensation for 2021, our, selling, general and administrative expenses increased 19.5% from 2020. The remaining increase was driven by ongoing investments and expenditures in network development and sales and marketing to drive the growth of Alignment’s Health Plan membership, continued hiring of employees to support that growth, and investments related to the IPO.
Depreciation and Amortization. Depreciation and amortization expense was $15.8 million and $15.1 million for the years ended December 31, 2021 and 2020, respectively, an increase of $0.7 million, or 4.8%. The increase was primarily due to the amount and timing of our capital expenditures and the associated depreciation relative to 2020.
Other Expenses
Interest expense. Interest expense was $17.4 million and $16.9 million for the years ended December 31, 2021 and 2020, respectively, an increase of $0.5 million or 2.9%. The increase in interest expense was primarily due to an increase in payment-in-kind interest of $4.0 million or 50%.
Other (income) expenses. Other (income) expenses were $(0.2) million and $0.7 million for the years ended December 31, 2021 and 2020, respectively, a decrease of $0.9 million. The decrease in expenses was primarily due to losses on the disposal of assets in 2020 that did not recur in 2021.
Liquidity and Capital Resources
General
To date, we have financed our operations principally through our IPO, private placements of our equity securities, revenues, and a loan agreement with CR Group (“CRG”). As of December 31, 2021, we had $466.6 million in cash.
In addition, we operate as a holding company in a highly regulated industry. Alignment Healthcare, Inc., our parent company, is dependent upon dividends and administrative expense reimbursements from our subsidiaries, most of which are subject to regulatory restrictions. We continue to maintain significant levels of aggregate excess statutory capital and surplus in our state-regulated operating subsidiaries. Cash at the parent company was $371.8 million at December 31, 2021.
On November 18, 2021, certain selling stockholders, including the Lead Sponsors, sold 9,200,000 shares of our common stock. The Company did not sell any shares, nor did the Company share count increase or decrease as a result of the transaction. The Company did not receive any proceeds from the sale of shares by the selling stockholders.
We may incur operating losses in the future due to the investments we intend to continue to make in expanding our operations and sales and marketing and due to the general and administrative costs we expect to incur in connection with continuing to operate as a public company. As a result, we may require additional capital resources to execute strategic initiatives to grow our business.
We believe that our liquid assets, together with anticipated revenues from our operations, will be sufficient to fund our operating and organic capital needs for at least the next 12 months. Our assessment of the period of time through which our financial resources will be adequate to support our operations is a forward-looking statement and involves risks and uncertainties. Our actual results could vary because of, and our future capital requirements will depend on, many factors, including our growth rate, the timing and extent of spending to expand our presence in existing markets, expand into new markets and increase our sales and marketing activities. We may in the future enter into arrangements to acquire or invest in complementary businesses, services and technologies, including intellectual property rights. We have based this estimate on assumptions that may prove to be wrong, and we could use our available capital resources sooner than we currently expect. We may be required to seek additional equity or debt financing. In the event that additional financing is required from outside sources, we may not be able to raise it on terms acceptable to us or at all. If we are unable to raise additional capital when desired, or if we cannot expand our operations or otherwise capitalize on our business opportunities because we lack sufficient capital, our business, results of operations, and financial condition would be adversely affected
Certain states in which we operate as a CMS-licensed Medicare Advantage company may require us to meet certain capital adequacy performance standards and tests. The National Association of Insurance Commissioners has adopted rules which, if implemented by the states, set minimum capitalization requirements for insurance companies, HMOs, and other entities bearing risk for healthcare coverage. The requirements take the form of risk-based capital (“RBC”) rules, which may vary from state to state. Certain states in which our health plans or risk bearing entities operate have adopted the RBC rules. Other states in which our health plans or risk bearing entities operate have chosen not to adopt the RBC rules, but instead have designed and implemented their own rules regarding capital adequacy. Our health plans or risk-bearing entities were in compliance with the
77
minimum capital requirements for all periods presented. See “Risk Factors—Risks Related to Regulation—State Regulation of Insurance-Related Products.”
Term Loan
On August 21, 2018, we entered into a term loan agreement (the "Term Loan") with CRG for $80.0 million, with an option to borrow up to an additional $20.0 million. In April 2019, we amended the Term Loan to increase its borrowing capacity by $75.0 million and drew down $35.0 million in May 2019. The Term Loan was subject to a commitment fee of $6.8 million and we incurred debt issuance costs of $3.6 million. The Term Loan matures in June 2023, at which time the full balance of the Term Loan, including the commitment fee and the payment-in-kind balance, will be due.
The commitment fees are deferred as part of debt issuance costs and are amortized to interest expense over the term using the effective interest method. The debt issuance costs are being amortized to interest expense over the term using the effective interest method.
The Term Loan bears interest at a rate of 10.25% payable on a quarterly basis. We have the option to pay a portion of the interest in cash with the remaining portion of the interest added to the principal balance as a payment-in-kind. The payment-in-kind is also subject to a commitment fee of 5%. The cash and payment-in-kind interest rates were 7.75% and 2.50%, respectively, through April 2019, and then converted to 7.50% and 2.75%, respectively. In 2021 and 2020, we utilized our option to pay the quarterly interest payments in both cash and payment-in-kind. Our total long-term debt balance of $154.1 million as of December 31, 2021 included the principal balance of $135.0 million, the initial commitment fee of $6.8 million, and the payment-in-kind interest on the principal balance of $12.0 million. The payment-in-kind interest on the principal balance is also subject to the commitment fee of $0.3 million for the year ended December 31, 2021. The amount was included in the long-term debt balance.
In addition, the Term Loan includes financial covenants regarding the maintenance of minimum liquidity of $6.0 million of operating cash, as defined, on a consolidated basis, at least $10.0 million in its cash accounts on a daily basis and minimum consolidated revenue amounts in the calendar years through 2022. As of December 31, 2021, we were in compliance with the financial covenants. The Term Loan is guaranteed by certain of our wholly owned subsidiaries and collateralized by all unrestricted assets.
Cash Flows
The following table presents a summary of our consolidated cash flows from operating, investing and financing activities for the periods indicated.
|
|
Year Ended December 31, |
|
|||||
(dollars in thousands) |
|
2021 |
|
|
2020 |
|
||
Net cash provided by (used in) operating activities |
|
$ |
(78,776 |
) |
|
$ |
7,561 |
|
Net cash used in investing activities |
|
|
(20,815 |
) |
|
|
(16,358 |
) |
Net cash provided by financing activities |
|
|
360,130 |
|
|
|
130,124 |
|
Net change in cash |
|
|
260,539 |
|
|
|
121,327 |
|
Cash and restricted cash at beginning of period |
|
|
207,811 |
|
|
|
86,484 |
|
Cash and restricted cash at end of period |
|
$ |
468,350 |
|
|
$ |
207,811 |
|
Operating Activities
For the year ended December 31, 2021, net cash used in operating activities was $78.8 million, a decrease of $86.4 million compared to net cash provided by operating activities of $7.6 million for the year ended December 31, 2020. Significant changes impacting net cash provided by operating activities for the year ended December 31, 2021 as compared to the year ended December 31, 2020 resulted from an increase in net loss offset by adjustments for non-cash items such as equity-based compensation and common stock payments. For the year ended December 31, 2021, net cash used in working capital, which is comprised of net cash provided by (used in) operating activities and cash used in the acquisition of property and equipment, was $97.1 million, a decrease of $89.0 million compared to $8.1 million for the year ended December 31, 2020. Significant changes include cash settlement of the SARs and reorganization and transaction-related expenses that occurred as part of the IPO, acquisition expenses, and an increase in accounts receivable due to growth.
Investing Activities
For the year ended December 31, 2021, net cash used in investing activities was $20.8 million, an increase of $4.4 million compared to net cash used in investing activities of $16.4 million for the year ended December 31, 2020. The increase primarily relates to incremental capital expenditures related to information technology and infrastructure projects.
78
Financing Activities
For the year ended December 31, 2021, net cash provided by financing activities was $360.1 million, an increase of $230.0 million compared to net cash provided by financing activities of $130.1 million for the year ended December 31, 2020. The increase primarily relates to proceeds from the IPO in the first quarter of 2021, which was higher than the funding received in 2020.
Material cash requirements from known contractual and other obligations
Our principal commitments consist of repayments of long-term debt, operating leases and certain purchase obligations. The following table summarizes our contractual and other obligations as of December 31, 2021:
|
|
Payments due by Period |
|
|||||||||||||||||
|
|
Total |
|
|
Less than |
|
|
1-3 years |
|
|
3-5 |
|
|
More than |
|
|||||
Long-term debt obligations(1) |
|
$ |
160,990 |
|
|
$ |
— |
|
|
$ |
160,990 |
|
|
$ |
— |
|
|
$ |
— |
|
Operating lease obligations |
|
|
11,213 |
|
|
|
4,126 |
|
|
|
7,087 |
|
|
|
— |
|
|
|
— |
|
Purchase obligations(2) |
|
|
16,410 |
|
|
|
9,536 |
|
|
|
6,874 |
|
|
|
— |
|
|
|
— |
|
Other obligations |
|
|
474 |
|
|
|
173 |
|
|
|
301 |
|
|
|
— |
|
|
|
— |
|
Total |
|
$ |
189,087 |
|
|
$ |
13,835 |
|
|
$ |
175,252 |
|
|
$ |
— |
|
|
$ |
— |
|
(1) Represents the estimated full cash repayment to our lender upon maturity of the Term Loan in June 2023, including the anticipated commitment fees and payments-in-kind balance.
(2) Includes fixed, minimum and estimated payments under our existing contractual obligations that are legally enforceable and binding for goods and services. These obligations include agreements that are cancelable with the payment of an early termination penalty and other funding commitments that require fixed or minimum levels of service to be purchased with a specific timing established. Purchase obligations exclude agreements that are cancelable without penalty.
Not included in the table above are our medical expenses payable which are included within current liabilities in our financial statements included in this Annual Report on Form 10-K.
Critical Accounting Policies and Estimates
The discussion and analysis of our financial condition and results of operations are based upon our consolidated financial statements, which have been prepared in accordance with U.S. generally accepted accounting principles and include the accounts of our wholly-owned subsidiaries and three variable interest entities (“VIEs”) in California and North Carolina that meet the consolidation requirements for accounting purposes. All intercompany transactions have been eliminated in consolidation. Noncontrolling interest is presented within the equity section of our consolidated balance sheets.
Certain accounting policies involve significant judgments and assumptions by management, which have a material impact on the carrying value of assets and liabilities and the recognition of income and expenses. Management considers these accounting policies to be critical accounting policies. The estimates and assumptions used by management are based on historical experience and other factors, which are believed to be reasonable under the circumstances. The significant accounting policies which we believe are the most critical to aid in fully understanding and evaluating our reported financial results are described below. Refer to Note 2 “Summary of Significant Accounting Policies” to our audited consolidated financial statements for more detailed information regarding our critical accounting policies.
Revenue
Payments by CMS to health plans are determined through a competitive bidding process with CMS and are based on the cost of care in a local market and the average utilization of services by the member enrolled. These payments are subject to periodic adjustments under CMS’s “risk adjustment model,” which compensates health plans based on the health severity and certain demographic factors of each individual member. Members diagnosed with certain conditions are paid at a higher monthly payment than members who are healthier. Under this risk adjustment model, CMS calculates the risk adjustment payment using diagnosis data from hospital inpatient, hospital outpatient and physician treatment settings. We and healthcare providers collect, capture, and submit the necessary and available diagnosis data to CMS within prescribed deadlines. Both premium and capitation revenue (including Medicare Part D) are subject to adjustments under the risk adjustment model.
Throughout the year, we estimate risk adjustment payments based upon the diagnosis data submitted and expected to be submitted to CMS. The risk adjustment payments are recorded as an adjustment to premium and capitation revenue. Our risk adjustment data is also subject to review by the government, including audit by regulators.
Receivables, including risk adjusted premium due from the government or through third-party payors, pharmacy rebates, and other receivables, are shown net of allowances for estimated uncollectible accounts and retroactive membership adjustments.
79
Medical Expenses Payable
Medical expenses payable includes estimates of our obligations for medical care services that have been rendered on behalf of our members and the members of third-party payors, but for which claims have either not yet been received or processed, loss adjustment expense reserve for the expected costs of settling these claims, and for liabilities related to physician, hospital and other medical cost disputes.
We develop estimates for medical expenses incurred but not yet paid (“IBNP”) which includes an estimate for claims incurred but not reported (“IBNR”) and a payable for adjudicated claims. IBNR is estimated using an actuarial process that is consistently applied and centrally controlled. Medical expenses payable also includes an estimate for the costs necessary to process unpaid claims at the end of each period. We estimate IBNR liability using actuarial methods that are commonly used by health insurance actuaries and meet Actuarial Standards of Practice. These actuarial methods consider factors, such as cost trends and completion factors that are assessed based on historical data for payment patterns, product mix, seasonality, utilization of health care services, and other relevant factors.
Completion Factors. A completion factor is an actuarial estimate, based upon historical experience and analysis of current trends, of the percentage of incurred claims during a given period adjudicated by us at the date of estimation. Completion factors are the most significant factors we use in developing our medical expenses payable estimates for periods prior to the most recent three months. Completion factors include judgments in relation to claim submissions such as the time from date of service to claim receipt, claim levels and processing cycles, as well as other factors. If actual claims submission rates from providers (which can be influenced by a number of factors, including provider mix and electronic versus manual submissions) or our claim processing patterns are different than estimated, our reserve estimates may be significantly impacted.
The following table illustrates the sensitivity of these factors and the estimated potential impact on our medical expenses payable estimates for those periods as of December 31, 2021:
Completion Factors |
|
Increase (Decrease) In Medical Expenses Payable |
|
|
(Decrease) Increase in Factors |
|
|
|
|
|
|
(in thousands) |
|
|
(3)% |
|
$ |
11,149 |
|
(2) |
|
|
7,432 |
|
(1) |
|
|
3,716 |
|
1 |
|
|
(3,716 |
) |
2 |
|
|
(7,432 |
) |
3 |
|
|
(11,149 |
) |
Medical Cost Per Member Per Month Trend Factors. Medical cost PMPM trend factors are significant factors we use in developing our medical expenses payable estimates for the most recent three months. Medical cost trend factors are developed through a comprehensive analysis of claims incurred in prior months, provider contracting and expected unit costs, benefit design and a review of a broad set of health care utilization indicators. These factors include but are not limited to pharmacy utilization trends, inpatient hospital authorization data and influenza incidence data from the National Centers for Disease Control. We also consider macroeconomic variables such as GDP growth, employment and disposable income. A large number of factors can cause the medical cost trend to vary from our estimates, including: our ability and practices to manage medical and pharmaceutical costs, changes in level and mix of services utilized; mix of benefits offered, including the impact of co-pays and deductibles; changes in medical practices; and catastrophes, epidemics and pandemics, such as COVID-19.
The following table illustrates the sensitivity of these factors and the estimated potential impact on our medical expenses payable estimates for the most recent two months as of December 31, 2021:
Medical Cost PMPM Quarterly Trend |
|
Increase (Decrease) In Medical Expenses Payable |
|
|
Increase (Decrease) in Factors |
|
|
|
|
|
|
(in thousands) |
|
|
3% |
|
$ |
2,472 |
|
2 |
|
|
1,648 |
|
1 |
|
|
824 |
|
(1) |
|
|
(824 |
) |
(2) |
|
|
(1,648 |
) |
(3) |
|
|
(2,472 |
) |
80
Each period, we re-examine previously established IBNR estimates based on actual claim submissions and other changes in facts and circumstances. As the IBNR estimates recorded in prior periods develop, we adjust the amount of the estimates and include the changes in estimates in medical expenses in the period in which the change is identified.
Actuarial Standards of Practice generally require that the IBNP estimates be adequate to cover obligations under moderately adverse conditions. Moderately adverse conditions are situations in which the actual claims are expected to be higher than the otherwise estimated value of such claims at the time of estimate.
In many situations, the claims amount ultimately settled will be different than the estimate that satisfies the Actuarial Standards of Practice. We include in our IBNP an estimate for medical claims liability under moderately adverse conditions, which represents the risk of adverse deviation of the estimates in its actuarial method of reserving.
We believe that medical expenses payable is adequate to cover future claims payments required. However, such estimates are based on knowledge of current events and anticipated future events. Therefore, the actual liability could differ materially from the amounts provided. The following tables provide information about incurred and paid claims development as of December 31, 2021:
|
|
Cumulative Incurred Claims, net of reinsurance for the |
|
|||||||||
Claims Incurred Year |
|
2019 |
|
|
2020 |
|
|
2021 |
|
|||
2019 |
|
$ |
274,871 |
|
|
$ |
256,810 |
|
|
$ |
253,759 |
|
2020 |
|
|
|
|
|
281,124 |
|
|
|
276,111 |
|
|
2021 |
|
|
|
|
|
|
|
|
327,224 |
|
||
Total |
|
|
|
|
|
|
|
$ |
857,094 |
|
||
|
|
Cumulative Claims paid, net of reinsurance for the |
|
|
Cumulative Number |
|
||||||||||
Claims Incurred Year |
|
2019 |
|
|
2020 |
|
|
2021 |
|
|
|
|
||||
2019 |
|
$ |
196,086 |
|
|
$ |
251,507 |
|
|
$ |
255,628 |
|
|
|
410,500 |
|
2020 |
|
|
|
|
|
206,288 |
|
|
|
275,016 |
|
|
|
336,212 |
|
|
2021 |
|
|
|
|
|
|
|
|
251,629 |
|
|
|
234,191 |
|
||
Total |
|
|
|
|
|
|
|
$ |
782,273 |
|
|
|
|
|||
Substantially all of the claims incurred but not paid balance as of December 31, 2021 relates to the current year.
There is no single or common claim frequency metric used in the health care industry. We believe a relevant metric for our health insurance business is the cumulative number of claims paid for each incurred year. Claims that did not result in a liability are not included in the frequency metric.
Recent Accounting Pronouncements
See Note 2 to our audited consolidated financial statements “Summary of Significant Accounting Policies—Recent Accounting Pronouncements Adopted” for more information.
Item 7A. Quantitative and Qualitative Disclosures About Market Risk.
Market risk represents the risk of loss that may impact our financial position due to adverse changes in financial market prices and rates. Our market risk exposure is primarily a result of exposure due to potential changes in inflation. We do not hold financial instruments for trading purposes.
Inflation Risk
Based on our analysis of the periods presented, we believe that inflation has not had a material effect on our operating results. Nonetheless, if our costs were to become subject to significant inflationary pressures, we may not be able to fully offset such higher costs through price increases. There can be no assurance that future inflation will not have an adverse impact on our operating results and financial condition.
81
Item 8. Financial Statements and Supplementary Data.
INDEX TO CONSOLIDATED FINANCIAL STATEMENTS
82
Report of Independent Registered Public Accounting Firm
To the stockholders and the Board of Directors of
Alignment Healthcare, Inc.:
Opinion on the Consolidated Financial Statements
We have audited the accompanying consolidated balance sheets of Alignment Healthcare, Inc. (the “Company”) as of December 31, 2021 and 2020, and the related consolidated statements of operations, changes in stockholders’ equity (deficit), and cash flows for each of the three years in the period ended December 31, 2021, and the related notes listed in the accompanying Index (collectively, the “financial statements”). In our opinion, the financial statements present fairly, in all material respects, the financial position of the Company as of December 31, 2021 and 2020, and the results of its operations and its cash flows for each of the three years in the period ended December 31, 2021, in conformity with accounting principles generally accepted in the United States of America.
Change in Accounting Principle
As discussed in Note 12 to the financial statements, the Company changed its method of accounting for leases effective January 1, 2020, due to the adoption of FASB Accounting Standards Update 2016-02, Leases (Topic ASC 842), using the modified retrospective transition approach.
Basis for Opinion
These financial statements are the responsibility of the Company’s management. Our responsibility is to express an opinion on the Company’s financial statements based on our audits. We are a public accounting firm registered with the Public Company Accounting Oversight Board (United States) (PCAOB) and are required to be independent with respect to the Company in accordance with the U.S. federal securities laws and the applicable rules and regulations of the Securities and Exchange Commission and the PCAOB.
We conducted our audits in accordance with the standards of the PCAOB. Those standards require that we plan and perform the audit to obtain reasonable assurance about whether the financial statements are free of material misstatement, whether due to error or fraud. The Company is not required to have, nor were we engaged to perform, an audit of its internal control over financial reporting. As part of our audits, we are required to obtain an understanding of internal control over financial reporting, but not for the purpose of expressing an opinion on the effectiveness of the Company’s internal control over financial reporting. Accordingly, we express no such opinion.
Our audits included performing procedures to assess the risks of material misstatement of the financial statements, whether due to error or fraud, and performing procedures that respond to those risks. Such procedures included examining, on a test basis, evidence regarding the amounts and disclosures in the financial statements. Our audits also included evaluating the accounting principles used and significant estimates made by management, as well as evaluating the overall presentation of the financial statements. We believe that our audits provide a reasonable basis for our opinion.
Critical Audit Matters
The critical audit matters communicated below are matters arising from the current-period audit of the financial statements that were communicated or required to be communicated to the audit committee and that (1) relate to accounts or disclosures that are material to the financial statements and (2) involved our especially challenging, subjective, or complex judgments. The communication of critical audit matters does not alter in any way our opinion on the financial statements, taken as a whole, and we are not, by communicating the critical audit matters below, providing separate opinions on the critical audit matters or on the accounts or disclosures to which they relate.
Medical expenses payable – Incurred but not paid claims - Refer to Notes 2 and 7 to the financial statements
Critical Audit Matter Description
Medical expenses payable includes estimates of obligations for medical care services that have been rendered on behalf of members and the members of the contracted third-party payors, but for which claims have either not yet been received or processed. These estimates are referred to as incurred but not yet paid (IBNP) claim liabilities of 77.1 million as of December 31, 2021, and includes an estimate for claims incurred but not reported (IBNR). The Company develops estimates for IBNR claim liability by using actuarial methods that requires management judgment in developing its estimates. These actuarial methods consider factors such as historical data for payment patterns, and assumptions of cost trends related to the medical cost per
83
member per month which may be impacted by seasonality and utilization of health care services and completion factors that assume time from date of service to claim receipt.
We identified the IBNR claim liability as a critical audit matter because of the significant assumptions made by management in estimating the liability. This required complex auditor judgment, and an increased extent of effort, including the involvement of actuarial specialists in performing procedures to evaluate the reasonableness of management’s methods, assumptions and judgments in developing the IBNR claim liability.
How the Critical Audit Matter Was Addressed in the Audit
Our audit procedures related to IBNR claim liability included the following, among others:
Revenue – Classification of revenue recognized related to Direct Contracting Entities (“DCE”) Refer to Note 2 to the financial statements
Critical Audit Matter Description
The Company launched two DCEs that participate in the Centers for Medicare & Medicaid Services (“CMS”) Innovation’s Direct Contracting Model. CMS serves as the claim adjudicator for institutional and specialists care, and directly pays for such fee for service claims. The DCEs are responsible for the cost of health care services related to the patient population attributed to the DCE by participating in 100% savings/losses via the risk share model and in some cases, are financially responsible for the supplemental benefits provided to the patients. The DCEs act as a principal in arranging for and controlling services provided directly by its contracts with primary care physicians, as well as services provided by preferred institutional care providers and specialists. Capitation payments for the DCE program are determined from an annual benchmark established by CMS. These payments, that are adjusted for variable considerations, represent revenue for providing health care service, including primary care as well as institutional and specialist care. Revenue recognized by the DCEs for the year ended December 31, 2021 was $37.7 million.
We identified classification of revenue recognized by the DCEs based on the Company’s principal versus agent conclusion, as a critical audit matter because of the significant assessment made by management in reaching the conclusion that the Company has control over services provided to customers. This required complex auditor judgment, and an increased extent of effort in performing procedures to evaluate the reasonableness of management’s judgments in reaching this conclusion.
How the Critical Audit Matter Was Addressed in the Audit
Our audit procedures related to classification of revenue from DCEs included the following, among others:
84
/s/ Deloitte & Touche LLP
Los Angeles, California
March 3, 2022
We have served as the Company’s auditor since 2019.
85
Alignment Healthcare, Inc.
Consolidated Balance Sheets
(amounts in thousands, except par value and share amounts)
|
|
December 31, |
|
|
December 31, |
|
||
Assets |
|
|
|
|
|
|
||
Current Assets: |
|
|
|
|
|
|
||
Cash |
|
$ |
466,600 |
|
|
$ |
207,311 |
|
Accounts receivable (less allowance for credit losses of $111 at December 31, 2021 and $0 at December 31, 2020, respectively) |
|
|
58,512 |
|
|
|
40,140 |
|
Prepaid expenses and other current assets |
|
|
27,747 |
|
|
|
17,225 |
|
Total current assets |
|
|
552,859 |
|
|
|
264,676 |
|
Property and equipment, net |
|
|
30,358 |
|
|
|
27,145 |
|
Right of use assets, net |
|
|
7,853 |
|
|
|
9,888 |
|
Goodwill and intangible assets, net |
|
|
35,116 |
|
|
|
34,645 |
|
Other assets |
|
|
4,709 |
|
|
|
2,148 |
|
Total assets |
|
$ |
630,895 |
|
|
$ |
338,502 |
|
Liabilities and Stockholders' Equity |
|
|
|
|
|
|
||
Current Liabilities: |
|
|
|
|
|
|
||
Medical expenses payable |
|
$ |
125,886 |
|
|
$ |
112,605 |
|
Accounts payable and accrued expenses |
|
|
17,431 |
|
|
|
15,675 |
|
Accrued compensation |
|
|
23,928 |
|
|
|
25,172 |
|
Total current liabilities |
|
|
167,245 |
|
|
|
153,452 |
|
Long-term debt, net of debt issuance costs |
|
|
150,620 |
|
|
|
144,168 |
|
Long-term portion of lease liabilities |
|
|
6,975 |
|
|
|
10,271 |
|
Total liabilities |
|
|
324,840 |
|
|
|
307,891 |
|
|
|
|
|
|
|
|||
Stockholders' Equity: |
|
|
|
|
|
|
||
Preferred stock, $.001 par value; 100,000,000 and 0 shares authorized as of |
|
|
— |
|
|
|
— |
|
Common stock, $.001 par value; 1,000,000,000 and 164,063,787 shares authorized |
|
|
188 |
|
|
|
164 |
|
Additional paid-in capital |
|
|
880,708 |
|
|
|
410,018 |
|
Accumulated deficit |
|
|
(574,856 |
) |
|
|
(379,571 |
) |
Total Alignment Healthcare, Inc. stockholders' equity |
|
|
306,040 |
|
|
|
30,611 |
|
Noncontrolling interest |
|
|
15 |
|
|
|
— |
|
Total stockholders' equity |
|
|
306,055 |
|
|
|
30,611 |
|
Total liabilities and stockholders' equity |
|
$ |
630,895 |
|
|
$ |
338,502 |
|
(1)
See accompanying notes to consolidated financial statements.
86
Alignment Healthcare, Inc.
Consolidated Statements of Operations
(amounts in thousands, except share and per share amounts)
|
|
Year Ended December 31, |
|
|||||||||
|
|
2021 |
|
|
2020 |
|
|
2019 |
|
|||
Revenues: |
|
|
|
|
|
|
|
|
|
|||
Earned premiums |
|
$ |
1,167,085 |
|
|
$ |
955,393 |
|
|
$ |
753,973 |
|
Other |
|
|
688 |
|
|
|
3,829 |
|
|
|
2,988 |
|
|
|
1,167,773 |
|
|
|
959,222 |
|
|
|
756,961 |
|
|
Expenses: |
|
|
|
|
|
|
|
|
|
|||
Medical expenses |
|
|
1,039,041 |
|
|
|
792,992 |
|
|
|
661,389 |
|
Selling, general, and administrative expenses |
|
|
290,991 |
|
|
|
156,398 |
|
|
|
110,134 |
|
Depreciation and amortization |
|
|
15,813 |
|
|
|
15,095 |
|
|
|
14,922 |
|
Total expenses |
|
|
1,345,845 |
|
|
|
964,485 |
|
|
|
786,445 |
|
Loss from operations |
|
|
(178,072 |
) |
|
|
(5,263 |
) |
|
|
(29,484 |
) |
Other expenses: |
|
|
|
|
|
|
|
|
|
|||
Interest expense |
|
|
17,443 |
|
|
|
16,931 |
|
|
|
14,897 |
|
Other (income) expenses |
|
|
(229 |
) |
|
|
732 |
|
|
|
351 |
|
Total other expenses |
|
|
17,214 |
|
|
|
17,663 |
|
|
|
15,248 |
|
Loss before income taxes |
|
|
(195,286 |
) |
|
|
(22,926 |
) |
|
|
(44,732 |
) |
Provision for income taxes |
|
|
— |
|
|
|
— |
|
|
|
— |
|
Net loss attributable to Alignment Healthcare, Inc. |
|
$ |
(195,286 |
) |
|
$ |
(22,926 |
) |
|
$ |
(44,732 |
) |
|
|
|
|
|
|
|
|
|
|
|||
Total weighted-average common shares outstanding - |
|
|
171,956,849 |
|
|
|
152,132,299 |
|
|
|
135,862,864 |
|
Net loss per share - basic and diluted |
|
$ |
(1.14 |
) |
|
$ |
(0.15 |
) |
|
$ |
(0.33 |
) |
(1)
See accompanying notes to consolidated financial statements.
87
Alignment Healthcare, Inc.
Consolidated Statements of Stockholders' Equity (Deficit)
(amounts in thousands, except par value and share amounts)
|
|
Common Stock |
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||
|
|
Shares |
|
|
Amount |
|
|
Additional |
|
|
Accumulated Deficit |
|
|
Noncontrolling interest |
|
|
Total |
|
||||||
Balance at January 1, 2019(1) |
|
|
147,157,801 |
|
|
$ |
147 |
|
|
$ |
278,111 |
|
|
$ |
(311,913 |
) |
|
$ |
— |
|
|
$ |
(33,655 |
) |
Net loss attributable to |
|
|
— |
|
|
|
— |
|
|
|
— |
|
|
|
(44,732 |
) |
|
|
— |
|
|
|
(44,732 |
) |
Equity-based compensation |
|
|
— |
|
|
|
— |
|
|
|
1,157 |
|
|
|
— |
|
|
|
— |
|
|
|
1,157 |
|
Equity repurchase |
|
|
— |
|
|
|
— |
|
|
|
(1,481 |
) |
|
|
— |
|
|
|
— |
|
|
|
(1,481 |
) |
Balance at December 31, 2019(1) |
|
|
147,157,801 |
|
|
$ |
147 |
|
|
$ |
277,787 |
|
|
$ |
(356,645 |
) |
|
$ |
— |
|
|
$ |
(78,711 |
) |
Net loss attributable to |
|
|
— |
|
|
|
— |
|
|
|
— |
|
|
|
(22,926 |
) |
|
|
— |
|
|
|
(22,926 |
) |
Issuance of common stock at |
|
|
16,905,986 |
|
|
|
17 |
|
|
|
131,612 |
|
|
|
— |
|
|
|
— |
|
|
|
131,629 |
|
Equity-based compensation |
|
|
— |
|
|
|
— |
|
|
|
2,124 |
|
|
|
— |
|
|
|
— |
|
|
|
2,124 |
|
Equity repurchase |
|
|
— |
|
|
|
— |
|
|
|
(1,505 |
) |
|
|
— |
|
|
|
— |
|
|
|
(1,505 |
) |
Balance at December 31, 2020(1) |
|
|
164,063,787 |
|
|
$ |
164 |
|
|
$ |
410,018 |
|
|
$ |
(379,571 |
) |
|
$ |
— |
|
|
$ |
30,611 |
|
Net loss attributable to Alignment |
|
|
— |
|
|
|
— |
|
|
|
— |
|
|
|
(195,286 |
) |
|
|
— |
|
|
|
(195,286 |
) |
Noncontrolling interest |
|
|
— |
|
|
|
— |
|
|
|
— |
|
|
|
— |
|
|
|
15 |
|
|
|
15 |
|
Issuance of common stock upon |
|
|
21,700,000 |
|
|
|
22 |
|
|
|
361,567 |
|
|
|
— |
|
|
|
— |
|
|
|
361,589 |
|
Issuance of common stock to |
|
|
573,782 |
|
|
|
1 |
|
|
|
6,479 |
|
|
|
— |
|
|
|
— |
|
|
|
6,480 |
|
Issuance of common stock to |
|
|
936,213 |
|
|
|
1 |
|
|
|
11,509 |
|
|
|
— |
|
|
|
— |
|
|
|
11,510 |
|
Forfeitures |
|
|
(80,169 |
) |
|
|
(1 |
) |
|
|
— |
|
|
|
— |
|
|
|
— |
|
|
|
(1 |
) |
Equity-based compensation |
|
|
— |
|
|
|
— |
|
|
|
92,611 |
|
|
|
— |
|
|
|
— |
|
|
|
92,611 |
|
Equity repurchase |
|
|
— |
|
|
|
— |
|
|
|
(1,474 |
) |
|
|
— |
|
|
|
— |
|
|
|
(1,474 |
) |
Balance at December 31, 2021 |
|
|
187,193,613 |
|
|
$ |
187 |
|
|
$ |
880,710 |
|
|
$ |
(574,857 |
) |
|
$ |
15 |
|
|
$ |
306,055 |
|
(1) The consolidated balances were derived from the audited consolidated financial statements as of December 31, 2020 and December 31, 2019, and were retroactively adjusted, including shares and per share amounts, as a result of the Reorganization. See Note 1 to the consolidated financial statements for additional details.
See accompanying notes to consolidated financial statements.
88
Alignment Healthcare, Inc.
Consolidated Statements of Cash Flows
(amounts in thousands)
|
|
Year Ended December 31, |
|
|||||||||
|
|
2021 |
|
|
2020 |
|
|
2019 |
|
|||
Operating Activities: |
|
|
|
|
|
|
|
|
|
|||
Net loss |
|
$ |
(195,286 |
) |
|
$ |
(22,926 |
) |
|
$ |
(44,732 |
) |
Adjustments to reconcile net loss to net cash provided by (used in) |
|
|
|
|
|
|
|
|
|
|||
Provision for credit loss |
|
|
111 |
|
|
|
118 |
|
|
|
1,424 |
|
Depreciation and amortization |
|
|
16,033 |
|
|
|
15,461 |
|
|
|
16,583 |
|
Amortization-debt issuance costs and investment discount |
|
|
2,254 |
|
|
|
2,192 |
|
|
|
1,949 |
|
Payment-in-kind interest |
|
|
4,197 |
|
|
|
4,015 |
|
|
|
3,414 |
|
Loss on disposal of property and equipment |
|
|
— |
|
|
|
1,006 |
|
|
|
418 |
|
Equity-based compensation and common stock payments |
|
|
110,600 |
|
|
|
2,124 |
|
|
|
1,157 |
|
Non-cash lease expense |
|
|
2,731 |
|
|
|
2,317 |
|
|
|
— |
|
Changes in operating assets and liabilities: |
|
|
|
|
|
|
|
|
|
|||
Accounts receivable |
|
|
(17,608 |
) |
|
|
(4,627 |
) |
|
|
(5,784 |
) |
Prepaid expenses and other current assets |
|
|
(10,340 |
) |
|
|
(11,990 |
) |
|
|
(2,683 |
) |
Other assets |
|
|
644 |
|
|
|
2,779 |
|
|
|
1,154 |
|
Medical expenses payable |
|
|
12,512 |
|
|
|
6,460 |
|
|
|
36,570 |
|
Accounts payable and accrued expenses |
|
|
437 |
|
|
|
645 |
|
|
|
1,294 |
|
Accrued compensation |
|
|
(1,244 |
) |
|
|
12,651 |
|
|
|
(196 |
) |
Lease liabilities |
|
|
(3,817 |
) |
|
|
1,277 |
|
|
|
— |
|
Noncurrent liabilities |
|
|
— |
|
|
|
(3,941 |
) |
|
|
(1,360 |
) |
Net cash provided by (used in) operating activities |
|
|
(78,776 |
) |
|
|
7,561 |
|
|
|
9,208 |
|
Investing Activities: |
|
|
|
|
|
|
|
|
|
|||
Asset acquisition, net of cash received |
|
|
(1,405 |
) |
|
|
— |
|
|
|
— |
|
Purchase of investments |
|
|
(2,475 |
) |
|
|
(1,575 |
) |
|
|
(320 |
) |
Sale of investments |
|
|
1,425 |
|
|
|
825 |
|
|
|
325 |
|
Acquisition of property and equipment |
|
|
(18,360 |
) |
|
|
(15,708 |
) |
|
|
(10,245 |
) |
Proceeds from the sale of property and equipment |
|
|
— |
|
|
|
100 |
|
|
|
— |
|
Net cash used in investing activities |
|
|
(20,815 |
) |
|
|
(16,358 |
) |
|
|
(10,240 |
) |
Financing Activities: |
|
|
|
|
|
|
|
|
|
|||
Issuance of long-term debt |
|
|
— |
|
|
|
— |
|
|
|
55,000 |
|
Debt issuance costs |
|
|
— |
|
|
|
— |
|
|
|
(854 |
) |
Purchase of noncontrolling interest |
|
|
15 |
|
|
|
— |
|
|
|
— |
|
Equity repurchase |
|
|
(1,474 |
) |
|
|
(1,505 |
) |
|
|
(1,981 |
) |
Issuance of common stock |
|
|
390,600 |
|
|
|
135,000 |
|
|
|
500 |
|
Common stock issuance costs |
|
|
(29,011 |
) |
|
|
(3,371 |
) |
|
|
— |
|
Net cash provided by financing activities |
|
|
360,130 |
|
|
|
130,124 |
|
|
|
52,665 |
|
Net increase in cash |
|
|
260,539 |
|
|
|
121,327 |
|
|
|
51,633 |
|
Cash and restricted cash at beginning of period |
|
|
207,811 |
|
|
|
86,484 |
|
|
|
34,851 |
|
Cash and restricted cash at end of period |
|
$ |
468,350 |
|
|
$ |
207,811 |
|
|
$ |
86,484 |
|
Supplemental disclosure of cash flow information: |
|
|
|
|
|
|
|
|
|
|||
Cash paid for interest |
|
$ |
10,992 |
|
|
$ |
10,720 |
|
|
$ |
9,527 |
|
Supplemental non-cash investing and financing activities: |
|
|
|
|
|
|
|
|
|
|||
Acquisition of property in accounts payable |
|
$ |
347 |
|
|
$ |
106 |
|
|
$ |
366 |
|
89
The following table provides a reconciliation of cash and restricted cash reported within the consolidated balance sheets to the total above:
|
|
December 31, 2021 |
|
|
December 31, 2020 |
|
|
December 31, 2019 |
|
|||
Cash |
|
$ |
466,600 |
|
|
$ |
207,311 |
|
|
$ |
86,484 |
|
Restricted cash in other assets |
|
|
1,750 |
|
|
|
500 |
|
|
|
— |
|
Total |
|
$ |
468,350 |
|
|
$ |
207,811 |
|
|
$ |
86,484 |
|
See accompanying notes to consolidated financial statements.
90
Alignment Healthcare, Inc.
Notes to Consolidated Financial Statements
(amounts in thousands, except share amounts)
1. Organization
Alignment Healthcare, Inc. (collectively, “we” or “us” or “our” or the “Company”), formerly, Alignment Healthcare Holdings, LLC, is a next generation, consumer-centric health care platform that is purpose-built to provide seniors with high quality, affordable care with a vastly improved consumer experience. Enabled by our innovative technology and care delivery model, the Company focuses on improving outcomes in the Medicare Advantage sector.
The Company’s operations primarily consist of the following:
Reorganization
We historically operated as a Delaware limited liability company under the name Alignment Healthcare Holdings, LLC. On March 17, 2021, Alignment Healthcare Holdings, LLC converted to a Delaware corporation pursuant to a statutory conversion and we changed our name to Alignment Healthcare, Inc. for purposes of completing an initial public offering ("IPO") (the "Reorganization"). As part of the Reorganization, Alignment Healthcare Partners, LP ("the Parent"), the sole unitholder of Alignment Healthcare Holdings, LLC, exchanged its membership units for our common stock and became the sole holder of our shares of common stock. Prior to the closing of the IPO, the Parent merged with and into the Company with Alignment Healthcare, Inc. surviving the merger.
The membership units that were owned by the Parent prior to the Reorganization were converted to our common stock using an approximately 1 to 260 common stock split. All share and per share amounts in these consolidated financial statements and related notes have been retroactively adjusted, where applicable, for all periods presented to give effect to the common stock split and exchange ratio applied in connection with the Reorganization. As a result, we reclassified the capital contributions associated with the issuance of the membership units to additional paid-in capital and common stock using a par value of $0.001 for all periods presented within the consolidated financial statements.
Initial Public Offering
On March 25, 2021, our Registration Statement on Form S-1 for the initial public offering of 27,200,000 shares of common stock was declared effective by the Securities and Exchange Commission. Our common stock began trading on March 26, 2021 on the Nasdaq Global Select Market under the ticker symbol “ALHC."
We completed an IPO through issuing and selling 21,700,000 shares of common stock and certain stockholders selling 5,500,000 shares of common stock, in each case at a price of $18.00 per share. We received proceeds of $361,589 after deducting underwriting discounts and commissions of $24,389 and deferred offering costs of $4,622. Deferred direct offering costs were capitalized and consisted of fees and expenses incurred in connection with the sale of our common stock in the IPO, including legal, accounting, printing and other offering related costs. Upon completion of the IPO, these deferred offering costs were reclassified from prepaid and other current assets to stockholders' equity and recorded against the net proceeds from the offering.
On April 6, 2021, pursuant to a partial exercise of the underwriters' over-allotment option, certain selling stockholders sold an additional 3,314,216 shares of common stock at the IPO price. The Company did not receive any proceeds from the sale of shares of common stock by the selling stockholders in the IPO. On November 18, 2021, certain selling stockholders, including certain of our principal stockholders, sold an additional 9,200,000 shares of our common stock. The Company did not sell any shares and did not receive any proceeds from the sale of shares by the selling stockholders. We incurred $1,045 in transaction costs in connection with this offering.
2. Summary of Significant Accounting Policies
Basis of Presentation
The accompanying consolidated financial statements and accompanying notes have been prepared in accordance with accounting principles generally accepted in the United States of America (“U.S. GAAP”). The consolidated financial statements include the accounts of the Company, our subsidiaries, and three immaterial variable interest entities in which we are the primary beneficiary. All intercompany transactions have been eliminated in consolidation. Noncontrolling interest is presented within the equity section of the consolidated balance sheets.
We have no components of other comprehensive income (loss), and accordingly, comprehensive income (loss) is the same as the net income (loss) for all periods presented.
91
Use of Estimates
The preparation of the consolidated financial statements requires management to make estimates and judgments that affect the amounts reported in the consolidated financial statements. Our significant estimates include, but are not limited to, the determination of medical expenses payable; the impact of risk adjustment provisions related to our Medicare contracts; collectability of receivables; right of use (“ROU”) assets and lease liabilities valuation; valuation of related impairment recognition of long-lived assets, including goodwill and intangible assets; equity-based compensation expense; and contingent liabilities. Estimates and judgments are based upon historical information and on various other assumptions that are believed to be reasonable under the circumstances. Actual results could differ materially from those estimates and the impact of any change in estimates is included in earnings in the period in which the estimate is adjusted.
Segments
We have determined that our chief executive officer is the chief operating decision maker (“CODM”) who regularly reviews financial operating results on a consolidated basis for purposes of allocating resources and evaluating financial performance. We operate and manage the business as one reporting and one operating segment, which is to provide healthcare services to our seniors. Factors used in determining the reportable segment include the nature of operating activities, our organizational and reporting structure, and the type of information reviewed by the CODM to allocate resources and evaluate financial performance. All of our assets are located in the United States.
Fair Value Measurements
Fair value is the price that would be received to sell an asset or paid to transfer a liability in an orderly transaction between market participants at the measurement date. Our current assets and current liabilities approximate fair value because of the short-term nature of these financial instruments. Financial instruments measured at fair value on a recurring basis were based upon a three-tier hierarchy as follows:
Level 1 - Quoted prices in active markets for identical assets or liabilities
Level 2 - Other inputs that are observable for the asset or liability, either directly or indirectly, for substantially the full term of the asset or liability
Level 3 - Unobservable inputs that reflect management’s best estimate of what market participants would use in pricing the asset or liability at the measurement date
The fair value of cash and restricted cash was determined based on Level 1 inputs. The fair value of US Treasury bills and certificate of deposits, which were included in other assets in the consolidated balance sheets, was determined based on Level 2 inputs. There were no assets or liabilities measured at fair value using Level 3 inputs for the years ended December 31, 2021 and 2020. Our long-term debt was reported at carrying value.
Revenue and Accounts Receivable
Earned premium revenue consisting of premium revenue and capitation revenue for the years ended December 31, 2021, 2020, and 2019 were as follows:
|
|
Year Ended |
|
|||||||||
|
|
2021 |
|
|
2020 |
|
|
2019 |
|
|||
Premium |
|
$ |
1,120,864 |
|
|
$ |
873,058 |
|
|
$ |
629,404 |
|
Capitation |
|
|
46,221 |
|
|
|
82,335 |
|
|
|
124,569 |
|
|
|
$ |
1,167,085 |
|
|
$ |
955,393 |
|
|
$ |
753,973 |
|
Premium revenue is derived monthly from the federal government based on our contract with the Centers for Medicare and Medicaid Services (“CMS”). In accordance with this arrangement, we assume the responsibility for the outcomes and the economic risk of funding our members’ health care, supplemental benefits and related administration costs. We recognize premium revenue in the month that members are entitled to receive health care services, and premiums collected in advance are deferred. The monthly reimbursement includes a fixed payment per member per month (“PMPM”), which is adjusted based on certain risk factors derived from medical diagnoses for our members. The adjustments are estimated by projecting the ultimate annual premium and are recognized ratably during the year, with adjustments each period to reflect changes in the estimated ultimate premium. Premiums are also recorded net of estimated uncollectible amounts and retroactive membership adjustments.
Capitation revenue consists primarily of capitated fees for medical care services provided by us under arrangements with our Third-Party Payors and from CMS related to our Direct Contracting Entities ("DCE").
Under those arrangements with Third-Party Payors, we receive a PMPM payment for a defined member population, and we are responsible for providing health care services to the member population over the contract period. We are solely responsible for the cost of health care services related to the member population and in some cases, we are financially responsible for the supplemental benefits provided by us to the members. We act as a principal in arranging for and controlling the services provided by our provider network and we are at risk for arranging and providing health care services.
The premium and capitation payments we receive monthly from CMS for our members are determined from our annual bid or similarly from Third-Party Payors under our capitation arrangement. These payments represent revenues for providing health care coverage, including Medicare Part D
92
benefits. Under the Medicare Part D program, our members and the members of our Third-Party Payors receive standard drug benefits. We may also provide enhanced benefits at our own expense. We recognize premium or capitation revenue for providing this insurance coverage in the month that members are entitled to receive health care services and any premium or capitation collected in advance is deferred. Our CMS payment related to Medicare Part D is subject to risk sharing through the Medicare Part D risk corridor provisions.
On April 1, 2021, we launched two DCEs that participate in the CMS Innovation’s Direct Contracting Model. CMS serves as the claim adjudicator for institutional and specialists care, and directly pays for such fee for service claims. The DCEs are responsible for the cost of health care services related to the patient population attributed to the DCE by participating in 100% savings/losses via the risk share model and in some cases, are financially responsible for the supplemental benefits provided to the patients. The DCEs act as a principal in arranging for and controlling services provided directly by its contracts with primary care physicians, as well as services provided by preferred institutional care providers and specialists. Capitation payments for the DCE program are determined from an annual benchmark established by CMS. These payments, that are adjusted for variable considerations, represent revenue for providing health care service, including primary care as well as institutional and specialist care. The DCEs recognize capitation revenue for providing these services in the period in which the performance obligations are satisfied by transferring services to the members. Revenue recognized by the DCEs for the year ended December 31, 2021 was $37,737.
Revenue Adjustments
Payments by CMS to health plans are determined via a competitive bidding process with CMS and are based upon the cost of care in a local market and the average utilization of services by the member enrolled. These payments are subject to periodic adjustments under CMS’ “risk adjustment model,” which compensates health plans based on the health severity and certain demographic factors of each individual member. Members diagnosed with certain conditions are paid at a higher monthly payment than members who are healthier. Under this risk adjustment model, CMS calculates the risk adjustment payment using diagnosis data from hospital inpatient, hospital outpatient, and physician treatment settings. The Company and health care providers collect, capture, and submit the necessary and available diagnosis data to CMS within prescribed deadlines. Both premium and capitation revenues (including Medicare Part D) are subject to adjustments under the risk adjustment model.
Throughout the year, we estimate risk adjustment payments based upon the diagnosis data submitted and expected to be submitted to CMS. Those estimated risk adjustment payments are recorded as an adjustment to premium and capitation revenue. Our risk adjustment data is also subject to review by the government, including audit by regulators.
Our recognized premium revenue for our Medicare Advantage Plans in California, North Carolina and Nevada are each subject to a minimum annual medical loss ratio (“MLR”) of 85%. The MLR represents medical costs as a percentage of premium revenue. The Code of Federal Regulations define what constitutes medical costs and premium revenue, including certain additional expenses related to improving the quality of care provided, and to exclude certain taxes and fees, in each case as permitted or required by CMS and applicable regulatory requirements. If the minimum MLR is not met, we are required to remit a portion of the premiums back to the federal government. The amount remitted, if any, is recognized as an adjustment to premium revenues in the consolidated statements of operations. There were no amounts payable for the MLR as of December 31, 2021 and December 31, 2020.
Medicare Part D payments are also subject to a federal risk corridor program, which limits a health plan’s overall losses or profit if actual spending for basic Medicare Part D benefits is much higher or lower than what was anticipated. Risk corridor is recorded within premium revenue. The risk corridor provisions compare costs targeted in our bids or Third-Party Payors’ bids to actual prescription drug costs, limited to actual costs that would have been incurred under the standard coverage as defined by CMS. Variances exceeding certain thresholds may result in CMS or Third-Party Payors making additional payments to us or require us to refund a portion of the premiums we received. We estimate and recognize an adjustment to premiums revenue related to these provisions based upon pharmacy claims experience. We record a receivable or payable at the contract level and classify the amount as current or long-term in our consolidated balance sheet based on the timing of expected settlement.
Variable consideration estimates related to DCE contract revenue are based on the most likely outcome method and that a significant reversal in the amount of cumulative revenue recognized would not occur.
Receivables, including risk adjusted premium due from the government or through Third-Party Payors, pharmacy rebates, and other receivables, are shown net of allowances for credit losses and retroactive membership adjustments.
Cash
Cash includes currency on hand with banks and financial institutions. We consider short-term investments with an original maturity of three months or less at the date of purchase to be cash equivalents. Carrying value approximates fair value due to the short-term maturity of the investments.
As of December 31, 2021 and 2020, cash equivalents were $50 and $0, respectively.
Restricted and Other Long-Term Assets
Restricted assets are composed of restricted cash and investments in US Treasury bills and certificate of deposits. The Company intends to hold its investments until maturity; therefore, these investments are stated at amortized cost. Premiums and discounts, if any, are amortized or accreted as interest expense or income over the life of the related asset using the effective interest method. As of December 31, 2021 and 2020, all investments had maturities with less than 12 months.
Restricted assets are required to be maintained at a financial institution within certain states. Due to the nature of the state’s requirements, these assets are classified as noncurrent assets regardless of the contractual maturity date.
93
Property and Equipment—Net
Property and equipment are carried at cost, net of accumulated depreciation. Expenditures for repairs and maintenance that do not improve or extend the life of the assets are expensed when incurred. Costs and the related accumulated depreciation are removed when property and equipment are sold or otherwise disposed of, and any resulting gains or losses are reflected in the consolidated statement of operations.
Software development activities typically consist of three phases: (1) planning, (2) application and infrastructure development, and (3) postimplementation. Costs incurred in the planning and postimplementation phases, including post-configuration training and repairs and maintenance, are expensed as incurred. Costs incurred in the application and infrastructure development phases, including significant enhancements and upgrades, are capitalized once the planning phase is completed and management authorizes the project to commence. Those costs include, but are not limited to, salaries and benefit expenses for employees who are directly associated with the development projects and outside contractor expenses. Software development costs that do not qualify for capitalization are expensed as incurred.
Depreciation expense is computed using the straight-line method generally based on the following estimated useful lives:
Description |
|
Estimated Service Lives (years) |
Computer and equipment |
|
5 |
Office equipment and furniture |
|
5-7 |
Software |
|
3-5 |
Leasehold improvements |
|
15 (or lease term, if shorter) |
Depreciation expense related to property and equipment used to service our members or at our clinics are included within medical expenses in the consolidated statements of operations.
Leases
We determine if an arrangement is a lease at inception and evaluate each lease arrangement to determine whether the lease is an operating or financing leases. ROU assets and lease liabilities are recognized at commencement date based on the present value of the future minimum lease payments over the lease term. ROU assets include upfront payments, if any, and excludes lease incentives. The lease terms may include options to extend or terminate the lease when it is reasonably certain that we will exercise that option.
We utilize our incremental borrowing rate to determine the present value of the lease payments if an interest rate is not implicit in the lease. Expenses for our operating and finance leases are recognized on a straight-line basis over the lease term and are recorded as selling, general and administrative expenses for operating leases and as depreciation expense and interest expense for finance leases.
We elected practical expedients permitted under the transition guidance, which allowed the carryforward of historical lease classification, assessment on whether a contract was or contains a lease and allowed for a cumulative-effect adjustment as of January 1, 2020 and did not restate previously reported results in the comparative periods. We also elected to account for lease and non-lease components as a single lease component. Leases with an initial term of 12 months are not included within the ROU assets and lease liabilities and the associated lease payments are recognized in the consolidated statements of income on a straight-line basis over the lease term. Operating leases are included in ROU assets and lease liabilities are included in accounts payable and accrued expenses and long-term portion of lease liabilities on the consolidated balance sheets.
Goodwill and Intangible Assets
Intangible assets are classified into three categories: (1) goodwill, (2) indefinite-lived intangible assets, and (3) definite-lived intangible assets.
Goodwill and indefinite-lived intangible assets are not amortized. For definite-lived intangible assets, we determine the useful lives of intangible assets after considering each asset’s specific facts and circumstances. Intangible assets that are determined to have definite lives are amortized on a
94
straight-line basis over their useful lives.
Impairment
Goodwill and indefinite-lived assets are tested for impairment on an annual basis and more frequently if indicators of impairment are present. Impairment tests are performed, at a minimum, in the fourth quarter of each year supported by our long-range business plan and annual planning process.
When testing goodwill for impairment, we first perform a qualitative assessment. If the qualitative assessment indicates that it is more likely than not that the carrying value of a reporting unit exceeds the estimated fair value, then a quantitative assessment is performed. We may elect to bypass the qualitative assessment and proceed directly to the quantitative assessment.
If the quantitative test is needed, we determine an appropriate valuation technique to estimate the fair value of the reporting unit as of the testing date. We utilize the income approach and the market approach to assess the most appropriate fair value for the reporting unit. Changes in economic and operating conditions impacting assumptions used in our analyses could result in goodwill impairment in future periods.
When testing indefinite-lived intangible assets other than goodwill for impairment, we first perform a qualitative analysis to determine whether it is more likely than not that an asset has been impaired. If it is more likely than not that an asset has been impaired, an impairment is evaluated by comparing the estimated fair value of the asset to its carrying value. An impairment charge is recognized if the asset’s estimated fair value is less than its carrying value.
Impairment of Long-Lived Assets
Long-lived assets consist of property and equipment and other finite-lived intangible assets. These assets are depreciated or amortized over their estimated useful life and are subject to impairment reviews. We periodically review long-lived assets whenever adverse events or changes in circumstances indicate the carrying value of the asset may not be recoverable.
We review these assets for impairment by comparing the sum of the expected future cash flows (undiscounted and without interest charges) to the carry value. If the sum of the estimated undiscounted future cash flows is less than the carrying value, an impairment determination is required. The amount of impairment is calculated by subtracting the fair value of the asset from the carrying value. An impairment charge, if any, is recognized within earnings from operations.
Medical Expenses
Medical expenses include claim payments, capitation payments, pharmacy costs net of rebates, allocations of certain centralized expenses, internal care delivery expenses and various other costs incurred to provide health insurance coverage and care to members, as well as estimates of future payments to hospitals and others for medical care and other supplemental benefits provided.
We have contracts with a network of hospitals, physicians, and other providers and compensate those providers and ancillary organizations based on contractual arrangements or CMS Medicare compensation guidelines. We pay these contracting providers either through fee-for-service arrangement in which the provider is paid negotiated rates for specific services provided or a capitation payment, which represent monthly contractual fees disbursed for each member regardless of medical services provided to the member. We are responsible for the entirety of the cost of health care services related to the member population, in addition to supplemental benefits provided by us to our seniors. We also record claims expenses related to our institutional and specialist care related to our DCE program with CMS as we act as the principal in the transaction.
Capitation-related expenses are recorded on an accrual basis during the coverage period. Expenses related to fee-for-service contracts are recorded in the period in which the related services are dispensed.
Pharmacy costs represent payments for members’ prescription drug benefits, net of rebates from drug manufacturers. Receivables for such pharmacy rebates are included in accounts receivable in the consolidated balance sheet.
Medical Expenses Payable
Medical expenses payable includes estimates of our obligations for medical care services that have been rendered on behalf of our members and the members of the Third-Party Payors, but for which claims have either not yet been received or processed, loss adjustment expense reserve for the expected costs of settling these claims, and for liabilities related to physician, hospital, and other medical cost disputes.
We develop estimates for medical expenses incurred but not yet paid (“IBNP”) which includes an estimate for claims incurred but not reported (“IBNR”) and a payable for adjudicated claims. IBNR is estimated using an actuarial process that is consistently applied and centrally controlled. Medical expenses payable also includes an estimate for the costs necessary to process unpaid claims at the end of each period. We estimate IBNR liability using actuarial methods that are commonly used by health insurance actuaries and meet Actuarial Standards of Practice. These actuarial methods consider factors, such as cost trends and completion factors that are assessed based on historical data for payment patterns, product mix, seasonality, utilization of health care services, and other relevant factors. Each period, we re-examine previously established IBNR estimates based on actual claim submissions and other changes in facts and circumstances. As the IBNR estimates recorded in prior periods develop, we adjust the amount of the estimates and include the changes in estimates in medical expenses in the period in which the change is identified.
95
Actuarial Standards of Practice generally require that the IBNP estimates be adequate to cover obligations under moderately adverse conditions. Moderately adverse conditions are situations in which the actual claims are expected to be higher than the otherwise estimated value of such claims at the time of estimate. In many situations, the claims amount ultimately settled will be different than the estimate that satisfies the Actuarial Standards of Practice. We include in our IBNP an estimate for medical claims liability under moderately adverse conditions, which represents the risk of adverse deviation of the estimates in our actuarial method of reserving. We believe that medical expenses payable is adequate to cover future claims payments required. However, such estimates are based on knowledge of current events and anticipated future events. Therefore, the actual liability could differ materially from the amounts provided.
We reassess the profitability of contracts for providing coverage to members when current operating results or forecasts indicate probable future losses. A premium deficiency reserve is established in current operations to the extent that the sum of expected future costs, claim adjustment expenses, and maintenance costs exceed related future premiums under contracts without consideration of investment income. For purposes of determining premium deficiencies, contracts are grouped in a manner consistent with the method of acquiring, servicing, and measuring the profitability of such contracts. Losses recognized as a premium deficiency result in a beneficial effect in subsequent periods as operating losses under these contracts are charged to the liability previously established.
Part D Subsidies
We also receive advance payments each month from CMS related to Catastrophic Reinsurance, Coverage Gap Discount, and the Low-Income Member Cost Sharing Subsidy (“Subsidies”). Reinsurance subsidies represent funding from CMS for our portion of prescription drug costs, which exceed the member’s out-of-pocket threshold or the catastrophic coverage level. Low-income cost subsidies represent funding from CMS for all or a portion of the deductible, the coinsurance and co-payment amounts above the out-of-pocket threshold for low-income beneficiaries. Additionally, the Health Care Reform Law mandates consumer discounts of 75% on brand-name prescription drugs for Part D plan participants in the coverage gap. The majority of the discounts are funded by the pharmaceutical manufacturers, while we fund a smaller portion and administer the application of the total discount. These Subsidies represent cost reimbursements under the Medicare Part D program and are recorded as deposits or payables.
These Subsidies received in excess of, or less than, actual subsidized benefits paid are refundable to or recoverable from CMS through an annual reconciliation process following the end of the contract year.
For 2021, we incurred $93,320 of subsidized benefits which were more than the $87,638 of Subsidies received by $5,682 which was recorded within prepaid expenses and other current assets on the consolidated balance sheets. For 2020, we incurred $70,594 of subsidized benefits which were more than the $59,402 of Subsidies received by $11,192 which was recorded within prepaid expenses and other current assets on the consolidated balance sheets.
Shared Risk Reserve Arrangements
We established a fund (also referred to as “a pool”) for risk and profit-sharing with various independent physician associations (“IPAs”). The pool enables us and our IPAs to share in the financial responsibility and/or upside associated with providing covered medical expenses to our members. The risk pool is based on a contractually agreed upon medical budget, typically based upon a percentage of revenue. If actual medical expenses are less than the budgeted amount, this results in a surplus. Conversely, if actual medical expenses are greater than the budgeted amount, this results in a deficit. We will distribute the surplus, or a portion thereof, to each IPA based upon contractual terms. Deficits are charged to shared risk providers’ risk pool as per the contractual term and evaluated for collectability at each reporting period.
We record risk-sharing receivables and payables on a gross basis on the consolidated balance sheet. Throughout the year, we evaluate expected losses on risk-sharing receivables and record the resulting expected losses to the reserve. We systematically build and release reserves based on adequacy and its assessment of expected losses on a monthly basis. Credit loss associated with risk share deficit receivables are recorded within medical expense in the consolidated statements of operations. As of December 31, 2021 and December 31, 2020, we recorded a valuation allowance for all of the risk-sharing receivable balance due to collection risk related to the balance. The risk-sharing payable is included within medical expenses payable on the consolidated balance sheet.
Concentrations of Credit Risk
Financial instruments that potentially subject us to concentrations of credit risk consist primarily of cash deposits and restricted investments with financial institutions. Accounts at each financial institution are insured by the Federal Deposit Insurance Corporation (“FDIC”) up to certain limits. At December 31, 2021 and December 31, 2020, there was $465,824 and $205,882, respectively, in excess of FDIC-insured limits.
Industry Tax
Section 9010 of the Patient Protection and Affordable Care Act imposes an annual, nondeductible insurance industry tax (“Industry Tax”), which is levied proportionately across the insurance industry for risk-based products. The Industry Tax was estimated based on a ratio of our net premiums written compared to the US Health insurance total net premiums. The Industry Tax was $0, $12,286, and $0 for the years ended December 31, 2021, 2020, and 2019, respectively, and was reported as selling, general and administrative expenses. The Industry Tax was on moratorium during 2019 and has been repealed for calendar years beginning after December 31, 2020.
96
Income Taxes
We account for income taxes using the asset and liability method. Deferred tax assets and liabilities are determined based on temporary differences between the bases used for financial reporting and income tax reporting purposes based on the enacted tax rates and laws that will be in effect at the time such temporary differences are expected to reverse.
The recognition of deferred tax assets requires an assessment to determine the realization of such assets. Realization refers to the incremental benefits achieved through the reductions in future taxes payable or refunds receivable from the deferred tax assets, assuming that the underlying deductible differences and carryforwards are the last items to enter into the determination of future taxable income. We establish a valuation allowance for tax assets when it is more likely than not that they will not be realized, based on all available positive and negative evidence.
We account for uncertainty in income taxes using a “more-likely-than-not” recognition threshold. We consider many factors when evaluating and estimating our tax positions and tax benefits, which may require periodic adjustments, and which may not accurately reflect actual outcomes. Interest and penalties related to uncertain tax benefits are recognized as a component of interest expense and income tax expense, respectively, in the consolidated statement of operations.
Member Acquisition Costs
Member acquisition costs primarily relate to internal and external broker commission costs. These member acquisition costs related to our health services contract with our members are expensed as incurred and are recorded as selling, general and administrative expenses. These short-term health services contract typically have a one-year term and may be canceled by the member.
Advertising Expenses
The Company expenses the costs of advertising as incurred. Advertising expenses were $3,581, $1,505, and $202, for the years ended December 31, 2021, 2020, and 2019, respectively, and were reported as selling, general and administrative expenses.
Equity-Based Compensation
Equity-based compensation expense is measured and recognized based on the grant date fair value of the awards. The grant date fair value of stock options is estimated using the Black-Scholes option pricing model. The grant date fair value of Restricted Stock Units (“RSUs”) and Restricted Stock Awards (“RSAs”) is estimated based on the fair value of our underlying common stock.
The Black-Scholes option pricing model requires the use of highly subjective assumptions, including the award’s expected term, the fair value of the underlying common stock, the expected volatility of the price of the common stock, risk-free interest rates, and the expected dividend yield of the common stock. The assumptions used to determine the fair value of the stock-based awards are management’s best estimates and involve inherent uncertainties and the application of judgment. The expected term represents the period the stock-based awards are expected to be outstanding. As we do not have sufficient historical experience for determining the expected term of the stock option awards granted, it was on the simplified method available under U.S. GAAP. As we do not have a substantial trading history, volatility assumptions were developed using the historical volatilities of a set of peer companies, adjusted for debt-equity leverage. Equity-based compensation expense for awards with service-based vesting only is recognized on a graded vesting schedule over the requisite service period of the awards, which is generally four years. We account for forfeitures as they occur.
Additionally, prior to the IPO, the Parent had granted its Class B and Class C units to certain of our executives and board members ("Incentive Units") and had also approved the Company’s Stock Appreciation Rights (“SARs”) Plan. Upon the IPO, SARs were modified and concurrently were partially settled in cash and partially settled with issuance of common stock, a portion of which is restricted as discussed in Note 10 below.
During March of 2021, we also amended certain of our contracts with third-party business partners and agreed to issue shares of common stock at the IPO price, in consideration for the discharge of certain contingent payment obligations under such agreements ("Stock Payment") as discussed in Note 10.
Equity-based compensation is recorded within selling, general and administrative expenses, and medical expenses based on the function of the applicable employee and non-employee.
Noncontrolling interest
Noncontrolling interest represents the portion of equity ownership in a subsidiary that is not attributable to Alignment Healthcare, Inc. The noncontrolling interest in a subsidiary was initially recognized at estimated fair value on April 1, 2021 and is presented within total equity in the Company's consolidated balance sheets. There was no net loss attributable to the noncontrolling interest for the year ended December 31, 2021 as the Company was responsible for 100% of the net loss in the first year of operations of that subsidiary.
97
Net Loss per Share
Net loss per share is calculated based on net loss attributable to Alignment Healthcare, Inc.'s shareholders. The following table sets forth the computation of basic and diluted net loss per share for the years ended December 31, 2021, 2020, and 2019:
|
|
Year Ended |
|
|||||||||
|
|
2021 |
|
|
2020 |
|
|
2019 |
|
|||
Numerator: |
|
|
|
|
|
|
|
|
|
|||
Net loss attributable to common stockholders |
|
$ |
(195,286 |
) |
|
$ |
(22,926 |
) |
|
$ |
(44,732 |
) |
Denominator: |
|
|
|
|
|
|
|
|
|
|||
Total weighted-average common shares outstanding, inclusive of restricted shares of common stock - |
|
|
181,917,964 |
|
|
|
161,323,531 |
|
|
|
147,157,803 |
|
Less: Restricted shares of common stock |
|
|
9,961,115 |
|
|
|
9,191,232 |
|
|
|
11,294,939 |
|
Total weighted-average common shares outstanding - |
|
|
171,956,849 |
|
|
|
152,132,299 |
|
|
|
135,862,864 |
|
Net loss per share: |
|
|
|
|
|
|
|
|
|
|||
Net loss per share - basic and diluted |
|
$ |
(1.14 |
) |
|
$ |
(0.15 |
) |
|
$ |
(0.33 |
) |
Basic net loss per share is the same as diluted net loss per share for periods presented as the inclusion of all potentially dilutive shares would have been anti-dilutive.
In addition to the restricted shares of common stock, we also excluded the following potential common shares, presented based on amounts outstanding at each period end, from the computation of diluted net loss per share as of December 31, 2021, 2020, 2019:
|
|
December 31, |
|
|||||||||
|
|
2021 |
|
|
2020 |
|
|
2019 |
|
|||
Stock options |
|
|
10,938,521 |
|
|
|
— |
|
|
|
— |
|
Restricted stock units |
|
|
1,662,282 |
|
|
|
— |
|
|
|
— |
|
Total |
|
|
12,600,803 |
|
|
|
— |
|
|
|
— |
|
Recent Accounting Pronouncements Adopted
On January 1, 2021, we early adopted Accounting Standards Update (“ASU”) No. 2017-04, Simplifying the Test for Goodwill Impairment. This ASU eliminates the requirement to calculate the implied fair value of goodwill to measure a goodwill impairment charge. A goodwill impairment charge would be recognized if the carrying amount of a reporting unit exceeds the estimated fair value of the reporting unit. This guidance did not have a material impact to our consolidated financial statements.
On January 1, 2021, we adopted ASU No. 2018-17, Targeted Improvements to Related Party Guidance for Variable Interest Entities, which provides clarification on determining whether a decision-making fee is a variable interest. This ASU requires reporting entities to consider indirect interests held through related parties under common control on a proportional basis rather than as the equivalent of a direct interest in its entirety. This guidance did not have a material impact to our consolidated financial statements.
On January 1, 2021, we adopted ASU No. 2018-15, Customer’s Accounting for Implementation Costs Incurred in a Cloud Computing Arrangement That Is a Service Contract, which aligns the requirements for capitalization implementation costs incurred in a hosting arrangement that is a service contract with the requirement for capitalizing implementation costs incurred to develop or obtain internal-use software. Capitalized implementation costs related to a hosting arrangement that is a service contract will be amortized over the term of the hosting arrangement. New disclosures are required. This guidance did not have a material impact to our consolidated financial statements.
3. Fair Value
U.S. Treasury bills and certificate of deposits are reported at amortized costs which is equivalent to fair value. The following tables present the carrying value and fair value of these financial instruments as of December 31, 2021 and 2020:
|
|
December 31, 2021 |
|
|||||||||||||
|
|
|
|
|
Fair Value |
|
||||||||||
|
|
Carrying |
|
|
Level 1 |
|
|
Level 2 |
|
|
Level 3 |
|
||||
U.S. Treasury bills |
|
$ |
1,375 |
|
|
$ |
— |
|
|
$ |
1,375 |
|
|
$ |
— |
|
Certificate of deposits |
|
|
1,071 |
|
|
|
— |
|
|
|
1,071 |
|
|
|
— |
|
Total |
|
$ |
2,446 |
|
|
$ |
— |
|
|
$ |
2,446 |
|
|
$ |
— |
|
98
|
|
December 31, 2020 |
|
|||||||||||||
|
|
|
|
|
Fair Value |
|
||||||||||
|
|
Carrying |
|
|
Level 1 |
|
|
Level 2 |
|
|
Level 3 |
|
||||
U.S. Treasury bills |
|
$ |
325 |
|
|
$ |
— |
|
|
$ |
325 |
|
|
$ |
— |
|
Certificate of deposits |
|
|
1,115 |
|
|
|
— |
|
|
|
1,115 |
|
|
|
— |
|
Total |
|
$ |
1,440 |
|
|
$ |
— |
|
|
$ |
1,440 |
|
|
$ |
— |
|
The carrying value of long-term debt represents the outstanding balance, net of unamortized debt issuance costs. As of December 31, 2021 the carrying value and fair value of our long-term debt was $150,620 and $154,367, respectively. As of December 31, 2020, the carrying value and fair value of our long-term debt was $144,168 and $149,965, respectively.
The fair value of our long-term debt is classified as a Level 3 financial instrument because certain inputs used to determine its fair value are not observable. The fair value was estimated using a discounted cash flow (“DCF”) methodology. The discount rate used in the DCF model was estimated based on a synthetic credit rating analysis for us, and a screening of market data to identify market yields of instruments within the range of identified credit ratings and with otherwise similar features.
Our nonfinancial assets and liabilities, which include goodwill, intangible assets, property, and equipment, are not required to be measured at fair value on a recurring basis. However, on a periodic basis, or whenever events or changes in circumstances indicate that their carrying value may not be recoverable, we assess these assets for impairment. No such impairment resulted during the years ended December 31, 2021, 2020, and 2019.
4. Accounts Receivable
Accounts receivable consisted of the following as of December 31, 2021 and 2020:
|
|
December 31, |
|
|
December 31, |
|
||
Government receivables |
|
$ |
19,685 |
|
|
$ |
10,392 |
|
Pharmacy rebates |
|
|
34,376 |
|
|
|
25,888 |
|
Other receivables |
|
|
4,562 |
|
|
|
3,860 |
|
Total accounts receivable |
|
|
58,623 |
|
|
|
40,140 |
|
Allowance for credit losses |
|
|
(111 |
) |
|
|
— |
|
Accounts receivable, net |
|
$ |
58,512 |
|
|
$ |
40,140 |
|
The allowance for expected credit losses for accounts receivable is based primarily on past collections experience relative to the length of time receivables are past due. However, when available evidence reasonably supports an assumption that future economic conditions will differ from current and historical payment collections, an adjustment is reflected in the allowance for expected credit losses. We record pharmacy rebates and other receivables based on contractual terms and expected collections and our estimation process for contractual allowances for such balances generally results in an allowance for balances outstanding greater than 90 days or if expected credit risks are known.
Receivables and any associated allowance are written off only when all collection attempts have failed and such amounts are determined unrecoverable. We regularly review the adequacy of these allowances based on a variety of factors, including age of the outstanding receivable and collection history. When circumstances related to specific collection patterns change, estimates of the recoverability of receivables are adjusted. Because substantially all of our receivable amounts are readily determinable and a large portion of our creditors are governmental authorities, our allowance for credit losses is insignificant.
We recorded credit loss related to accounts receivable of $111, $118, $1,424 during the years ended December 31, 2021, 2020, and 2019, respectively. The amounts were recorded in selling general, and administrative expenses in the consolidated statements of operations.
99
5. Property and Equipment
Property and equipment consisted of the following as of December 31, 2021 and 2020:
|
|
December 31, |
|
|
December 31, |
|
||
Computers and equipment |
|
$ |
9,164 |
|
|
$ |
8,309 |
|
Office equipment and furniture |
|
|
4,416 |
|
|
|
4,363 |
|
Software |
|
|
98,031 |
|
|
|
79,204 |
|
Leasehold improvements |
|
|
6,196 |
|
|
|
6,083 |
|
Construction in progress |
|
|
753 |
|
|
|
1,893 |
|
Subtotal |
|
|
118,560 |
|
|
|
99,852 |
|
Less accumulated depreciation |
|
|
(88,202 |
) |
|
|
(72,707 |
) |
Property and equipment-net |
|
$ |
30,358 |
|
|
$ |
27,145 |
|
Depreciation expense for the year ended December 31, 2021 was $15,671, of which $220 was included in medical expenses. Depreciation expense for the years ended December 31, 2020 and 2019 was $15,134 and $16,257, respectively, of which $366 and $1,661, respectively, was included in medical expenses.
6. Goodwill and Intangible Assets
Intangible assets consisted of the following as of December 31, 2021 and 2020:
|
|
December 31, 2021 |
||||||||||||
|
|
Gross Carrying Value |
|
|
Accumulated Amortization |
|
|
Net Carrying Value |
|
|
Weighted Average Life |
|||
Goodwill |
|
$ |
29,303 |
|
|
$ |
— |
|
|
$ |
29,303 |
|
|
|
License (indefinite lived) |
|
|
4,917 |
|
|
|
— |
|
|
|
4,917 |
|
|
|
Plan member relationships |
|
|
2,700 |
|
|
|
2,311 |
|
|
|
389 |
|
|
9 years |
Other |
|
|
1,050 |
|
|
|
543 |
|
|
|
507 |
|
|
2 - 10 years |
|
|
$ |
37,970 |
|
|
$ |
2,854 |
|
|
$ |
35,116 |
|
|
|
|
|
December 31, 2020 |
||||||||||||
|
|
Gross Carrying Value |
|
|
Accumulated Amortization |
|
|
Net Carrying Value |
|
|
Weighted Average Life |
|||
Goodwill |
|
$ |
29,303 |
|
|
$ |
— |
|
|
$ |
29,303 |
|
|
|
License (indefinite lived) |
|
|
4,500 |
|
|
|
— |
|
|
|
4,500 |
|
|
|
Plan member relationships |
|
|
2,700 |
|
|
|
2,034 |
|
|
|
666 |
|
|
9 years |
Other |
|
|
633 |
|
|
|
457 |
|
|
|
176 |
|
|
2 - 10 years |
|
|
$ |
37,136 |
|
|
$ |
2,491 |
|
|
$ |
34,645 |
|
|
|
Amortization expense relating to intangible assets for the years ended December 31, 2021, 2020, and 2019, was $362, $327, and $327, respectively. Estimated amortization expense relating to intangible assets for each of the next five years ending December 31, is as follows:
2022 |
|
$ |
386 |
|
2023 |
|
|
226 |
|
2024 |
|
|
82 |
|
2025 |
|
|
60 |
|
2026 |
|
|
60 |
|
Thereafter |
|
|
82 |
|
|
|
$ |
896 |
|
There were no impairment charges related to goodwill and intangible assets for the years ended December 31, 2021, 2020, and 2019.
100
7. Medical Expenses Payable
The following table is a detail of medical expenses payable as of December 31, 2021 and 2020:
|
|
December 31, |
|
|
December 31, |
|
||
Claims incurred but not paid |
|
$ |
77,073 |
|
|
$ |
82,391 |
|
Capitation payable, risk-sharing payable, and other |
|
|
48,813 |
|
|
|
30,214 |
|
|
|
$ |
125,886 |
|
|
$ |
112,605 |
|
Each period, we re-examine previously established outstanding claims reserve estimates based on actual claims submissions and other changes in facts and circumstances. As more complete claim information becomes available, we adjust the amount of the estimates and include the changes in estimates in claim costs in the period in which the change is identified. Substantially, all of the total claims paid by us are known and settled within the first year from the date of service, and substantially, all remaining claim amounts are paid within a three-year period.
The following table presents components of the change in medical expenses payable as of December 31 2021, 2020, and 2019 :
|
|
December 31, |
|
|
December 31, |
|
|
December 31, |
|
|||
Claims incurred but not paid - beginning balance |
|
$ |
82,391 |
|
|
$ |
83,939 |
|
|
$ |
52,898 |
|
Incurred related to: |
|
|
|
|
|
|
|
|
|
|||
Current year |
|
|
327,224 |
|
|
|
281,124 |
|
|
|
274,871 |
|
Prior years |
|
|
(8,064 |
) |
|
|
(19,494 |
) |
|
|
(11,113 |
) |
Total incurred, net of reinsurance |
|
|
319,160 |
|
|
|
261,630 |
|
|
|
263,758 |
|
Payments related to: |
|
|
|
|
|
|
|
|
|
|||
Current year |
|
|
251,629 |
|
|
|
206,288 |
|
|
|
196,086 |
|
Prior years |
|
|
72,849 |
|
|
|
56,890 |
|
|
|
36,631 |
|
Total payments, net of reinsurance |
|
|
324,478 |
|
|
|
263,178 |
|
|
|
232,717 |
|
Claims incurred but not paid - ending balance |
|
|
77,073 |
|
|
|
82,391 |
|
|
|
83,939 |
|
Other medical expenses payable |
|
|
48,813 |
|
|
|
30,214 |
|
|
|
18,445 |
|
Total medical expenses payable |
|
$ |
125,886 |
|
|
$ |
112,605 |
|
|
$ |
102,384 |
|
In March 2020, the COVID-19 outbreak was declared a pandemic. The COVID-19 virus disproportionately impacts older adults, especially those with chronic illnesses, which describes many of the seniors we serve. For the three months ended March 31, 2021, we experienced higher claims costs due to COVID-19 related inpatient admissions. However, for the remainder of fiscal year 2021, we saw a decline in COVID-related utilization (compared to the first quarter) as vaccination rates improved across our senior population. The Delta and Omicron variants caused a rebound in COVID-related inpatient utilization during the second half of 2021, however, the increase in utilization did not reach first quarter of 2021 levels given overall vaccination rates. While COVID had a less significant impact on our second, third, and fourth quarter medical expense relative to our first quarter medical expense, we remain cautious of the potential impact of the Delta and Omicron variants in the future. Cumulatively, incurred claims increased in 2021 due to higher membership. The ultimate impact of COVID-19 to us and our financial condition is presently unknown and we continue to monitor the impact of COVID-19 on our claims reserve estimate.
We re-examine previously established outstanding claims reserve estimates based on actual claims submissions and other changes in facts and circumstances. We recognized a favorable prior year development, excluding provision for adverse deviation, of $4,166, $14,552, and $8,169 for the years ended December 31, 2021, 2020, and 2019, respectively. The favorable prior year development incurred in 2021, 2020 and 2019 was primarily due to better-than-expected claims recoveries and actual claims expense being less than expected. The impact was greater in 2020 given focused claim recovery activities that commenced in the latter half of 2019 and continued in 2020.
The following tables provide information about incurred and paid claims development as of December 31, 2021:
|
|
Cumulative Incurred Claims, Net of Reinsurance For the Years Ended December 31, |
|
|||||||||
Claims Incurred Year |
|
2019 |
|
|
2020 |
|
|
2021 |
|
|||
2019 |
|
$ |
274,871 |
|
|
$ |
256,810 |
|
|
$ |
253,759 |
|
2020 |
|
|
|
|
|
281,124 |
|
|
|
276,111 |
|
|
2021 |
|
|
|
|
|
|
|
|
327,224 |
|
||
Total |
|
|
|
|
|
|
|
$ |
857,094 |
|
||
101
|
|
Cumulative Claims Paid, Net of Reinsurance For the Years Ended December 31, |
|
|
Cumulative Number of |
|
||||||||||
Claims Incurred Year |
|
2019 |
|
|
2020 |
|
|
2021 |
|
|
|
|
||||
2019 |
|
$ |
196,086 |
|
|
$ |
251,507 |
|
|
$ |
255,628 |
|
|
|
410,500 |
|
2020 |
|
|
|
|
|
206,288 |
|
|
|
275,016 |
|
|
|
336,212 |
|
|
2021 |
|
|
|
|
|
|
|
|
251,629 |
|
|
|
234,191 |
|
||
Total |
|
|
|
|
|
|
|
$ |
782,273 |
|
|
|
|
|||
Substantially all of the claims incurred but not paid as of December 31, 2021 relate to the current year.
There is no single or common claim frequency metric used in the health care industry. We believe a relevant metric for our health insurance business is the cumulative number of claims paid for each incurred year. Claims that did not result in a liability are not included in the frequency metric.
8. Long-Term Debt
Long-term debt is recorded at carrying value in the consolidated balance sheets. The carrying value of long-term debt outstanding, net of unamortized debt issuance costs, consisted of the following as of December 31, 2021 and 2020:
|
|
December 31, |
|
|
December 31, |
|
||
Long-term debt |
|
$ |
154,112 |
|
|
$ |
149,915 |
|
Less unamortized debt issuance costs |
|
|
(3,492 |
) |
|
|
(5,747 |
) |
Long-term debt-net of amortization |
|
|
150,620 |
|
|
|
144,168 |
|
Less current portion of long-term debt |
|
|
— |
|
|
|
— |
|
Long-term debt - net of current portion |
|
$ |
150,620 |
|
|
$ |
144,168 |
|
In August 2018, we entered into a term loan for $80,000 with an option to borrow up to an additional $20,000. In April 2019, we amended the term loan to increase our borrowing capacity by $75,000. The terms and conditions in the term loan remain the same unless otherwise stated in the amendment. The term loan was subject to a commitment fee of $6,750 and we incurred debt issuance costs of $3,625.
Debt issuance costs relate to attorney fees, other third-party costs, and commitment fees that represent 5% of the amount borrowed. We are required to pay the commitment fees when the term loan is due or when the term loan is repaid, whichever comes first. Debt issuance costs were deferred and are amortized to interest expense over the debt term using the effective interest method. Debt issuance costs are presented in the consolidated balance sheet as a direct deduction from the carrying value of the term loan.
The term loan (including the related amendment) bears interest at a rate of 10.25% payable on a quarterly basis. We have the option to pay a portion of the interest rate in cash, and the remaining portion of the interest rate will be added to the debt principal balance as a payment-in-kind. The payment-in-kind is also subject to a commitment fee of 5%. The cash and payment-in-kind interest rates were 7.75% and 2.5%, respectively, through April 2019 and converted to 7.50% and 2.75%, respectively, for the remainder of 2019 and 2020. In 2021 and 2020, we utilized our option to pay the quarterly interest payments in both cash and payment-in-kind. As of December 31, 2021, the total long-term debt balance of $154,112 included the principal balance of $135,000, the initial commitment fee of $6,750, and the payment-in-kind interest on the principal balance of $12,082. The payment-in-kind interest on the principal balance is also subject to the commitment fee which was $280 as of December 31, 2021. This amount was also included in the long-term debt balance. As of December 31, 2020, the total long-term debt balance of $149,915 included the principal balance of $135,000, the initial commitment fee of $6,750, and payment-in-kind interest of $8,051. The payment-in-kind interest on the principal balance was subject to the commitment fee which was $114 as of December 31, 2020.
The term loan matures in , at which time the full balance of the term loan, including the commitment fee and the payment-in-kind balance, will be due.
In addition, the term loan includes financial covenants regarding the maintenance of minimum liquidity of $6,000 of operating cash, as defined, on a consolidated basis, at least $10,000 in its cash accounts on a daily basis and minimum consolidated revenue amounts. The term loan also contains certain nonfinancial covenants. As of December 31, 2021 and 2020, we were in compliance with all financial and nonfinancial covenants.
The term loan was entered into by our wholly owned subsidiary and is also guaranteed by certain of our wholly owned subsidiaries and collateralized by all unrestricted assets of our subsidiaries.
9. Income Taxes
There was no income tax expense for the years ended December 31, 2021 and 2020.
The reconciliation of income tax expense recorded in the consolidated statement of operations and amounts computed at the statutory federal
income tax rate for the years ended December 31, 2021 and 2020, were as follows:
102
|
|
2021 |
|
|
2020 |
|
|
2019 |
|
|||||||||||||||
|
|
Amount |
|
|
Percentage |
|
|
Amount |
|
|
Percentage |
|
|
Amount |
|
|
Percentage |
|
||||||
Loss before tax at statutory federal rate |
|
$ |
(41,010 |
) |
|
|
21.0 |
% |
|
$ |
(4,814 |
) |
|
|
21.0 |
% |
|
$ |
(9,394 |
) |
|
|
21.0 |
% |
Valuation allowance |
|
|
42,597 |
|
|
|
(21.8 |
) |
|
|
(833 |
) |
|
|
3.6 |
|
|
|
12,066 |
|
|
|
(27.0 |
) |
State income tax - net of federal tax benefit |
|
|
(10,412 |
) |
|
|
5.3 |
|
|
|
(1,289 |
) |
|
|
5.6 |
|
|
|
(2,892 |
) |
|
|
6.5 |
|
Nondeductible expenses |
|
|
293 |
|
|
|
(0.1 |
) |
|
|
60 |
|
|
|
(0.2 |
) |
|
|
187 |
|
|
|
(0.4 |
) |
Equity-based compensation |
|
|
621 |
|
|
|
(0.3 |
) |
|
|
446 |
|
|
|
(1.9 |
) |
|
|
— |
|
|
|
— |
|
Cumulative deferred adjustment and other |
|
|
(394 |
) |
|
|
0.2 |
|
|
|
2,600 |
|
|
|
(11.3 |
) |
|
|
— |
|
|
|
— |
|
ACA Health insurer fee |
|
|
— |
|
|
|
— |
|
|
|
2,580 |
|
|
|
(11.3 |
) |
|
|
— |
|
|
|
— |
|
Provision to return adjustment |
|
|
(11 |
) |
|
|
— |
|
|
|
1,250 |
|
|
|
(5.5 |
) |
|
|
33 |
|
|
|
(0.1 |
) |
Nondeductible executive compensation |
|
|
8,316 |
|
|
|
(4.3 |
) |
|
|
— |
|
|
|
— |
|
|
|
— |
|
|
|
— |
|
Net deferred taxes |
|
$ |
— |
|
|
|
|
|
$ |
— |
|
|
|
|
|
$ |
— |
|
|
|
|
|||
The components of deferred income taxes as of December 31, 2021 and 2020, were as follows:
|
|
December 31, |
|
|
December 31, |
|
||
Deferred tax assets: |
|
|
|
|
|
|
||
Federal and state net operating loss carryforwards |
|
$ |
97,039 |
|
|
$ |
90,351 |
|
Employee benefits |
|
|
38,398 |
|
|
|
5,466 |
|
Interest deduction limitation |
|
|
8,062 |
|
|
|
4,484 |
|
Other |
|
|
1,471 |
|
|
|
1,340 |
|
Gross deferred tax assets |
|
|
144,970 |
|
|
|
101,641 |
|
Deferred tax liabilities: |
|
|
|
|
|
|
||
Intangibles |
|
|
(1,252 |
) |
|
|
(1,491 |
) |
Depreciation |
|
|
(545 |
) |
|
|
(1,646 |
) |
Lease liabilities |
|
|
(516 |
) |
|
|
(262 |
) |
Gross deferred tax liabilities |
|
|
(2,313 |
) |
|
|
(3,399 |
) |
Net deferred tax assets |
|
|
142,657 |
|
|
|
98,242 |
|
Valuation allowance |
|
|
(142,657 |
) |
|
|
(98,242 |
) |
Net deferred taxes |
|
$ |
— |
|
|
$ |
— |
|
Valuation allowances are provided when it is considered more likely than not that deferred tax assets will not be realized. The valuation allowances primarily relate to future tax benefits on certain federal and state net operating loss (“NOL”) carryforwards. For the years ended December 31, 2021 and 2020, federal NOL carryforwards were $343,323 and $322,808, respectively. For the years ended December 31, 2021 and 2020, state NOL carryforwards were $374,006 and $343,140, respectively, and $56,457 of the total federal net operating loss carryforwards have an indefinite life while the remaining federal and state net operating loss carryforwards begin to expire in 2033 if not utilized.
Of the total NOL carryforwards, approximately $19,031 of federal and $13,221 of California NOL carryforwards relate to Alignment Health Plan, Inc. for which the utilization of the federal NOL carryforward is subject to a federal Section 382 limitation of $870 per year, and the utilization of the California NOL carryforwards is subject to a similar California annual limitation. In June 2020, California’s Governor signed into law Assembly Bill (“AB”) 85 suspending California NOL utilization for taxpayers with more than $1 million of taxable income, effective for tax years 2020, 2021, and 2022. AB 85 includes an extended carryover period for the suspended NOLs with an additional year carryforward for each year of suspension.
We have cumulative NOLs as of December 31, 2021 and 2020. Given the history of losses, and after consideration for the risk associated with estimates of future taxable income, we established a full valuation allowance against net deferred tax assets at December 31, 2021 and 2020. As a result of the Tax Cuts and Jobs Act (“TCJA”), the federal NOLs generated in 2018 through 2020 will be carried forward indefinitely and are limited to an 80% deduction of taxable income. The 80% limitation is not applicable to NOLs generated before 2018. An exception to the TCJA federal NOL modification applies to nonlife insurance companies (e.g., Alignment Health Plan Inc.). Alignment Health Plan Inc.’s NOL treatment is the same as those NOLs generated in tax years 2017 and prior.
Additionally, an “ownership change” as defined under Section 382 of the Internal Revenue Code, could potentially limit the ability to utilize certain tax attributes including the Company’s substantial NOLs. Ownership change is generally defined as any significant change in ownership of more than 50% of its stock over a three-year testing period. If, as a result of current or future transactions involving our common stock, we undergo cumulative ownership changes which exceed 50% over the testing period, our ability to utilize our NOL carryforwards would be subject to additional limitations under IRC Section 382. We continue to monitor changes in ownership with respect to these income tax provisions.
The CARES Act, which was enacted on March 27, 2020, provides for deferred payment of the employer portion of social security taxes due between March 27, 2020 and December 31, 2020, with 50% due by December 31, 2021 and the remaining 50% due by December 31, 2022. We began deferring the employer portion of its social security taxes in April 2020. As of December 31, 2021 and 2020, the deferred portion of social security taxes amounted to $1,072 and $2,140, respectively.
As of December 31, 2021 and 2020, there were no liabilities for unrecognized tax benefits.
103
10. Equity-Based Compensation
2021 Equity Incentive Plan
In connection with the IPO, on March 25, 2021, our Board of Directors adopted the 2021 Equity Incentive Plan (the “2021 Plan”). Under the 2021 Plan, employees, consultants and directors of our company and our affiliates that perform services for us are eligible to receive awards. The 2021 Plan provides for the grant of incentive stock options (“ISOs”), non-statutory stock options (“NSOs”), stock appreciation rights, restricted shares, performance awards, other share-based awards (including restricted stock units) and other cash-based awards. ISOs may be granted only to employees, including officers. All other awards may be granted to employees, including officers, non-employee directors and consultants. The maximum number of shares available for issuance under the 2021 Plan may not exceed 20,744,444 shares (subject to a discretionary annual increase of up to 4% effective as of January 1 of each year for 10 years).
IPO-Equity Awards
Stock options
Our outstanding stock options generally vest 25% annually over four years and generally expire 10 years from the date of the grant. The 2021 Plan provides that stock option grants will be made at no less than the estimated fair value of common stock at the date of the grant.
The following is a summary of the stock option transactions as of and for the year ended December 31, 2021:
|
|
Stock Options Outstanding |
|
|||||||||||||
(amounts in thousands, except shares and per share amount) |
|
Shares Subject to Options Outstanding |
|
|
Weighted- Average Exercise Price per Option |
|
|
Weighted- Average Remaining Contractual Terms (in years) |
|
|
Aggregate Intrinsic Value |
|
||||
Balances as of December 31, 2020 |
|
|
— |
|
|
$ |
— |
|
|
|
|
|
|
|
||
Options granted |
|
|
11,263,389 |
|
|
|
18.02 |
|
|
|
|
|
|
|
||
Options exercised |
|
|
— |
|
|
|
— |
|
|
|
|
|
|
|
||
Options forfeited / expired |
|
|
(324,868 |
) |
|
|
18.15 |
|
|
|
|
|
|
|
||
Balances as of December 31, 2021 |
|
|
10,938,521 |
|
|
$ |
18.02 |
|
|
|
9.17 |
|
|
$ |
— |
|
Vested |
|
|
— |
|
|
$ |
— |
|
|
|
— |
|
|
$ |
|
|
Exercisable as of December 31, 2021 |
|
|
— |
|
|
$ |
— |
|
|
|
— |
|
|
$ |
— |
|
Aggregate intrinsic value represents the difference between the exercise price of the option and the closing price of our common stock. The aggregate intrinsic value of options exercised for the years ended December 31, 2021, 2020, and 2019 was $0. The fair value of options granted during the year ended December 31, 2021 was $85,043. As the options were all granted in 2021 there was no related compensation expense in 2020 and 2019.
The weighted-average assumptions used to determine the fair value of stock options granted during the periods presented were as follows:
|
|
Year Ended December 31, |
|||
|
|
2021 |
|
|
|
Expected term (in years)(1) |
|
|
6.25 |
|
|
Expected volatility(2) |
|
33.7% - 41.7% |
|
|
|
Risk-free interest rate(3) |
|
0.9% - 1.4% |
|
|
|
Dividend yield(4) |
|
0% |
|
|
|
(1)
(2)
(3)
(4)
Restricted Stock Awards
Our outstanding RSAs that were granted following the IPO generally vest 25% annually over four years. RSAs converted from Pre-IPO awards generally vest on the later of the fourth anniversary of the original vesting commencement date or 50% annually on the first and second anniversary of the IPO (see “Pre-IPO Equity” and "Modifications" sections below for details).
104
The following is a summary of RSA transactions as of and for the year ended December 31, 2021:
|
|
Restricted Shares |
|
|
Weighted-Average Grant Date Fair Value |
|
||
Unvested and outstanding as of December 31, 2020 |
|
|
— |
|
|
$ |
— |
|
Converted |
|
|
10,348,789 |
|
|
|
8.47 |
|
Granted |
|
|
214,669 |
|
|
|
18.00 |
|
Vested |
|
|
(1,869,509 |
) |
|
|
1.21 |
|
Forfeited |
|
|
(80,169 |
) |
|
|
3.49 |
|
Unvested and outstanding as of December 31, 2021 |
|
|
8,613,780 |
|
|
$ |
10.32 |
|
Restricted Stock Units
Our outstanding RSUs generally vest 25% annually over four years.
The following is a summary of RSU transactions as of and for the year ended December 31, 2021:
|
|
Restricted Stock Units |
|
|
Weighted-Average Grant Date Fair Value |
|
||
Unvested and outstanding as of December 31, 2020 |
|
|
— |
|
|
$ |
— |
|
Granted |
|
|
1,740,523 |
|
|
|
18.54 |
|
Vested |
|
|
— |
|
|
|
— |
|
Cancelled/forfeited |
|
|
(78,241 |
) |
|
|
18.41 |
|
Unvested and outstanding as of December 31, 2021 |
|
|
1,662,282 |
|
|
$ |
18.54 |
|
Non-Employee Awards
During the year ended December 31, 2021, total payment of $10,328, under the Company’s Stock Payment arrangement, as discussed in Note 2, was settled upon our successful IPO in 573,782 shares of our common stock at $18 per share with 214,669 of such common stock restricted and vesting over of a performance period of four years. The unrecognized stock compensation related to these RSAs of $2,315 will be recognized over a graded vesting schedule over the performance period of the award.
Pre-IPO equity
Our Parent issued Incentive Units to certain employees, board members, and advisors, which were profits interests issued in Class B and Class C units. As of the IPO, only the time-vesting portion of Class B Incentive Units were fully vested.
In 2014, Alignment Healthcare Holdings, LLC’s Board of Directors adopted a Stock Appreciation Rights Plan (“SARs Plan”), under which Alignment Healthcare Holdings, LLC had granted awards in the form of SARs to employees, officers, directors, consultants, and other service providers of the Company.
Stock Appreciation Rights
80% of each SAR award vested 25% annually over four years and only becomes payable to the extent vested upon a qualified change in control (“Time-vesting SARs”), while the remaining 20% vests concurrent to the change in control (“Performance-vesting SARs”). The IPO was not considered a change in control under the original terms of the SARs. We have the option to settle SARs in either cash or equity upon an IPO.
In conjunction with the IPO, on March 24, 2021, the Company modified the Performance-vesting SARs to be converted into RSAs which vest 50% annually on each of the first and second anniversaries of the IPO. Vested Time-vesting SARs were settled approximately 50% in cash and 50% in common stock. The amount of SARs settled in cash was $11,399. The conversion of SARs resulted in the issuance of 300,489 RSAs.
The following table summarizes the equity-based awards activity as if the SARs were converted to RSAs and common stock at the earliest period presented.
105
|
|
Equivalent Shares of Restricted and Common Stock |
|
|
Outstanding at January 1, 2019 |
|
|
2,107,646 |
|
Grants |
|
|
— |
|
Canceled |
|
|
(262,723 |
) |
Outstanding at December 31, 2019 |
|
|
1,844,923 |
|
Grants |
|
|
— |
|
Canceled |
|
|
(156,695 |
) |
Outstanding at December 31, 2020 |
|
|
1,688,228 |
|
Grants |
|
|
— |
|
Canceled |
|
|
(110,719 |
) |
Cash settlement or converted into common stock |
|
|
(1,277,020 |
) |
Converted into unvested RSAs |
|
|
(300,489 |
) |
Outstanding at December 31, 2021 |
|
|
— |
|
Incentive Units
A portion of Incentive Units vest annually over four years (“Time-vesting Incentive Units”) and the remaining Incentive Units vest upon a change in control (“Performance-vesting Incentives Units”). The IPO was not considered a change in control under the original terms of the Incentive Units.
The following table summarizes the equity-based awards activity as if the Series B and C Incentive Units were converted to RSAs and common stock at the earliest period presented.
|
|
Equivalent Shares of RSA and Common Stock |
|
|
Weighted Average Grant Date Fair Value |
|
||
Balance as of January 1, 2019 |
|
|
19,316,762 |
|
|
$ |
0.60 |
|
Granted |
|
|
3,813,383 |
|
|
|
0.58 |
|
Canceled |
|
|
(944,631 |
) |
|
|
0.33 |
|
Redeemed |
|
|
— |
|
|
|
— |
|
Balance as of December 31, 2019 |
|
|
22,185,514 |
|
|
0.61 |
|
|
Granted |
|
|
2,738,479 |
|
|
|
2.42 |
|
Canceled |
|
|
(1,041,398 |
) |
|
|
0.44 |
|
Redeemed |
|
|
— |
|
|
|
— |
|
Balance as of December 31, 2020 |
|
|
23,882,595 |
|
|
0.83 |
|
|
Granted |
|
|
— |
|
|
|
— |
|
Canceled |
|
|
— |
|
|
|
— |
|
Redeemed |
|
|
(231,313 |
) |
|
|
0.44 |
|
Converted into common stock |
|
|
(13,602,982 |
) |
|
|
0.66 |
|
Converted into unvested RSAs |
|
|
(10,048,300 |
) |
|
|
1.06 |
|
Balance as of December 31, 2021 |
|
|
— |
|
|
$ |
— |
|
The following table summarizes unvested equity-based awards activity as if the Series B and C Incentive Units were converted to restricted common stock at the earliest period presented:
|
|
Equivalent Shares of Restricted Common Stock |
|
|
Weighted Average Grant Date Fair Value |
|
||
Balance as of January 1, 2019 |
|
|
9,412,545 |
|
|
$ |
0.44 |
|
Granted |
|
|
3,813,384 |
|
|
|
0.58 |
|
Vested |
|
|
(369,656 |
) |
|
|
0.48 |
|
Balance as of December 31, 2019 |
|
|
12,856,273 |
|
|
$ |
0.48 |
|
Granted |
|
|
2,738,479 |
|
|
|
2.42 |
|
Vested |
|
|
(3,788,924 |
) |
|
|
0.41 |
|
Balance as of December 31, 2020 |
|
|
11,805,828 |
|
|
$ |
0.96 |
|
Granted |
|
|
— |
|
|
|
— |
|
Vested |
|
|
(1,757,528 |
) |
|
|
0.33 |
|
Converted into unvested RSAs |
|
|
(10,048,300 |
) |
|
|
1.06 |
|
Balance as of December 31, 2021 |
|
|
— |
|
|
$ |
— |
|
106
Modifications
In conjunction with the Reorganization, the conversion of the Incentive Units into our RSAs was made pursuant to antidilution provisions of the original awards which required the award holders to be kept whole. As a result, there was no incremental compensation cost associated with the conversion.
In conjunction with the IPO, the Company modified the Time-vesting Incentive Units to be converted into RSAs and subject to the same time-vesting conditions upon the IPO, and modified the Performance-vesting SARs and Performance-vesting Incentive Units to be converted into RSAs which vest upon the later of the fourth anniversary of the original vesting commencement date or 50% annually on the first and second anniversary of the IPO.
Historically, no equity-based compensation expense was recognized for the SARs or Performance-vesting Incentive Units as the change in control was not probable.
As a result of the conversion and modification, we determined that the RSAs converted from the Performance-vesting SARs and the Performance-vesting Incentive Units should be remeasured as of the date of the modification (March 25, 2021).
The RSAs converted from the SARs were previously classified as liabilities and subject to remeasurement at fair value each reporting period. After the modification the converted RSAs were classified as equity, and were measured using the IPO stock price which will be recognized over the remaining modified vesting periods. The incremental compensation cost resulting from these modifications was $79,355.
Equity-Based Compensation Expense
Total equity-based compensation expense was presented on the statement of operations as follows:
|
|
Year Ended December 31, |
|
|||||||||
(amounts in thousands) |
|
2021 |
|
|
2020 |
|
|
2019 |
|
|||
Selling, general and administrative expenses |
|
$ |
106,581 |
|
|
$ |
2,124 |
|
|
$ |
1,157 |
|
Medical expenses |
|
|
15,418 |
|
|
|
— |
|
|
|
— |
|
Total equity-based compensation expense |
|
$ |
121,999 |
|
|
$ |
2,124 |
|
|
$ |
1,157 |
|
As of December 31, 2021, there was $110,534 in unrecognized compensation expense related to all non-vested awards (RSAs, options and RSUs) that will be recognized over the weighted-average period of 1.76 years.
11. Regulatory Requirements and Restricted Funds
Our health plans or risk-bearing entities are required to maintain minimum capital requirements prescribed by various regulatory authorities in each of the states in which it operates.
Risk-Based Capital Regulatory
The National Association of Insurance Commissioners has adopted rules, which, if implemented by the states, set minimum capitalization requirements for insurance companies, HMOs, and other entities bearing risk for health care coverage. The requirements take the form of risk-based capital (“RBC”) rules, which may vary from state to state. Certain states in which our health plans or risk bearing entities operate in have adopted the RBC rules. Our health plans or risk-bearing entities were in compliance with the minimum capital requirements for all periods presented.
Tangible Net Equity
Our health plan in California is required to comply with the tangible net equity (“TNE”) requirements. The required amount is the larger of: (1) $1,000; (2) 2% of the first $150,000 of annualized premium revenue, plus 1% of annualized premium revenue in excess of $150,000; or (3) 8% of the first $150,000 of annualized health care expenditures, except for those paid on a capitated or managed hospital payment basis, plus 4% of the annualized health care expenditures in excess of $150,000, except those paid on a capitated or managed hospital payment basis, plus 4% of annualized hospital expenditures paid on a managed hospital payment basis. We were in compliance with the TNE requirement for all periods presented.
We have the ability to provide additional capital to each of our health plans or risk-bearing entities when necessary to ensure that the RBC and TNE requirements are met.
107
Certain states regulate the payment of dividends, loans, or other cash transfers from our regulated subsidiaries to our non-regulated subsidiaries and parent company. Such payments may require approval by state regulatory authorities and are limited based on certain financial criteria, such as the entity’s level of statutory income and statutory capital and surplus, or the entity’s level of tangible net equity or net worth, among other measures. These regulations vary by state. Our state regulated subsidiaries had aggregate regulatory capital of approximately $65,138 and $36,302 as of December 31, 2021 and 2020, respectively, which exceeded aggregate minimum regulatory requirements of $28,152 and $20,898, respectively. The amount of undistributed dividends from our regulated subsidiaries that may be paid out to our parent without regulatory approval was $24,957 and $9,614 as of December 31, 2021 and 2020, respectively. We were in compliance with the RBC and TNE requirements as of December 31, 2021 and 2020.
Restricted Assets
Pursuant to the regulations governing our subsidiaries, we maintain certain deposits required by the government authorities in the form of cash, certificates of deposit and Treasury bills as protection in the event of insolvency. The use of funds from these investments is limited as required by regulation in the various states in which we operate, or as needed in the event of insolvency. Therefore, these deposits are reported within other assets on the consolidated balance sheets.
We hold these assets until maturity, at which time these assets will renew or are invested in a similar type of investment instrument. Given the regulatory requirements, we expect to hold these investments for long-term. As a result, we do not expect the value of these investments to decline significantly due to a sudden change in market interest rates. These investments are carried at amortized cost, which approximates fair value.
12. Leases
Our leases are primarily for our corporate office, including parking spaces, and healthcare services operating facilities and expire at various intervals up through 2025. The majority of our leases contain renewal options, some of which include options to extend the lease for up to five years per option.
The majority of our leases are comprised of fixed payments. When certain portions of the lease payments are not fixed, we consider those payments to be variable in nature. These variable lease payments include, but are not limited to, common area maintenance, parking, taxes and insurance. These variable payments are not included in the ROU asset or lease liability and are recorded within selling, general and administrative expenses in the consolidated statement of operations and are recorded based upon actual costs in the period incurred.
Certain leases also contain rent escalation clauses that require additional rental amounts in the later years of the term. Rent expense for leases with rent escalation is recognized on a straight-line basis over the minimum lease term. The lease agreements do not contain any material residual value guarantees or material restrictive covenants.
At December 31, 2021, $7,853 of operating ROU assets were recorded as right of use assets on the consolidated balance sheets. Lease liabilities of $3,706 and $6,975 were included in accounts payable and accrued expenses and long-term lease liabilities, respectively. At December 31, 2020, $9,888 of operating ROU assets were recorded as right of use assets on the consolidated balance sheets. Lease liabilities of $3,351 and $10,271 were included in accounts payable and accrued expenses and long-term lease liabilities, respectively. Total fixed operating lease costs and variable operating lease cost, excluding short-term lease and finance lease costs, were $3,466 and $365, respectively, and $3,515 and $429, respectively, for the years ended December 31, 2021 and 2020, respectively, and are included within selling, general and administrative expenses in the consolidated statement of operations. Short term and finance lease costs were immaterial. For the year-ended December 31, 2021 and 2020, cash paid for amounts included in the measurement of lease liabilities included within our operating cash flows was $3,817 and $3,310, respectively.
Lease liabilities are based on the net present value of the remaining lease payments over the remaining lease term. In determining the present value of lease payments, the Company used its incremental borrowing rate based on the information available at the lease commencement date.
The weighted average remaining lease term for operating leases is 2.5 years with a weighted average discount rate 7.5% at December 31, 2021.
The weighted average remaining lease term for finance leases is 2.8 years with a weighted average discount rate 7.5% at December 31, 2021.
In the year ended December 31, 2021, $784 and $0 of operating lease and finance lease assets, respectively were exchanged for lease liabilities related to newly commenced leases.
The following table summarizes our lease assets and liabilities as of December 31, 2021 and 2020:
108
|
|
December 31, |
|
|
December 31, |
|
||
Lease assets |
|
|
|
|
|
|
||
Operating lease assets |
|
$ |
7,446 |
|
|
$ |
9,337 |
|
Finance lease assets |
|
|
407 |
|
|
|
551 |
|
Total lease assets |
|
$ |
7,853 |
|
|
$ |
9,888 |
|
Lease liabilities |
|
|
|
|
|
|
||
Current |
|
|
|
|
|
|
||
|
|
3,559 |
|
|
|
3,213 |
|
|
|
|
147 |
|
|
|
138 |
|
|
Non-current |
|
|
|
|
|
|
||
Operating lease liabilities |
|
|
6,692 |
|
|
|
9,841 |
|
|
|
283 |
|
|
|
430 |
|
|
Total lease liabilities |
|
$ |
10,681 |
|
|
$ |
13,622 |
|
Maturities of lease liabilities under operating leases by fiscal year are as follows:
|
|
As of December 31, 2021 |
|
|
2022 |
|
$ |
4,126 |
|
2023 |
|
|
4,440 |
|
2024 |
|
|
2,524 |
|
2025 |
|
|
123 |
|
2026 |
|
|
— |
|
Thereafter |
|
|
— |
|
Total lease payments |
|
$ |
11,213 |
|
Less: Interest |
|
|
962 |
|
Present value of lease liabilities |
|
$ |
10,251 |
|
Maturities of lease liabilities under finance leases by fiscal year are as follows:
|
|
As of December 31, 2021 |
|
|
2022 |
|
$ |
173 |
|
2023 |
|
|
173 |
|
2024 |
|
|
128 |
|
2025 |
|
|
— |
|
2026 |
|
|
— |
|
Thereafter |
|
|
— |
|
Total lease payments |
|
$ |
474 |
|
Less: Interest |
|
|
44 |
|
|
$ |
430 |
|
|
We sublease space not used in our operations. For the year ended December 31, 2021 and 2020, sublease income was $229 and $274.
On January 1, 2020, we adopted ASU No. 2016-02, Leases (Topic 842) using the modified retrospective method. This ASU required leases to be classified as either operating or finance. Operating leases resulted in straight-line expense while finance leases resulted in a front-loaded expense pattern. As a result of the adoption of the new standard, we recorded an initial lease liability and right-of-use asset of $15,682 and $11,129, respectively, as of January 1, 2020. The difference between the initial lease liability and the right-of-use asset was primarily due to deferred rent.
13. Employee Benefit Plans
All full-time employees are eligible to participate in a 401(k) plan that we sponsor upon completing 90 days of services. Eligible employees are permitted to contribute up to the maximum amount allowed by law. We match 100% of contributions not exceeding 4% of the employee's compensation. We made matching contributions of $2,051, $1,592, and $1,269 during 2021, 2020, and 2019, respectively, and were included within selling general, and administrative expenses in the consolidated statement of operations.
14. Commitments and Contingencies
Legal Proceedings
We record a liability and accrue the costs for a loss when an unfavorable outcome is probable and the amount of the loss can be reasonably estimated. In some cases, no estimate of the possible loss or range of loss in excess of amounts accrued, if any, can be made because of the inherently
109
unpredictable nature of legal and regulatory proceedings. While the liability and accrued costs reflect our best estimate, the actual amounts may materially be different.
We may be involved in various litigation matters in the ordinary course of business. In the opinion of management, the ultimate resolution of legal proceedings is not expected to have a material adverse effect on the consolidated financial statements. Amounts accrued for legal proceedings were not material as of December 31, 2021 and 2020.
Standby Letter of Credit
We issued a standby letter of credit to one of our third-party payors in conjunction with commitments to perform. The standby letter of credit in the amount of $775 could be increased up to $1,163 based upon certain criteria. The standby letter of credit automatically renews on an annual basis in February and is collateralized by a savings account in the same amount. The standby letter of credit was renewed in February 2022.
Professional Liability Insurance
We maintain coverage for professional liability, errors and omissions, directors and officers, employment practices liability insurance, and worker’s compensation. The professional liability insurance policy is claims based while the other insurance policies are occurrence based. Such policies provide coverage for our employees, certain covered physicians, loss of income due to potential business interruption, and possible destruction or theft of assets. There have not been any reductions in coverage nor have there been any claims, which have exceeded such coverage(s) for the year ended December 31, 2021 and 2020.
Medical Reinsurance (Stop-Loss Insurance)
We utilize medical insurance (or stop-loss agreement) to limits excess losses on individual members. Under the terms of the stop-loss agreement, we are reimbursed for certain proportions of the cost of each member’s hospital expenses in excess of a specified deductible in a coverage period, limited to $2,000 in aggregate per member per coverage period. For California, we have until April 30, 2022, to submit claims to the reinsurance carrier with dates of service prior to October 1, 2021. The coverage period starts October 1 to September 30 of the following year. As of September 30, 2021, we renewed our expiring policy for the 2021–2022 coverage period with all existing terms and conditions remaining intact.
For North Carolina and Nevada, we have until July 31, 2022, to submit claims to the reinsurance carrier with dates of service prior to January 1, 2022. Each coverage period runs January 1 to December 31. As of December 31, 2021, we renewed our expiring policy for the 2022 coverage period with all existing terms and conditions remaining intact. Reinsurance premiums are included in medical costs in the consolidated statement of operations.
In the event that the third party with whom we have contracted is unable to meet its obligations under the stop-loss agreement, we remain 100% liable for paying such claim amounts submitted.
Item 9. Changes in and Disagreements with Accountants on Accounting and Financial Disclosure.
None.
Item 9A. Controls and Procedures.
Evaluation of Disclosure Controls and Procedures:
Under the supervision and with the participation of our management, including the Chief Executive Officer and Chief Financial Officer, we have evaluated the effectiveness of our disclosure controls and procedures (as defined in Rules 13a-15(e) and 15d-15(e) under the Securities Exchange Act of 1934, as amended (the “Exchange Act”), as of the end of the period covered by this report. Based on that evaluation, the Chief Executive Officer and Chief Financial Officer have concluded that these disclosure controls and procedures were effective at the reasonable assurance level as of December 31, 2021.
In designing and evaluating our disclosure controls and procedures, management recognizes that any controls and procedures, no matter how well designed and operated, can provide only reasonable assurance of achieving the desired control objectives and management necessarily applies its judgment in evaluating the cost-benefit relationship of possible controls and procedures.
Management’s Annual Report on Internal Control Over Financial Reporting
This Annual Report does not include a report of management's assessment regarding internal control over financial reporting or an attestation report of the Company’s registered public accounting firm due to a transition period established by rules of the SEC for newly public companies.
Further, we and our independent registered public accounting firm were not required to perform an evaluation of our internal control over financial reporting as of year ended December 31, 2021 in accordance with the provisions of the Sarbanes-Oxley Act. Accordingly, we cannot provide assurance that we have identified all, or that we will not in the future have additional, material weaknesses.
110
Changes to our Internal Controls over Financial Reporting:
There were no material changes in our internal control over financial reporting during the year ended December 31, 2021 that have materially affected, or are reasonably likely to materially affect, our internal control over financial reporting. As a result of the COVID-19 pandemic, certain employees began working remotely in March 2020. We have not identified any material changes in our internal control over financial reporting as a result of these changes to the working environment, in part because our internal control over financial reporting was designed to operate in a remote working environment. We are continually monitoring and assessing the COVID-19 situation to determine any potential impact on the design and operating effectiveness of our internal controls over financial reporting
Item 9B. Other Information.
None.
Item 9C. Disclosure Regarding Foreign Jurisdictions that Prevent Inspections.
Not applicable.
111
PART III
Item 10. Directors, Executive Officers and Corporate Governance.
The information required by this Item is hereby incorporated by reference to our definitive proxy statement for the 2022 Annual Meeting of Stockholders.
We have adopted a code of ethics and business conduct that applies to all employees, including our Chief Executive Officer (our principal executive officer) and Chief Financial Officer (our principal financial officer), and employees, as well as each member of our Board of Directors. The code of ethics and business conduct is available on our website at www.alignmenthealthcare.com under the Investor Relations section. We intend to satisfy any disclosure requirement under Item 5.05 of Form 8-K regarding an amendment to, or waiver from, a provision of the code of ethics by posting such information on our website, at the address specified above.
Item 11. Executive Compensation.
The information required by this Item is hereby incorporated by reference to our definitive proxy statement for the 2022 Annual Meeting of Stockholders.
Item 12. Security Ownership of Certain Beneficial Owners and Management and Related Stockholder Matters.
The information required by this Item is hereby incorporated by reference to our definitive proxy statement for the 2022 Annual Meeting of Stockholders.
Item 13. Certain Relationships and Related Transactions, and Director Independence.
The information required by this Item is hereby incorporated by reference to our definitive proxy statement for the 2022 Annual Meeting of Stockholders.
Item 14. Principal Accounting Fees and Services.
The information required by this Item is hereby incorporated by reference to our definitive proxy statement for the 2022 Annual Meeting of Stockholders.
112
PART IV
Item 15. Exhibits, Financial Statement Schedules.
The following documents are filed as a part of this report:
(a) (1) Financial Statements: The Financial Statements described in Part II. Item 8 and beginning on page 82 are filed as part of this Annual Report on Form 10-K.
(a) (3) Exhibits: The following exhibits are filed or furnished with or incorporated by reference this Annual Report on Form 10-K.
113
Exhibit Number |
|
Description |
3.1 |
|
|
3.2 |
|
|
4.1 |
|
|
4.2* |
|
|
10.1 |
|
|
10.2 |
|
|
10.3 |
|
|
10.4 |
|
|
10.5 |
|
|
10.6 |
|
|
10.7+ |
|
|
10.8+ |
|
|
10.9+ |
|
|
10.10+ |
|
|
10.11+ |
|
|
10.12+* |
|
|
10.13+* |
|
|
10.14+ |
|
|
10.15+ |
|
|
10.16+ |
|
|
10.17+ |
|
|
10.18+ |
|
|
10.19 |
|
|
10.20 |
|
|
21.1* |
|
|
23.1* |
|
|
31.1* |
|
|
31.2* |
|
114
32.1** |
|
|
32.2** |
|
|
101.INS* |
|
Inline XBRL Instance Document – the instance document does not appear in the Interactive Data File because XBRL tags are embedded within the Inline XBRL document. |
101.SCH* |
|
Inline XBRL Taxonomy Extension Schema Document |
101.CAL* |
|
Inline XBRL Taxonomy Extension Calculation Linkbase Document |
101.DEF* |
|
Inline XBRL Taxonomy Extension Definition Linkbase Document |
101.LAB* |
|
Inline XBRL Taxonomy Extension Label Linkbase Document |
101.PRE* |
|
Inline XBRL Taxonomy Extension Presentation Linkbase Document |
104* |
|
Cover Page Interactive Data File (embedded within the Inline XBRL document) |
* Filed herewith.
** Furnished herewith
+ Indicates management contract or compensatory plan.
Item 16. Form 10-K Summary.
None.
115
SIGNATURES
Pursuant to the requirements of Section 13 or 15(d) of the Securities Exchange Act of 1934, as amended, the Registrant has duly caused this Report to be signed on its behalf by the undersigned, thereunto duly authorized.
|
|
Alignment Healthcare, Inc. |
|
|
|
|
|
Date: March 3, 2022 |
|
By: |
/s/ John Kao |
|
|
|
John Kao |
|
|
|
President and Chief Executive Officer |
Pursuant to the requirements of the Securities Exchange Act of 1934, as amended, this Report has been signed below by the following persons on behalf of the Registrant in the capacities and on the dates indicated.
Signature |
|
Title |
|
Date |
|
|
|
|
|
/s/ John Kao |
|
President and Chief Executive Officer (Principal Executive Officer) |
|
March 3, 2022 |
John Kao |
|
|
|
|
|
|
|
|
|
/s/ Thomas Freeman |
|
Chief Financial Officer (Principal Financial Officer) |
|
March 3, 2022 |
Thomas Freeman |
|
|
|
|
|
|
|
|
|
/s/ Joseph Konowiecki |
|
Chairman of the Board |
|
March 3, 2022 |
Joseph Konowiecki |
|
|
|
|
|
|
|
|
|
/s/ Jody Bilney |
|
Director |
|
March 3, 2022 |
Jody Bilney |
|
|
|
|
|
|
|
|
|
/s/ Thomas Carella |
|
Director |
|
March 3, 2022 |
Thomas Carella |
|
|
|
|
|
|
|
|
|
/s/ David Hodgson |
|
Director |
|
March 3, 2022 |
David Hodgson |
|
|
|
|
|
|
|
|
|
/s/ Yon Jorden |
|
Director |
|
March 3, 2022 |
Yon Jorden |
|
|
|
|
|
|
|
|
|
/s/ Jacqueline Kosecoff |
|
Director |
|
March 3, 2022 |
Jacqueline Kosecoff |
|
|
|
|
|
|
|
|
|
/s/ Jeffrey Margolis |
|
Director |
|
March 3, 2022 |
Jeffrey Margolis |
|
|
|
|
|
|
|
|
|
/s/ Margaret McCarthy |
|
Director |
|
March 3, 2022 |
Margaret McCarthy |
|
|
|
|
|
|
|
|
|
/s/ Mark McClellan |
|
Director |
|
March 3, 2022 |
Mark McClellan |
|
|
|
|
|
|
|
|
|
/s/ Robbert Vorhoff |
|
Director |
|
March 3, 2022 |
Robbert Vorhoff |
|
|
|
|
|
|
|
|
|
116
Similar companies
See also UNITEDHEALTH GROUP INC - Annual report 2022 (10-K 2022-12-31) Annual report 2023 (10-Q 2023-09-30)See also Cigna Group - Annual report 2022 (10-K 2022-12-31) Annual report 2023 (10-Q 2023-09-30)
See also HUMANA INC - Annual report 2022 (10-K 2022-12-31) Annual report 2023 (10-Q 2023-09-30)
See also CENTENE CORP - Annual report 2022 (10-K 2022-12-31) Annual report 2023 (10-Q 2023-09-30)
See also MOLINA HEALTHCARE, INC. - Annual report 2022 (10-K 2022-12-31) Annual report 2023 (10-Q 2023-09-30)
