P3 Health Partners Inc. - Annual Report: 2022 (Form 10-K)
UNITED STATES
SECURITIES AND EXCHANGE COMMISSION
WASHINGTON, D.C. 20549
FORM 10-K
☒ | ANNUAL REPORT PURSUANT TO SECTION 13 OR 15(d) OF THE SECURITIES EXCHANGE ACT OF 1934 |
For the fiscal year ended December 31, 2022
or
☐ | TRANSITION REPORT PURSUANT TO SECTION 13 OR 15(d) OF THE SECURITIES EXCHANGE ACT OF 1934 |
For the transition period from to
Commission file number: 001-40033

P3 Health Partners Inc.
(Exact name of registrant as specified in its charter)
Delaware | 85-2992794 |
(State or other jurisdiction of incorporation or organization) | (I.R.S. Employer Identification No.) |
2370 Corporate Circle Suite 300 Henderson, Nevada | 89074 |
(Address of principal executive offices) | (Zip code) |
Registrant’s telephone number, including area code: (702) 910-3950
Securities registered pursuant to Section 12(b) of the Act:
Name of each exchange | ||
Title of each class | Trading Symbol(s) | on which registered |
Class A common stock, par value $0.0001 per share Warrants, each whole warrant exercisable for one | PIII PIIIW | The Nasdaq Stock Market LLC The Nasdaq Stock Market LLC |
Securities registered pursuant to Section 12(g) of the Act: None
Indicate by check mark if the registrant is a well-known seasoned issuer, as defined in Rule 405 of the Securities Act.
Yes ☐ No ☒
Indicate by check mark if the registrant is not required to file reports pursuant to Section 13 or Section 15(d) of the Act.
Yes ☐ No ☒
Indicate by check mark whether the registrant (1) has filed all reports required to be filed by Section 13 or 15(d) of the Securities Exchange Act of 1934 during the preceding 12 months (or for such shorter period that the registrant was required to file such reports), and (2) has been subject to such filing requirements for the past 90 days. Yes ☒ No ☐
Indicate by check mark whether the Registrant has submitted electronically every Interactive Data File required to be submitted pursuant to Rule 405 of Regulation S-T (§232.405 of this chapter) during the preceding 12 months (or for such shorter period that the registrant was required to submit such files). Yes ☒ No ☐
Indicate by check mark whether the registrant is a large accelerated filer, an accelerated filer, a non-accelerated filer, a smaller reporting company, or an emerging growth company. See the definitions of “large accelerated filer,” “accelerated filer,” “smaller reporting company,” and “emerging growth company” in Rule 12b-2 of the Exchange Act.
Large accelerated filer ☐ | Accelerated filer ☒ | Non-accelerated filer ☐ | Smaller reporting company ☒ | Emerging growth company ☒ |
If an emerging growth company, indicate by check mark if the registrant has elected not to use the extended transition period for complying with any new or revised financial accounting standards provided pursuant to Section 13(a) of the Exchange Act. ☐
Indicate by check mark whether the registrant has filed a report on and attestation to its management’s assessment of the effectiveness of its internal control over financial reporting under Section 404(b) of the Sarbanes-Oxley Act (15 U.S.C. 7262(b)) by the registered public accounting firm that prepared or issued its audit report. ☐
If securities are registered pursuant to Section 12(b) of the Act, indicate by check mark whether the financial statements of the registrant included in the filing reflect the correction of an error to previously issued financial statements. ☐
Indicate by check mark whether any of those error corrections are restatements that required a recovery analysis of incentive-based compensation received by any of the registrant’s executive officers during the relevant recovery period pursuant to §240.10D-1(b). ☐
Indicate by check mark whether the registrant is a shell company (as defined in Rule 12b-2 of the Act). Yes ☐ No ☒
The aggregate market value of the registrant’s voting and non-voting stock held by non-affiliates on June 30, 2022 (the last business day of the registrant’s most recently completed second fiscal quarter) based on the closing price on that date as reported by the Nasdaq Stock Market was approximately $93 million.
As of March 15, 2023, the registrant had 41,578,890 shares of Class A common stock, par value $0.0001 and 202,024,923 shares of Class V common stock, par value $0.0001 outstanding.
DOCUMENTS INCORPORATED BY REFERENCE
Portions of the registrant’s definitive proxy statement for its 2023 annual meeting of stockholders, if filed with the Securities and Exchange Commission (the “SEC”) within 120 days after December 31, 2022, are incorporated by reference into Part III of this Annual Report on Form 10-K, or such Part III information will be provided in an amendment filed on Form 10-K/A with the SEC no later than 120 days after December 31, 2022.
TABLE OF CONTENTS
CAUTIONARY STATEMENT REGARDING FORWARD-LOOKING STATEMENTS
This Annual Report on Form 10-K for the fiscal year ended December 31, 2022 (the “Form 10-K”) contains “forward-looking statements” within the meaning of the safe harbor provisions of the U.S. Private Securities Litigation Reform Act of 1995. We intend such forward-looking statements to be covered by the safe harbor provisions for forward-looking statements contained in Section 27A of the Securities Act of 1933, as amended (the “Securities Act”), and Section 21E of the Securities Exchange Act of 1934, as amended (the “Exchange Act”). All statements other than statements of historical facts contained in this Form 10-K, including statements regarding our future results of operations and financial position, business and growth strategy, prospective products, product approvals, research and development costs, future revenue, timing and likelihood of success, plans and objectives of management for future operations, our ability to continue as a going concern, future results of anticipated products and prospects, plans and objectives of management, are forward-looking statements. In some cases, you can identify forward-looking statements by terms such as “may,” “will,” “should,” “expect,” “plan,” “anticipate,” “could,” “intend,” “target,” “project,” “contemplate,” “believe,” “estimate,” “predict,” “potential,” “would” or “continue” or the negative of these terms or other similar expressions, although not all forward-looking statements contain these words.
The forward-looking statements in this Form 10-K are only predictions and are based largely on our current expectations and projections about future events and financial trends that we believe may affect our business, financial condition and results of operations. These forward-looking statements speak only as of the date of this Form 10-K and are subject to a number of known and unknown risks, uncertainties and assumptions, and other important factors that may cause our actual results, performance or achievements to be materially different from any future results, performance or achievements expressed or implied by the forward-looking statements, including those described under the sections in this Form 10-K in Part I, Item 1A. “Risk Factors” and Part II, Item 7. “Management’s Discussion and Analysis of Financial Condition and Results of Operations” and elsewhere in this Form 10-K.
Because forward-looking statements are inherently subject to risks and uncertainties, some of which cannot be predicted or quantified and some of which are beyond our control, you should not rely on these forward-looking statements as predictions of future events. The events and circumstances reflected in our forward-looking statements may not be achieved or occur and actual results could differ materially from those projected in the forward-looking statements. Moreover, we operate in an evolving environment. New risk factors and uncertainties may emerge from time to time, and it is not possible for management to predict all risk factors and uncertainties. Except as required by applicable law, we do not plan to publicly update or revise any forward-looking statements contained herein, whether as a result of any new information, future events, changed circumstances or otherwise.
You should read this Form 10-K and the documents that we reference in this Form 10-K and have filed as exhibits hereto completely and with the understanding that our actual future results, performance and achievements may be materially different from what we expect. We qualify all of our forward-looking statements by these cautionary statements.
Unless the context otherwise requires, “we,” “us,” “our,” “P3” and the “Company” refer to P3 Health Partners Inc. and its subsidiaries. “Foresight” refers to the Company prior to the Closing (defined below), and “P3 LLC” refers to (i) with respect to periods prior to the consummation of the Business Combinations (defined below), FAC Merger Sub LLC, a Delaware limited liability company and wholly owned subsidiary of Foresight (“Merger Sub”), and (ii) with respect to periods after the consummation of the Business Combinations, the surviving entity of the P3 Merger (defined below), which was renamed P3 Health Group, LLC.
1
SUMMARY RISK FACTORS
Our business is subject to numerous risks and uncertainties, including those described in Part I, Item 1A. “Risk Factors” in this Form 10-K. You should carefully consider these risks and uncertainties when investing in our common stock. The principal risks and uncertainties affecting our business include the following:
| ● | Our management has performed an analysis of our ability to preserve an adequate level of liquidity for a period extending 12 months from the date of this filing and has identified substantial doubt about our ability to continue as a going concern. |
| ● | We may need to raise additional capital to fund our existing operations or develop and commercialize new services or expand our operations. |
| ● | We have a history of net losses. We expect to continue to incur losses for the foreseeable future and may never achieve or maintain profitability. |
| ● | We may not be able to maintain compliance with our debt covenants in the future, or obtain required waivers from our lenders, which could result in an event of default. |
| ● | Our relatively limited operating history makes it difficult to evaluate our future prospects and the risks and challenges we may encounter. |
| ● | Goodwill and other intangible assets represent a substantial component of our total assets. If future operating performance were to fall below current projections of if there are material changes to management’s assumptions, we could be required to recognize non-cash charges to operating earnings for goodwill and/or other intangible asset impairment, which could be significant. |
| ● | The spread of COVID-19 or potential new variants of COVID-19 may adversely impact our operations and as a result, may materially and adversely affect our business and financial results. |
| ● | We rely on our management team and key employees, and our business, financial condition, cash flows and results of operations could be harmed if we are unable to retain qualified personnel. |
| ● | Our growth depends in part on our ability to identify and develop successful new geographies, physician partners, payors and patients. If we are not able to successfully manage our growth or execute upon our growth strategies, there may be material adverse effect on our business, financial condition, cash flows and results of operations. |
| ● | If growth in the number of patients and physician partners on our platform decreases, or the number of services that we are able to provide to physician partners and members decreases, due to legal, economic or business developments, our business, financial condition and results of operations will be harmed. |
| ● | We primarily depend on reimbursement by third-party payors, as well as payments by individuals, which could lead to delays and uncertainties in the timing and process of reimbursement, including any changes or reductions in Medicare reimbursement rates or rules. |
| ● | The termination or non-renewal of the MA contracts held by the health plans with which we contract, or the termination or nonrenewal of our contracts with those plans, could have a material adverse effect on our revenue and our operations. |
| ● | We are dependent on our affiliated professional entities, physician partners and other providers to effectively manage the quality and cost of care and perform obligations under payor contracts. |
| ● | Reductions in the quality ratings of the health plans we serve could have a material adverse effect on our business, results of operations, financial condition and cash flows. |
| ● | Developments affecting spending by the healthcare industry could adversely affect our business. |
2
| ● | We depend on our information technology systems, and any failure of these systems could harm our business. |
| ● | Security breaches, loss of data and other disruptions could compromise sensitive information related to our business or prevent us from accessing critical information and expose us to liability, which could adversely affect our business and our reputation. |
| ● | If our or our vendors’ security measures fail or are breached and unauthorized access to a client’s data or information systems is obtained, our services may be perceived as insecure, we may incur significant liabilities, our reputation may be harmed, and we could lose sales, clients and members. |
| ● | We conduct business in a heavily regulated industry and if we fail to adhere to all of the complex government laws and regulations that apply to our business, we could incur fines or penalties or be required to make changes to our operations or experience adverse publicity, any or all of which could have a material adverse effect on our business, results of operations, financial condition, cash flows, and reputation. |
| ● | If our arrangements with our affiliated professional entities and other physician partners are found to constitute the improper rendering of medical services or fee splitting under applicable state laws, our business, financial condition and our ability to operate in those states could be adversely impacted. |
| ● | We face inspections, reviews, audits and investigations under federal and state government programs and contracts. These audits could have adverse findings that may negatively affect our business, including our results of operations, liquidity, financial condition and reputation. |
| ● | The impact on us of recent healthcare legislation and other changes in the healthcare industry and in healthcare spending is currently unknown, but may adversely affect our business, financial condition and results of operations. |
| ● | Our only significant asset is the ownership of a minority of the economic interest in P3 LLC, and such ownership may not be sufficient to generate the funds necessary to meet our financial obligations or to pay any dividends on our Class A common stock, par value $0.0001 per share (the “Class A common stock”). |
| ● | We will be required to make payments under the Tax Receivable Agreement, dated as of December 3, 2021, by and among P3 LLC and the members of P3 LLC from time to time party thereto (the “Tax Receivable Agreement”) for certain tax benefits we may claim, and the amounts of such payments could be significant. |
| ● | Certain of the former owners of P3 Health Group Holdings, LLC (the “P3 Equityholders”) have substantial control over us, and their interests, along with the interests of other P3 Equityholders, in our business may conflict with yours. |
| ● | Foresight Sponsor Group, LLC (the “Sponsor”), Chicago Pacific Founders and other Exempt Persons are not limited in their ability to compete with the Company, and the corporate opportunity provisions in our amended and restated certificate of incorporation could enable such persons to benefit from corporate opportunities that might otherwise be available to the Company, which presents potential conflicts of interest. |
| ● | We have identified material weaknesses in our internal control over financial reporting. If we fail to establish and maintain effective internal controls in accordance with Section 404 of the Sarbanes-Oxley Act, we may not be able to accurately report our financial results or file our periodic reports in a timely manner, which may cause adverse effects on our business and may cause investors to lose confidence in our reported financial information and may lead to a decline in the price of our Class A common stock. |
| ● | Failure to comply with the continued listing standards of Nasdaq could result in significant material adverse consequences, including a limited availability of market quotations, liquidity for our securities and a decreased ability to issue additional securities or obtain additional financing in the future. |
| ● | Other risks and uncertainties described in this Form 10-K, including those under Part I, Item 1A. “Risk Factors.” |
3
PART I
Item 1. Business.
Background
We were incorporated in Delaware as Foresight Acquisition Corp. (“Foresight”) on August 20, 2020. On December 3, 2021 (the “Closing Date”), we completed the Business Combinations (defined and discussed more fully below) with P3 Health Group Holdings, LLC, a Delaware limited liability company (“P3 Health Group Holdings”) and we changed our name to P3 Health Partners Inc. Following the Business Combinations, we are organized in an “Up-C” structure, in which P3 Health Partners Inc. is the sole manager of P3 Health Group, LLC and directly owns approximately 17.1% of P3 Health Group, LLC as of December 31, 2022. Substantially all of the Company’s assets are held and operations are conducted by P3 LLC and its subsidiaries, and the Company’s only assets are equity interests in P3 LLC.
Business Combinations
The Business Combinations were effected pursuant to (1) an agreement and plan of merger, dated as of May 25, 2021 (as amended, the “Merger Agreement”), by and among Foresight, P3 Health Group Holdings and Merger Sub, and (2) the transaction and combination agreement, dated as of May 25, 2021 (as amended, the “Transaction and Combination Agreement”), by and among Foresight, FAC-A Merger Sub Corp., a Delaware corporation and a wholly owned subsidiary of Foresight, FAC-B Merger Sub Corp., a Delaware corporation and a wholly owned subsidiary of Foresight (together with FAC-A Merger Sub Corp., the “Merger Corps”), CPF P3 Blocker-A, LLC, a Delaware limited liability company, CPF P3 Blocker-B, LLC, a Delaware limited liability company (together with CPF P3 Blocker-A, LLC, the “Blockers”), CPF P3 Splitter, LLC, a Delaware limited liability company, Chicago Pacific Founders Fund-A, L.P., a Delaware limited partnership, and Chicago Pacific Founders Fund-B, L.P., a Delaware limited partnership (together with Chicago Pacific Founders Fund-A, L.P., the “Blocker Sellers”), pursuant to which, among other things, P3 Health Group Holdings merged with and into Merger Sub (the “P3 Merger”), with Merger Sub as the surviving company, which was renamed P3 LLC, and the Merger Corps merged with and into the Blockers, with the Blockers as the surviving entities and wholly owned subsidiaries of Foresight (collectively, the “Business Combinations”).
The Business Combinations resulted in the presentation of the Company’s consolidated financial statements on different bases for the year ended December 31, 2022, the period December 3, 2021 through December 31, 2021 (the “Successor Period”), and the period January 1, 2021 through December 2, 2021 (the “Predecessor Period”). The Company has not provided pro forma statements of operations and cash flows for the years ended December 31, 2022 and 2021. Accordingly, references to certain financial results in 2022 and 2021 may not be comparable.
Overview
P3 is a patient-centered and physician-led population health management company. We strive to offer superior care to those patients that we serve. Founded and led by physicians, P3 is a team of doctors, clinicians and healthcare professionals with a shared passion for delivering value-based care (“VBC”). We believe our leadership team’s more than 20 years of experience in VBC and population health management, combined with our strong payor relationships, large community-based physician networks and custom technology platform uniquely position us to empower physicians, align incentives for healthcare providers and payors and improve the clinical outcomes for the communities we serve.
As fellow healthcare professionals, we understand the challenges physicians face when providing VBC. We have leveraged that expertise to build our “P3 Care Model.” The key attributes that differentiate P3 include: 1) patient centricity, 2) physician leadership, and 3) our delegated/integrated care model. Tactically, we typically leverage the community’s existing healthcare infrastructure to build a strong network of local physicians. We primarily contract with local physicians to enter the P3 network using an affiliate model, rather than building and staffing our own clinics or acquiring individual practices. By doing so, we preserve the existing patient-physician relationship, allow physicians to maintain their independence and have a built-in patient panel on Day 1. We then align physician incentives and provide our team tools and technology to support our physician partners in a VBC system and care for the patients we have the honor and privilege to serve together. These affiliated physicians provided care to approximately 90% of our primary care physicians as of December 31, 2022. We augment these affiliate partnerships with employed Primary Care Physicians (“PCPs,”), P3 operated clinics, and wellness centers. Furthermore, unlike our peers, we offer a broad delegated care model
4
in which we take on the responsibility to reshape the local healthcare market to provide high quality care for patients throughout the care continuum.
We operate in the $829 billion Medicare market, which covers approximately 65 million eligible lives as of 2021. This segment is supported by numerous tailwinds. Approximately 60% of Americans suffer from a chronic disease with 40% suffering from two or more. Additionally, over 10,000 individuals age into Medicare each day, with 48% choosing Medicare Advantage plans. Our core focus is the Medicare Advantage (“MA”) market, specifically counties where there are over 10,000 MA eligible lives. MA spending is expected to grow an average of 7.2% annually and MA plan penetration of the Medicare beneficiary population is projected to increase from 48% of the overall Medicare market in 2022 to 61% of the overall Medicare market by 2031.
In MA, the Centers for Medicare & Medicaid Services (“CMS”) pays health plans a monthly sum per member to manage all health expenses of a participating member. Our platform focuses exclusively on Medicare Advantage and manages the needs of our members through subscription-like per-member-per-month (“PMPM”) arrangements with health plans or payors. From there, the economics of our care model are further impacted by our ability to drive total cost of care savings and bend the cost curve. Our model allows us to “do well” while also “doing good.”
The U.S. healthcare system is ripe for change and disruption, and we believe that the P3 Care Model is distinctly situated to address several pain points, including:
· | Unsustainable and rising healthcare costs. The United States spent $4.3 trillion, representing 18.3% of GDP, on healthcare in 2021. National health expenditures are projected to grow 5.1% per year from 2021 to 2030, according to CMS. While representing only 17% of the United States population, the 65 and older age group accounted for 21% of all healthcare spending in 2021, with an average spend of approximately $13,000 per person. This segment is growing faster than the rest of the population and is projected to reach 22% of the United States population by 2050. Healthcare expenditures are particularly concentrated in this age group in large part due to the high rate of chronic conditions. Rising healthcare costs disproportionally impact low- and middle-income seniors, who often embrace Medicare Advantage plans. This is our area of focus given we believe we can have the greatest clinical and financial impact on this population. Improved care management of seniors is critical to reducing the rapid growth in U.S. healthcare spending. |
· | Inadequate access to primary care and PCP shortages. The current fee-for-service (“FFS”) reimbursement model leads to relatively lower pay for PCPs as well as fewer quality touchpoints with patients. We believe that factors like these directly contribute to fewer physicians considering, or staying, in the field of primary care. |
· | Sub-optimal quality of care and sub-optimal clinical outcomes. |
· | PCP burnout and dissatisfaction. The traditional FFS model values quantity over quality, which has been shown to lead to physician burnout and jeopardizes the long-term sustainability of the independent primary care business model. According to a 2022 Physicians Foundation report, six in 10 physicians show signs of burnout, compared to four in 10 in 2018. In addition, as average reimbursement rates decline in an FFS model, physicians would need to continually increase the number of patients seen to sustain their practice. |
· | Difficulty in maintaining PCP independence. Small physician practices deliver the majority of care in the U.S.—with 53.7% of physicians working in practices with 10 or fewer physicians, per a 2021 American Medical Association report. That report also found that 2020 was the first year in which a minority (49.1%) of PCPs worked in a practice that was wholly owned by physicians (e.g., private practice). This represented a decrease of approximately 5% from 2018 (54.0%). In our experience, physicians who have chosen to work at smaller practices throughout their careers tend to do so because they value their independence. Given the increasingly significant financial and administrative burdens, these physicians are generally unable to maintain independence while effectively transitioning to a VBC model. We believe that allowing them to maintain their independence increases their engagement with population health management practices, which is key to transforming the healthcare system. |
· | Limited collaboration between PCPs and payors. Over the years, we have seen that payors recognize the importance of PCPs in directing and managing total cost of care. Payors have attempted to increase their proximity to primary care physicians through acquisitions and investments in care delivery services and technologies. However, a payor’s ability to |
5
impact physician workflows continues to be structurally limited by the multi-payor nature of most physician practices. This makes it challenging for any single payor to achieve the level of integration we believe is needed to improve clinical engagement and effectively manage healthcare costs. We believe this creates significant opportunity for a platform to partner directly and create alignment between payors and physicians.
We overcome these hurdles with a differentiated model that we believe is an attractive option for patients, physicians and payors. P3 honors the existing social and moral contract between patients and their PCPs, partnering with local physicians using an affiliate model. We risk-stratify our patients to help our physician partners prioritize care for those who need it the most. We also provide care teams to serve as an extension of the physician’s practice. These teams provide wraparound services to our patients and collaborate with the patients’ caregivers to ensure patients have the tools to successfully navigate their healthcare journey across the care continuum. We have made significant investments in technology to customize patient care management plans. Taken as a whole, our P3 Care Model helps facilitate enhanced clinical outcomes for our key stakeholders, resulting in a 98% physician retention rate from 2018 through December 31, 2022, 96% patient satisfaction rate, a hospitalization rate 34% lower than the MA FFS benchmark, and an emergency department visit rate 50% lower than the MA FFS benchmark.
We are led by one of the most experienced management teams in population health. Our executive team has a track record of more than 20 years in the healthcare industry. These years of experience have fostered strong relationships in the managed care, physician and payor segments. This is paired with a deep understanding of physicians, patients, technology, payments and branding. Lastly, the core of our care model is based on their collective years of experience in medical cost management. We believe these critical facets position our team to successfully navigate and enable the shift to patient-centric, physician-led, VBC.
We Deliver VBC to the Fastest Growing Market in Healthcare
A need for a new payment structure and an aging U.S. population
Historically, healthcare in the U.S. has been focused on reacting to acute events, which resulted in the development of the FFS payment model. The FFS model unintentionally incentivizes the volume of patients and services performed rather than the quality of services and care—resulting in a deprioritization of preventative services and overall health of the patient. Beyond sub-optimal clinical outcomes, FFS results in significant healthcare spend. As 10,000 seniors age into Medicare each day and prevalence of chronic conditions increases, the need for lower healthcare spend leads the push towards VBC and additional offerings such as Medicare Advantage.
VBC and Medicare Advantage
Medicare Advantage serves as an alternative to traditional Medicare. Medicare Advantage is an integrated plan that includes both Part A and Part B coverage. Most Medicare Advantage plans also offer Part D, vision, hearing, dental and other benefits. Typically, the out-of-pocket costs are lower for Medicare Advantage plans than traditional Medicare, but patients are limited to seeing physicians within the plan’s network and some coverage of certain specialty services may require PCPs’ referrals and plan authorizations.
Medicare Advantage has been well received since it was introduced, with penetration among Medicare beneficiaries increasing from 13% in 2004 to 48% in 2022 and is projected to increase to 61% by 2031. This trend reflects the understanding that Medicare Advantage plans are financially and clinically valuable to Medicare eligible patients.
Our Market Opportunity
We believe there is significant white space opportunity. As of December 31, 2022, we have contracted with 2,800 primary care physicians, an increase of 33% from 2,100 at December 31, 2021. This represents less than 1% of the total number of PCPs in the U.S. of approximately 502,000. The industry is primed for a platform like ours, which allows physicians to remain independent while accessing financial resources and infrastructure to support a VBC model.
We believe our total addressable market is represented by the approximately 65 million Americans (approximately 17% of the total population) who were enrolled in either traditional Medicare or Medicare Advantage nationally in 2021, which represented $829 billion of annual spend. Within this, we believe our core addressable market to be the Medicare Advantage market, specifically
6
within moderate-to-highly populated Medicare Advantage eligible dense counties, which we define as having greater than 10,000 Medicare eligible lives. By multiplying these approximately 28 million Medicare Advantage members by an average $1,000 per member per month spend, we estimate this represents a core addressable market size of approximately $300 billion.
The P3 Care Model
Patient-Centric
Patient wellness, not sickness. The VBC model rewards superior clinical outcomes and value delivered to the patient. With this in mind, we built our model to consider the whole patient rather than individual illnesses as they arise. We work with our physician partners to develop a holistic view of a patient’s health over time to understand the most effective methods to empower their patients to actively participate in and better manage their health (e.g., medication adherence, complete understanding of potential impediments to receiving care).
Robust care teams. We staff dedicated care managers and care navigators to help ensure end-to-end patient care across the full continuum. Care navigators are responsible for day-to-day patient care (e.g., scheduling appointments, assisting with check-ins, etc.). Care managers, on the other hand, tend to have more medical responsibilities (e.g., reviewing patient charts, coordinating care with PCPs, ensuring appropriate documentation, etc.) and serve as a communication point across care teams. Together, they complement our network of physicians and enable the highest quality of care for our patients—ensuring they are being seen at the right time by the appropriate physician and all corresponding documentation and communication has been streamlined.
Personalized care. Using our proprietary technology platform for integrated data reporting, physicians can stratify their patient panels based on risk. Identifying patients who are high risk (or rising risk) helps prioritize those patients who may need to be seen more often or require additional resources to improve their health. Additionally, our tailored tech suite provides our physician partners with detailed insights to understand what is driving individual patient clinical outcomes and medical costs. Leveraging this data, we then collaborate with physicians to build individualized, longitudinal care plans, catered to the needs of individual patients.
Physician-Led
Collaborative and supportive partnerships. As former physicians, we have a deep understanding of the way in which physicians are trained. In our experience, most physicians not only understand the value of a VBC model, but also want to provide their patients with the highest quality care. However, the way in which most physicians today were trained caters to an FFS model. To support the VBC model, we provide training to physicians on best clinical practices based on nationally recognized care guidelines. As a result, we have seen physicians deliver cost saving, quality healthcare. Unlike some of our peers, we typically enter markets with our affiliate physician model and contract directly with physician groups or independent physicians to enter the P3 network rather than primarily building and staffing our own clinics or acquiring physician practices. By doing so, we preserve the existing patient-physician relationship and create a built-in patient panel on Day 1. Affiliate physicians retain their independence, while gaining access to P3’s teams, tools and technologies that are key to success in a VBC model. P3’s care teams become an extension of each physician’s office and support our collective patients to navigate the health care system, collaborate with caregivers, and enable a successful health care journey. All P3 affiliated physicians must pass an annual credentialing process and maintain compliance with all regulatory standards.
Aligned incentives. Our model properly aligns physicians’ incentives with clinical outcomes, ensuring patients receive the optimal care they deserve. To do this, we offer several types of incentive-based payments to our affiliated physicians. First, as physicians join our network, we continue to pay them on an FFS basis per visit, or structure a contract to offer a monthly, fixed, capitated payment for each patient paneled to their practice. Additionally, we provide quality incentive payments to our physician partners as they close quality gaps in care, enable patient access and improve documentation. Finally, as improved clinical outcomes result in reduced medical costs, we share the savings between P3 and our physician partners. These contracts were built with the physician in mind, which is reflected in our results—a 98% physician retention rate from 2018 through December 31, 2022. Aligning physician incentives with performance on growth, quality, patient disease documentation, and medical expense creates better economics within their practices.
7
Broad Delegated Care Model
Reshaping local healthcare. Our more than 20 years of experience in the population health management space has allowed us to build the capabilities to better control and manage the delivery of services across the full care continuum. Our team has the ability to take on additional services from our payor partners, including networking, credentialing, utilization management and claims processing. In order to take on these functions, our teams must pass regular delegation audits by CMS as well as our payor partners. By assuming responsibility for the patient’s entire care experience, we can tailor care provision and coordination to their individual needs. We take on this added burden, as it allows us to reshape the local healthcare market and accelerate the shift from a FFS model to a VBC model.
Delegated services. Through delegation, we can build local networks of physicians and specialists to meet the needs of our patients. By creating a captive network, we ensure that our network of physicians and specialists are properly educated on best clinical practices based on national recognized care guidelines. Furthermore, delegation allows us to align incentives across the full continuum, not just the PCP office. With additional tools like utilization management, we ensure that quality care is delivered in the appropriate care setting. To help with care delivery effectiveness, we perform concurrent reviews to manage acute and post-acute hospitals for length of stay and appropriateness. Finally, by taking on responsibility for processing and paying claims, we are able to ensure the appropriate payment for the appropriate care. Ownership over claims creates value and helps to accelerate the reduction of unnecessary medical costs.
P3 Technology/Health Hub
The backbone of our P3 Care Model is our proprietary technology platform—P3 Technology/Health Hub—which enables physicians, care teams, patients and their family members to engage in the care journey. Our platform was purposefully built as a data and technology-enabled care ecosystem that drives preventive rather than reactive care.
P3 Technology/Health Hub integrates clinical and claims data from more than 250 disparate data points each month from payors, outpatient and inpatient facilities and other ancillary care settings. By using P3 Technology/Health Hub at the time of patient onboarding, we are able to assign patient risk levels using our proprietary risk stratification tool that leverages multiple parameters to prioritize patients who require additional resources. We continually collect data on patients from multiple sources so our care teams can proactively and dynamically deliver individualized care based on changes to a patient’s health profile. For example, within approximately 12 hours of a hospitalization—even out of state—our physician partners are notified and alerted to the patient’s clinical status. Our care managers also monitor patient care and provide physicians with insights to enable additional care across settings and locations. These factors create a positive feedback loop, whereby our technology accelerates clinical outcomes, improving strong performance, and further growing our business.
The P3 Technology/Health Hub is built on multiple products, including:
Provider Portal. This physician-facing product enables our physician partners to understand, care for and monitor their patients. Physicians can access a risk stratified patient list based on historical diagnoses, suspect diagnoses, ER visits, chronic comorbidities and socio-economic factors, among others. By using this, P3 is able to present physicians with care opportunities, Healthcare Effectiveness Data and Information Set (“HEDIS®”) gaps in care and drug substitution opportunities, which directly translate into stronger cost management. Analyzing the risk-stratified patient-level data helps physicians and office staff strategize patient scheduling to optimize their resources and work hours to meet the healthcare needs of the patients that need the most care. Provider Portal also generates additional possible conditions that the physicians can screen for during patient visits. This exercise gives physicians a longitudinal view of patients’ health and any potential medical conditions they may have developed since their last annual wellness visit. This represents an important opportunity for physicians to address the conditions which otherwise may have been missed during initial health reviews of the patient.
Provider Portal is also used by our internal certified coders to review and reconcile claims data with electronic medical record and charts data. This provides P3 an opportunity to capture dropped or missed codes documented in the patient’s medical record that were not properly converted during the initial submission of claims by our physician partner offices. This practice also ensures that the diagnosis data that is submitted to health plans is validated with appropriate supporting documentation for seamless acceptance by CMS for year-over-year risk calculation for our patients.
8
P3 Care Connect. P3 Care Connect is a comprehensive management tool used by P3 care management, utilization management and concurrent review teams. P3 Care Connect enables P3 care managers to provide concierge and individualized care for specific, high-risk and special needs populations. This capability allows our platform and its constituents to deliver highly impactful clinical programs aimed to reduce cost and improve clinical outcomes while optimizing efficiency. Care orchestration through a combination of program management, cohort building, care plan and assessment builders help our care managers build more intelligent care plans. P3 Care Connect allows our care and medical management teams to process prior authorizations, track P3 patient referrals within our network throughout the care continuum and manage a concurrent review for inpatient services through an automated platform that improves efficiency and auditability of existing business workflows. This tool also enables a streamlined communication between P3 and primary care physicians, specialists and other ancillary care physicians who are involved in the care of our patients.
Analytic Management Tools. Analytic Management Tools is a business intelligence platform that converts data into visualizations and real-time metrics to empower decision making at every level across the organization. It helps our administrative teams deliver a data driven approach for a better, more engaged physician experience and act as a support system to their practices.
This tool combines data management with data analysis to evaluate and transform complex data sets into meaningful, actionable information used to support effective strategic, tactical and operational insights. It also provides comprehensive information that drives performance to improve clinical outcomes and quality of care and creates physician profiles and cost analysis to improve healthcare management. With an embedded Risk Adjustment engine, it allows the organization to determine the burden of illness for our patients while providing stratification clinical data to physicians.
Our Value Proposition
We believe that our P3 Care Model is effective, differentiated and represents a ‘win’ for all key stakeholders.
Patients
Our P3 Care Model of partnering with local physicians allows patients to maintain their relationship with their existing physicians. We believe this is key to delivering stronger clinical outcomes and support for our patients, as evidenced by our patient satisfaction rate of 96%. Our model deploys care teams for each individual patient to assist in the continuity and coordination of care. This support allows for seamless interactions across multiple physicians and various care settings. Connectivity minimizes unnecessary progression of disease or downstream care, which is evident in our results.
Physicians
We believe our model supports and empowers physicians, care teams, and practices in their transition from a traditional FFS model to a VBC model. Importantly, we enable physicians to implement VBC protocols while maintaining their independence. Additionally, our P3 Care Model leverages an innovative technology suite that provides physicians with the tools to drive better clinical outcomes. Enabling physicians to own much of this process also allows for improved personal satisfaction on their journey to VBC, resulting in our 98% physician retention rate from 2018 through December 31, 2022 on our network of approximately 2,800 physicians at December 31, 2022.
Payors
Our model is differentiated in our ability to also partner directly with payors. We have a proven ability to manage medical costs and improve clinical outcomes of our lives under management on behalf of our payor partners. This is evidenced by the receipt of inbound partnership requests from payors to improve growth, quality and profitability in their markets. We believe there is a significant and growing demand from payors as they capitate risk and transition to VBC.
9
Competitive Differentiation
Broad delegated care model
Under our at-risk model, we are financially responsible for the medical costs associated with our attributed patients across the care continuum. Our broad delegated care model enables us to better manage and control critical aspects of care beyond the PCP office. By taking on additional, delegated services from our payor partners, including networking, credentialing, utilization management and claims processing, we can better control care delivery, align incentives across the care continuum, and ensure that quality care is delivered and paid for in the appropriate care setting.
Rapidly scalable, capital efficient model
We have demonstrated the rapid scalability of our model with organic revenue growth of 99% from 2018 to 2022. This is in part due to the capital efficiency of our affiliate model and in part due to our ability to grow through multiple channels. Because we primarily partner with physicians and physician groups or payors, we do not need to build brick and mortar clinics or acquire practices to enter a new market; therefore, we require less upfront capital to enter a market and can take the time to establish a market presence and build patient recognition and familiarity as well as other relationships before investing significant funds. While many of our competitors employ the buy / build or joint-venture partnership model, our approach has a minimal “ramp-up” period and thus a faster expected near-term path to profitability. Furthermore, our ability to effectively leverage existing physician bases across the U.S. accelerates our speed to scale.
Highly experienced management team
Our management team has extensive experience in population health management, the MA space, and leading the transition to VBC throughout the United States.
Our executive team has worked hard to build cultural alignment around our vision to transform healthcare. This vision and values permeate throughout our organization and are embraced by our employees and partners. Furthermore, our executive team has been thoughtful and strategic about fostering a culture of mentorship to pass on their extensive industry knowledge to future P3 leaders.
Virtuous growth cycle
Our model incentivizes all constituencies across the care spectrum to work together by aligning incentives directly based on growth, care quality, patient disease documentation, and medical expense improvements. Our model creates better physician economics within their practices. When all constituencies benefit, we all capture the meaningful value generated by the P3 Care Model by improving clinical outcomes and decreasing the cost of care. Our ability to drive savings allows us to continuously innovate, support our physician partners and engage patients on the P3 platform.
Our Growth Strategy
We intend to utilize our competitive strengths and capitalize on favorable industry trends to increase our footprint within our current markets and across new states and counties to ultimately increase the number of physicians and patients we serve.
Additional membership through current relationships. Recent data suggests that the number of Medicare-eligible patients and Medicare Advantage penetration rates will continue to increase in the upcoming years. We believe that this trend will translate into increased coverage by our current payor partners in our existing markets. As these new patients enroll in Medicare Advantage through our payors, they become attributed to our platform with little incremental cost to us.
Furthermore, we believe our physician partners will also increase their patient coverage as the number of available Medicare Advantage lives increases. We expect to be favorably positioned to benefit from this source of growth, bolstered by the sticky physician-patient relationship and our platform’s ability to assist our physician partners in more effectively managing healthcare quality, patient experience and cost.
10
Expansion in current markets. Based on our ability to provide a compelling value proposition for physicians looking to shift to value-based care while remaining independent, we believe there is significant opportunity to grow lives in our current markets in Arizona, California, Florida, Nevada, and Oregon. Additionally, we have the opportunity to expand our existing membership base through our payor partners’ presence in our current markets.
Expansion into adjacent markets. Once we establish a presence in a geography, we are then able to leverage our regional infrastructure and our relationships with payors as we expand into adjacent geographies. We are more easily able to deploy this ‘land and expand’ strategy once we have established the P3 brand in a particular market.
Expansion into new markets. We are constantly evaluating our pipeline of opportunities to continue growing our membership. Based on our analysis and experience to date, we have identified a list of target markets that we believe are ideal candidates for the P3 Care Model, whether across physicians or payors. We can facilitate this growth through new payor contracts, new network partnerships via joint ventures or expanding into a new market as part of an existing payor contract. We target entering three to five new markets each year based on this proven strategy.
Execute on accretive acquisitions. While our growth to date has been organic, we believe there are additional robust opportunities to acquire additional lives across both physicians and payors.
Competition
The healthcare industry is highly competitive and fragmented. Our primary competition remains the status quo, FFS environment that much of the healthcare system operates in today. We currently face competition in every aspect of our business, including in offering a favorable reimbursement structure for existing physician partners and attracting payors and physician partners who are not contracted with us, from a range of large- and medium-sized local and national companies that provide care under a variety of models that could attract patients, providers and payors. Our primary competitors in the population health management space include Oak Street Health, Cano Health and agilon health, in addition to numerous local provider networks, hospitals and health systems. Moreover, large, well-financed payors have in some cases developed their own managed care services tools and may provide these services to their physicians and patients at discounted prices or may seek to expand their relationships with additional competing physicians or physician networks. Other organizations may also seek to apply specialized services or programs, including providing data analytics or disease-based programs, designed to enable physicians or payors to operate successfully under VBC arrangements. Our competitors typically vary by geography, and we may also encounter competition in the future from other new entrants. Our growth strategy and our business could be adversely affected if we are not able to continue to access existing geographies, successfully expand into new geographies or maintain or establish new relationships with payors and physician partners.
See “Risk Factors—Risks Related to Our Business and Industry—We operate in a competitive industry, and if we are not able to compete effectively, our business, financial condition and results of operations will be harmed.”
The principal competitive factors in our business include the nature and caliber of relationships with physicians; patient healthcare quality, outcomes and cost; the strength of relationships with payors; the quality of the physician experience; local geography leadership position; and the strength of the underlying economic model. We believe our platform, partnership and network model enables us to compete favorably.
Intellectual Property
We rely on a combination of trademark laws in the U.S. as well as confidentiality procedures and contractual provisions to protect our trade secrets, including proprietary technology, databases and our brand.
We have a federal trademark registration application for “P3 Health Partners” in the U.S. We also have filed other applications to protect names and marks that are meaningful to our business in the U.S. across various states and local jurisdictions, including for the use of the local brand created within each of our geographies, and will pursue additional trademark registrations to the extent we believe it would be beneficial and cost-effective.
We are the controller of a variety of registered domain names that include “p3hp” and similar variations.
11
We have developed proprietary technology and processes that support our operational programs and clinical insights, including our P3 Technology/Health Hub, which is a proprietary system that aids in the aggregation and analysis of third-party data we collect. Our internally developed technology is continuously refined to support the needs of our platform and partners. Although we do not currently hold a patent for P3 Technology/Health Hub, we have filed provisional patent applications relating to the P3 Technology/Health Hub, and we continue to regularly assess the most appropriate methods of protecting our intellectual property and may decide to pursue available protections in the future.
We maintain our intellectual property and confidential business information in a number of ways. For instance, we have a policy of requiring all employees and consultants to execute confidentiality agreements upon the commencement of an employment or consulting relationship with us. Our employee agreements also require relevant employees to assign to us all rights to any inventions made or conceived during their employment with us in accordance with applicable law. In addition, we have a policy of requiring individuals and entities with which we discuss potential business relationships to sign non-disclosure agreements. Lastly, our contracts with physicians include confidentiality and non-disclosure provisions.
We may be unable to obtain, maintain and enforce our intellectual property rights, and assertions by third parties that we violate their intellectual property rights could have a material adverse effect on our business, financial condition and results of operations.
Human Capital
As of December 31, 2022, we had approximately 600 employees. We consider our relationship with our employees to be good. None of our employees are represented by a labor union or party to a collective bargaining agreement.
Our human capital resources objectives include sourcing, recruiting, developing, retaining, rewarding, recognizing and integrating our existing and prospective employees. We recognize that attracting, motivating and retaining diverse, skilled and purpose-driven talent at all levels is vital to continuing our success. By improving employee retention and engagement, we also improve our ability to protect the long-term interests of our stakeholders and stockholders. We invest in our employees through high-quality benefits, various health and wellness initiatives, and social events that bring our employees together to support the communities in which we live and work. We offer competitive compensation packages, ensuring fairness in internal compensation practices.
People join P3 because of our mission: to ensure providers and their patients get the healthcare they deserve. Together with our employees and physician partners, we have defined our core values as:
| ● | People: Our attitude is respecting and valuing everyone. Our community is strong and safe. We are “family” and we take care of each other with the same intensity as we take care of our patients. |
| ● | Passion: Our heart is our patients. Our soul is our clinicians. Our strength is our people and culture. |
| ● | Purpose: Our core is fixing health care. Our mindset is disciplined purposeful growth. |
Our human capital efforts are supported by our dedicated human resources team. This team supports the business in identifying and recruiting top talent, supporting the onboarding of new hires through an employee orientation program, providing a structured approach to performance management that allows leaders and employees to collaborate to set organizational goals, chart plans, and assign targets such that it becomes a systematic process to achieving goals and objectives and having productive conversations about performance outcomes and career development. Our talent management framework enables us to meet the human capital and business needs within the organization. From identification of critical roles to succession planning and retention management practices, the team provides resources and tools, and leads the processes and experiences that enable us to make sure that we have everything in place to successfully execute on our talent management strategy.
Our efforts to promote a positive employee experience and build a diverse and inclusive culture are further supported and enhanced by local and national in-person and virtual events, including town halls, in-office celebrations and employee activity committees. We have also developed a taskforce that seeks to drive focused and targeted diversity and inclusion efforts, including employee focus groups and participation up and down the organization to ensure all voices are heard.
12
Government Regulation
Regulatory Licensing and Certification
Many states, including Florida, require regulatory approval, including licensure and certification, before establishing certain types of clinics offering certain professional and ancillary services, including the services P3 offers. The operations of the P3 owned and managed clinics are subject to extensive federal, state and local regulation relating to, among other things, the adequacy of medical care, equipment, personnel, operating policies and procedures, and proof of financial ability to operate. Our ability to operate profitably will depend in part on the ability of P3 owned and managed clinics and its providers to obtain and maintain all necessary licenses and other approvals, and maintain updates to their enrollment in the Medicare and Medicaid programs, including the addition of new clinic locations, providers and other enrollment information. In addition, certain ancillary services such as the provision of diagnostic laboratory testing require additional state and federal licensure and regulatory oversight, including oversight by CMS, under Clinical Laboratory Improvement Amendments of 1988 (“CLIA”) which requires all clinical laboratories to meet certain quality assurance, quality control and personnel standards, and comparable state laboratory licensing authorities. Standards for testing under CLIA are based on the complexity of the tests performed by the laboratory, with tests classified as “high complexity,” “moderate complexity,” or “waived.” P3 owned and managed clinics hold CLIA Certificates of Waiver and perform certain CLIA-waived tests, which subjects such clinics to certain CLIA requirements. Sanctions for failure to comply with applicable state and federal licensing, certification and other regulatory requirements include suspension, revocation or limitation of the applicable authorization, significant fines and penalties and/or an inability to receive reimbursement from government healthcare programs and other third-party payors.
With respect to P3’s providers participating in its network, P3 providers must meet minimum requirements to apply for participation or continued participation with P3 through a credentialing process, including, without limitation, having a valid, current medical license and Drug Enforcement Administration registration, if required for the provider’s scope of practice, the absence of any debarment, suspension, exclusion or other restriction from receiving payments from any government or other third-party payor program, and clearing National Practitioner Data Bank of any reports and/or disciplinary actions. P3’s credentialing program is designed to meet CMS and the National Committee for Quality Assurance (“NCQA”) credentialing requirements as well as applicable federal and state laws. P3’s credentialing committee is comprised of a group of multispecialty providers with responsibilities for thoroughly reviewing each P3 provider’s qualifications and credentials. Providers are generally recredentialed every three years or more often if necessary, which is consistent with industry guidelines. In addition, network providers are required under their participating provider agreements with P3 to have established an ongoing quality assurance program. Moreover, P3’s contracts may allow P3 to withhold compensation from time to time based upon the providers meeting certain quality metrics, including HEDIS quality measures and care coordination metrics.
State Corporate Practice of Medicine and Fee-Splitting Laws
Our arrangements with our affiliated professional entities and other physician partners are subject to various state laws, commonly referred to as corporate practice of medicine and fee-splitting laws, which are intended to prevent unlicensed persons from interfering with or influencing the physician’s professional judgment, and prohibiting the sharing of professional service fees with non-professional or business interests. These laws vary from state to state, including those where the Company does business, and are subject to broad interpretation and enforcement by state regulators. For example, the corporate practice of medicine prohibition in Nevada has only been established through attorney general opinions and there is no statutory or regulatory fee-splitting prohibition in the state. Arizona’s corporate practice of medicine was established under older case law, and more recent legislation suggests that the prohibition may not be strictly enforced in the state. Oregon prohibits the corporate practice of medicine but has an exception for professional corporations with majority physician ownership where a non-licensed person or entity may hold minority ownership interest in such professional corporation. Florida does not prohibit the corporate practice of medicine but has professional fee-splitting laws, which prohibit the sharing of professional fees based on referrals for professional services.
California’s corporate practice of medicine doctrine has been developed through statutes, case law and state attorney general opinions. The general prohibition on the corporate practice of medicine arises out of the California Business and Professions Code, which has been enforced through case law and attorney general opinions. In California, physicians and certain licensed professionals cannot be employed by non-professional corporations, except under limited exceptions which do not apply to the Company. Additionally, all clinical decisions and certain business or management decisions that result in control over a physician’s practice of medicine or a licensed professional’s clinical decisions must be made by a physician or licensed professional and not by an unlicensed person or entity. California also prohibits professional fee splitting arrangements, but management fees based on a percentage of gross
13
revenue or similar arrangement that is commensurate with fair market value of services provided by the management company are generally permissible.
We believe we have structured our management services agreements with the our affiliated professional entities to comply with the corporate practice of medicine and fee-splitting laws of Nevada, and we expect to enter into similar agreements with affiliated professional entities in California and other states where we may operate in the future, where all clinical decisions and other business and management decisions that result in control over a physician’s practice of medicine or a licensed professional’s clinical decisions remain exclusively with the affiliated professional entities, their physician shareholders and the physicians and licensed professionals employed and contracted by such entities.
A determination of non-compliance against us and/or our affiliated professional entities or other physician partners based on the reinterpretation of existing laws or adoption of new laws could lead to adverse judicial or administrative action, civil or criminal penalties, receipt of cease-and-desist orders from state regulators, loss of provider licenses, and/or restructuring of these arrangements.
Healthcare Fraud and Abuse Laws
We are subject to a number of federal and state healthcare regulatory laws that restrict certain business practices in the healthcare industry. These laws include, but are not limited to, federal and state anti-kickback, false claims, self-referral and other healthcare fraud and abuse laws.
The federal Anti-Kickback Statute (“AKS”) prohibits, among other things, knowingly and willfully offering, paying, soliciting or receiving remuneration, directly or indirectly, in cash or kind, to induce or reward either the referral of an individual for, or the purchase, order or recommendation of, any good or service, for which payment may be made under federal and state healthcare programs such as Medicare and Medicaid. A person or entity does not need to have actual knowledge of the statute or specific intent to violate it in order to have committed a violation.
Several courts have interpreted the AKS’s intent requirement to mean that if any one purpose of an arrangement involving remuneration is to induce referrals of federal healthcare covered business, the AKS has been violated.
The AKS includes statutory exceptions and regulatory safe harbors that protect certain arrangements. By way of example, the AKS safe harbor for value-based arrangements and the safe harbor for arrangements between managed care organizations and downstream contractors both require, among other things, that the arrangement does not induce a person or entity to reduce or limit medically necessary items or services furnished to any patient. Failure to meet the requirements of an applicable AKS safe harbor, however, does not render an arrangement illegal. Rather, the government may evaluate such arrangements on a case-by-case basis, taking into account all facts and circumstances, including the parties’ intent and the arrangement’s potential for abuse, and may be subject to greater scrutiny by enforcement agencies.
The Stark Law prohibits a physician who has a financial relationship, or who has an immediate family member who has a financial relationship, with entities providing designated health services (“DHS”) from referring Medicare and Medicaid patients to such entities for the furnishing of DHS, unless an exception applies. The Stark Law also prohibits the entity from billing for any such prohibited referral. Unlike the AKS, the Stark Law is violated if the financial arrangement does not meet an applicable exception, regardless of any intent by the parties to induce or reward referrals or the reasons for the financial relationship and the referral.
The federal False Claims Act (“FCA”) prohibits a person from knowingly presenting, or caused to be presented, a false or fraudulent request for payment from the federal government, or from making a false statement or using a false record to have a claim approved. A claim includes “any request or demand” for money or property presented to the United States government. Moreover, the government may assert that a claim including items and services resulting from a violation of the AKS or the Stark Law constitutes a false or fraudulent claim for purposes of the civil FCA. Penalties for a violation of the FCA include fines for each false claim, plus up to three times the amount of damages caused by each false claim. Private individuals also have the ability to bring actions under these false claims laws in the name of the government alleging false and fraudulent claims presented to or paid by the government (or other violations of the statutes) and to share in any amounts paid by the entity to the government in fines or settlement. Such suits, known as qui tam actions, are pervasive in the healthcare industry.
14
Further, the Civil Monetary Penalties Statute authorizes the imposition of civil monetary penalties, assessments and exclusion against an individual or entity based on a variety of prohibited conduct, including, but not limited to offering remuneration to a federal health care program beneficiary that the individual or entity knows or should know is likely to influence the beneficiary to order or receive health care items or services from a particular provider. Moreover, in certain cases, providers who routinely waive copayments and deductibles for Medicare and Medicaid beneficiaries can also be held liable under the AKS and civil FCA. One of the statutory exceptions to the prohibition is non-routine, unadvertised waivers of copayments or deductible amounts based on individualized determinations of financial need or exhaustion of reasonable collection efforts. The U.S. Department of Health and Human Services (“HHS”) Office of Inspector General emphasizes, however, that this exception should only be used occasionally to address special financial needs of a particular patient. Although this prohibition applies only to federal healthcare program beneficiaries, the routine waivers of copayments and deductibles offered to patients covered by commercial payors may implicate applicable state laws related to, among other things, unlawful schemes to defraud, excessive fees for services, tortious interference with patient contracts and statutory or common law fraud.
The Health Insurance Portability and Accountability Act, as amended by the Health Information Technology for Economic and Clinical Health Act of 2009 (collectively, “HIPAA”), also established federal criminal statutes that prohibit, among other things, knowingly and willfully executing, or attempting to execute, a scheme to defraud any healthcare benefit program, including private third-party payors, and knowingly and willfully falsifying, concealing or covering up a material fact or making any materially false, fictitious or fraudulent statement in connection with the delivery of or payment for healthcare benefits, items or services. Similar to the AKS, a person or entity does not need to have actual knowledge of the statute or specific intent to violate it in order to have committed a violation.
Several states in which we operate have also adopted similar fraud and abuse laws as described above. The scope of these laws and the interpretations of them vary from state to state and are enforced by state courts and regulatory authorities, each with broad discretion. Some state fraud and abuse laws apply to items or services reimbursed by any payor, including patients and commercial insurers, not just those reimbursed by a federally funded healthcare program.
Violation of any of these laws or any other governmental regulations that apply may result in significant penalties, including, without limitation, administrative civil and criminal penalties, damages, disgorgement, fines, additional reporting requirements and compliance oversight obligations, in the event that a corporate integrity agreement or other agreement is required to resolve allegations of noncompliance with these laws, the curtailment or restructuring of operations, exclusion from participation in governmental healthcare programs and/or individual imprisonment.
Healthcare Reform
In the United States, there have been, and we expect there will continue to be, a number of legislative and regulatory changes to the healthcare system, many of which are intended to contain or reduce healthcare costs. By way of example, in the United States, the Affordable Care Act, as amended by the Health Care and Education Reconciliation Act (collectively, the “ACA”), substantially changed the way healthcare is financed by both governmental and private insurers. The ACA required, among other things, CMS to establish a Medicare shared savings program that promotes accountability and coordination of care through the creation of Accountable Care Organizations (“ACOs”). The Medicare shared savings program allows for providers, physicians and other designated health care professionals and suppliers to form ACOs and voluntarily work together to invest in infrastructure and redesign delivery processes to give coordinated high quality care to their Medicare patients, avoid unnecessary duplication of services and prevent medical errors. ACOs that achieve quality performance standards established by CMS are eligible to share in a portion of the Medicare program’s cost savings. ACO program methodologies and participation requirements are updated by CMS for each performance year and participants are expected to comply with such program requirements and required to report on performance after the close of the year. ACOs that fail to comply with such program requirements can face penalties or even termination of their participation in the Medicare shared savings program.
Since its enactment, there have been judicial, executive and Congressional challenges to certain aspects of the ACA. On June 17, 2021, the U.S. Supreme Court dismissed the most recent judicial challenge to the ACA without specifically ruling on the constitutionality of the ACA. Prior to the Supreme Court’s decision, President Biden issued an executive order initiating a special enrollment period from February 15, 2021 through August 15, 2021 for purposes of obtaining health insurance coverage through the ACA marketplace. The executive order also instructed certain governmental agencies to review and reconsider their existing policies and rules that limit access to healthcare.
15
In addition, other legislative changes have been proposed and adopted since the ACA was enacted. These changes included aggregate reductions to Medicare payments to providers, which went into effect on April 1, 2013 and, due to subsequent legislative amendments to the statute, will remain in effect through 2032, with the exception of a temporary suspension from May 1, 2020 through March 31, 2022, unless additional Congressional action is taken. In addition, on January 2, 2013, the American Taxpayer Relief Act of 2012 was signed into law, which, among other things, reduced Medicare payments to several providers, including hospitals, and increased the statute of limitations period for the government to recover overpayments to providers from three to five years.
Additionally, the Center for Medicare and Medicaid Innovation continues to test an array of value-based alternative payment models, including the Global and Professional Direct Contracting Model to allow Direct Contracting Entities to negotiate directly with the government to manage traditional Medicare beneficiaries and share in the savings and risks generated from managing such beneficiaries. Although we currently do not participate in these pilot payment models, we may choose to do so in the future. Additional changes that may affect our business include the expansion of new programs such as Medicare payment for performance initiatives for physicians under the Medicare Access and CHIP Reauthorization Act of 2015, which first affected physician payment in 2019. At this time, it is unclear how the introduction of the Medicare quality payment program will impact overall physician reimbursement. In addition, there likely will continue to be regulatory proposals directed at containing or lowering the cost of healthcare, as government healthcare programs and other third-party payors transition from FFS to value-based reimbursement models, which can include risk-sharing, bundled payment and other innovative approaches. It is possible that the federal or state governments will implement additional reductions, increases, or changes in reimbursement in the future under government programs that may adversely affect us or increase the cost of providing our services. The implementation of cost containment measures or other healthcare reforms may prevent us from being able to generate revenue or attain growth, any of which could have a material impact on our business.
Further, healthcare providers and industry participants are also subject to a growing number of requirements intended to promote the interoperability and exchange of patient health information. For example, on April 5, 2021, healthcare providers and certain other entities became subject to information blocking restrictions pursuant to the Cures Act that prohibit practices that are likely to interfere with the access, exchange or use of electronic health information, except as required by law or specified by the HHS as a reasonable and necessary activity. Violations may result in penalties or other disincentives. It is unclear at this time what the costs of compliance with the new rules will be and what additional risks there may be to our business.
Data Privacy and Security Laws
We are subject to a number of federal and state laws and regulations that govern the collection, use, disclosure, and protection of health-related and other personal information, including health information privacy and security laws, data breach notification laws, and consumer protection laws and regulations (e.g., Section 5 of the Federal Trade Commission Act). For example, HIPAA imposes obligations on “covered entities,” including certain healthcare providers, such as the affiliated professional entities, health plans, and healthcare clearinghouses, and their respective “business associates” that create, receive, maintain or transmit individually identifiable health information for or on behalf of a covered entity, such as P3, as well as their covered subcontractors with respect to safeguarding the privacy, security and transmission of individually identifiable health information. Entities that are found to be in violation of HIPAA, whether as the result of a breach of unsecured protected health information (“PHI”), a complaint about privacy practices, or an audit by HHS, may be subject to significant civil, criminal, and administrative fines and penalties and/or additional reporting and oversight obligations if required to enter into a resolution agreement and corrective action plan with HHS to settle allegations of HIPAA non-compliance.
In addition, certain state laws, such as the Confidentiality of Medical Information Act, the California Consumer Privacy Act, and the California Privacy Rights Act, govern the privacy and security of personal information, including health-related information in certain circumstances, some of which are more stringent than HIPAA and many of which differ from each other in significant ways and may not have the same effect, thus complicating compliance efforts.
Failure to comply with these laws, where applicable, can result in the imposition of significant civil and/or criminal penalties and private litigation. Privacy and security laws, regulations, and other obligations are constantly evolving, may conflict with each other to complicate compliance efforts, and can result in investigations, proceedings, or actions that lead to significant civil and/or criminal penalties and restrictions on data processing.
16
Federal and State Insurance and Managed Care Laws
Regulation of downstream risk-sharing arrangements, including, but not limited to, at-risk and other value-based arrangements, varies significantly from state to state. Some states require downstream entities and risk-bearing entities to obtain an insurance license, a certificate of authority, or an equivalent authorization, in order to participate in downstream risk-sharing arrangements with payors. In some states, statutes, regulations and/or formal guidance explicitly address whether and in what manner the state regulates the transfer of risk by a payor to a downstream entity. However, the majority of states do not explicitly address the issue, and in such states, regulators may nonetheless interpret statutes and regulations to regulate such activity. If downstream risk-sharing arrangements are not regulated directly in a particular state, the state regulatory agency may nonetheless require oversight by the licensed payor as the party to such a downstream risk-sharing arrangement. Such oversight is accomplished via contract and may include the imposition of reserve requirements, as well as reporting obligations. Further, state regulatory stances regarding downstream risk-sharing arrangements can change rapidly and codified provisions may not keep pace with evolving risk-sharing mechanisms and other new value-based reimbursement models. Certain of the states where we currently operate or may choose to operate in the future regulate the operations and financial condition of risk bearing organizations like us and our affiliated providers. By way of example, P3 recently acquired Medcore HP, a licensed health plan under the Knox Keene Act, which subjects the entity to certain capital requirements, licensing or certification, governance controls, utilization review and grievance procedures, among others. While these regulations have not had a material impact on our business to date, as we continue to expand, for example, through acquisitions or otherwise, these rules may require additional resources and capitalization and add complexity to our business.
Seasonality
Our business experiences some variability depending upon the time of the year. While new patients are attributed to our platform throughout the year, we experience the largest portion of our at-risk membership growth during the first quarter. Operations in our new markets generally begin on January 1, at which time our payor partners attribute patients to our physician partners as our agreements with those payors in those geographies become effective. This coincides with the beginning of the Medicare program year, when plan enrollment selections made during the prior Annual Enrollment Period, which runs each year from October 15 to December 7, take effect.
In addition, in January of each year, CMS revises the risk adjustment factor for each patient based upon health conditions documented in the prior year, leading to an overall increase in per-member revenue. As the year progresses, our per-member revenue declines as new members join us typically with less complete or accurate documentation (and therefore lower risk-adjustment scores) and patient morbidity disproportionately impacts our higher-risk (and therefore greater revenue) members.
Medical costs will vary seasonally depending on a number of factors, including the weather and the number of calendar working days in a given period. Certain illnesses, such as the influenza virus, are far more prevalent during colder months of the year, which will result in an increase in medical expenses during these time periods. We therefore expect to see higher levels of per member medical costs in the first and fourth quarters.
Additional Information
We were incorporated under the laws of the State of Delaware on August 20, 2020 under the name Foresight Acquisition Corp. Upon the closing of the Business Combinations, we changed our name to P3 Health Partners Inc. Our principal executive offices are located at 2370 Corporate Circle, Suite 300, Henderson, NV 89074 and our telephone number is (702) 910-3950. Our website is www.p3hp.com. Under the investor relations page of the Company’s website, ir.p3hp.org, we make available free of charge a variety of information for investors, including our annual reports on Form 10-K, quarterly reports on Form 10-Q, current reports on Form 8-K, Proxy Statements on Schedule 14A and any amendments to those materials filed or furnished pursuant to Section 13(a) or 15(d) of the Securities Exchange Act of 1934, as amended, as soon as reasonably practicable after we electronically file that material with or furnish it to the Securities and Exchange Commission (“SEC”). The information found on our website is not part of this or any other report we file with, or furnish to, the SEC.
17
Item 1A. Risk Factors.
Our business involves a high degree of risk. You should carefully consider the risks and uncertainties described below, together with all of the other information in this Form 10-K. The occurrence of any of the events described below could harm our business, operating results, financial condition, liquidity, or prospects. In any such event, the market price of our Class A common stock could decline, and you may lose all or part of your investment. Additional risks and uncertainties not presently known to us, or that we currently deem immaterial, may also impair our business. See “Cautionary Statement Regarding Forward-Looking Statements.”
Risks Related to Our Business and Financial Results
Our management has performed an analysis of our ability to continue as a going concern and has identified substantial doubt about our ability to continue as a going concern.
As of December 31, 2022, we had $17.5 million in cash available to fund future operations. Without additional funding, management believes that our existing cash resources are not sufficient to support planned operations for at least the next year from the issuance of this Form 10-K. Based on their assessment, our management has raised concerns about our ability to continue as a going concern. As substantial doubt about our ability to continue as a going concern exists, our ability to finance our operations through the sale and issuance of debt or equity securities or through bank or other financing could be impaired. Our ability to continue as a going concern may depend on our ability to obtain additional capital. Management continues to explore raising additional capital through a combination of debt financing, other non-dilutive financing, and/or equity financing to supplement the Company’s capitalization and liquidity. Our ability to obtain financing on reasonable terms is subject to factors beyond the Company’s control, including general economic, political, and financial market conditions. The capital markets have in the past experienced, are currently experiencing, and may in the future experience, periods of upheaval that could impact the availability and cost of equity and debt financing and there can be no assurance that such financing will be available on terms commercially acceptable to the Company. If we are unable to raise additional capital or generate cash flows necessary to fund our operations, we may not be able to compete successfully and may need to scale back, discontinue, or cease certain operations, which would harm our business, financial condition, and results of operations.
Risks Related to Our Operating History and Early Stage of Growth
We have a history of net losses. We expect to continue to incur losses for the foreseeable future and we may never achieve or maintain profitability.
For the year ended December 31, 2022, the Successor Period of 2021, and the Predecessor Period of 2021, we incurred net losses of $1,561.6 million, $57.9 million, and $146.4 million, respectively. As of December 31, 2022, we had an accumulated deficit of $309.5 million. We expect that our operating expenses will continue to increase as we grow our business, build relationships with physician partners and payors, develop new services and comply with the requirements associated with being a public company. Since our inception, we have financed our operations primarily through cash we obtained as a result of the Business Combinations, private placements of equity securities, issuances of promissory notes, payments received from various payors and borrowings under our credit facilities. We may not succeed in sufficiently increasing our revenue to offset these expenses. Consequently, we may not be able to achieve and maintain profitability for the current or any future fiscal year. We may never be able to generate sufficient revenue to achieve or sustain profitability and our recent and historical growth should not be considered indicative of our future performance.
We may need to raise additional capital to fund our existing operations or develop and commercialize new services or expand our operations.
We may need to spend significant amounts to expand our existing operations, including expansion into new geographies, to improve our platform and to develop new services. Based upon management’s assessment of the Company’s ability to continue as a going concern as described above in the risk factor entitled “Our management has performed an analysis of our ability to continue as a going concern and has identified substantial doubt about our ability to continue as a going concern,” we believe that our existing cash, cash equivalents and restricted cash may not be sufficient to fund our operating and capital needs for at least the next 12 months. We maintain the majority of our cash, cash equivalents and restricted cash in accounts with major U.S. financial institutions, and our deposits at these institutions, at times, may exceed insured limits. Market conditions can impact the viability of these institutions. In
18
the event of failure of any of the financial institutions where we maintain our cash, cash equivalents and restricted cash, there can be no assurance that we would be able to access uninsured funds in a timely manner or at all. Any inability to access or delay in accessing these funds could adversely affect our business and financial position.
Our expectation regarding the sufficiency of funds is based on assumptions that may prove to be wrong, and we could use our available capital resources sooner than we currently expect. Until such time, if ever, as we can generate sufficient revenue, we may finance our cash needs through a combination of equity offerings and debt financings or other sources. In addition, we may seek additional capital due to favorable market conditions or strategic considerations, even if we believe that we have sufficient funds for our current or future operating plans.
Our present and future funding requirements will depend on many factors, including:
| ● | our ability to achieve revenue growth; |
| ● | our ability to effectively manage medical expense amounts; |
| ● | the cost of expanding our operations, including our geographic scope, and our offerings, including our marketing efforts; |
| ● | our rate of progress in launching, commercializing and establishing adoption of our services; and |
| ● | the effect of competing technological and market developments. |
To the extent that we raise additional capital through the sale of equity or convertible debt securities, your ownership interest will be diluted, and the terms of these securities may include liquidation or other preferences that adversely affect your rights as a securityholder. For example, on December 13, 2022, in connection with our issuance of an unsecured promissory note (the “VGS Promissory Note”) to VBC Growth SPV LLC (“VGS”), we entered into a Warrant Agreement with VGS (the “VGS Warrant Agreement”) pursuant to which P3 LLC issued warrants to purchase 429,180 shares of our Class A common stock at an exercise price of $4.26 per share (the “VGS Warrants”) to VGS. In addition, debt financing and preferred equity financing, if available, may involve agreements that include covenants limiting or restricting our ability to take specific actions, such as incurring additional debt, making capital expenditures or declaring dividends and these forms of financing may have rights, preferences, and privileges senior to those of holders of our common stock. If we raise additional funds through collaborations, strategic alliances or marketing, distribution or licensing arrangements with third parties, we may be required to relinquish valuable rights to our technologies, intellectual property, or future revenue streams or grant licenses on terms that may not be favorable to us. Furthermore, any capital raising efforts may divert our management from their day-to-day activities, which may adversely affect our ability to advance development activities. If we are unable to raise additional funds when needed, we may be required to delay, limit, reduce or terminate development efforts.
Our business and the markets in which we operate are new and rapidly evolving, which makes it difficult to evaluate our future prospects and the risks and challenges we may encounter.
Our business and the markets in which we operate are new and rapidly evolving which make it difficult to evaluate and assess the success of our business to date, our future prospects and the risks and challenges that we may encounter. These risks and challenges include our ability to:
| ● | attract new members and partner physicians to our platform and position our platform as a convenient and accepted way to access and deliver healthcare; |
| ● | retain our current members, affiliated professional entities and other physician partners and encourage them to continue to utilize our platform and services; |
| ● | gain market acceptance of our services and products with members and physicians and maintain and expand such relationships; |
| ● | comply with existing and new laws and regulations applicable to our business and in our industry; |
19
| ● | anticipate and respond to changes in Medicare reimbursement rates and the markets in which we operate; |
| ● | react to challenges from existing and new competitors; |
| ● | maintain and enhance our reputation and brand; |
| ● | effectively manage our growth and business operations, including new geographies; |
| ● | forecast our revenue, which includes reimbursements, and budget for, and manage, our expenses, including our medical expense amounts, and capital expenditures; |
| ● | hire and retain talented individuals at all levels of our organization; |
| ● | maintain and improve the infrastructure underlying our platform, including our data protection, intellectual property and cybersecurity; and |
| ● | successfully update our platform and services, including expanding our services into different healthcare products and services, develop and update our software, offerings and services to benefit our members. |
If we fail to understand fully or adequately address the challenges that we are currently encountering or that we may encounter in the future, including those challenges described here and elsewhere in this “Risk Factors” section, our business, financial condition and results of operations could be adversely affected. If the risks and uncertainties that we plan for when operating our business are incorrect or change, or if we fail to manage these risks successfully, our results of operations could differ materially from our expectations and our business, financial condition and results of operations could be adversely affected.
Our relatively limited operating history makes it difficult to evaluate our future prospects and the risks and challenges we may encounter.
We were established in 2017 and we are continuing to grow our marketing and management capabilities. Consequently, predictions about our future success or viability may not be as accurate as they could be if we had a longer operating history. If our growth strategy is not successful, we may not be able to continue to grow our revenue or operations. Our relatively limited operating history, evolving business and rapid growth make it difficult to evaluate our future prospects and the risks and challenges we may encounter, and we may not continue to grow at or near historical rates.
In addition, as a business with a limited operating history, we may encounter unforeseen expenses, difficulties, complications, delays and other known and unknown challenges. We are transitioning to a company capable of supporting commercialization, sales and marketing. We may not be successful in such a transition and, as a result, our business may be adversely affected.
20
We may not be able to maintain compliance with our debt covenants in the future which could result in an event of default.
Our Term Loan Facility (as defined herein) with CRG Partners (the “Lender”) and the VGS Promissory Note contain affirmative and negative covenants which, among other things, require us to maintain minimum liquidity and annual minimum revenue levels that increase over time and restrict P3 LLC’s ability and the ability of its subsidiaries from, among other things, incurring certain indebtedness and liens, and making certain restricted payments. If we breach these or other financial covenants and fail to secure a waiver or forbearance from the lenders, such breach or failure could result in an event of default and accelerate the repayment of the outstanding or the exercise of other rights or remedies that our lenders may have under applicable law. As of December 31, 2022, the Company was not in compliance with the Term Loan Facility or VGS Promissory Note covenants related to issuance of the 2022 financial statements with an audit opinion free of a “going concern” qualification. The lenders have granted a waiver of the covenant under the debt agreements related to the existence of a “going concern” qualification in the audit opinion for our audited financial statements for the fiscal year ended December 31, 2022. We were in compliance with all other covenants under the debt agreements as of December 31, 2022. However, there can be no assurance that we will be able to maintain compliance with these covenants in the future or that the lenders under the Facility or the lenders of any future indebtedness we may incur will grant us any such waiver or forbearance in the future.
We may experience difficulties in managing our growth and expanding our operations.
We expect to experience significant growth in the scope of our operations. Our ability to manage our operations and future growth will require us to continue to improve our operational, financial and management controls, compliance programs and reporting systems. We may not be able to implement improvements in an efficient or timely manner and may discover deficiencies in existing controls, programs, systems and procedures, which could have an adverse effect on our business, reputation and financial results. Additionally, rapid growth in our business may place a strain on our human and capital resources.
We may not recognize the anticipated benefits of recent and future acquisitions and any such acquisitions could disrupt our operations and have a material adverse effect on our business, financial condition and results of operations.
The anticipated benefits of the Company’s Business Combinations, other recent acquisitions, including the Medcore Acquisition in December 2021, and any future acquisitions may not be realized fully, or at all, and may take longer to realize than expected. Anticipated benefits of any acquisition may be affected by, among other things, competition and our ability to grow and manage growth profitably. Further, we may not be able to continue the operational success or successfully finance or integrate any businesses that we acquire. The integration of any acquisition may divert management’s time and resources from our core business and disrupt our operations or may result in conflicts with our business. Any acquisition may not be successful, may reduce our cash reserves, may negatively affect our earnings and financial performance and, to the extent financed with the proceeds of debt, may increase our indebtedness. We cannot ensure that any acquisition we make will not have a material adverse effect on our business, financial condition and results of operations.
A significant portion of our assets consists of other intangible assets, the value of which may be reduced if we determine that those assets are impaired.
As of December 31, 2022, the net carrying value of other intangible assets represented $751.1 million, or 86% of our total assets. Indefinite-lived intangible assets are evaluated for impairment annually, or more frequently if circumstances indicate impairment may have occurred. Definite-lived intangible assets totaling $750.4 million are amortized over 10 years.
Due to the decrease in the share price over the second and fourth quarters of 2022, the Company recorded a significant goodwill impairment charge of $1,315.0 million during the year ended December 31, 2022. If future operating performance were to fall below current projections or if there are material changes to management’s assumptions, we could be required to recognize additional non-cash charges to operating earnings for other intangible asset impairment, which could be significant.
21
Risks Related to Our Business and Industry
The COVID-19 pandemic has impacted, and may, along with future pandemics or epidemics, continue to impact, our operations and may materially and adversely affect our business and financial results.
COVID-19 continues to impact the United States and the rest of the world and the pandemic has led to significant economic disruption. The impact of COVID-19 on the economy and the healthcare industry is ongoing. We continue to monitor the impact of COVID-19 on our business. The extent to which COVID-19 or a new pandemic, epidemic, or outbreak of an infectious disease may directly or indirectly impact our operations and results of operations will depend on multiple factors, including, but not limited to the ultimate geographic spread of the disease, the duration and scope of the outbreak, the emergence of variants, the availability and efficacy of vaccines, and government, social, business and other actions that are taken in response to the pandemic or outbreak. We may be unable to properly anticipate or prepare for these events and, as a result, our business may be materially adversely impacted.
Due to COVID-19 or another pandemic or public health emergency, we may not be able to document the health conditions of our members as completely as we have in the past. Medicare pays capitation using a “risk adjustment model,” which compensates providers based on the health status (acuity) of each individual member. Payers with higher acuity members receive more, and those with lower acuity members receive less. Medicare requires that a patient’s health issues be documented annually regardless of the permanence of the underlying causes. Historically, this documentation was required to be completed during an in-person visit with a patient. As part of the Coronavirus Aid, Relief and Economic Security Act (“CARES Act”), Medicare is allowing documentation for conditions identified during video visits with patients. However, given the disruption caused by COVID-19, it is unclear whether we will be able to document the health conditions of our members as comprehensively as we did before COVID-19, which may adversely impact our revenue in future periods.
Due to our recurring contracted revenue model, the COVID-19 pandemic did not have a material impact on our revenue during 2021 and 2022. Nearly 99% of our total revenue in 2022 and 98% of our total revenue in 2021 is recurring, consisting of fixed per member per month capitation payments received from MA health plans. Based upon claims paid to date, our direct costs in medical claims expense related to COVID-19 claims were approximately $95.5 million for the period from March 1, 2020 through December 31, 2022. We expect to incur additional COVID-19 related costs given the volume of positive cases and “breakthrough” cases (positive cases in vaccinated patients) present in our markets. Because of the nature of capitation arrangements, the full impact of the COVID-19 pandemic may not be fully reflected in our results of operations and overall financial condition until future periods.
To the extent the COVID-19 pandemic adversely affects our business and financial results, it may also have the effect of heightening many of the other risks described in this “Risk Factors” section, including but not limited to the fact that our platform and the other systems or networks used in our business may experience an increase in attempted cyberattacks or targeted intrusion, ransomware, and phishing campaigns seeking to take advantage of shifts to employees working remotely using their household or personal internet networks. The success of any of these unauthorized attempts could substantially impact our platform, the proprietary and other confidential data contained therein or otherwise stored or processed in our operations, and ultimately our business, including but not limited to increased expenses incurred to improve our security controls and to remediate security vulnerabilities.
We rely on our management team and key employees and our business, financial condition, cash flows and results of operations could be harmed if we are unable to retain qualified personnel.
Our success depends largely upon the continued services of key members of senior management and other key employees. Most key employees are at-will employees and therefore they may terminate employment with us at any time with no advance notice. We also rely on our leadership team in the areas of managed care, operations and general and administrative functions. From time to time, there may be changes in our management team resulting from the hiring or departure of executives, which could disrupt our business. The replacement of one or more of our executive officers or other key employees would likely involve significant time and costs and may significantly delay or prevent the achievement of our business objectives. Our business would also be adversely affected if we fail to adequately plan for succession of our leadership or if we fail to effectively recruit, integrate, retain and develop key talent and/or align our talent with our business needs, in light of the current rapidly changing environment.
Competition for qualified personnel in our industry is intense due to the limited number of individuals who possess the required skills and experience. In particular, we face substantial competition for physicians and other healthcare providers. As a result, as we continue to grow and enter new geographies, it may be difficult for us to hire additional qualified personnel with the necessary
22
skills. We continued to experience labor shortages in 2022, in part due to the ongoing effects of COVID-19. A number of factors have and may in the future adversely affect the labor force available to us or increase labor costs, including high employment levels, federal unemployment subsidies, increased wages offered by other employers, vaccine mandates and other government regulations. In addition, we have experienced high employee turnover and expect to continue to experience high employee turnover in the future. New hires require significant training and, in most cases, take significant time before such personnel achieve full productivity. New employees may not become as productive as we expect, and we may be unable to hire or retain sufficient numbers of qualified individuals. If our retention efforts are not successful or our employee turnover rate increases in the future, our business, financial condition, cash flows and results of operations will be harmed.
Finally, as job candidates often consider the value of the stock options or other equity instruments they are to receive in connection with their employment, the volatility in the price of our stock may adversely affect our ability to attract or retain highly skilled personnel. Further, the requirement to expense stock options and other equity instruments may discourage us from granting the size or type of stock option or equity awards that job candidates require to join our company. Failure to attract new personnel or failure to retain and motivate our current personnel could have a material adverse effect on our business, financial condition and results of operations.
Our growth depends in part on our ability to identify and develop successful new geographies, physician partners, payors and patients. If we are not able to successfully execute upon our growth strategies, there may be a material adverse effect on our business, financial condition, cash flows and results of operations.
Our business depends on our ability to identify and develop successful geographies and relationships with physician partners and payors, and to successfully execute upon our growth initiatives to increase the profitability of our physician partners. In order to pursue our strategy successfully, we must effectively implement our platform, partnership and network model, including identifying suitable candidates and successfully building relationships with and managing integration of new physician partners and payors. We contract with a limited number of affiliated professional entities and other physician partners and rely on such physicians within each geography. Our growth initiatives in our existing geographies depend, in part, on our physician partners’ ability to increase their capacity to service Medicare patients, and to effectively meet increased patient demand. Our affiliated professional entities and other physician partners may encounter difficulties in recruiting additional primary care physicians to their practices due to many factors, including significant competition in their geographies. Accordingly, the loss or dissatisfaction of any physician partners, our inability to recruit and integrate physician partners into our model, or the failure of our affiliated professional entities or other physician partners to recruit additional primary care physicians or manage and scale capacity to timely meet patient demand, could substantially harm our brand and reputation, impact our competitiveness, inhibit widespread adoption of our platform, partnership and network model and impair our ability to attract new physician partners and maintain existing physician partnerships, both in new geographies and in geographies in which we currently operate, which could have a material adverse effect on our business, financial condition, cash flows and results of operations.
Further, our growth strategy depends, in part, on securing and integrating new high-caliber physician partners and expanding into new geographies in which we have little or no operating experience. Integration and other risks can be more pronounced for larger and more complicated relationships or relationships outside of our core business space, or if multiple relationships are pursued simultaneously. Additionally, new geographies may be characterized by stakeholder preferences for, and experience with, rates of MA enrollment, MA reimbursement rates, payor concentration and rates of unnecessary variability in and utilization of medical care that differ from those in the geographies where our existing operations are located. Likewise, new geographies into which we seek to expand may have laws and regulations that differ from those applicable to our current operations. As an immature and rapidly growing company, we may be unfamiliar with the regulatory requirements in each geography that we enter, and we may be forced to incur significant expenditures to ensure compliance with requirements to which we are subject. If we are unable or unwilling to incur such costs, our growth in new geographies may be less successful than in our current geographies.
Further, our growth to date has increased the significant demands on our management, operational and financial systems, infrastructure and other resources. We must continue to improve our existing systems for operational and financial management, including our reporting systems, procedures and controls. These improvements could require significant capital expenditures and place increasing demands on our management. We may not be successful in managing or expanding our operations or in maintaining adequate financial and operating systems and controls. If we do not successfully manage these processes, our business, financial condition, cash flows and results of operations could be harmed.
23
If growth in the number of patients and physician partners on our platform decreases, or the number of services that we are able to provide to physician partners and members decreases, due to legal, economic or business developments, our business, financial condition and results of operations will be harmed.
Substantially all of our total revenue relates to federal government healthcare programs. The policies and decisions made by the federal government regarding these programs have a substantial impact on our profitability. Additionally, our future results of operations depend, in part, on our ability to expand our services and offerings, including broadening our continuum of care. As we grow our member base, we will need to maintain and grow our network of providers. Certain of our providers are permitted to provide services on other platforms, and therefore, our success will be dependent on our ability to retain and recruit highly trained and licensed physicians and other providers to our platform.
There are sometimes wide variations in the established per member reimbursement rates as a result of, among other things, members’ risk status, acuity levels and age, plan benefit design and geography. As the composition of our membership base changes, due to programmatic, competitive, regulatory, benefit design, economic or other changes, there is a corresponding change to our premium revenue, costs and margins, which could have a material adverse effect on our business, financial condition, cash flows and results of operations.
Additional factors that could affect our ability to sell products and services include, but are not limited to:
| ● | price, performance and functionality of our solution; |
| ● | availability, price, performance and functionality of competing solutions; |
| ● | our ability to develop and sell complementary services; |
| ● | stability, performance and security of our hosting infrastructure and hosting services; and |
| ● | changes in healthcare laws, regulations or trends. |
Any of these consequences could lower retention rate and have a material adverse effect on our business, financial condition and results of operations.
If the estimates and assumptions we use to project the size, revenue or medical expense amounts of our target geographies are inaccurate or the cost of providing services exceeds the amounts received by us, our future growth prospects may be impacted, and we may generate losses or fail to attain financial performance targets.
We often do not have access to reliable historical data regarding the size, revenue or medical expense levels of our target geographies or potential physician partners. As a result, our market opportunity estimates and financial forecasts developed as we enter into a new geography, are subject to significant uncertainty, and are based on assumptions and estimates that may not prove to be accurate. The estimates and forecasts in this Form 10-K relating to the size and expected growth of the market for our services and the estimates of our market opportunity may prove to be inaccurate.
Principal assumptions relating to our market opportunity include estimates of the total number and average length of relationships between MA patients and their physicians, historical MA patient growth rates, amount of revenue and medical expenses associated with MA members expected to be attributed to our affiliated professional entities and other physician partners and historical experience that such physician partners have with a similar platform. Our opportunity is based on the assumption that our platform, partnership and network model will be more attractive to potential physician partners than competing options. However, potential physician partners may elect to pursue a different strategic option.
Changes in our anticipated ratio of medical expense to revenue can significantly impact our financial results. Accordingly, the failure to adequately predict and control medical costs and expenses could have a material adverse effect on our business, results of operations, financial condition and cash flows. Additionally, the medical expenses of patients may be outside of our affiliated providers’ control in the event that patients take certain actions that increase such expenses, such as unnecessary hospital visits. If we
24
underestimate or do not correctly predict the cost of the care our affiliated providers furnish to patients, we might be underpaid for the care that must be provided to patients, which could have a negative impact on our results of operations and financial condition.
We primarily depend on reimbursement by third-party payors, as well as payments by individuals, which could lead to delays, uncertainties and disagreements regarding the timing and process of reimbursement, including any changes or reductions in Medicare reimbursement rates or rules.
The reimbursement process is complex and can involve lengthy delays. Although we recognize revenue when we provide services to patients, we may from time to time experience delays in receiving the associated capitation payments or, for patients on fee-for-service arrangements, the reimbursement for the service provided. In addition, third-party payors may disallow, in whole or in part, requests for reimbursement based on determinations that the patient is not eligible for coverage, certain amounts are not reimbursable under plan coverage, were for services provided that were not medically necessary, or additional supporting documentation is necessary. Third-party payors are also increasingly focused on controlling healthcare costs, and such efforts, including any revisions to reimbursement policies, may further reduce, complicate or delay our reimbursement claims. Further, the Medicare program and its reimbursement rates and rules, upon which many third-party payors base their reimbursement rate, are subject to frequent change. Retroactive adjustments may change amounts realized from third-party payors. As described below, we are subject to audits by such payors, including governmental audits of our Medicare claims, and may be required to repay these payors if a finding is made that we were incorrectly reimbursed. Delays, uncertainties and disagreements regarding the reimbursement process may adversely affect accounts receivable, increase the overall costs of collection and cause us to incur additional borrowing and other costs related to resolving disagreements or uncertainties. For example, in July 2021, a discrepancy was identified in the service agreement with one of our health plans in the way the revenue of Medicare Part C and Medicare Part D was being calculated compared to the definitions of “revenue” under the service agreement. This discrepancy resulted in a contract dispute and a renegotiation of the service agreement. We have determined it is probable that resolution of this discrepancy will result in an additional payment to the health plan of approximately $10.6 million. This contingent liability is recorded in health plan settlements payable in the Company’s consolidated balance sheets presented in this Form 10-K. See Note 21 “Commitments and Contingencies” to the consolidated financial statements included elsewhere in this Form 10-K for additional information on the impact of this discrepancy.
In addition, certain of our patients are covered under health plans that require the patient to cover a portion of their own healthcare expenses through the payment of copayments or deductibles. We may not be able to collect the full amounts due with respect to these payments that are the patient’s financial responsibility, or in those instances where physicians provide services to uninsured individuals. To the extent permitted by law, amounts not covered by third-party payors are the obligations of individual patients for which we may not receive whole or partial payment. Any increase in cost shifting from third-party payors to individual patients, including as a result of high deductible plans for patients, increases our collection costs and reduces overall collections, which we may not be able to offset with sufficient revenue.
In response to the COVID-19 pandemic, the CMS, the federal agency responsible for administering the Medicare program, made several changes in the manner in which Medicare will pay for telehealth visits, many of which relax previous requirements, including site requirements for both the providers and patients, telehealth modality requirements and others. State law applicable to telehealth, particularly licensure requirements, has also been relaxed in many jurisdictions as a result of the COVID-19 pandemic. It is unclear which, if any, of these changes will remain in place permanently and which will be rolled-back following the COVID-19 pandemic. If regulations change to restrict our ability to or prohibit us from delivering care through telehealth modalities, our financial condition and results of operations may be adversely affected.
The termination or non-renewal of the Medicare Advantage contracts held by the health plans with which we contract, or the termination or nonrenewal of our contracts with those plans, could have a material adverse effect on our revenue and operations.
We contract with health plans to provide capitated care services with respect to certain of their MA members. Our operations are dependent on a concentrated number of payors with whom we contract to provide services to members. Our contracts with four health plans to provide capitated care services for their members collectively accounted for approximately 79% and 67% of our capitated revenue for the years ended December 31, 2021 and 2022, respectively. If a plan with which we contract for these services loses its MA contracts with CMS, receives reduced or insufficient government reimbursement under the MA program, decides to discontinue its MA and/or commercial plans, decides to contract with another company to provide capitated care services to its members, or decides to directly provide care, our contract with that plan could be at risk and we could lose revenue. In addition,
25
certain of our contracts with health plans are terminable without cause. If any of these contracts were terminated, certain patients covered by such plans may choose to shift to another PCP within their health plan’s network. Moreover, our inability to maintain our agreements with health plans, in particular with key payors such as Centene Corporation, Atrio Health Plans, United Healthcare and Aetna, with respect to their MA members or to negotiate favorable terms for those agreements in the future, could result in the loss of patients and could have a material adverse effect on our profitability and business.
The healthcare industry has also experienced a trend of consolidation, resulting in fewer but larger payors that have significant bargaining power, given their market share. Payments from payors are the result of negotiated rates. These rates may decline based on renegotiations and larger payors having significant bargaining power to negotiate higher discounted fee arrangements with healthcare providers. As a result, payors increasingly are demanding discounted fee structures or the assumption by healthcare providers of all or a portion of the financial risk related to paying for care provided through capitation agreements.
If any of our affiliated professional entities or other physician partners lose their regulatory licenses, permits and/or accreditation status, or become ineligible to receive reimbursement under Medicare or Medicaid or other third-party payors, there may be a material adverse effect on our business, financial condition, cash flows, or results of operations.
The operations of our managed clinics through our affiliated professional entities or other physician partners are subject to extensive federal, state and local regulation relating to, among other things, the adequacy of medical care, equipment, personnel, operating policies and procedures, fire prevention, rate-setting and compliance with building codes and environmental protection. Our managed clinics and affiliated professional entities are also subject to extensive laws and regulation relating to facility and professional licensure, conduct of operations, including financial relationships among healthcare providers, Medicare and Medicaid fraud and abuse and physician self-referrals, and maintaining updates to our affiliated professional entities’ enrollment in the Medicare and Medicaid programs, including the addition of new clinic locations, providers and other enrollment information. Our managed clinics and affiliated professional entities are subject to periodic inspection by licensing authorities and accreditation organizations to assure their continued compliance with these various standards. There can be no assurance that these regulatory authorities will determine that all applicable requirements are fully met at any given time. Should any of our managed clinics or affiliated professional entities be found to be noncompliant with these requirements, we could be assessed fines and penalties, could be required to refund reimbursement amounts or could lose our licensure or Medicare and/or Medicaid certification or accreditation so that we or affiliated professional entities are unable to receive reimbursement from such programs and possibly from other third-party payors, any of which could materially adversely affect our business, financial condition, cash flows or results of operations.
We are dependent on our affiliated professional entities and other physician partners and other providers to effectively manage the quality and cost of care and perform obligations under payor contracts.
Our success depends upon our continued ability to collaborate with and expand a network of high-caliber affiliated professional entities and other physician partners who can provide high quality of care, improve clinical outcomes and effectively manage healthcare costs, which are key drivers of our profitability. Our physician partners could demand an increased payment arrangement or take other actions, or fail to take actions, that could result in higher medical costs, lower quality of care for our members, harm to our reputation or create difficulty meeting regulatory or other requirements. Likewise, our physician partners could take actions contrary to our instructions, requests, policies or objectives or applicable law, or could have economic or business interests or goals that are or become inconsistent with our own. Further, our physician partners may not engage with our platform to assist in improving overall quality of care and management of healthcare costs, which could produce results that are inconsistent with our estimates and financial models and negatively impact our growth.
In addition to receiving care from our affiliated professional entities and other physician partners, our members also receive care from an array of hospitals, specialists and ancillary providers who typically contract directly with our payors. We cannot guarantee the quality and efficiency of services from such providers, over which we have no control. Members who receive sub-optimal healthcare from such providers may be dissatisfied with our physician partners, which would have a negative impact on member satisfaction and retention. Any of these consequences could adversely impact our business, financial condition and results of operations.
We could also experience significant losses if the expenses incurred to deliver healthcare services to our attributed members exceed revenue we receive from payors in respect of our attributed members. Under a capitation contract, a payor typically prospectively pays periodic capitation payments representing a prospective budget from which its physician partnerships manage
26
healthcare expenses on behalf of the population enrolled with that physician partnership. To manage total medical services expense, we rely on our affiliated professional entities’ and other physician partners’ ability to improve clinical outcomes, implement clinical initiatives to provide a better healthcare experience for our members and accurately and sufficiently document the risk profile of our members. While our contracts vary, generally, if the cost of medical care provided exceeds the corresponding capitation revenue we receive, we may realize operating deficits, which are typically not capped, and could lead to substantial losses.
Reductions in the quality ratings of the health plans we serve could have a material adverse effect on our business, results of operations, financial condition and cash flows.
As a result of the Affordable Care Act, as amended by the Health Care and Education Reconciliation Act (the “ACA”), the level of reimbursement each health plan receives from CMS is dependent, in part, upon the quality rating of the MA plan. Such ratings impact the percentage of any cost savings rebate and any bonuses earned by such health plan. Since a significant portion of our revenue is expected to be calculated as a percentage of CMS reimbursement received by these health plans with respect to our patients, reductions in the quality ratings of a health plan that we serve could have a material adverse effect on our business, results of operations, financial condition and cash flows.
Given each health plan’s control of its plans and the many other providers that serve such plans, we believe that we will have limited ability to influence the overall quality rating of any such plan. The Bipartisan Budget Act, passed in February 2018, implemented certain changes to prevent artificial inflation of star ratings for MA plans offered by the same organization. In addition, CMS has terminated plans that have had a rating of less than three stars for three consecutive years, whereas MA plans with five stars are permitted to conduct enrollment throughout almost the entire year. Because low quality ratings can potentially lead to the termination of a plan that we serve, we may not be able to prevent the potential termination of a contracting plan or a shift of patients to other plans based upon quality issues which could, in turn, have a material adverse effect on our business, results of operations, financial condition and cash flows.
We operate in a competitive industry, and if we are not able to compete effectively, our business, financial condition and results of operations will be harmed.
Our industry is competitive and we expect it to attract increased competition, which could make it difficult for us to succeed. We currently face competition in various aspects of our business, including in offering a favorable reimbursement structure for physician partners and potential physician partners and attracting payors and physician partners who are not contracted with us, from a range of companies that provide similar services under different care models that could attract patients, providers and payors, including hospitals, managed service organizations and provider networks and data analysis consultants. Further, individual physicians who are contracted within our network may affiliate with our competitors. Competition from hospitals, managed service organizations and provider networks and data analysis consultants, payors and other parties could result in payors changing the benefit structure that is offered to our members, which could negatively impact our profitability and market share.
Our primary competitors include Oak Street Health, Inc., Cano Health, Inc. and agilon health, inc., in addition to numerous local provider networks, hospitals and health systems. Moreover, large, well-financed payors have in some cases developed their own managed services tools and may provide these services to their physicians and patients at discounted prices, or may seek to expand their relationships with additional competing physicians or physician networks, including in geographic areas we serve. This may result in a more competitive environment and increased challenges to grow at the rates we have projected. We expect that competition will continue to increase as a result of consolidation in the healthcare industry and increased demand for its services.
Some of our competitors may have greater name recognition, particularly in local geographies, longer operating histories, superior products or services and significantly greater resources than we do. Further, our current or potential competitors may be acquired by or partner with third parties with greater resources than we have. As a result, our competitors may be able to respond more quickly and effectively than we can to new or changing opportunities, technologies, standards or customer requirements and may have the ability to initiate or withstand substantial benefits structure and premium competition. In addition, current and potential competitors have established, and may in the future establish, cooperative relationships with providers of complementary services, technologies or services to increase the attractiveness of their services.
Accordingly, new competitors or alliances may emerge that have greater market share, a larger customer base, better data aggregation systems, greater marketing expertise, greater financial resources and larger marketing teams than we have, which could
27
put us at a competitive disadvantage. Our competitors could also be better positioned to serve certain segments of the healthcare delivery industry, which could create additional pressure on the premiums that our payors are able to charge. If we are unable to successfully compete, our business, financial condition, cash flows and results of operations could be materially adversely affected.
Our future growth and the profitability of our business will depend in large part upon the effectiveness and efficiency of our marketing efforts, and our ability to develop brand awareness cost-effectively.
Our business success depends on our ability to attract and retain members, which significantly depends on our marketing practices. Our future growth and profitability will depend in large part upon the effectiveness and efficiency of our marketing efforts, including our ability to:
| ● | create greater awareness of our brand; |
| ● | identify the most effective and efficient levels of spending in each market, media and specific media vehicle; |
| ● | determine the appropriate creative messages and media mix for advertising, marketing and promotional expenditures; |
| ● | effectively manage marketing costs (including creative and media) to maintain acceptable consumer acquisition costs; |
| ● | select the most effective markets, media and specific media vehicles in which to advertise; and |
| ● | convert consumer inquiries into clients and members. |
We believe that developing and maintaining widespread awareness of our brand in a cost-effective manner is critical to achieving widespread adoption of our services and attracting new clients and members. Our brand promotion activities may not generate consumer awareness or increase revenue, and even if they do, any increase in revenue may not offset the expenses we incur in building our brand. If we fail to successfully promote and maintain our brand, or incur substantial expenses in doing so, we may fail to attract or retain members necessary to realize a sufficient return on our brand-building efforts or to achieve the widespread brand awareness that is critical for broad adoption of our brands.
Developments affecting spending by the healthcare industry could adversely affect our business.
The U.S. healthcare industry has changed significantly in recent years, and we expect that significant changes will continue to occur. General reductions in expenditures by healthcare industry participants could result from, among other things:
| ● | government regulations or private initiatives that affect the manner in which healthcare providers interact with patients, payors or other healthcare industry participants, including changes in pricing or means of delivery of healthcare products and services; |
| ● | consolidation of healthcare industry participants; |
| ● | reductions in government funding for healthcare; and |
| ● | adverse changes in business or economic conditions affecting healthcare payors or providers or other healthcare industry participants. |
Any of these changes in healthcare spending could adversely affect our revenue. Even if general expenditures by industry participants remain the same or increase, developments in the healthcare industry may result in reduced spending in some or all of the specific markets that we serve now or in the future. However, the timing and impact of developments in the healthcare industry are difficult to predict. We cannot assure you that the demand for our solutions and services will continue to exist at current levels or that we will have adequate technical, financial, and marketing resources to react to changes in the healthcare industry.
28
We and our affiliated professional entities and other physician partners may become subject to medical liability claims, which could cause us to incur significant expenses and may require us to pay significant damages if the claims are not covered by insurance.
Our overall business entails the risk of medical liability claims. Although we and our affiliated professionals carry insurance covering medical malpractice claims in amounts that we believe are appropriate in light of the risks attendant to the services rendered, successful medical liability claims could result in substantial damage awards that exceed the limits of our and those affiliated professionals’ insurance coverage. We carry or will carry professional liability insurance for the Company and each of our healthcare professionals. Additionally, all of the network providers that contract or will contract with us separately carry or will carry professional liability insurance for themselves and their healthcare professionals. Professional liability insurance is expensive and insurance premiums may increase significantly in the future, particularly as we expand our services. As a result, adequate professional liability insurance may not be available to us and our affiliated professionals in the future at acceptable costs or at all, which may negatively impact our and our affiliated professionals’ ability to provide services to members, and thereby adversely affect our overall business and operations.
Any claims made against us or our affiliated professionals that are not fully covered by insurance could be costly to defend against, result in substantial damage awards, and divert the attention of our management and our affiliated professional entities from our operations, which could have a material adverse effect on our business, financial condition and results of operations. In addition, any claims may adversely affect our business or reputation.
If we or our affiliated professional entities or other physician partners fail to comply with applicable data interoperability and information blocking rules, our consolidated results of operations could be adversely affected.
The 21st Century Cures Act (the “Cures Act”), which was passed and signed into law in December 2016, includes provisions related to data interoperability, information blocking and patient access. In March 2020, the HHS, Office of the National Coordinator for Health Information Technology, (“ONC”), and CMS finalized and issued complementary rules that are intended to clarify provisions of the Cures Act regarding interoperability and information blocking, and include, among other things, requirements surrounding information blocking, changes to ONC’s health IT certification program and requirements that CMS regulated payors make relevant claims/care data and provider directory information available through standardized patient access and provider directory application programming interfaces that connect to provider electronic health record systems. The companion rules will transform the way in which healthcare providers, health IT developers, health information exchanges/health information networks (“HIEs/HINs”), and health plans share patient information, and create significant new requirements for healthcare industry participants. For example, the ONC rule, which went into effect on April 5, 2021, prohibits healthcare providers, health IT developers of certified health IT, and HIEs/HINs from engaging in practices that are likely to interfere with, prevent, materially discourage, or otherwise inhibit the access, exchange or use of electronic health information (“EHI”), also known as “information blocking.” To further support access and exchange of EHI, the ONC rule identifies eight “reasonable and necessary activities” as exceptions to information blocking activities, as long as specific conditions are met. Any failure to comply with these rules could have a material adverse effect on our business, results of operations and financial condition.
Our business and operations would suffer in the event of information technology system failures, security breaches, cyberattacks or other deficiencies in cybersecurity.
Our information technology systems facilitate our ability to conduct our business. While we have disaster recovery systems and business continuity plans in place, any disruptions in our disaster recovery systems or the failure of these systems to operate as expected could, depending on the magnitude of the problem, adversely affect our operating results by limiting our capacity to effectively monitor and control our operations. Despite our implementation of a variety of security measures, our information technology systems could be subject to physical or electronic break-ins, and similar disruptions from unauthorized tampering or any weather-related disruptions where our headquarters is located. In addition, in the event that a significant number of our management personnel were unavailable in the event of a disaster, our ability to effectively conduct business could be adversely affected.
In the ordinary course of our business, we, our affiliated professional entities or other physician partners collect and store sensitive data, including personally identifiable information, protected health information (“PHI”), intellectual property and proprietary business information owned or controlled by us or our employees, members and other parties. We manage and maintain our applications and data utilizing a combination of on-site systems and cloud-based data centers. We utilize external security and
29
infrastructure vendors to provide and manage parts of our information technology systems, including our data centers. These applications and data encompass a wide variety of business-critical information, including research and development information, customer information, commercial information and business and financial information. We face a number of risks with respect to the protection of this information, including loss of access, inappropriate use or disclosure, unauthorized access, inappropriate modification and the risk of being unable to adequately monitor and audit and modify our controls over our critical information. This risk extends to the third-party vendors and subcontractors we use to manage this sensitive data or otherwise process it on our behalf. A breach or failure of our or our third-party vendors’ or subcontractors’ network, hosted service providers or vendor systems could result from a variety of circumstances and events, including third-party action, employee negligence or error, malfeasance, malware (e.g., ransomware), computer viruses, cyberattacks by computer hackers such as denial-of-service and phishing attacks, failures during the process of upgrading or replacing software and databases, power outages, hardware failures, telecommunication failures, user errors, or catastrophic events. If these third-party vendors or subcontractors fail to protect their information technology systems and our confidential and proprietary information, we may be vulnerable to disruptions in service and unauthorized access to our confidential or proprietary information and we could incur liability and reputational damage.
The secure processing, storage, maintenance and transmission of information are vital to our operations and business strategy, and we devote significant resources to protecting such information. Although we take reasonable measures to protect sensitive data from unauthorized access, use or disclosure, our information technology and infrastructure may still be vulnerable to, and we have in the past experienced, low-threat attacks by hackers or breaches due to employee error, malfeasance or other malicious or inadvertent disruptions. Further, attacks upon information technology systems are increasing in their frequency, levels of persistence, sophistication and intensity, and are being conducted by sophisticated and organized groups and individuals with a wide range of motives and expertise. Furthermore, because the techniques used to obtain unauthorized access to, or to sabotage, systems change frequently and often are not recognized until launched against a target, we may be unable to anticipate these techniques or implement adequate preventative measures. We may also experience security breaches that may remain undetected for an extended period. Any such breach or interruption could compromise our networks and the information stored there could be accessed by unauthorized parties, publicly disclosed, lost or stolen. Our information systems must also be continually updated, patched and upgraded to protect against known vulnerabilities. The volume of new vulnerabilities has increased markedly, as has the criticality of patches and other remedial measures. In addition to remediating newly identified vulnerabilities, previously identified vulnerabilities must also be continuously addressed. Accordingly, we are at risk that cyberattackers exploit these known vulnerabilities before they have been addressed.
We and certain of our service providers are from time to time subject to cyberattacks and security incidents. While we do not believe that we have experienced any significant system failure, accident or security breach to date, if such an event were to occur and cause interruptions in our operations, it could result in legal claims or proceedings, and liability under federal or state laws that protect the privacy of personal information, and corresponding regulatory penalties. In addition, we could face criminal liability, damages for contract breach and incur significant costs for remedial measures to prevent future occurrences and mitigate past violations. Notice of breaches may be required to be made to affected individuals or other state or federal regulators, and for extensive breaches, notice may need to be made to the media or State Attorneys General. Such a notice could harm our reputation and our ability to compete. Although we maintain insurance covering certain security and privacy damages and claim expenses, we may not carry insurance or maintain coverage sufficient to compensate for all liability and in any event, insurance coverage would not address the reputational damage that could result from a security incident. Despite our implementation of security measures to prevent unauthorized access, our data is currently accessible through multiple channels, and there is no guarantee we can protect our data from breach. Unauthorized access, loss or dissemination could also disrupt our operations and damage our reputation, any of which could adversely affect our business.
Actual or perceived failures to comply with applicable data protection, privacy and security laws, regulations, standards and other requirements could adversely affect our business, financial condition and results of operations.
Numerous state and federal laws, regulations, standards and other legal obligations, including consumer protection laws and regulations, which govern the collection, dissemination, use, access to, confidentiality, security and processing of personal information, including health-related information, could apply to our operations or the operations of our partners. For example, HIPAA, as amended by the Health Information Technology for Economic and Clinical Health Act of 2009, and regulations implemented thereunder (collectively, “HIPAA”), imposes privacy, security and breach notification obligations on certain healthcare providers, health plans, and healthcare clearinghouses, known as covered entities, as well as their business associates that perform certain services that involve creating, receiving, maintaining or transmitting individually identifiable health information for or on
30
behalf of such covered entities, and their covered subcontractors. HIPAA requires covered entities, such as the affiliated professional entities or other physician partners, and business associates, such as us, to develop and maintain policies with respect to the protection of, use and disclosure of PHI, including the adoption of administrative, physical and technical safeguards to protect such information, and certain notification requirements in the event of a breach of unsecured PHI.
Additionally, under HIPAA, covered entities must report breaches of unsecured PHI to affected individuals without unreasonable delay, not to exceed 60 days following discovery of the breach by a covered entity or its agents. Notification also must be made to the HHS Office for Civil Rights and, in certain circumstances involving large breaches, to the media. Business associates must report breaches of unsecured PHI to covered entities within 60 days of discovery of the breach by the business associate or its agents. A non-permitted use or disclosure of PHI is presumed to be a breach under HIPAA unless the covered entity or business associate establishes that there is a low probability the information has been compromised consistent with requirements enumerated in HIPAA.
Entities that are found to be in violation of HIPAA as the result of a breach of unsecured PHI, a complaint about privacy practices or an audit by HHS may be subject to significant civil, criminal and administrative fines and penalties and/or additional reporting and oversight obligations if required to enter into a resolution agreement and corrective action plan with HHS to settle allegations of HIPAA non-compliance. HIPAA also authorizes state Attorneys General to file suit on behalf of their residents. Courts may award damages, costs and attorneys’ fees related to violations of HIPAA in such cases. While HIPAA does not create a private right of action allowing individuals to sue us in civil court for violations of HIPAA, its standards have been used as the basis for duty of care in state civil suits such as those for negligence or recklessness in the misuse or breach of PHI.
Even when HIPAA does not apply, according to the Federal Trade Commission (the “FTC”), violating consumers’ privacy rights or failing to take appropriate steps to keep consumers’ personal information secure may constitute unfair and/or deceptive acts or practices in violation of Section 5(a) of the Federal Trade Commission Act. The FTC expects a company’s data security measures to be reasonable and appropriate in light of the sensitivity and volume of consumer information it holds, the size and complexity of its business, and the cost of available tools to improve security and reduce vulnerabilities.
Further, certain states have also adopted comparable privacy and security laws and regulations which govern the privacy, processing and protection of health-related and other personal information. Such laws and regulations will be subject to interpretation by various courts and other governmental authorities, thus creating potentially complex compliance issues for us and our future customers and strategic partners. For example, the state of Nevada enacted a law that went into force on October 1, 2019 and requires companies to honor consumers’ requests to no longer sell their data. In addition, the California Consumer Privacy Act of 2018 (the “CCPA”) went into effect on January 1, 2020. The CCPA creates individual privacy rights for California consumers and increases the privacy and security obligations of entities handling certain personal information. The CCPA provides for civil penalties for violations, as well as a private right of action for data breaches that has increased the likelihood of, and risks associated with, data breach litigation. The CCPA has increased our compliance costs and potential liability, and similar laws have passed in Virginia, Colorado, Connecticut and Utah and have been proposed at the federal level and in other states, reflecting a trend toward more stringent privacy legislation in the United States. The enactment of such laws could have potentially conflicting requirements that would make compliance challenging. Further, the California Privacy Rights Act (the “CPRA”) generally went into effect on January 1, 2023, and significantly amends the CCPA. The CPRA imposes additional data protection obligations on covered businesses, including additional consumer rights processes, limitations on data uses, new audit requirements for higher risk data, and opt outs for certain uses of sensitive data. It also created a new California data protection agency authorized to issue substantive regulations and could result in increased privacy and information security enforcement. Additional compliance investment and potential business process changes may also be required. In addition, California’s Confidentiality of Medical Information Act (the “CMIA”) places restrictions on the use and disclosure of health information, including PHI, and other personally identifying information, and can impose a significant compliance obligation. Violations of the CMIA can result in criminal, civil and administrative sanctions, and the CMIA also provides individuals a private right of action with respect to disclosures of their health information that violate CMIA. In the event that we are subject to or affected by HIPAA, the CCPA, the CPRA or other domestic privacy and data protection laws, any liability from failure to comply with the requirements of these laws could adversely affect our financial condition.
Although we work to comply with applicable laws, regulations and standards, our contractual obligations and other legal obligations, these requirements are evolving and may be modified, interpreted and applied in an inconsistent manner from one jurisdiction to another, and may conflict with one another or other legal obligations with which we must comply. Any failure or perceived failure by us or our employees, representatives, contractors, consultants, collaborators, or other third parties to comply with
31
such requirements or adequately address privacy and security concerns, even if unfounded, could result in additional cost and liability to us, damage our reputation, and adversely affect our business and results of operations.
Legal proceedings in connection with the Business Combinations, the outcome of which is uncertain, could draw the attention of our management team away from the operation of our business.
Prior to execution of the definitive agreements for the Business Combinations, Hudson Vegas Investment SPV, LLC, (“Hudson”), one of our existing equity holders, asserted that it had an option to purchase additional equity interests in P3 Health Group Holdings, LLC (“Legacy P3”) in connection with the pending transaction with Foresight (the “Purchase Option”). We do not agree that the Purchase Option applies to the Business Combinations. On June 11, 2021, Hudson filed an action in the Delaware Court of Chancery (the “Hudson Action”), in which it challenged the Business Combinations. Specifically, Hudson purports to assert claims against Legacy P3, the members of the Legacy P3 Board of Managers, certain of the Legacy P3 officers and Chicago Pacific Founders Fund, L.P. (“CPF”), for breach of the Third Amended and Restated Limited Liability Company Agreement of Legacy P3, dated as of April 16, 2020 (the “Legacy P3 LLC Agreement”), (against Legacy P3 and CPF), breach of fiduciary duty (against certain of Legacy P3’s officers) and breach of alleged contractual standards of conduct (against the Legacy P3 Board of Managers) in connection with the process leading up to, and approval of, the Business Combinations. In the Hudson Action, Hudson sought to enjoin the consummation of the Business Combinations, and seeks a declaration that the Business Combinations violate its rights under the Legacy P3 LLC Agreement, a declaration that the members of the Legacy P3 Board of Managers and certain of Legacy P3’s officers breached their fiduciary duties, and money damages including attorneys’ fees.
See “Item 3. Legal Proceedings” for a description of the Hudson Class D Dispute proceedings.
Defending or settling this lawsuit could draw the attention of our management team away from the operation of our business and while we are indemnified by the P3 Equityholders for costs in connection with this lawsuit, it is possible that we could nonetheless incur financial losses if disputes arise with respect to the extent of the indemnification obligations.
Any future litigation against us could be costly and time-consuming to defend.
We may become subject, from time to time, to legal proceedings, federal and state audits, government investigations, and payor audits, investigations, overpayments, and claims that arise in the ordinary course of business such as claims brought by our clients in connection with commercial disputes or employment claims made by our current or former associates. Litigation and audits may result in substantial costs and may divert management’s attention and resources, which may substantially harm our business, financial condition and results of operations. Insurance may not cover such claims, may not provide sufficient payments to cover all of the costs to resolve one or more such claims and may not continue to be available on terms acceptable to us. A claim brought against us that is uninsured or underinsured could result in unanticipated costs, thereby reducing our earnings and leading analysts or potential investors to reduce their expectations of our performance, which could reduce the market price of our Class A common stock or publicly traded warrants.
Changes in U.S. tax laws, and the adoption of tax reform policies or changes in tax legislation or policies in jurisdictions outside of the United States, could adversely affect our operating results and financial condition.
We are subject to federal and state income and non-income taxes in the United States. Tax laws, regulations, and administrative practices in various jurisdictions may be subject to significant change, with or without notice, due to economic, political, and other conditions, and significant judgment is required in evaluating and estimating these taxes. For example, legislation commonly known as the Inflation Reduction Act (“IRA”), was signed into law on August 16, 2022. Among other things, the IRA includes a 1% excise tax on corporate stock repurchases, applicable to repurchases after December 31, 2022. We are in the process of evaluating the potential impacts of the IRA to us.
Our effective tax rates could be affected by numerous factors, such as entry into new businesses and geographies, changes to our existing business and operations, acquisitions and investments and how they are financed, changes in our stock price, changes in our deferred tax assets and liabilities and their valuation, and changes in the relevant tax, accounting, and other laws, regulations, administrative practices, principles and interpretations. We are required to take positions regarding the interpretation of complex statutory and regulatory tax rules and on valuation matters that are subject to uncertainty, and tax authorities may challenge the positions that we take.
32
Our quarterly results may fluctuate significantly, which could adversely impact the value of our Class A common stock and publicly traded warrants.
Our quarterly results of operations, including our revenue, net loss and cash flows, has varied and may vary significantly in the future, and period-to-period comparisons of our results of operations may not be meaningful. Accordingly, our quarterly results should not be relied upon as an indication of future performance. Our quarterly financial results may fluctuate as a result of a variety of factors, many of which are outside of our control, including, without limitation, the following:
| ● | our ability to maintain and grow the number of members on our platform; |
| ● | the demand for and types of services that are offered on our platform by providers; |
| ● | the timing of recognition of revenue, including possible delays in the recognition of revenue due to sometimes unpredictable implementation timelines; |
| ● | the amount and timing of operating expenses related to the maintenance and expansion of our business, operations and infrastructure; |
| ● | our ability to effectively manage the size and composition of our network of healthcare providers relative to the level of demand for services from our members and our clients’ members and patients; |
| ● | our ability to respond to competitive developments, including pricing changes and the introduction of new products and services by our competitors; |
| ● | client and member renewal rates and the timing and terms of client and member renewals; |
| ● | changes to our pricing model; |
| ● | our ability to introduce new features and services and enhance our existing platform and our ability to generate significant revenue from new features and services; |
| ● | the impact of outages of our platform and associated reputational harm; |
| ● | security or data privacy breaches and associated remediation costs; |
| ● | the timing of expenses related to the development or acquisition of technologies or businesses; and |
| ● | the COVID-19 pandemic or other pandemics. |
Any fluctuation in our quarterly results may not accurately reflect the underlying performance of our business and could cause a decline in the trading price of our Class A common stock and publicly traded warrants.
Our only significant asset is the ownership of a minority of the economic interest in P3 LLC, and such ownership may not be sufficient to generate the funds necessary to meet our financial obligations or to pay any dividends on our Class A common stock.
We have no direct operations and no significant assets other than the ownership of a minority of the economic interests in P3 LLC. As of December 31, 2022, we owned approximately 17.1% of the economic interests in P3 LLC. We depend on P3 LLC and its subsidiaries for distributions, loans and other payments to generate the funds necessary to meet our financial obligations, including to satisfy our obligations under the Tax Receivable Agreement, or to pay any dividends with respect to our Class A Common Stock. Legal and contractual restrictions in agreements governing the indebtedness of P3 LLC and its subsidiaries may limit our ability to obtain cash from P3 LLC. The earnings from, or other available assets of, P3 LLC and its subsidiaries may not be sufficient to enable us to satisfy our financial obligations, including our obligations under the Tax Receivable Agreement, or pay any dividends on our Class A common stock should we decide to do so. P3 LLC will be classified as a partnership for U.S. federal income tax purposes and,
33
as such, will generally not be subject to entity level U.S. federal income tax. Instead, taxable income will be allocated to holders of P3 LLC units, including us. As a result, we generally will incur taxes on our allocable share of any net taxable income generated by P3 LLC. Under the terms of the P3 LLC Amended and Restated Limited Liability Agreement (the “P3 LLC A&R LLC Agreement”), and the Tax Receivable Agreement, P3 LLC will be obligated to make tax distributions or payments to holders of its P3 LLC units, including us, except to the extent such distributions or payments would render P3 LLC insolvent or are otherwise prohibited by law or the terms of any credit facility. In addition to our tax payment obligations, we will also incur expenses related to our operations and our interests in P3 LLC, including costs and expenses of being a publicly traded company, all of which could be significant. To the extent that we require funds and P3 LLC or its subsidiaries are restricted from making distributions under applicable law or regulation or under the terms of their financing arrangements, or are otherwise unable to provide such funds, it could materially adversely affect our liquidity and financial condition, including our ability to pay our income taxes when due.
Risks Related to Our Legal and Regulatory Environment
We conduct business in a heavily regulated industry and if we fail to adhere to all of the complex government laws and regulations that apply to our business, we could incur fines or penalties or be required to make changes to our operations or experience adverse publicity, any or all of which could have a material adverse effect on our business, results of operations, financial condition, cash flows, and reputation.
The U.S. healthcare industry is heavily regulated and closely scrutinized by federal, state and local governments. Comprehensive statutes and regulations govern the manner in which we provide and bill for services and collect reimbursement from governmental programs and private payors, our contractual relationships and arrangements with healthcare providers and vendors, our marketing activities and other aspects of our operations. Of particular importance are:
| ● | the federal Anti-Kickback Statute (the “AKS”), which prohibits the knowing and willful offer, payment, solicitation or receipt of any bribe, kickback, rebate or other remuneration for referring an individual, in return for ordering, leasing, purchasing or recommending or arranging for or to induce the referral of an individual or the ordering, purchasing or leasing of items or services covered, in whole or in part, by any federal healthcare program, such as Medicare and Medicaid. Although there are several statutory exceptions and regulatory safe harbors protecting certain common activities from prosecution, the exceptions and safe harbors are drawn narrowly. By way of example, the AKS safe harbor for value-based arrangements requires, among other things, that the arrangement does not induce a person or entity to reduce or limit medically necessary items or services furnished to any patient. Failure to meet the requirements of a safe harbor, however, does not render an arrangement illegal, although such arrangements may be subject to greater scrutiny by government authorities. Further, a person or entity does not need to have actual knowledge of the statute or specific intent to violate it to have committed a violation; |
| ● | the federal physician self-referral law (the “Stark Law”), which, subject to limited exceptions, prohibits physicians from referring Medicare or Medicaid patients to an entity for the provision of certain designated health services (“DHS”), if the physician or a member of such physician’s immediate family has a direct or indirect financial relationship (including an ownership interest or a compensation arrangement) with the entity, and prohibits the entity from billing Medicare or Medicaid for such DHS. Unlike the AKS, the Stark Law is violated if the financial arrangement does not meet an applicable exception, regardless of any intent by the parties to induce or reward referrals or the reasons for the financial relationship and the referral; |
| ● | the federal False Claims Act (the “FCA”), which imposes civil and criminal liability on individuals or entities that knowingly submit false or fraudulent claims for payment to the government or knowingly make, or cause to be made, a false statement in order to have a false claim paid, including qui tam or whistleblower suits. There are many potential bases for liability under the FCA. The government has used the FCA to prosecute Medicare and other government healthcare program fraud; including alleged upcoding or improper coding of diagnosis codes under the risk-adjustment methodology, billing for services not provided, and providing care that is not medically necessary or that is substandard in quality. In addition, we could be held liable under the FCA if we are deemed to “cause” the submission of false or fraudulent claims by, for example, providing inaccurate billing, coding or risk adjustment information to our affiliated professional entities and other physician partners through Provider Portal and Analytic Management Tools, respectively. The government may also assert that a claim including items or services resulting from a violation of the AKS or Stark Law constitutes a false or fraudulent claim for purposes of the FCA; |
34
| ● | the Civil Monetary Penalties Statute, which prohibits, among other things, an individual or entity from offering remuneration to a federal healthcare program beneficiary that the individual or entity knows or should know is likely to influence the beneficiary to order or receive healthcare items or services from a particular provider; |
| ● | the criminal healthcare fraud provisions of HIPAA and related rules that prohibit knowingly and willfully executing a scheme or artifice to defraud any healthcare benefit program or falsifying, concealing or covering up a material fact or making any material false, fictitious or fraudulent statement in connection with the delivery of or payment for healthcare benefits, items or services. Similar to the AKS, a person or entity does not need to have actual knowledge of the statute or specific intent to violate it to have committed a violation; |
| ● | reassignment of payment rules that prohibit certain types of billing and collection practices in connection with claims payable by the Medicare or Medicaid programs; |
| ● | similar state law provisions pertaining to anti-kickback, self-referral and false claims issues, some of which may apply to items or services reimbursed by any payor, including patients and commercial insurers; |
| ● | laws that regulate debt collection practices; |
| ● | a provision of the Social Security Act that imposes criminal penalties on healthcare providers who fail to disclose, or refund known overpayments; |
| ● | federal and state laws that prohibit providers from billing and receiving payment from Medicare and Medicaid for services unless the services are medically necessary, adequately and accurately documented, and billed using codes that accurately reflect the type and level of services rendered; and |
| ● | federal and state laws pertaining to the provision of services by nurse practitioners and physician assistants in certain settings, physician supervision of those services, and reimbursement requirements that depend on the types of services provided and documented and relationships between physician supervisors and nurse practitioners and physician assistants. |
The laws and regulations in these areas are complex, changing and often subject to varying interpretations. As a result, there is no guarantee that a government authority will find that we or our affiliated professional entities or other physician partners are in compliance with all such laws and regulations that apply to our business. Further, because of the breadth of these laws and the narrowness of the statutory exceptions and safe harbors available, it is possible that some of the business activities undertaken by us or our affiliated professional entities or other physician partners could be subject to challenge under one or more of these laws, including, without limitation, our patient assistance programs that waive or reduce the patient’s obligation to pay copayments, coinsurance or deductible amounts owed for the services we provide to them if they meet certain financial need criteria. If our operations are found to be in violation of any of such laws or any other governmental regulations that apply, we may be subject to significant penalties, including, without limitation, administrative, civil and criminal penalties, damages, fines, disgorgement, the curtailment or restructuring of operations, integrity oversight and reporting obligations, exclusion from participation in federal and state healthcare programs and imprisonment. In addition, any action against us or our affiliated professional entities or other physician partners for violation of these laws or regulations, even if we successfully defend against it, could cause us to incur significant legal expenses, divert our management’s attention from the operation of our business and result in adverse publicity, or otherwise experience a material adverse impact on our business, results of operations, financial condition, cash flows, reputation as a result.
If any of our owned or managed clinics lose their regulatory licenses, permits and/or registrations, as applicable, or become ineligible to receive reimbursement under Medicare, Medicaid or other third-party payors, there may be a material adverse effect on our business, financial condition, cash flows, or results of operations.
The operations of our owned and managed clinics through affiliated professional entities and other physician partners are subject to extensive federal, state and local regulation relating to, among other things, the adequacy of medical care, equipment, personnel, operating policies and procedures and proof of financial ability to operate. Our owned and managed clinics and affiliated professional entities and other physician partners are also subject to extensive laws and regulation relating to facility and professional
35
licensure, conduct of operations, including financial relationships among healthcare providers, Medicare, Medicaid and state fraud and abuse and physician self-referrals, and maintaining updates to our and our affiliated professional entities’ and other physician partners’ enrollment in the Medicare and Medicaid programs, including addition of new clinic locations, providers and other enrollment information. Our owned and managed clinics are subject to periodic inspection by licensing authorities to assure their continued compliance with these various standards. There can be no assurance that these regulatory authorities will determine that all applicable requirements are fully met at any given time. Should any of our owned or managed clinics be found to be noncompliant with these requirements, we could be assessed fines and penalties, could be required to refund reimbursement amounts or could lose our licensure or Medicare and/or Medicaid certification so that we or our affiliated professional entities and other physician partners are unable to receive reimbursement from such programs and possibly from other third-party payors, any of which could materially adversely affect our business, financial condition, cash flows or results of operations.
If our arrangements with our affiliated professional entities and other physician partners are found to constitute the improper rendering of medical services or fee splitting under applicable state laws, our business, financial condition and our ability to operate in those states could be adversely impacted.
Our contractual relationships with our affiliated professional entities and other physician partners may implicate certain state laws that generally prohibit non-professional entities from providing licensed medical services or exercising control over licensed physicians or other healthcare professionals (such activities generally referred to as the “corporate practice of medicine”) or engaging in certain practices such as fee-splitting with such licensed professionals. The interpretation and enforcement of these laws vary significantly from state to state. There can be no assurance that these laws will be interpreted in a manner consistent with our practices or that other laws or regulations will not be enacted in the future that could have a material and adverse effect on our business, financial condition and results of operations. Regulatory authorities, state boards of medicine, state attorneys general and other parties may assert that, despite the agreements through which we operate, we are engaged in the provision of medical services and/or that our arrangements with our affiliated professional entities and other physician partners constitute unlawful fee-splitting. If a jurisdiction’s prohibition on the corporate practice of medicine or fee-splitting is interpreted in a manner that is inconsistent with our practices, we would be required to restructure or terminate our arrangements with our affiliated professional entities and other physician partners to bring our activities into compliance with such laws. A determination of non-compliance, or the termination of or failure to successfully restructure these relationships could result in disciplinary action, penalties, damages, fines, and/or a loss of revenue, any of which could have a material and adverse effect on our business, financial condition and results of operations. State corporate practice and fee-splitting prohibitions also often impose penalties on healthcare professionals for aiding in the improper rendering of professional services, which could discourage physicians and other healthcare professionals from providing clinical services to members of the health plans with whom we contract.
We face inspections, reviews, audits and investigations under federal and state government programs and contracts. These audits could have adverse findings that may negatively affect our business, including our results of operations, liquidity, financial condition and reputation.
As a result of our participation in the Medicare and Medicaid programs, we are subject to various governmental inspections, reviews, audits and investigations to verify our compliance with these programs and applicable laws and regulations. Other third-party payors may also reserve the right to conduct audits. We also periodically conduct internal audits and reviews of our regulatory compliance. An adverse inspection, review, audit or investigation could result in:
| ● | refunding amounts we have been paid pursuant to the Medicare or Medicaid programs or from payors; |
| ● | state or federal agencies imposing fines, penalties and other sanctions on us; |
| ● | temporary suspension of payment for new patients to the facility or agency; |
| ● | decertification or exclusion from participation in the Medicare or Medicaid programs or one or more payor networks; |
| ● | self-disclosure of violations to applicable regulatory authorities; |
| ● | damage to our reputation; |
36
| ● | the revocation of a facility’s or agency’s license; |
| ● | criminal penalties; |
| ● | a corporate integrity agreement with HHS’s Office of Inspector General; and |
| ● | loss of certain rights under, or termination of, our contracts with payors. |
We have in the past and will likely in the future be required to refund amounts we have been paid and/or pay fines and penalties as a result of these inspections, reviews, audits and investigations. If adverse inspections, reviews, audits or investigations occur and any of the results noted above occur, it could have a material adverse effect on our business and operating results. Furthermore, the legal, document production and other costs associated with complying with these inspections, reviews, audits or investigations could be significant.
Our records and submissions to a health plan may contain inaccurate or unsupportable information regarding risk adjustment scores of members, which could cause us to overstate or understate our revenue and subject us to various penalties.
The claims and encounter records that we submit to health plans may impact data that support the Medicare Risk Adjustment Factor (“RAF”) scores attributable to members. These RAF scores determine, in part, the revenue to which the health plans and, in turn, we or our affiliated professional entities or other physician partners are entitled for the provision of medical care to such members. The data submitted to CMS by each health plan is based, in part, on medical charts and diagnosis codes that we prepare and submit to the health plans. Each health plan generally relies on us and our affiliated professional entities or other physician partners to appropriately document and support such RAF data in our medical records. Each health plan also relies on us and our affiliated professional entities or other physician partners to appropriately code claims for medical services provided to members. Erroneous claims and erroneous encounter records and submissions could result in inaccurate revenue and risk adjustment payments, which may be subject to correction or retroactive adjustment in later periods. This corrected or adjusted information may be reflected in financial statements for periods subsequent to the period in which the revenue was recorded. We might also need to refund a portion of the revenue that we received, which refund, depending on its magnitude, could damage our relationship with the applicable health plan and could have an adverse effect on our business, results of operations, financial condition and cash flows.
Additionally, CMS audits MA plans for documentation to support RAF-related payments for members chosen at random. The MA plans ask providers to submit the underlying documentation for members that they serve. It is possible that claims associated with members with higher RAF scores could be subject to more scrutiny in a CMS or plan audit. There is a possibility that an MA plan may seek repayment from us should CMS make any payment adjustments to the MA plan as a result of its audits. The plans also may hold us liable for any penalties owed to CMS for inaccurate or unsupportable RAF scores provided by us or our affiliated professional entities or other physician partners. In addition, we could be liable for penalties to the government under the federal FCA, that include a monetary penalty adjusted for inflation on an annual basis for each false claim, plus up to three times the amount of damages caused by each false claim, which can be as much as the amounts received directly or indirectly from the government for each such false claim.
CMS has indicated that payment adjustments will not be limited to RAF scores for the specific MA enrollees for which errors are found but may also be extrapolated to the entire MA plan subject to a particular CMS contract. Based on a recent final rule issued by CMS in January 2023, although 2011 to 2017 plan years are still subject to audit, overpayments to MA plans that are identified as a result of a Risk Adjustment Data Validation (“RADV”), audit will only be subject to extrapolation for plan year 2018 and any subsequent plan year. In addition, CMS will not apply an adjustment factor, known as a FFS Adjuster, in RADV audits to account for potential differences in diagnostic coding between the MA program and Medicare FFS program. We are continuing to assess the potential impact this final rule may have on our business and operations.
There can be no assurance that a health plan will not be randomly selected or targeted for review by CMS or that the outcome of such a review will not result in a material adjustment in our revenue and profitability, even if the information we submitted to the plan is accurate and supportable.
37
The impact on us of recent healthcare legislation and other changes in the healthcare industry and in healthcare spending is currently unknown, but may adversely affect our business, financial condition and results of operations.
The impact on us of healthcare reform legislation and other changes in the healthcare industry and in healthcare spending is currently unknown, but may adversely affect our business, financial condition and results of operations. Our revenue is dependent on the healthcare industry and could be affected by changes in healthcare spending, reimbursement and policy. The healthcare industry is subject to changing political, regulatory and other influences. By way of example, the ACA, which was enacted in 2010, made major changes in how healthcare is delivered and reimbursed, and it increased access to health insurance benefits to the uninsured and underinsured populations of the United States.
Since its enactment, there have been judicial, executive and Congressional challenges to certain aspects of the ACA. On June 17, 2021, the U.S. Supreme Court dismissed the most recent judicial challenge to the ACA brought by several states without specifically ruling on the constitutionality of the ACA. Prior to the Supreme Court’s decision, President Biden issued an executive order initiating a special enrollment period from February 15, 2021 through August 15, 2021 for purposes of obtaining health insurance coverage through the ACA marketplace. The executive order also instructed certain governmental agencies to review and reconsider their existing policies and rules that limit access to healthcare.
Other legislative changes have been proposed and adopted since the ACA was enacted. These changes include aggregate reductions to Medicare payments to providers, which began in 2013 and will remain in effect through 2032, with the exception of a temporary suspension from May 1, 2020 through March 30, 2022, unless additional Congressional action is taken. In January 2013, the American Taxpayer Relief Act of 2012 was signed into law, which, among other things, further reduced Medicare payments to several types of providers, including hospitals, imaging centers and cancer treatment centers, and increased the statute of limitations period for the government to recover overpayments to providers from three to five years. New laws may result in additional reductions in Medicare and other healthcare funding, which may materially adversely affect consumer demand and affordability for our products and services and, accordingly, the results of our financial operations. Additional changes that may affect our business include the expansion of new programs such as Medicare payment for performance initiatives for physicians under the Medicare Access and CHIP Reauthorization Act of 2015 (“MACRA”), which first affected physician payment in 2019. At this time, it is unclear how the introduction of the Medicare quality payment program will impact overall physician reimbursement.
Such changes in the regulatory environment may also result in changes to our payer mix that may affect our operations and revenue. In addition, certain provisions of the ACA authorize voluntary demonstration projects, which include the development of bundling payments for acute, inpatient hospital services, physician services and post-acute services for episodes of hospital care. Further, the ACA may adversely affect payors by increasing medical costs generally, which could have an effect on the industry and potentially impact our business and revenue as payors seek to offset these increases by reducing costs in other areas.
In addition, new legislative proposals to reform healthcare and government insurance programs, along with the trend toward managed healthcare in the United States, could result in reduced demand and prices for our services. We expect that additional state and federal healthcare reform measures will be adopted in the future, any of which could limit the amounts that federal and state governments and other third-party payers will pay for healthcare products and services, which could adversely affect our business, financial condition and results of operations.
The evolving regulation of value-based reimbursement models may have a material adverse effect on our operations.
Regulation of downstream risk-sharing arrangements, including, but not limited to, global risk and other value-based arrangements, varies significantly from state to state. Some states require downstream entities and risk-bearing entities to obtain an insurance license, a certificate of authority, or an equivalent authorization, in order to participate in downstream risk-sharing arrangements with payors. In some states, statutes, regulations and/or formal guidance explicitly address whether and in what manner the state regulates the transfer of risk by a payor to a downstream entity. However, the majority of states do not explicitly address the issue, and in such states, regulators may nonetheless interpret statutes and regulations to regulate such activity. If downstream risk-sharing arrangements are not regulated directly in a particular state, the state regulatory agency may nonetheless require oversight by the licensed payor as the party to such a downstream risk-sharing arrangement. Such oversight is accomplished via contract and may include the imposition of reserve requirements, as well as reporting obligations. Further, state regulatory stances regarding downstream risk-sharing arrangements can change rapidly and codified provisions may not keep pace with evolving risk-sharing mechanisms and other new value-based reimbursement models. Certain of the states where we currently operate or may choose to
38
operate in the future regulate the operations and financial condition of risk bearing organizations like us and our affiliated providers. These regulations can include capital requirements, licensing or certification, governance controls and other similar matters. As a result, new and existing laws, regulations or guidance could have a material adverse effect on our operations and could subject us to the risk of restructuring or terminating our arrangements with our affiliated professional entities or other physician partners, as well as the risk of regulatory enforcement, penalties and sanctions, if state and federal enforcement agencies disagree with our interpretation of these laws. While these regulations have not had a material impact on our business to date, as we continue to expand, these rules may require additional resources and capitalization and add complexity to our business.
Regulatory proposals directed at containing or lowering the cost of healthcare, including the Direct Contracting Model, and our participation, voluntary or otherwise, in such proposed models, could impact our business, financial condition, cash flows and operations.
The ACA also required CMS to establish a Medicare shared savings program that promotes accountability and coordination of care through the creation of ACOs. The Medicare shared savings program allows for providers, physicians and other designated healthcare professionals and suppliers to form ACOs and voluntarily work together to invest in infrastructure and redesign delivery processes to give coordinated high quality care to their Medicare patients, avoid unnecessary duplication of services and prevent medical errors. ACOs that achieve quality performance standards established by CMS are eligible to share in a portion of the Medicare program’s cost savings. We have an ACO in Arizona participating in the Medicare Shared Savings Plan (“MSSP”), and is subject to ACO program methodologies and participation requirements that are updated by CMS for each performance year. We and our affiliated providers as ACO participants are expected to comply with such program requirements and are required to report to CMS on performance after the close of the year. Failure to comply with such program requirements could subject us and our affiliated providers to significant penalties and, in some cases, termination from participating in MSSP.
Additionally, the Center for Medicare and Medicaid Innovation continues to test an array of value-based alternative payment models, including the Global and Professional Direct Contracting Model to allow Direct Contracting Entities to negotiate directly with the government to manage traditional Medicare beneficiaries and share in the savings and risks generated from managing such beneficiaries. Although we currently do not participate in these pilot payment models, we may choose to do so in the future. Additional changes that may affect our business include the expansion of new programs such as Medicare payment for performance initiatives for physicians under the MACRA, which first affected physician payment in 2019. At this time, it is unclear how the introduction of the Medicare quality payment program will impact overall physician reimbursement. In addition, there likely will continue to be regulatory proposals directed at containing or lowering the cost of healthcare, as government healthcare programs and other third-party payors transition from FFS to value-based reimbursement models, which can include risk-sharing, bundled payment and other innovative approaches. It is possible that the federal or state governments will implement additional reductions, increases, or changes in reimbursement in the future under government programs that may adversely affect us or increase the cost of providing our services. The implementation of cost containment measures or other healthcare reforms may prevent us from being able to generate revenue or attain growth, any of which could have a material impact on our business.
Risks Related to Ownership of Our Common Stock
We have identified material weaknesses in our internal control over financial reporting. If we fail to establish and maintain effective internal controls in accordance with Section 404 of the Sarbanes-Oxley Act, we may not be able to accurately report our financial results or file our periodic reports in a timely manner, which may cause adverse effects on our business and may cause investors to lose confidence in our reported financial information and may lead to a decline in the price of our Class A common stock.
The Sarbanes-Oxley Act of 2002 (the “Sarbanes-Oxley Act”) requires, among other things, that we maintain effective disclosure controls and procedures and internal control over financial reporting. We are required to furnish a report by management on, among other things, the effectiveness of our internal control over financial reporting pursuant to Section 404(a) of the Sarbanes-Oxley Act in our annual reports. This assessment must include disclosure of any material weaknesses identified by our management in our internal control over financial reporting. Additionally, once we no longer qualify as an “emerging growth company,” we will be required to have our independent registered public accounting firm provide an attestation report on the effectiveness of our internal control over financial reporting. An adverse report may be issued in the event our independent registered public accounting firm is not satisfied with the level at which our controls are documented, designed or operating.
39
Effective internal control over financial reporting is necessary for us to provide reliable financial reports in a timely manner. When evaluating our internal control over financial reporting, we have identified, and we may identify additional, material weaknesses that we may not be able to remediate in time to meet the applicable deadline imposed upon us for compliance with the requirements of Section 404. In connection with the audits of our consolidated financial statements for the years ended December 31, 2018, 2019, 2020 and 2021, and the restatement of our consolidated financial statements for the years ended December 31, 2020 and 2019, we concluded that there were material weaknesses in our internal control over financial reporting, which continued to exist as of December 31, 2022. A material weakness is a deficiency, or a combination of deficiencies, in internal control over financial reporting, such that there is a reasonable possibility that a material misstatement of the annual or interim financial statements will not be prevented or detected on a timely basis. We did not maintain appropriately designed entity-level controls impacting the control environment, risk assessment procedures, and effective monitoring controls to prevent or detect material misstatement to the consolidated financial statements. These material weaknesses are specifically attributed to the following: (i) we did not have adequate policies and procedure or sufficient qualified resources with sufficient technical knowledge to maintain effective controls over the accounting related to significant accounts and related financial statement disclosures; (ii) we did not design and implement a sufficient risk assessment process to identify and assess risks impacting control over financial reporting; and (iii) we had ineffective evaluation and determination as to whether the components of internal control were present and functioning. As a consequence of these entity-level material weaknesses, we did not design, implement, and maintain effective control activities within certain business processes and the information technology environment to mitigate the risk of material misstatement in financial reporting. Specifically: (i) we did not maintain effective controls over our information systems to ensure that relevant and reliable information was communicated on a timely basis across the organization to support the financial reporting process. Particularly, we did not design and implement effective information technology general controls in the areas of user access related to certain information technology systems that support our financial reporting process. We also did not maintain sufficient segregation of duties over the performance of control activities for financial close and reporting, including over the review of account reconciliations and journal entries; (ii) we did not design and maintain effective management review controls at a sufficient level of precision over the accounting for transactions related to the risk adjustment factor receivable and related revenue, capitated revenue classification, premium deficiency reserves, business combinations, goodwill and intangibles, income taxes, warrant valuation, and equity awards. This material weakness resulted in certain material corrections to the financial statements; (iii) we did not design and maintain effective controls at a sufficient level of precision over the estimation of claims expense and payable including controls over the review of historical claims data, including the completeness and accuracy of data used to determine the financial statement amounts; and (iv) we did not design and maintain effective controls over accounting for complex transactions, including the inaccurate attribution of net income or loss to the controlling and non-controlling interest for subsidiaries that are variable interest entities, the improper classification of the Class A Units as permanent equity instead of temporary equity, and the improper accounting of preferred returns in equity and interest expense, as no recognition is necessary until legally declared.
We have taken and are taking steps to remediate these material weaknesses through (i) hiring qualified accounting, financial reporting, IT, and other key management personnel with public company experience, (ii) engaging an external advisor to assist with the risk assessment process, documenting internal controls, including enhancing controls to ensure proper communication of critical information, review and approvals; evaluating effectiveness of internal controls and assist with the remediation of deficiencies and training of personnel, as necessary, and establishment of a formal internal audit function and (iii) enhancing policies and procedures documentation for key areas of accounting, including each area where a material weakness was identified. However, we are still in the process of implementing these steps and cannot assure investors that these measures will significantly improve or remediate the material weaknesses described above. We have identified other deficiencies in our internal control over financial reporting that have not risen to the level of a material weakness, which we are in the process of remediating.
If we are unable to successfully remediate the material weaknesses or identify any future significant deficiencies or material weaknesses, are unable to comply with the requirements of Section 404 in a timely manner or assert that our internal control over financial reporting is ineffective, or if our independent registered public accounting firm is unable to express an opinion as to the effectiveness of our internal control over financial reporting, the accuracy and timing of our financial reporting may be adversely affected, a material misstatement in our financial statements could occur, and we may be unable to maintain compliance with securities law requirements regarding timely filing of periodic reports, which may adversely affect our business and the price of our Class A common stock may decline as a result. Investors may also lose confidence in the accuracy and completeness of our financial reports, the market price of our Class A common stock and warrants could be negatively affected, and we could become subject to investigations by Nasdaq Stock Market LLC (“Nasdaq”), the SEC or other regulatory authorities, which would require additional financial and management resources.
40
In addition, even if we remediate the material weaknesses, we will be required to expend significant time and resources to further improve our internal controls over financial reporting, including by further expanding our finance and accounting staff to meet the demands placed upon us as a public company, including the requirements of the Sarbanes-Oxley Act. If we fail to adequately staff our accounting and finance function to remediate our material weaknesses or fail to maintain adequate internal control over financial reporting, any new or recurring material weaknesses could prevent our management from concluding that our internal control over financial reporting is effective and impair our ability to prevent material misstatements in our financial statements, which could cause our business to suffer.
We are an “emerging growth company” and we have elected to comply with reduced public company reporting requirements, which could make our Class A common stock less attractive to investors.
We are an “emerging growth company,” as defined in the Jumpstart Our Business Startups Act of 2012 (“JOBS Act”). For as long as we continue to be an emerging growth company, we are eligible for certain exemptions from various public company reporting requirements. These exemptions include, but are not limited to, (i) not being required to comply with the auditor attestation requirements of Section 404 of the Sarbanes-Oxley Act, (ii) reduced disclosure obligations regarding executive compensation in our periodic reports, proxy statements and registration statements, (iii) exemptions from the requirements of holding a nonbinding advisory vote on executive compensation and shareholder approval of any golden parachute payments not previously approved, (iv) not being required to provide audited financial statements for certain periods and (v) an extended transition period to comply with new or revised accounting standards applicable to public companies. We will remain an emerging growth company until the earlier of (a) the last day of the fiscal year in which we have total annual gross revenue of $1.235 billion or more; (b) the last day of the fiscal year following the fifth anniversary of the date of the completion of the initial public offering of Foresight; (c) the date on which we have issued more than $1.0 billion in nonconvertible debt during the previous three years; or (d) the date on which we are deemed to be a large accelerated filer under the rules of the SEC, which means the market value of our Class A common stock that is held by non-affiliates exceeds $700 million as of the last business day of our second fiscal quarter. In addition, we have chosen to take advantage of the extended transition period to comply with new or revised accounting standards applicable to public companies. As a result, the information that we provide to holders of our Class A common stock may be different than you might receive from other public reporting companies in which you hold equity interests. We cannot predict if investors will find our Class A common stock less attractive as a result of reliance on these exemptions. If some investors find our Class A common stock less attractive as a result of our reduced disclosure, there may be a less active trading market for our Class A common stock and the market price for the Class A common stock may be more volatile.
We cannot predict the impact our dual-class structure may have on the stock price of our Class A common stock.
We cannot predict whether our dual-class structure will result in a lower or more volatile market price of our Class A common stock or in adverse publicity or other adverse consequences. For example, certain index providers have policies that restrict or prohibit the inclusion of companies with multiple-class share structures in certain of their indices, including the Russell 2000 and the S&P 500, S&P MidCap 400 and S&P SmallCap 600, which together make up the S&P Composite 1500. Beginning in 2017, MSCI, a leading stock index provider, opened public consultations on their treatment of no-vote and multi-class structures and temporarily barred new multi-class listings from certain of its indices; however, in October 2018, MSCI announced its decision to include equity securities “with unequal voting structures” in its indices and to launch a new index that specifically includes voting rights in its eligibility criteria. Under the announced policies, our dual-class capital structure will make us ineligible for inclusion in certain indices, and as a result, mutual funds, exchange-traded funds and other investment vehicles that attempt to passively track those indices will not be investing in our stock. It is possible that these policies may depress the valuations of publicly traded companies that are excluded from the indices compared to those of other similar companies that are included. Because of our dual-class structure, we will likely be excluded from certain of these indices and we cannot assure you that other stock indices will not take similar actions. Given the sustained flow of investment funds into passive strategies that seek to track certain indices, exclusion from stock indices would likely preclude investment by many of these funds and could make shares of our Class A common stock less attractive to other investors. As a result, the market price of shares of our Class A common stock could be adversely affected.
41
Delaware law and our certificate of incorporation and bylaws contain certain provisions, including anti-takeover provisions that limit the ability of stockholders to take certain actions and could delay or discourage takeover attempts that stockholders may consider favorable.
Our certificate of incorporation and bylaws, and the General Corporation Law of the State of Delaware (“DGCL”), contain provisions that could have the effect of rendering more difficult, delaying, or preventing an acquisition that stockholders may consider favorable, including transactions in which stockholders might otherwise receive a premium for their shares. These provisions could also limit the price that investors might be willing to pay in the future for shares of Class A common stock, and therefore depress the trading price of Class A common stock. These provisions could also make it difficult for stockholders to take certain actions, including electing directors who are not nominated by the current members of our board of directors or taking other corporate actions, including effecting changes in our management. Among other things, the certificate of incorporation and the bylaws include provisions:
| ● | providing for a classified board of directors with staggered, three-year terms; |
| ● | regarding the ability of the board of directors to issue shares of preferred stock, including “blank check” preferred stock and to determine the price and other terms of those shares, including preferences and voting rights, without stockholder approval, which could be used to significantly dilute the ownership of a hostile acquirer; |
| ● | prohibiting cumulative voting in the election of directors, which limits the ability of minority stockholders to elect director candidates; |
| ● | regarding the limitation of the liability of, and the indemnification of, directors and officers; |
| ● | providing that certain transactions are not “corporate opportunities” and that, subject to certain exceptions, Foresight Sponsor Group, LLC, (the “Sponsor”) or the Chicago Pacific Founders funds or their respective affiliates and any of their respective principals, members, directors, partners, stockholders, officers, employees or other representatives, or any director or stockholder who is not employed by us or our subsidiaries, are not subject to the doctrine of corporate opportunity and such persons do not have any fiduciary duty to refrain from engaging directly or indirectly in the same or similar business activities or lines of business as us or any of our subsidiaries; |
| ● | regarding the ability of the board of directors to amend the bylaws, which may allow the board of directors to take additional actions to prevent an unsolicited takeover and inhibit the ability of an acquiror to amend the bylaws to facilitate an unsolicited takeover attempt; and |
| ● | regarding advance notice procedures with which stockholders must comply to nominate candidates to the board of directors or to propose matters to be acted upon at a stockholders’ meeting, which could preclude stockholders from bringing matters before annual or special meetings of stockholders and delay changes in the board of directors and also may discourage or deter a potential acquirer from conducting a solicitation of proxies to elect the acquirer’s own slate of directors or otherwise attempting to obtain control of our company. |
These provisions, alone or together, could delay or prevent hostile takeovers and changes in control or changes in our board of directors or management.
The Sponsor and the Chicago Pacific Founders funds, which are significant stockholders in our company, and their respective affiliates and representatives, non-employee directors and other non-employee stockholders will not be limited in their ability to compete with us, and the corporate opportunity provisions in our certificate of incorporation could enable such persons to benefit from corporate opportunities that might otherwise be available to us, which presents potential conflicts of interest.
Our certificate of incorporation provides that subject to certain exceptions, the Sponsor and the Chicago Pacific Founders funds and their respective affiliates and any of their respective principals, members, directors, partners, stockholders, officers, employees or other representatives, or any director or stockholder who is not employed by us or our subsidiaries, would not be
42
restricted from owning assets or engaging in businesses that compete directly or indirectly with us or any of our subsidiaries. In particular, subject to the limitations of applicable law and the certificate of incorporation, these persons may among other things:
| ● | engage in a corporate opportunity in the same or similar business activities or lines of business in which we or our affiliates have a reasonable expectancy interest or property right; |
| ● | purchase, sell or otherwise engage in transactions involving securities or indebtedness of us or our affiliates, provided that such transactions do not violate our insider trading policies; and |
| ● | otherwise compete with us. |
One or more of these persons may become aware, from time to time, of certain business opportunities (such as acquisition opportunities) and may direct such opportunities to other businesses in which they have invested, in which case we may not become aware of or otherwise have the ability to pursue such opportunities. Further, such businesses may choose to compete with us for these opportunities, possibly causing these opportunities to not be available to us or causing them to be more expensive for us to pursue. As a result, our renunciation of our interest and expectancy in any business opportunity that may be from time to time be presented to such persons, could adversely impact our business or prospects if attractive business opportunities are procured by such parties for their own benefit rather than for ours.
The provision of our certificate of incorporation requiring exclusive forum in certain courts in the State of Delaware or the federal district courts of the United States for certain types of lawsuits may have the effect of discouraging lawsuits against our directors and officers.
Our certificate of incorporation requires, to the fullest extent permitted by law, that (i) any derivative action or proceeding brought on our company’s behalf, (ii) any action asserting a claim of breach of a fiduciary duty owed by any of our directors, officers or stockholders to our company or our stockholders, (iii) any action asserting a claim against our company arising pursuant to any provision of the DGCL or the certificate of incorporation or our bylaws or (iv) any action asserting a claim against our company governed by the internal affairs doctrine will have to be brought in a state court located within the State of Delaware (or if no state court of the State of Delaware has jurisdiction, the federal district court for the District of Delaware), in all cases subject to the courts having personal jurisdiction over the indispensable parties named as defendants. The foregoing provision will not apply to claims seeking to enforce any liability or duty created by the Exchange Act.
Additionally, unless we consent in writing to the selection of an alternative forum, the federal district courts of the United States of America shall be the exclusive forum for the resolution of any complaint asserting a cause of action arising under the Securities Act.
Although we believe these exclusive forum provisions benefit our company by providing increased consistency in the application of Delaware law and federal securities laws in the types of lawsuits to which each applies, the exclusive forum provisions may limit a stockholder’s ability to bring a claim in a judicial forum that it finds favorable for disputes with us or any of our directors, officers or stockholders, which may discourage lawsuits with respect to such claims. Further, in the event a court finds either exclusive forum provision contained in our certificate of incorporation to be unenforceable or inapplicable in an action, we may incur additional costs associated with resolving such action in other jurisdictions, which could harm our business, operating results and financial condition.
An active, liquid trading market for our Class A common stock may not be sustained.
There can be no assurance that we will be able to maintain an active trading market for our Class A common stock on Nasdaq or any other exchange in the future. If an active market for our Class A common stock is not maintained, or if we fail to satisfy the continued listing standards of Nasdaq for any reason and our Class A common stock is delisted, it may be difficult for our stockholders to sell their Class A common stock without depressing the market price for our Class A common stock, or at all. An inactive trading market may also impair our ability to both raise capital by selling shares of capital stock, attract and motivate employees through equity incentive awards and acquire other companies, products, or technologies by using shares of capital stock as consideration.
43
There may be sales of a substantial amount of our Class A common stock in future by our stockholders, and these sales could cause the price of our Class A common stock to fall.
As of December 31, 2022, there were approximately 41.6 million shares of Class A common stock outstanding and an additional approximately 201.6 million shares of Class V common stock, which are exchangeable, together with P3 LLC units, for an equivalent number of shares of Class A common stock. Our issued and outstanding shares of Class A common stock are freely transferable, except for any shares held by our “affiliates,” as that term is defined in Rule 144 under the Securities Act. As of December 31, 2022, approximately 62.2% of the outstanding shares of Class A common stock (on an as-converted and as-exchanged basis) were held by entities affiliated with us and our executive officers and directors.
In addition, pursuant to the Amended and Restated Registration Rights and Lock-Up Agreement that we entered into with certain of our stockholders, we are obligated to register the resale of shares of Class A common stock held by such stockholders and issuable upon the exercise or exchange of securities held by such stockholders. In addition, these stockholders are entitled to demand the registration of such shares of Class A common stock subject to certain minimum requirements and also have certain “piggyback” registration rights with respect to registration statements we file.
Upon effectiveness of any registration statement we file for the resale of shares held by such stockholders, and upon the expiration of the lock-up periods applicable to such stockholders, these stockholders may sell large amounts of our Class A common stock in the open market or in privately negotiated transactions, which could have the effect of increasing the volatility in the share price of our Class A common stock or putting significant downward pressure on the price of our Class A common stock.
Sales of substantial amounts of our Class A common stock in the public market, or the perception that such sales will occur, could adversely affect the market price of our Class A common stock and make it difficult for us to raise funds through securities offerings in the future.
There can be no assurance that we will be able to comply with the continued listing standards of Nasdaq.
If Nasdaq delists our securities from trading on its exchange for failure to meet the listing standards, we could face significant material adverse consequences including:
| ● | a limited availability of market quotations for our securities; |
| ● | reduced liquidity for our securities; |
| ● | a determination that our Class A common stock is a “penny stock,” which will require brokers trading in our Class A common stock to adhere to more stringent rules and possibly result in a reduced level of trading activity in the secondary trading market for our securities; |
| ● | a limited amount of news and analyst coverage; and |
| ● | a decreased ability to issue additional securities or obtain additional financing in the future. |
On May 18, 2022, we received a notification from the listing qualifications department of Nasdaq indicating that as a result of our delinquency in the filing of our Annual Report on Form 10-K for the fiscal year ended December 31, 2021 and our Quarterly Report on Form 10-Q for the quarterly period ended March 31, 2022, we were not in compliance with the requirements for continued listing under Listing Rule 5250(c)(1) (the “Listing Rule”), which requires listed companies to timely file all required periodic financial reports with the SEC. On August 17, 2022, we received a second deficiency notice from Nasdaq as a result of the delay in filing our Quarterly Report on Form 10-Q for the quarterly period ended June 30, 2022 (the “Second Quarter Form 10-Q”), indicating that any additional Nasdaq exception to allow the Company to regain compliance with all delinquent filings, including the Second Quarter Form 10-Q, would be limited to September 27, 2022. On September 28, 2022, because we did not file the delinquent periodic reports prior to the expiration of the compliance period, the Nasdaq Listing Qualifications Department initiated a process to delist our securities from Nasdaq. We subsequently appealed Nasdaq’s delisting determination by requesting a hearing before the Nasdaq Hearing Panel (the “Panel”), which was granted by the Nasdaq Staff. Prior to the scheduled Panel hearing, we regained compliance
44
with the Listing Rule following the filing of our three delinquent periodic reports with the SEC on October 21, 2022. We received a letter from the Nasdaq Staff informing us that our filing delinquency had been cured and we were in compliance with all applicable listing standards and accordingly, that the scheduled hearing before the Panel had been determined to be moot and had been cancelled, and that our securities would continue to be listed and traded on Nasdaq.
While we have regained compliance with the Nasdaq listing standards, there is no assurance that we will remain in compliance with the listing requirements of Nasdaq in the future. We cannot guarantee that any actions we take to prevent future non-compliance or to regain compliance with Nasdaq’s listing requirements in the future will be successful.
Risks Related to Our Warrants
Our warrants may have an adverse effect on the market price of our Class A common stock.
Foresight issued 10,819,105 warrants to purchase shares of our Class A common stock (the “Public Warrants”) as part of the units offered in its initial public offering and, simultaneously with the closing of its initial public offering, Foresight issued in a private placement an aggregate of 832,500 units, including (i) an aggregate of 277,500 private placement warrants, each exercisable to purchase one share of Class A common stock at $11.50 per share, subject to adjustment (the “Private Placement Warrants”), and (ii) an aggregate of 832,500 shares of Class A common stock.
In addition, on December 13, 2022, in connection with our issuance of the VGS Promissory Note (see Note 12 “Debt” to the consolidated financial statements included elsewhere in this Form 10-K), we issued to VGS warrants to purchase 429,180 shares of Class A common stock.
To the extent such warrants are exercised, additional shares of our Class A common stock will be issued, which will result in dilution to our stockholders and increase the number of shares of Class A common stock eligible for resale in the public market. Sales of substantial numbers of such shares in the public market or the fact that such warrants may be exercised could adversely affect the market price of our Class A common stock.
We may redeem your unexpired Public Warrants prior to their exercise at a time that is disadvantageous to you, thereby making your Public Warrants worthless.
We have the ability to redeem outstanding Public Warrants at any time after they become exercisable and prior to their expiration, at a price of $0.01 per Public Warrant if, among other things, the last reported sales price of our Class A common stock equals or exceeds $18.00 per share (as adjusted for stock splits, stock dividends, reorganizations, recapitalizations and the like) for any 20 trading days within a 30 trading-day period ending on the third trading day prior to the date we send the notice of such redemption to the Public Warrant holders. If and when the Public Warrants become redeemable by us, we may exercise our redemption right even if we are unable to register or qualify the underlying securities for sale under all applicable state securities laws. Redemption of the outstanding Public Warrants could force you (i) to exercise your Public Warrants and pay the exercise price therefor at a time when it may be disadvantageous for you to do so, (ii) to sell your Public Warrants at the then-current market price when you might otherwise wish to hold your Public Warrants or (iii) to accept the nominal redemption price which, at the time the outstanding Public Warrants are called for redemption, is likely to be substantially less than the market value of your Public Warrants.
In addition, we may redeem your Public Warrants commencing 90 days after they become exercisable and prior to their expiration, at a price of $0.10 per Public Warrant if, among other things, the last reported sale price of our Class A common stock equals or exceeds $10.00 per share (as adjusted for stock splits, stock dividends, reorganizations, recapitalizations and the like) on the trading day prior to the date on which we send the notice of redemption to the Public Warrant holders. In such a case, the holders will be able to exercise their Public Warrants for cash or on a cashless basis prior to redemption and receive that number of shares of Class A common stock determined based on the redemption date and the fair market value of our Class A common stock. The value received upon exercise of the Public Warrants (1) may be less than the value the holders would have received if they had exercised their Public Warrants at a later time where the underlying share price is higher and (2) may not compensate the holders for the value of the Public Warrants, including because the number of shares of Class A common stock received in connection with such an exercise is capped at 0.361 shares of Class A common stock per whole Public Warrant (subject to adjustment) irrespective of the remaining life of the Public Warrants.
45
None of the Private Placement Warrants will be redeemable by us so long as they are held by the Sponsor or its permitted transferees.
Certain of our warrants are accounted for as liabilities and the changes in value of these warrants could have a material effect on our financial results.
On April 12, 2021, the Acting Chief Accountant and Acting Director of the Division of Corporation Finance of the SEC published a statement on the SEC’s website indicating that the terms of the public and private warrants issued by many special purpose acquisition companies may need to be accounted for as liabilities, rather than as equity (the “SEC Warrant Accounting Statement”). As a result of the SEC Warrant Accounting Statement, Foresight, along with many other current and former special purpose acquisition companies, concluded that certain warrants should be presented as liabilities with subsequent fair value remeasurement and engaged a valuation firm to determine the fair market value of its warrants. Accordingly, Foresight reevaluated the accounting treatment of the Public Warrants to purchase 10,819,105 shares of Class A common stock and Private Placement Warrants to purchase 277,500 shares of Class A common stock, and determined to classify all of the warrants as derivative liabilities measured at fair value, with changes in fair value each period reported in earnings.
As a result, included on our consolidated balance sheet as of December 31, 2022 contained elsewhere in this Form 10-K are derivative liabilities related to embedded features contained within the warrants. Accounting Standards Codification 815, Derivatives and Hedging, provides for the remeasurement of the fair value of such derivatives at each balance sheet date, with a resulting non-cash gain or loss related to the change in the fair value being recognized in earnings in the statements of operations. As a result of the recurring fair value measurement, our financial statements and results of operations may fluctuate quarterly, based on factors, which are outside of its control. Due to the recurring fair value measurement, we expect that we will recognize non-cash gains or losses on our warrants each reporting period and that the amount of such gains or losses could be material.
Risks Related to the Tax Receivable Agreement
Our sole material asset is our interest in P3 LLC, and, accordingly, we depend on distributions from P3 LLC to pay our taxes and expenses, including payments under the Tax Receivable Agreement. P3 LLC’s ability to make such distributions may be subject to various limitations and restrictions.
We are a holding company and have no material assets other than our ownership in P3 LLC. As such, we have no independent means of generating revenue or cash flow, and our ability to pay taxes and operating expenses or declare and pay dividends in the future, if any, will be dependent upon the financial results and cash flows of P3 LLC and its subsidiaries, and distributions we receive from P3 LLC. There can be no assurance that P3 LLC and its subsidiaries will generate sufficient cash flow to distribute funds to us, or that applicable state law and contractual restrictions, including negative covenants in any debt agreements of P3 LLC or its subsidiaries, will permit such distributions. The credit agreement governing P3 LLC’s credit facilities restrict its ability to make distributions to the Company, and future debt instruments or other agreements may restrict the ability of P3 LLC to make distributions to the Company or of P3 LLC’s subsidiaries to make distributions to P3 LLC.
P3 LLC will continue to be treated as a partnership for U.S. federal income tax purposes and, as such, generally will not be subject to any entity-level U.S. federal income tax. Instead, taxable income will be allocated to holders of P3 LLC Units, including us. Accordingly, we will incur income taxes on our allocable share of any net taxable income of P3 LLC. Under the terms of the P3 LLC A&R LLC Agreement, P3 LLC will be obligated, subject to various limitations and restrictions, including with respect to any debt agreements, to make tax distributions to holders of P3 LLC Units, including us. In addition to tax expenses, we will also incur expenses related to our operations, including payments under the Tax Receivable Agreement, which could be substantial. We intend, as its sole manager, to cause P3 LLC to make cash distributions to the owners of P3 LLC Units in an amount sufficient to (i) fund all of such owners’ tax obligations in respect of taxable income allocated to such owners and (ii) cover our operating expenses, including payments under the Tax Receivable Agreement. However, P3 LLC’s ability to make such distributions may be subject to various limitations and restrictions, such as restrictions on distributions under contracts or agreements to which P3 LLC is then a party, including debt agreements, or any applicable law, or that would have the effect of rendering P3 LLC insolvent. If P3 LLC does not have sufficient funds to pay tax or other liabilities or to fund its operations, it may have to borrow funds, which could materially adversely affect its liquidity and financial condition and subject it to various restrictions imposed by any such lenders. To the extent that we are unable to make timely payments under the Tax Receivable Agreement for any reason, the unpaid amounts will be deferred and will accrue interest until paid. Our failure to make any payment required under the Tax Receivable Agreement (including any
46
accrued and unpaid interest) within 90 calendar days of the date on which the payment is required to be made will constitute a material breach of a material obligation under the Tax Receivable Agreement, which will terminate the Tax Receivable Agreement and accelerate future payments thereunder, unless the applicable payment is not made because (i) P3 LLC is prohibited from making such payment under the terms of the Tax Receivable Agreement or the terms governing certain of its indebtedness or (ii) P3 LLC does not have, and despite using commercially reasonable efforts cannot obtain, sufficient funds to make such payment. In addition, if P3 LLC does not have sufficient funds to make distributions, its ability to declare and pay cash dividends will also be restricted or impaired.
Under the P3 LLC A&R LLC Agreement, P3 LLC will, from time to time, make distributions in cash to its equityholders (including us) pro rata, in amounts at least sufficient to cover the taxes on their allocable share of taxable income of P3 LLC. As a result of (i) potential differences in the amount of net taxable income allocable to us and to P3 LLC’s other equityholders, (ii) the lower tax rates currently applicable to corporations as opposed to individuals, and (iii) the favorable tax benefits that we anticipate from any purchase of P3 Existing Units in connection with the Business Combinations and future redemptions or exchanges by the P3 Equityholders of P3 LLC Units for Class A common stock or cash pursuant to the P3 LLC A&R LLC Agreement, tax distributions payable to us may be in amounts that exceed our actual tax liabilities with respect to the relevant taxable year, including our obligations under the Tax Receivable Agreement. Our board of directors will determine the appropriate uses for any excess cash so accumulated, which may include, among other uses, the payment of other expenses or dividends on our stock, although we will have no obligation to distribute such cash (or other available cash) to our stockholders. Except as otherwise determined by us as the sole manager of P3 LLC, no adjustments to the exchange ratio for P3 LLC Units and corresponding shares of our Class A common stock will be made as a result of any cash distribution by us or any retention of cash by us. To the extent we do not distribute such excess cash as dividends on our Class A common stock, we may take other actions with respect to such excess cash, for example, holding such excess cash or lending it (or a portion thereof) to P3 LLC, which may result in shares of our Class A common stock increasing in value relative to the value of P3 LLC Units. The holders of P3 LLC Units may benefit from any value attributable to such cash balances if they acquire shares of our Class A common stock in exchange for their P3 LLC Units, notwithstanding that such holders may previously have participated as holders of P3 LLC Units in distributions by P3 LLC that resulted in such excess cash balances.
We will be required to make payments under the Tax Receivable Agreement for certain tax benefits we may claim, and the amounts of such payments could be significant.
In connection with the closing of the Business Combinations, we entered into the Tax Receivable Agreement with certain of the P3 Equityholders and P3 LLC. The Tax Receivable Agreement generally provides for the payment by us to the P3 Equityholders of 85% of the income tax benefits, if any, that we actually realize (or are deemed to realize in certain circumstances) in periods after the closing as a result of: (i) increases in our proportionate share of the tax basis of P3 LLC’s assets resulting from Business Combinations, future redemptions or exchanges by the P3 Equityholders of P3 LLC Units for our Class A common stock or cash and certain distributions (or deemed distributions) by P3 LLC; and (ii) certain other tax benefits resulting from payments we make under the Tax Receivable Agreement. We will retain the benefit of the remaining 15% of these cash savings. The amount of the cash payments that we may be required to make under the Tax Receivable Agreement could be significant and is dependent upon significant future events and assumptions, including the timing of the exchanges of P3 LLC units, the price of our Class A common stock at the time of each exchange, the extent to which such exchanges are taxable transactions and the amount of the exchanging P3 Equityholder’s tax basis in its P3 LLC units at the time of the relevant exchange. The amount of such cash payments is also based on assumptions as to the amount and timing of taxable income we generate in the future, the U.S. federal income tax rate then applicable and the portion of our payments under the Tax Receivable Agreement that constitute interest or give rise to depreciable or amortizable tax basis. Moreover, payments under the Tax Receivable Agreement will be based on the tax reporting positions that we determine, which tax reporting positions are subject to challenge by taxing authorities. We will be dependent on distributions from P3 LLC to make payments under the Tax Receivable Agreement, and we cannot guarantee that such distributions will be made in sufficient amounts or at the times needed to enable us to make our required payments under the Tax Receivable Agreement, or at all. Any payments made by us to the P3 Equityholders under the Tax Receivable Agreement will generally reduce the amount of overall cash flow that might have otherwise been available to us. The payments under the Tax Receivable Agreement are also not conditioned upon the P3 Equityholders maintaining a continued ownership interest in P3 LLC or us. We may recognize an estimated liability under the Tax Receivable Agreement of approximately $530.0 million if all P3 Equityholders redeem or exchange their P3 LLC units for Class A common stock or cash at the earliest possible date permitted under the P3 LLC A&R LLC Agreement and assuming (a) the generation of sufficient future taxable income, (b) a trading price of $10 per share of Class A common stock at the time of the redemption or exchanges, (c) a constant corporate combined U.S. federal and state income tax rate of 23.89% and (d) no material changes in tax law.
47
In certain cases, payments under the Tax Receivable Agreement may be accelerated and/or significantly exceed the actual benefits, if any, we realize in respect of the tax attributes subject to the Tax Receivable Agreement.
The Tax Receivable Agreement provides that if we breach any of our material obligations under the Tax Receivable Agreement, if we undergo a change of control or if, at any time, we elect an early termination of the Tax Receivable Agreement, then the Tax Receivable Agreement will terminate and our obligations, or our successor’s obligations, to make payments under the Tax Receivable Agreement would accelerate and become immediately due and payable. The amount due and payable in those circumstances is determined based on certain assumptions, including an assumption that we would have sufficient taxable income to fully utilize all potential future tax benefits that are subject to the Tax Receivable Agreement. We may need to incur debt to finance payments under the Tax Receivable Agreement to the extent our cash resources are insufficient to meet our obligations under the Tax Receivable Agreement as a result of timing discrepancies or otherwise.
As a result of the foregoing, (i) we could be required to make cash payments to the P3 Equityholders that are greater than the specified percentage of the actual benefits we ultimately realize in respect of the tax benefits that are subject to the Tax Receivable Agreement, and (ii) we would be required to make a cash payment equal to the present value of the anticipated future tax benefits that are the subject of the Tax Receivable Agreement, which payment may be made significantly in advance of the actual realization, if any, of such future tax benefits. In these situations, our obligations under the Tax Receivable Agreement could have a substantial negative impact on our liquidity and could have the effect of delaying, deferring or preventing certain mergers, asset sales, other forms of business combination, or other changes of control due to the additional transaction costs a potential acquirer may attribute to satisfying such obligations. There can be no assurance that we will be able to finance our obligations under the Tax Receivable Agreement.
We will not be reimbursed for any payments made to P3 Equityholders under the Tax Receivable Agreement in the event that any tax benefits are disallowed.
We will not be reimbursed for any cash payments previously made to the P3 Equityholders pursuant to the Tax Receivable Agreement if any tax benefits initially claimed by us are subsequently challenged by a taxing authority and are ultimately disallowed. Instead, any excess cash payments made by us to a P3 Equityholder will be netted against any future cash payments that we might otherwise be required to make under the terms of the Tax Receivable Agreement. However, a challenge to any tax benefits initially claimed by us may not arise for a number of years following the initial time of such payment or, even if challenged early, such excess cash payment may be greater than the amount of future cash payments that we might otherwise be required to make under the terms of the Tax Receivable Agreement and, as a result, there might not be future cash payments from which to net against. The applicable U.S. federal income tax rules are complex and factual in nature, and there can be no assurance that the Internal Revenue Service or a court will not disagree with our tax reporting positions. As a result, it is possible that we could make cash payments under the Tax Receivable Agreement that are substantially greater than our actual cash tax savings.
Certain of the P3 Equityholders may receive payments under the Tax Receivable Agreement, and their interests may conflict with yours.
The P3 Equityholders may receive payments from us under the Tax Receivable Agreement upon any redemption or exchange of their P3 LLC units, including the issuance of shares of our Class A common stock upon any such redemption or exchange. As a result, the interests of the P3 Equityholders may conflict with the interests of holders of our Class A common stock. For example, the P3 Equityholders may have different tax positions from us which could influence their decisions regarding whether and when to dispose of assets, whether and when to incur new or refinance existing indebtedness, especially in light of the existence of the Tax Receivable Agreement, and whether and when we should terminate the Tax Receivable Agreement and accelerate our obligations thereunder. In addition, the structuring of future transactions may take into consideration tax or other considerations of P3 Equityholders even in situations where no similar considerations are relevant to us.
General Risk Factors
We may be subject to securities litigation, which is expensive and could divert management attention.
The market price of our securities may be volatile and, in the past, companies that have experienced volatility in the market price of their securities have been subject to securities class action litigation. We may be the target of this type of litigation in the
48
future. Securities litigation against us could result in substantial costs and divert management’s attention from other business concerns, which could seriously harm its business.
Because we have no current plans to pay cash dividends on our Class A common stock for the foreseeable future, you may not receive any return on investment unless you sell your Class A common stock for a price greater than that which you paid for it.
We may retain future earnings, if any, for future operations, expansion and debt repayment and have no current plans to pay any cash dividends for the foreseeable future. Any decision to declare and pay dividends will be made at the discretion of our board of directors and will depend on, among other things, our results of operations, financial condition, cash requirements, contractual restrictions and other factors that our board of directors may deem relevant. In addition, our ability to declare dividends may be limited by restrictive covenants contained in any existing or future indebtedness. As a result, you may not receive any return on an investment in our Class A common stock unless you sell your Class A common stock for a price greater than that which you paid for it.
The market price and trading volume of our Class A common stock and Public Warrants may be volatile and could decline significantly.
The trading price of our securities may fluctuate substantially and may be lower than the price at which you purchase such securities. There can be no assurance that the market price of Class A common stock and Public Warrants will not fluctuate widely or decline significantly in the future in response to a number of factors, including those described in this “Risk Factors” section, many of which are beyond our control and may not be related to our operating performance, and which may limit or prevent investors from readily selling their Class A common stock or Public Warrants and may otherwise negatively affect the liquidity of the Class A common stock or Public Warrants. These fluctuations could cause you to lose all or part of your investment.
Factors affecting the trading price of our securities may include:
| ● | actual or anticipated fluctuations in our quarterly financial results or the quarterly financial results of companies perceived to be similar to us; |
| ● | changes in the market’s expectations about our operating results; |
| ● | success of competitors; |
| ● | our operating results failing to meet the expectation of securities analysts or investors in a particular period; |
| ● | changes in financial estimates and recommendations by securities analysts concerning us or the health population management industry in general; |
| ● | operating and stock price performance of other companies that investors deem comparable to us; |
| ● | our ability to market new and enhanced products on a timely basis; |
| ● | changes in laws and regulations affecting our business; |
| ● | our ability to meet compliance requirements; |
| ● | commencement of, or involvement in, litigation involving us; |
| ● | changes in our capital structure, such as future issuances of securities or the incurrence of additional debt; |
| ● | the volume of shares of our Class A common stock available for public sale; |
| ● | any major change in our board of directors or management; |
49
| ● | sales of substantial amounts of Class A common stock by our directors, executive officers or significant stockholders or the perception that such sales could occur; and |
| ● | general economic and political conditions such as recessions, interest rates, fuel prices, international currency fluctuations, public health crises, and acts of war or terrorism. |
A loss of investor confidence in the market for retail stocks or the stocks of other companies which investors perceive to be similar to us could depress our stock price regardless of our business, prospects, financial condition or results of operations. A decline in the market price of our securities also could adversely affect our ability to issue additional securities and our ability to obtain additional financing in the future.
If securities or industry analysts do not publish research or publish inaccurate or unfavorable research about our business, the price and trading volume of our securities could decline.
The trading market for our securities depends in part on the research and reports that securities or industry analysts publish about us or our business. We do not control these analysts, and the analysts who publish information about us may have relatively little experience with us or our industry, which could affect their ability to accurately forecast our results and could make it more likely that we fail to meet their estimates. If few or no securities or industry analysts cover us, the trading price for our securities would be negatively impacted. If one or more of the analysts who covers us downgrades our securities, publishes incorrect or unfavorable research about us, ceases coverage of us, or fails to publish reports on us regularly, demand for and visibility of our securities could decrease, which could cause the price or trading volumes of our securities to decline.
We will continue to incur significantly increased costs and devote substantial management time as a result of operating as a public company.
As a public company, we will continue to incur significant legal, accounting and other expenses. For example, we are subject to the reporting requirements of the Exchange Act and are required to comply with the applicable requirements of the Sarbanes-Oxley Act and the Dodd-Frank Wall Street Reform and Consumer Protection Act, as well as rules and regulations of the SEC and Nasdaq, including the establishment and maintenance of effective disclosure and financial controls, corporate governance requirements and required filings of annual, quarterly and current reports with respect to our business and results of operations. Any failure to develop or maintain effective controls or any difficulties encountered in their implementation or improvement could harm our results of operations or cause us to fail to meet our reporting obligations. We expect that continued compliance with these requirements will increase our legal and financial compliance costs and will make some activities more time-consuming and costly. In addition, we expect that our management and other personnel will need to divert attention from operational and other business matters to devote substantial time to these public company requirements. In particular, we expect to incur significant expenses and devote substantial management effort toward ensuring compliance with the requirements of Section 404 of the Sarbanes-Oxley Act, which will increase when we are no longer an emerging growth company. We are in the process of hiring additional legal and accounting personnel and may in future need to hire additional accounting and financial staff with appropriate public company experience and technical accounting knowledge and may need to establish an internal audit function.
We also expect that being a public company will make it more expensive for us to obtain director and officer liability insurance, and we may be required to accept reduced coverage or incur substantially higher costs to obtain coverage. This could also make it more difficult for us to attract and retain qualified people to serve on our board of directors, board committees or as executive officers.
Our results of operations and financial condition are subject to management’s accounting judgments and estimates, as well as changes in accounting policies.
The preparation of our financial statements requires us to make estimates and assumptions affecting the reported amounts of our assets, liabilities, revenues and expenses. If these estimates or assumptions are incorrect, it could have a material adverse effect on our results of operations or financial condition. Generally accepted accounting principles in the U.S. are subject to interpretation by the Financial Accounting Standards Board, the American Institute of Certified Public Accountants, the SEC, and various bodies formed to promulgate and interpret appropriate accounting principles. A change in these principles or interpretations could have a significant effect on our reported financial results, and could affect the reporting of transactions completed before the announcement of a change.
50
Increased scrutiny of, and evolving expectations for, sustainability and environmental, social, and governance (“ESG”) initiatives could increase our costs, harm our reputation and adversely impact our financial results.
We, as with other companies, are facing increasing scrutiny related to our ESG practices and disclosures from certain investors, capital providers, shareholder advocacy groups, other market participants, customers, and other stakeholder groups. For example, certain institutional and individual investors have requested various ESG-related information and disclosures as they increasingly incorporate ESG criteria in making investment and voting decisions. With this increased focus, public reporting regarding ESG practices is becoming more broadly expected. Such increased scrutiny may result in increased costs, changes in demands for certain products, enhanced compliance or disclosure obligations, or other adverse impacts on our business, financial condition or results of operations.
While we may at times engage in voluntary initiatives (such as voluntary disclosures, certifications, or goals, among others), such initiatives may be costly and may not have the desired effect. For example, expectations around company’s management of ESG matters continues to evolve rapidly, in many instances due to factors that are out of our control. In addition, we may commit to certain initiatives or goals and we may not ultimately be able to achieve such commitments or goals due to cost, technological constraints, or other factors that are within or outside of our control. Moreover, actions or statements that we may take based on expectations, assumptions, or third-party information that we currently believe to be reasonable may subsequently be determined to be erroneous or be subject to misinterpretation. Even if this is not the case, our current actions may subsequently be determined to be insufficient by various stakeholders. If our ESG practices and reporting do not meet investor, consumer, employee, or other stakeholder expectations, which continue to evolve, our brand, reputation and customer retention may be negatively impacted, and we may be subject to investor or regulator engagement regarding such matters, even if they are currently voluntary. Certain market participants, including major institutional investors, use third-party benchmarks or scores to measure our ESG practices in making investment and voting decisions. As ESG best practices, reporting standards and disclosure requirements continue to develop, we may incur increasing costs related to ESG monitoring and reporting. In addition, new sustainability rules and regulations have been adopted and may continue to be introduced in various states and other jurisdictions. Operating in more than one jurisdiction is likely to make our compliance with ESG and sustainability-related rules more complex and expensive, and potentially expose us to greater levels of legal risks associated with our compliance. Our failure to comply with any applicable rules or regulations could lead to penalties and adversely impact our reputation, customer attraction and retention, access to capital and employee retention. Such ESG matters may also impact our suppliers and customers, which may augment or cause additional impacts on our business, financial condition, or results of operations.
Our management has limited experience in operating a public company.
Our executive officers and certain directors have limited experience in the management of a publicly traded company. Our management team may not successfully or effectively manage the transition to a public company subject to significant regulatory oversight and reporting obligations under federal securities laws. Their limited experience in dealing with the increasingly complex laws pertaining to public companies could be a significant disadvantage in that it is likely that an increasing amount of our management’s time may be devoted to these activities which will result in less time being devoted to the management and growth of the company. It is possible that we will be required to expand our employee base and hire additional employees to support our operations as a public company, which will increase our operating costs in future periods.
Item 1B. Unresolved Staff Comments.
None.
Item 2. Properties.
As of December 31, 2022, our principal executive office is located in Henderson, NV, where we occupy facilities totaling approximately 34,000 square feet, primarily under a lease that expires in July 2030. We use this facility for principal corporate activities. We also lease offices in Tucson, AZ; Las Vegas, NV; Salem, OR; Stockton, CA; and the St. Petersburg/Tampa areas, FL. We believe that our facilities are adequate to meet our needs for the immediate future, and that, should it be needed, suitable additional space will be available to accommodate any such expansion of our operations.
51
Item 3. Legal Proceedings.
The Company is a party to various claims, legal and regulatory proceedings, lawsuits and administrative actions arising in the ordinary course of business and associated with the Business Combinations. The Company carries general and professional liability insurance coverage to mitigate the Company’s risk of potential loss in such cases. An accrual is established when a specific contingency is probable and estimable. The Company also faces contingencies that are reasonably possible to occur that cannot currently be estimated. The Company believes that disposition of these matters will not have a material adverse effect on the Company’s consolidated financial position, net loss or cash flows. It is the Company’s policy to expense costs associated with loss contingencies, including any related legal fees, as they are incurred.
Books and Records Action
On April 19, 2021, two members of the P3 Board of Managers, Joseph Straus and Jonathan Bradburn, filed a lawsuit in the Delaware Court of Chancery captioned Straus et al v. P3 Health Group Holdings, LLC, C.A. No. 2021-0335-JTL (the “Books and Records Action”). In the Books and Records Action, Straus and Bradburn sought an order requiring P3 to produce certain books and records relating to the process leading up to, and the approval of, the Business Combinations. On May 21, 2021, P3 filed its answer to the complaint in the Books and Records Action. P3 believes that it has produced all documents sought in the Books and Records Action. While the matter is pending, there are no outstanding requests associated with the Books and Records Action.
Hudson Class D Dispute
On June 11, 2021, Hudson Vegas Investment SPV, LLC (“Hudson”), a holder of P3’s Class D Units, filed an action in the Delaware Court of Chancery captioned Hudson Vegas Investments SPV, LLC v. Chicago Pacific Founders Fund, L.P., et al., C.A. No. 2021-0518-JTL (the “Hudson Action”), in which it challenged the Business Combinations. Specifically, Hudson purports to assert claims against P3, certain managers that were on the P3 Board of Managers, certain of its officers, and Chicago Pacific Founders Fund, L.P. (“CPF”) for breach of P3’s then-existing LLC agreement (the “LLC Agreement”) (against P3 and CPF), breach of fiduciary duty (against certain of P3’s officers) and breach of contract claims related to the then-existing LLC Agreement (against the P3 Board of Managers) in connection with the process leading up to, and approval of, the Business Combinations. In the Hudson Action, Hudson sought to enjoin the consummation of the Business Combinations and seeks a declaration that the Business Combinations violate its rights under the P3 then-existing LLC Agreement, a declaration that certain managers on the P3 Board of Managers and certain of P3’s officers breached their fiduciary duties, and money damages including attorneys’ fees.
On June 13, 2021, P3 filed an action in the Delaware Court of Chancery captioned P3 Health Group Holdings, L.L.C. v. Hudson Vegas Investment SPV, LLC, C.A. No. 2021-0519-JTL (the “P3 Action”). In the P3 Action, P3 seeks: (i) a declaration that the Business Combinations do not violate Section 3.10 of P3’s Existing LLC Agreement; and (ii) reformation of a provision of P3’s Existing LLC Agreement. The P3 Action was consolidated with the Hudson Action. The combined cases are captioned In re P3 Health Group Holdings, L.L.C, C.A. No. 2021-0518-JTL.
On June 22, 2021, Hudson filed a motion for expedited proceedings in the Hudson Action in which it sought expedited discovery and a hearing on its motion for preliminary injunction to enjoin the consummation of the Business Combinations. The defendants in the Hudson Action determined not to oppose Hudson’s motion for expedited proceedings and engaged in expedited discovery in advance of a preliminary injunction hearing that took place September 9, 2021.
On September 14, 2021, the Court of Chancery issued an oral ruling denying Hudson’s motion for preliminary injunction due to the lack of probability of success on the merits or, with respect to the Section 5.10 of the then-existing P3 LLC Agreement (the “Purchase Option”) only, lack of a showing of irreparable harm based on the condition that the escrow described below be created. In its ruling, the Court held that Hudson had not demonstrated a reasonable probability of success on its claims, except for its claim under the Purchase Option, which – if applicable – would allow Hudson to exercise an option to purchase additional equity interests in P3 in connection with the pending transaction with Foresight. With respect to the Purchase Option claim, the Court declined to address the merits and instead denied Hudson’s motion finding that Hudson failed to demonstrate irreparable harm. This ruling was made subject to the condition that Defendants memorialize their commitment to escrow, pending final resolution of this action, the consideration Hudson would be entitled to receive if it is determined that the Purchase Option can be validly exercised, in a stipulation filed with the Court. On September 17, 2021, Defendants filed a stipulation and proposed order regarding escrow which confirmed their commitment to do so and to cause the Payment Spreadsheet (as that term is defined in Section 2.01(f) of the Merger Agreement) to
52
provide that such consideration will be directed to such escrow. The Court granted and entered the stipulation and proposed order on September 17, 2021.
The former members of P3 (other than Hudson) have agreed to indemnify the Company and P3 LLC following the Closing, for any damages, including reasonable attorney’s fees, arising out of matters relating to the dispute with Hudson.
On December 27, 2021, Hudson filed a Motion for Leave to Amend the Verified Complaint. The proposed Amended Complaint contains certain of Hudson’s original claims and also adds additional claims, including bad faith breach of contract claims against certain of the former P3 Managers, an additional contractual claim against P3, and a tortious interference with contract claim against Foresight Acquisition Corp., Foresight Acquisition Corp. II, P3 Partners Inc., Sameer Mathur, and Greg Wasson. Defendants informed Hudson that they did not oppose the Motion for Leave to Amend the Verified Complaint, and on February 4, 2022, Hudson filed its Verified Amended Complaint.
On March 9, 2022, all Defendants moved to dismiss the Verified Amended Complaint. The briefing on Defendants’ Motion to Dismiss was completed on May 17, 2022.
On March 25, 2022, Hudson served its Second Request for the Production of Documents directed to Defendants, and on April 14, 2022, Defendants filed a Motion to Stay Discovery and for Protective Order Pending Resolution of Motions to Dismiss (the “Motion to Stay”). Defendants served formal responses and objections to the Second Request for the Production of Documents on April 25, 2022. Hudson opposed the Motion to Stay on May 12, 2022. On July 13, 2022, the Court heard argument on both the Motions to Dismiss and the Motion to Stay and took the matters under advisement.
From September 12, 2022 and through November 7, 2022, the Court issued a series of Orders ruling on the Motions to Dismiss. Such Orders provided for the dismissal with prejudice of (i) Hudson’s claim to a Purchase Option and (ii) Hudson’s claim to a priority right to cash distributed as a result of the transactions; and (iii) the denial of each of the various Motions to Dismiss for lack of personal jurisdiction.
The Court granted in part and denied in part a motion to dismiss filed by Mr. Leisure, Mr. Kazarian, Mr. Abdou, Mr. Bacchus, Mr. Garrett, Mr. Price, Ms. Glisson, and Mr. Leavitt (the “Manager Defendants”) with respect to Hudson’s claim for bad faith breach of contract under a variety of theories. The Court also granted in part and denied in part the Manager Defendants’ motion, permitting Hudson’s bad faith breach of contract claim to proceed against the Manager Defendants on certain theories, but dismissing other theories, including that the Manager Defendants committed a bad faith breach of contract by failing to act in good faith to facilitate the Purchase Option.
On November 7, 2022, the Court issued an order denying in part and granting in part the motion to dismiss the breach of fiduciary claims against the officer Defendants, including Mr. Kazarian, Mr. Abdou, Mr. Bacchus, Ms. Glisson, and Ms. Puathasnanon. The Court allowed certain theories for these claims to survive the motion to dismiss, but it dismissed other theories for the claims, including that the officers “fail[ed] to engage in an adequate auction or sale process.” On November 9, 2022, the Court issued an order denying the motion to dismiss the claim against Mr. Mathur for tortious interference with Hudson’s contract rights. The parties are now currently engaged in discovery on Hudson’s surviving claims.
Item 4. Mine Safety Disclosures.
Not applicable.
53
PART II
Item 5. Market for Registrant’s Common Equity, Related Stockholder Matters and Issuer Purchases of Equity Securities.
Market Information
On December 3, 2021, our Class A common stock and warrants began trading on the Nasdaq Capital Market under the symbols “PIII” and “PIIIW,” respectively. There is no trading market for shares of our Class V common stock.
Holders
As of March 15, 2023, there were 14 holders of record of our Class A common stock and 56 holders of Class V common stock. The actual number of holders of our Class A common stock is greater than the number of record holders and includes holders whose Class A common stock are held in street name by brokers and other nominees.
Dividend Policy
We have never declared or paid any cash dividends on our capital stock. We currently intend to retain all available funds and future earnings, if any, for the operation and expansion of our business and do not anticipate declaring or paying any dividends in the foreseeable future. Any future determination related to our dividend policy will be made at the discretion of our board of directors after considering our financial condition, results of operations, capital requirements, business prospects and other factors the board of directors deems relevant, and subject to the restrictions contained in any financing instruments. The terms of our existing Term Loan Facility (as defined below) preclude us from paying cash dividends without consent. Our ability to declare dividends may also be limited by restrictive covenants pursuant to any other future debt or equity financing agreements.
Stock Performance Graph
The following graph and related information provide a comparison of the cumulative total return for our Class A common stock, the S&P 500 Index and the S&P 500 Healthcare Index between April 6, 2021 (the date our common stock commenced trading on Nasdaq) through December 31, 2022. All values assume an initial investment of $100 and reinvestment of any dividends. The comparisons are based on historical data and are not indicative of, nor intended to forecast, the future performance of our Class A common stock.
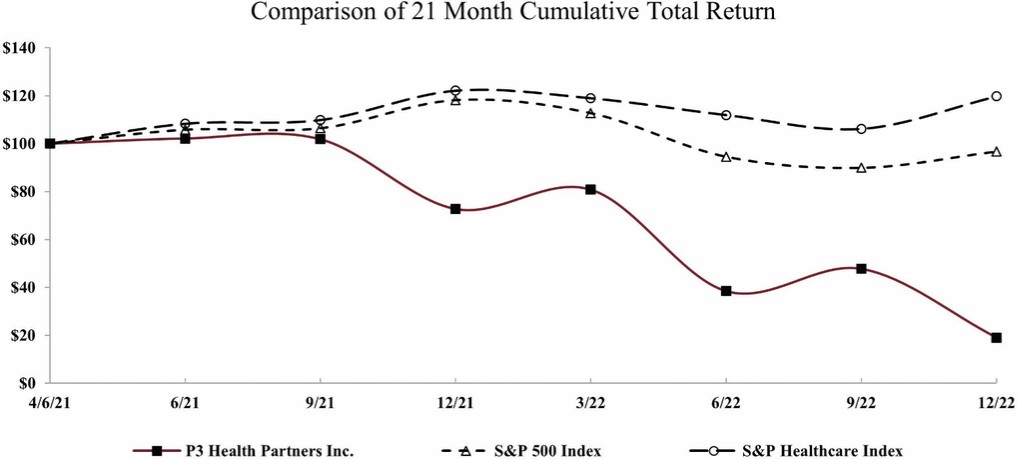
54
The performance graph above and related information shall not be deemed to be “filed” for purposes of Section 18 of the Exchange Act, or otherwise subject to the liabilities of that section or Sections 11 and 12(a)(2) of the Securities Act, and shall not be incorporated by reference into any registration statement or other document filed by us with the SEC, whether made before or after the date of this Form 10-K, regardless of any general incorporation language in such filing, except as shall be expressly set forth by specific reference to such filing.
Recent Sales of Unregistered Securities
There was no unregistered sale of our equity securities during the fiscal year ended December 31, 2022, that were not otherwise disclosed in a Current Report on Form 8-K.
Purchases of Equity Securities by the Issuer and Affiliated Purchaser
None.
Item 6. [Reserved]
55
Item 7. Management’s Discussion and Analysis of Financial Condition and Results of Operations.
The following discussion and analysis is intended to provide the reader with an understanding of our business, including an overview of our results of operations and liquidity. It should be read in conjunction with the consolidated financial statements and related notes to the consolidated financial statements included elsewhere in this Form 10-K. This discussion contains forward-looking statements, such as those relating to our plans, objectives, expectations, intentions and beliefs that involve numerous risks and uncertainties. Our actual results may differ materially from those anticipated in any forward-looking statements as a result of many factors, including those set forth under “Cautionary Statement Regarding Forward-Looking Statements,” “Item 1A. Risk Factors” and elsewhere in this Form 10-K. Our historical results are not necessarily indicative of the results that may be expected for any periods in the future.
Overview
P3 is a patient-centered and physician-led population health management company. We strive to offer superior care to all those in need. We believe that the misaligned incentives in the FFS healthcare payment model and the fragmentation between physicians and care teams has led to sub-optimal clinical outcomes, limited access, high spending and unnecessary variability in the quality of care. We believe that a platform such as ours, which helps to realign incentives and focuses on treating the full patient, is uniquely positioned to address these healthcare challenges.
We have leveraged the expertise of our management team’s more than 20 years of experience in population health management, to build our “P3 Care Model.” The key attributes that differentiate P3 include: 1) patient-focused model, 2) physician-led model, and 3) our broad delegated model. Our model operates by entering into arrangements with payors providing for monthly payments to manage the total healthcare needs of members attributed to our primary care physicians. In tandem, we enter into arrangements directly with existing physician groups or independent physicians in the community to join our VBC network. In our model, physicians are able to retain their independence and entrepreneurial spirit, while gaining access to the tools, teams and technologies that are key to success in a VBC model, all while sharing in the savings from successfully improving the quality of patient care and reducing costs.
We operate in the $829 billion Medicare market, which covers approximately 65 million eligible lives as of 2021. Our core focus is the MA market, which makes up approximately 48% of the overall Medicare market, or nearly 28 million Medicare eligible lives in 2022. Medicare beneficiaries may enroll in a Medicare Advantage plan, under which payors contract with the CMS to provide a defined range of healthcare services that are comparable to Medicare FFS (which is also referred to as “traditional Medicare”).
We predominantly enter into capitated contracts with the nation’s largest health plans to provide holistic, comprehensive healthcare to Medicare Advantage members. Under the typical capitation arrangement, we are entitled to PMPM fees from payors to provide a defined range of healthcare services for Medicare Advantage health plan members attributed to our PCPs. These PMPM fees comprise our capitated revenue and are determined as a percent of the premium (“POP”) payors receive from CMS for these members. Our contracted recurring revenue model offers us highly predictable revenue and rewards us for providing high-quality care rather than driving a high volume of services. In this capitated arrangement, our goals are well-aligned with payors and patients alike—the more we improve health outcomes, the more profitable we will be over time.
Under this capitated contract structure, we are generally responsible for all members’ medical costs across the care continuum, including, but not limited to emergency room and hospital visits, post-acute care admissions, prescription drugs, specialist physician spend, and primary care spend. Keeping members healthy is our primary objective. When they need medical care, delivery of the right care in the right setting can greatly impact outcomes. When our members need care outside of our network of PCPs, we utilize a number of tools including network management, utilization management and claims processing to ensure that the appropriate quality care is provided.
Our company was formed in 2017 and our first at-risk contract became effective on January 1, 2018. We have demonstrated an ability to rapidly scale, primarily entering markets with our affiliate physician model, and expanding to a PCP network of approximately 2,800 physicians, in 15 markets (counties) across five states in five full years of operations as of December 31, 2022. Our platform has enabled us to grow our revenue by an average of 99% annually from December 31, 2018 to December 31, 2022. As of December 31, 2022, our PCP network served approximately 100,400 at-risk MA members. We believe we have significant growth
56
opportunities available to us across existing and new markets, with less than 1% of the 502,000 PCPs in the U.S. currently included in our physician network.
COVID-19 and Macroeconomic Update
The COVID-19 pandemic continues to evolve, with pockets of resurgence and the emergence of variant strains contributing to continued uncertainty about its scope, duration, severity, trajectory, and lasting impact. COVID-19 disproportionately impacts older adults, especially those with chronic illnesses, which describes many of our patients. Due to our recurring contracted revenue model, the COVID-19 pandemic did not have a material impact on P3’s revenue during 2021 and 2022. Nearly 99% the Company’s total revenue during the year ended December 31, 2022 is recurring, consisting of fixed monthly PMPM capitation payments received from MA health plans. We estimate that we have incurred approximately $95.5 million of direct costs in medical claims expense related to COVID-19 claims during the period from March 1, 2020 through December 31, 2022. We expect to incur additional COVID-19 related costs given the volume of positive cases and “breakthrough” cases (positive cases in vaccinated patients) present in our markets.
Because of the nature of capitation arrangements, the full impact of the COVID-19 pandemic may not be fully reflected in our results of operations and overall financial condition until future periods. The full extent to which COVID-19 will directly or indirectly impact our future results of operations and financial condition will depend on multiple factors. In addition, the economy may continue to be impacted as a result of the COVID-19 pandemic, including any resurgences to infections, and actions taken in response to it. Such factors include, but are not limited to, the scope and duration of stay-at-home practices and business closures and restrictions, government-imposed or recommended suspensions of elective procedures, and expenses required for supplies and personal protective equipment. Because of these factors, management may not be able to fully estimate the length or severity of the impact of the pandemic on our business. However, management will continue to closely evaluate and monitor the nature and extent of these potential impacts to our business, results of operations and liquidity.
Business Combinations
On December 3, 2021, we consummated the Business Combinations by and among Foresight and P3 Health Group Holdings and the other parties thereto. As a result of the Business Combinations (see Note 5 “Business Combinations” to the consolidated financial statements included elsewhere in this Form 10-K), the Company was deemed to be the acquirer for accounting purposes, and P3 Health Group Holdings, which is the business conducted prior to the closing of the Business Combinations, was deemed to be the acquiree and accounting predecessor. The Business Combinations were accounted for as a business combination using the acquisition method of accounting, and the Successor’s (defined below) financial statements reflect a new basis of accounting that is based on the fair value of net assets acquired. As a result of the application of the acquisition method of accounting as of the effective time of the Business Combinations, the financial statements of P3 Health Group Holdings as “Predecessor” for the periods prior to the Closing Date and of the Company as “Successor” for the periods after the Closing Date, including the consolidation of P3 Health Group Holdings, are presented on different bases for the year ended December 31, 2022, the Successor Period, and the Predecessor Period. The historical financial information of the Company (the acquirer) has not been reflected in the Predecessor Period financial statements.
Recent Acquisitions
On December 27, 2021 and December 31, 2021, respectively, the Company acquired the net assets of Omni IPA Medical Group, Inc. (“Omni”) and 100% of the equity interests of Medcore Health Plan, Inc. (“Medcore HP”) for a total purchase price of $40.0 million, including contingent consideration of $3.5 million (together, the “Medcore Acquisition”). Medcore HP is a health plan licensed under the California Knox-Keene Health Care Service Plan Act of 1975 (the “Knox Keene Act”) and Omni is an independent practice association located in California. Omni serves as Medcore HP’s contracted physician network providing medical services to Medcore HP’s patients and members.
The Knox Keene Act requires entities that participate in downstream risk-sharing arrangements, including global risk and VBC arrangements, to be licensed health plans. Our acquisition of Medcore HP allows our network of providers to participate in global risk and VBC arrangements with California payors. Through this transaction, we intend to replicate our affiliate model to contract with local physicians and grow our network in California.
57
Key Factors Affecting our Performance
Growing Medicare Advantage Membership on Our Platform
Membership and revenue are tied to the number of members attributed to our physician network by our payors. We believe we have multiple avenues to serve additional members, including through:
| ● | Growth in membership under our existing contracts and existing markets: |
| o | Patients who are attributed to our physician network who (a) age into Medicare and elect to enroll in MA or (b) elect to convert from Medicare FFS to MA. |
| ● | Adding new contracts (either payor contracts or physician contracts) in existing markets. |
| ● | Adding new contracts (either payor contracts or physician contracts) in adjacent and new markets. |
The strength of our affiliate physician model and its multiple avenues of growth is evident by our growth from 2018 to December 31, 2022.
At December 31, 2022, the number of MA at-risk members on our platform was approximately 100,400 compared to approximately 67,000 at December 31, 2021, representing a compound annual growth rate (“CAGR”) of 41% over this period. The table below illustrates membership growth from 2021 to 2022:
| December 31, |
|
|
| |||
2022 |
| 2021 | CAGR |
| |||
MA at-risk members |
| 100,400 |
| 67,000 |
| 41 | % |
Year-over-year % change | 50 | % | 32 | % | |||
Growing Existing Contract Membership
According to CMS, the Medicare market covers approximately 65 million eligible lives as of 2021. MA penetration of the Medicare beneficiary population has increased from 26% in 2011 to 48% in 2022 of the overall Medicare beneficiary market making up nearly 28 million Medicare eligible lives. As new patients age-in to Medicare and enroll in MA through our payors, they become attributed to our network of physicians with little incremental cost to us.
In addition to age-ins, Medicare eligible patients can change their enrollment selections during select periods throughout the year. Our sales and marketing teams actively work with local community partners to connect with Medicare eligible patients and make them aware of their healthcare choices and the services that we offer with our VBC model, including greater access to their physicians and customized care plans catered to their needs. The ultimate effect of our marketing efforts is increased awareness of P3 and additional patients choosing us as their primary care provider. We believe that our marketing efforts also help to grow our payor partners’ membership base as we grow our own patient base and help educate patients about their choices on Medicare, further aligning our model with that of healthcare payors.
Growing Membership in Adjacent and New Markets
Our affiliate model allows us to quickly and efficiently enter into new and adjacent markets in two ways: 1) partnering with payors and 2) partnering with providers. Because our model honors the existing patient-provider relationship, we are able to deploy our care model around existing physicians in a given a market. By utilizing the local healthcare infrastructure, we can quickly build a network of PCPs to serve the healthcare needs of contracted members.
Our business development and managed care teams maintain an active pipeline of new partnership opportunities for both providers and payors. These potential opportunities are developed through significant inbound interest and the deep relationships our team has developed with their more than 20 years of experience in the VBC space and our proactive assessment of expansion markets. When choosing a market to enter, we make our decision on a county-by-county basis across the United States. We look at various
58
factors including: (i) population size, (ii) payor participants and concentration, (iii) health system participants and concentration, and (iv) competitive landscape.
When entering a new market, we supplement the existing physician network with local market leadership teams and support infrastructure to drive the improvement in medical cost and quality. When entering an adjacent market, we are able to leverage the investments we previously made to have a faster impact on our expanded footprint. We have historically demonstrated success in effectively growing into new and adjacent markets. As of December 31, 2022, we operate in 15 markets, markets being counties, across five states. P3 is actively pursuing opportunities to expand operations to additional states in the Southwest and Midwest. One of the primary uses of the net proceeds we obtained from the consummation of the Business Combinations and the concurrent private placement of 20,370,307 shares (the “PIPE Shares”) of our Class A common stock, for an aggregate purchase price of $203.7 million (the “PIPE Investment”) is to fund the investment required to enter these new markets and to take on additional new contracts.
Growing Membership in Existing Markets
Once established in a market, we have an opportunity to efficiently expand both our provider and payor contracts. Given the benefits PCPs experience from joining our P3 Care Model, which offers providers the teams, tools and technologies to better support their patient base, we often experience growth in our affiliate network after entering a market. Because of the benefits, we have also historically experienced high retention with our affiliate providers. From 2018 through 2022, we experienced a 98% physician retention rate in our affiliate provider network. By expanding our affiliate provider network and adding new physicians to the P3 network, we can quickly increase the number of contracted at-risk members under our existing health plan arrangements.
Additionally, by expanding the number of contracted payors, we can leverage our existing infrastructure to quickly increase our share of patients within our physician network. We have a proven ability to manage medical costs and improve clinical outcomes of our lives under management on behalf of our payor partners. This is evidenced by the receipt of inbound partnership requests from payors to improve growth, quality and profitability in their markets.
Growing Capitated Revenue Per Member
Medicare pays capitation using a risk adjusted model, which compensates payors based on the health status, or acuity, of each individual member. Payors with higher acuity members receive a higher payment and those with lower acuity members receive a lower payment. Moreover, some of our capitated revenue also includes adjustments for performance incentives or penalties based on the achievement of certain clinical quality metrics as contracted with payors. Given the prevalence of FFS arrangements, our patients often have historically not participated in a VBC model, and therefore their health conditions are poorly documented. Through the P3 Care Model, we determine and assess the health needs of our patients and create an individualized care plan consistent with those needs. We capture and document health conditions as a part of this process. We expect that our PMPM revenue will continue to improve the longer members participate in our care model as we better understand and assess their health status (acuity) and coordinate their medical care.
Effectively Managing Member Medical Expense
Our medical claims expense is our largest expense category, representing 82% of our total operating expenses (excluding goodwill impairment) for the year ended December 31, 2022. We manage our medical costs by improving our members access to healthcare. Our care model focuses on maintaining health and leveraging the primary care setting as a means of avoiding costly downstream healthcare costs, such as emergency department visits and acute hospital inpatient admissions. The power of our model is reflected in the relative performance of our network when compared to local FFS benchmarks.
Achieving Operating Efficiencies
As a result of our affiliate model and ability to leverage our existing local and national infrastructure, we generate operating efficiencies at both the market and enterprise level. Our local corporate, general and administrative expense, which includes our local leadership, care management teams and other operating costs to support our markets, are expected to decrease over time as a percentage of revenue as we add members to our existing contracts, grow membership with new payor and physician contracts, and our revenue subsequently increases. Our corporate general and administrative expenses at the enterprise level include resources and technology to support payor contracting, quality, data management, delegated services, finance and legal functions. While we expect
59
our absolute investment in our enterprise resources to increase over time, we expect our investment will decrease as a percentage of revenue when we are able to leverage our infrastructure across a broader group of at-risk members. We expect our corporate, general and administrative expenses to increase in absolute dollars in the future as we continue to invest to support growth of our business, as well as due to the costs required to operate as a public company, including insurance coverage, investments in internal audit, investor relations and financial reporting functions, fees paid to the Nasdaq Stock Market, and increased legal and audit fees.
Impact of Seasonality
Our operational and financial results reflect some variability depending upon the time of year in which they are measured. This variability is most notable in the following areas:
At-Risk Member Growth. While new members are attributed to our platform throughout the year, we experience the largest portion of our at-risk member growth during the first quarter. Contracts with new payors typically begin on January 1, at which time new members become attributed to our network of physicians. Additionally, new members are attributed to our network on January 1, when plan enrollment selections made during the prior Annual Enrollment Period from October 15 through December 7 of the prior year take effect.
Revenue Per Member. Our revenue is based on percentage of premium we have negotiated with our payors as well as our ability to accurately and appropriately document the acuity of a member’s health status. We experience some seasonality with respect to our per member revenue as it will generally decline over the course of the year. In January of each year, CMS revises the risk adjustment factor for each patient based upon health conditions documented in the prior year, leading to an overall increase in per-patient revenue. As the year progresses, our per-patient revenue declines as new patients join us typically with less complete or accurate documentation (and therefore lower risk-adjustment scores) and patients with more severe acuity profiles (and, therefore, higher per member revenue rates) expire.
Medical Costs. Medical expense is driven by utilization of healthcare services by our attributed membership. Medical expense will vary seasonally depending on a number of factors, including the weather and the number of business days. Certain illnesses, such as the influenza virus, are far more prevalent during colder months of the year, which will result in an increase in medical expenses during these time periods. We would therefore expect to see higher levels of per-member medical expense in the first and fourth quarters. Business days can also create year-over-year comparability issues if one year has a different number of business days compared to another.
Non-GAAP Financial Measures and Key Performance Metrics
We use certain financial measures, which are not calculated in accordance with accounting principles generally accepted in the U.S. (“GAAP”), as well as certain key performance metrics, to supplement our consolidated financial statements. The measures set forth below should not be considered in isolation from, or as a substitute for, financial information presented in compliance with GAAP, and non-GAAP financial measures and key performance metrics as used by us may not be comparable to similarly titled measures used by other companies. Our presentation of these measures should not be construed as an inference that our future results will be unaffected by unusual or non-recurring items. The presentation of non-GAAP financial measures and key performance metrics provides additional information to investors regarding our results of operations that our management believes is useful for identifying trends, analyzing and benchmarking the performance of our business.
Non-GAAP Financial Measures
Adjusted EBITDA
The key non-GAAP metric we utilize to measure our profitability and performance is Adjusted EBITDA. We present Adjusted EBITDA because we believe it helps investors understand underlying trends in our business and facilitates an understanding of our operating performance from period to period because it facilitates a comparison of our recurring core business operating results.
By definition, EBITDA consists of net income (loss) before interest, income taxes, depreciation and amortization. We define Adjusted EBITDA as EBITDA, further adjusted to exclude the effect of certain supplemental adjustments, such as mark-to-market warrant gain/loss, premium deficiency reserves, equity-based compensation expense, and certain other items that we believe are not
60
indicative of our core operating performance. Our definition of Adjusted EBITDA may not be the same as the definitions used in any of our debt agreements.
Adjusted EBITDA is not a measure of performance or liquidity calculated in accordance with GAAP. It is unaudited and should not be considered an alternative to, or more meaningful than, net income (loss) as an indicator of our operating performance. Uses of cash flows that are not reflected in Adjusted EBITDA include capital expenditures, interest payments, debt principal repayments, and other expenses defined above, which can be significant. As a result, Adjusted EBITDA should not be considered as a measure of our liquidity.
Because of these limitations, Adjusted EBITDA should not be considered in isolation or as a substitute for performance measures calculated in accordance with GAAP. We compensate for these limitations by relying primarily on our GAAP results and using Adjusted EBITDA on a supplemental basis. You should review the reconciliation of net loss to Adjusted EBITDA set forth below and not rely on any single financial measure to evaluate our business.
The following table sets forth a reconciliation of our net loss, the most directly comparable GAAP metric, to Adjusted EBITDA (in thousands):
| Successor | Predecessor | ||||||||
Year Ended | December 3, 2021 | January 1, 2021 | ||||||||
December 31, | through December | through December | ||||||||
| 2022 |
| 31, 2021 |
|
| 2, 2021 | ||||
Net loss | $ | (1,561,557) | $ | (57,938) | $ | (146,400) | ||||
Interest expense, net |
| 11,404 |
| 893 |
| 9,824 | ||||
Depreciation and amortization expense |
| 87,289 |
| 7,150 |
| 1,574 | ||||
Provision for income taxes |
| 1,862 |
| — |
| — | ||||
Mark-to-market of stock warrants |
| (9,865) |
| (2,272) |
| 7,665 | ||||
Premium deficiency reserve |
| (11,461) |
| 26,277 |
| 11,559 | ||||
Equity-based compensation |
| 19,404 |
| 4,635 |
| 3,701 | ||||
Transaction and other related costs(1) |
| 14,050 |
| — |
| 37,563 | ||||
Goodwill impairment |
| 1,314,952 |
| — |
| — | ||||
Other(2) |
| 6,008 |
| 429 |
| (147) | ||||
Adjusted EBITDA loss | $ | (127,914) | $ | (20,826) | $ | (74,661) | ||||
| (1) | Transaction and other related costs consist of accounting, legal, and advisory fees and bonus incurred related to the Business Combinations, the Medcore Acquisition, and other transactions that were completed, pending, or abandoned. |
| (2) | During the year ended December 31, 2022, other consists of (i) income related to the release of indemnity funds previously escrowed as part of the Medcore Acquisition and (ii) interest income, offset by (iii) accounting, legal, and professional services expenses incurred related to the restatement of our consolidated financial statements for the years ended December 31, 2020, 2019, and 2018 and the condensed consolidated financial statements for the quarterly periods ended March 31, 2021, June 30, 2021, September 30, 2021, March 31, 2020, June 30, 2020, and September 30, 2020, (iv) expenses for third-party consultants to assist us with the development, implementation, and documentation of new and enhanced internal controls and processes for compliance with Sarbanes-Oxley Section 404(b), and (v) severance expense. During the combined Successor and Predecessor periods included in the year ended December 31, 2021, other consists of interest income offset by valuation allowance on our notes receivable. |
Medical Margin
Medical margin is a non-GAAP financial metric. We present medical margin because we believe it helps investors understand underlying trends in our business and facilitates an understanding of our operating performance from period to period because it facilitates a comparison of our recurring core business operating results.
Medical margin represents the amount earned from capitation revenue after medical claims expenses are deducted. Medical claims expenses represent costs incurred for medical services provided to our members. As our platform grows and matures over time, we expect medical margin to increase in absolute dollars; however, medical margin PMPM may vary as the percentage of new members brought onto our platform fluctuates. New membership added to the platform is typically dilutive to medical margin PMPM. Furthermore, in light of COVID-19, we continue to evaluate the ultimate impact of the pandemic on medical margin.
61
Medical margin should not be considered in isolation or as a substitute for performance measures calculated in accordance with GAAP. We compensate for these limitations by relying primarily on our GAAP results and using medical margin on a supplemental basis. You should review the reconciliation of operating loss to medical margin set forth below and not rely on any single financial measure to evaluate our business.
The following table presents our medical margin (dollars in thousands):
| Successor |
|
| Predecessor | ||||||
Year Ended | December 3, 2021 | January 1, 2021 | ||||||||
December 31, | through December | through December | ||||||||
2022 | 31, 2021 | 2, 2021 | ||||||||
Capitated revenue | $ | 1,034,800 | $ | 57,224 | $ | 567,735 | ||||
Less: medical claims expenses |
| (972,725) |
| (62,344) |
| (550,869) | ||||
Medical margin | $ | 62,075 | $ | (5,120) | $ | 16,866 | ||||
The following table sets forth a reconciliation of our operating loss, the most directly comparable GAAP metric, to medical margin (in thousands):
| Successor |
|
| Predecessor | ||||||
Year Ended | December 3, 2021 | January 1, 2021 | ||||||||
December 31, | through December | through December | ||||||||
2022 | 31, 2021 | 2, 2021 | ||||||||
Operating loss | $ | (1,560,913) | $ | (58,888) | $ | (129,058) | ||||
Other patient service revenue |
| (14,671) |
| (1,538) |
| (10,867) | ||||
Other medical expenses |
| 84,499 |
| 4,533 |
| 41,596 | ||||
Premium deficiency reserve |
| (11,461) |
| 26,277 |
| 11,559 | ||||
Corporate, general and administrative expenses |
| 157,284 |
| 16,983 |
| 100,243 | ||||
Sales and marketing expenses |
| 5,096 |
| 364 |
| 1,818 | ||||
Depreciation and amortization |
| 87,289 |
| 7,149 |
| 1,575 | ||||
Goodwill impairment |
| 1,314,952 |
| — |
| — | ||||
Medical margin | $ | 62,075 | $ | (5,120) | $ | 16,866 | ||||
Network Contribution
Network contribution is a non-GAAP financial metric. We present network contribution because we believe it helps investors understand underlying trends in our business and facilitates a broader understanding of our operating performance from period to period because it facilitates a comparison of our recurring core business operating results.
We define network contribution as total operating revenue less the sum of: (i) medical claims expenses and (ii) other medical expenses including physician compensation expense related to surplus sharing and bonuses and other direct medical expenses incurred to improve care for our members. We believe this metric provides insight into the economics of the P3 Care Model, as it includes all medical claims expense associated with our members’ care as well as partner compensation and additional medical costs we incur as part of our aligned partnership model. Other medical expenses are largely variable and proportionate to the level of surplus in each respective market, among other cost factors.
Network contribution should not be considered in isolation or as a substitute for performance measures calculated in accordance with GAAP. We compensate for these limitations by relying primarily on our GAAP results and using network contribution on a supplemental basis. You should review the reconciliation of operating loss to network contribution set forth below and not rely on any single financial measure to evaluate our business.
62
The following table presents our network contribution (dollars in thousands):
| Successor |
|
| Predecessor | ||||||
Year Ended | December 3, 2021 | January 1, 2021 | ||||||||
December 31, | through December | through December | ||||||||
2022 | 31, 2021 | 2, 2021 | ||||||||
Total operating revenue | $ | 1,049,471 | $ | 58,762 | $ | 578,602 | ||||
Less: medical claims expenses |
| (972,725) |
| (62,345) |
| (550,869) | ||||
Less: other medical expenses |
| (84,499) |
| (4,532) |
| (41,596) | ||||
Network contribution | $ | (7,753) | $ | (8,115) | $ | (13,863) | ||||
The following table sets forth a reconciliation of our operating loss, the most directly comparable GAAP metric, to network contribution (in thousands):
| Successor |
|
| Predecessor | ||||||
Year Ended | December 3, 2021 | January 1, 2021 | ||||||||
December 31, | through December | through December | ||||||||
2022 | 31, 2021 | 2, 2021 | ||||||||
Operating loss | $ | (1,560,913) | $ | (58,888) | $ | (129,058) | ||||
Premium deficiency reserve |
| (11,461) |
| 26,277 |
| 11,559 | ||||
Corporate, general and administrative expenses |
| 157,284 |
| 16,983 |
| 100,243 | ||||
Sales and marketing expenses |
| 5,096 |
| 364 |
| 1,818 | ||||
Depreciation and amortization |
| 87,289 |
| 7,149 |
| 1,575 | ||||
Goodwill impairment |
| 1,314,952 |
| — |
| — | ||||
Network contribution | $ | (7,753) | $ | (8,115) | $ | (13,863) | ||||
Key Performance Metrics
We monitor the following financial and performance metrics to help us evaluate our business, identify trends affecting our business, formulate business plans and make strategic decisions (dollars in thousands):
Successor | Predecessor | |||||||||
As of and For the Year Ended | As of and from December 3, 2021 | January 1, 2021 | ||||||||
December 31, | through December | through December | ||||||||
| 2022 |
| 31, 2021 |
|
| 2, 2021 | ||||
MA at-risk members |
| 100,400 |
| 67,000 |
| N/A | ||||
Affiliate PCPs | 2,800 | 2,100 | N/A | |||||||
Platform support costs |
| $ | 119,167 |
| $ | 14,292 | $ | 78,293 | ||
MA At-Risk Members
MA at-risk members represent the approximate number of MA members for whom we receive a fixed PMPM fee under capitation arrangements as of the end of the period.
Affiliate Primary Care Physicians
Affiliate primary care physicians represent the approximate number of primary care physicians included in our affiliate network, with whom members may be attributed under our capitation arrangements, as of the end of the period.
Platform Support Costs
Our platform support costs, which include regionally-based support personnel and other operating costs to support our markets, are expected to decrease over time as a percentage of revenue as our physician partners add members and our revenue grows. Our operating expenses at the enterprise level include resources and technology to support payor contracting, clinical program
63
development, quality, data management, finance, and legal functions. We exclude costs related to the operations of our owned medical clinics and wellness centers.
The table below represents costs to support our markets and enterprise functions, which are included in corporate, general and administrative expenses (dollars in thousands):
| Successor |
|
| Predecessor |
| ||||||
Year Ended | December 3, 2021 | January 1, 2021 |
| ||||||||
December 31, | through December | through December |
| ||||||||
2022 | 31, 2021 | 2, 2021 |
| ||||||||
Platform support costs | $ | 119,167 | $ | 14,292 | $ | 78,293 | |||||
% of Total operating revenue |
| 11.4 | % |
| 24.3 | % |
| 13.5 | % | ||
Key Components of Results of Operations
Revenue
Capitated revenue. We contract with health plans using an at-risk model. Under the at-risk model, we are responsible for the cost of all covered health care services provided to members assigned by the health plans to the Company in exchange for a fixed payment, which generally is a POP based on health plans’ premiums received from CMS. Through this capitation arrangement, we stand ready to provide assigned Medicare Advantage members all their medical care via our directly employed and affiliated physician/specialist network.
The premiums health plans receive are determined via a competitive bidding process with CMS and are based on the costs of care in local markets and the average utilization of services by patients enrolled. Medicare pays capitation using a “risk adjustment model,” which compensates providers based on the health status (acuity) of each individual patient. Medicare Advantage plans with higher acuity patients receive higher premiums. Conversely, Medicare Advantage plans with lower acuity patients receive lesser premiums. Under the risk adjustment model, capitation is paid on an interim basis based on enrollee data submitted for the preceding year and is adjusted in subsequent periods after final data is compiled. As premiums are adjusted via this risk adjustment model (via a Risk Adjustment Factor, “RAF”), our PMPM payments will change commensurately with how our contracted Medicare Advantage plans’ premiums change with CMS.
Management determined the transaction price for these contracts is variable as it primarily includes PMPM fees, which can fluctuate throughout the course of the year based on the acuity of each individual enrollee. In certain contracts, PMPM fees also include adjustments for items such as performance incentives or penalties based on the achievement of certain clinical quality metrics as contracted with payors. Capitated revenue is recognized based on an estimated PMPM transaction price to transfer the service for a distinct increment of the series (e.g., month) and is recognized net of projected acuity adjustments and performance incentives or penalties as management can reasonably estimate the ultimate PMPM payment of those contracts. We recognize revenue in the month in which attributed members are entitled to receive healthcare benefits during the contract term. The capitation amount is subject to possible retroactive premium risk adjustments based on the member’s individual acuity.
Other patient service revenue. Other patient service revenue is comprised primarily of encounter-related fees to treat patients outside of our at-risk arrangements at company owned clinics. Other patient service revenue also includes ancillary fees earned under contracts with certain payors for the provision of certain care coordination and other care management services. These services are provided to patients covered by these payors regardless of whether those patients receive their care from our directly employed or affiliated medical groups.
Operating Expenses
Medical expense. Medical expense primarily includes costs of all covered services provided to members by non-P3 employed providers. This also includes an estimate of the cost of services that have been incurred, but not yet reported (“IBNR”). Estimates for incurred claims are based on historical enrollment and cost trends while also taking into consideration operational changes. Future and actual results typically differ from estimates. Differences could result from an overall change in medical expenses per member, changes in member mix or simply due to the addition of new members. IBNR estimates are made on an accrual basis and adjusted in future periods as required. To the extent we revise our estimates of IBNR claims for prior periods up or down, there would be a
64
correspondingly unfavorable or favorable effect on our current period results that may or may not reflect changes in long term trends in our performance.
Premium deficiency reserve. Premium deficiency reserves (“PDR”) are recognized when it is probable that expected future health care costs and maintenance costs under a group of existing contracts will exceed anticipated future premiums and stop-loss insurance recoveries on those contracts. PDR represents the advance recognition of a probable future loss in the current period’s financial statements.
Corporate, general and administrative expense. Corporate, general and administrative expenses include employee-related expenses, including salaries and related costs and equity-based compensation for our executive, technology infrastructure, operations, clinical and quality support, finance, legal, and human resources departments. In addition, general and administrative expenses include all corporate technology and occupancy costs.
Sales and marketing expense. Sales and marketing expenses consist of costs related to patient and provider marketing and community outreach. These expenses capture all costs for both our local and enterprise sales and marketing efforts.
Depreciation and amortization expense. Depreciation expense is associated with our property and equipment, including leasehold improvements, computer equipment and software, furniture and fixtures, and internally developed software. Amortization expense is associated with definite lived intangible assets, including trademarks and tradenames, customer contracts, provider network agreements, and payor contracts.
Other (Income)/Expense
Interest expense, net. Interest expense primarily consists of interest on our Term Loan Facility (as defined herein).
Mark-to-market of stock warrants. Mark-to-market of stock warrants consists of the change in the fair value on the revaluation of warrant liabilities associated with our public, private placement, and forward purchase warrants.
Other. Other consists of gains and losses resulting from other transactions.
Income Taxes
P3 LLC is treated as a partnership for U.S. federal and most applicable state and local income tax jurisdictions. As a partnership, P3 LLC is generally not subject to U.S. federal, state and local income taxes. Any taxable income or loss generated by P3 LLC is passed through to and included within the taxable income or loss of its members, including us, on a pro rata basis. We are subject to U.S. federal income taxes, in addition to state and local income taxes with respect to our allocable share of any taxable income or loss generated by P3 LLC.
Non-controlling Interests
We consolidate the financial results of P3 LLC and report a non-controlling interest on our consolidated statements of operations, representing the portion of net income or loss attributable to the non-controlling interest. The weighted average ownership percentages during the period are used to calculate the net income or loss attributable to P3 Health Partners Inc. and the non-controlling interest.
Results of Operations
The Business Combinations resulted in the presentation of the Company’s consolidated financial statements on different bases for the year ended December 31, 2022, the Successor Period, and the Predecessor Period. The Company has not provided pro forma statements of operations and cash flows for the years ended December 31, 2022 and 2021. Accordingly, references to certain financial results in 2022 and 2021 may not be comparable.
The historical financial information of Foresight (a special purpose acquisition company or a “SPAC”) prior to the Business Combinations has not been included in the Predecessor financial statements as this information has been determined not to be useful to
65
a user of the financial statements. SPACs deposit the proceeds from their initial public offerings into segregated trust accounts until a business combination occurs, at which point they are utilized to fund the business combination. The operations of a SPAC until the closing of a business combination, other than income from the trust account investments and transaction expenses, are nominal. Accordingly, the only activity reported in the Predecessor Period was the operations of P3 LLC. Foresight’s historical financial information is excluded from the Predecessor financial information. Thus, the financial results of the Successor and Predecessor entities are expected to be largely consistent with the exception of certain financial statement line items impacted by the Business Combinations. Management believes reviewing our operating results for the twelve-month period ended December 31, 2021 by combining the results of the Predecessor and Successor periods is more useful in discussing our overall operating performance when compared to the same period in the prior year. When we refer to the year ended December 31, 2021 herein, we are referring to the combined Successor and Predecessor periods contained in the year ended December 31, 2021.
The following discussion and analysis of our results of operations and liquidity compares the year ended December 31, 2022 with the combined results of the Successor and Predecessor periods of 2021.
The following table sets forth our consolidated statements of operations data for the periods indicated (dollars in thousands):
Successor | Predecessor | |||||||||||||||||
Year Ended | December 3, 2021 | January 1, 2021 | ||||||||||||||||
December 31, | % of | through | % of | through | % of | |||||||||||||
| 2022 |
| Revenue(1) |
|
| December 31, 2021 |
| Revenue(1) |
|
| December 2, 2021 |
| Revenue(1) |
| ||||
Operating revenue: |
|
|
|
|
|
|
|
|
| |||||||||
Capitated revenue | $ | 1,034,800 | 99 | % | $ | 57,225 |
| 97 | % | $ | 567,735 |
| 98 | % | ||||
Other patient service revenue |
| 14,671 | 1 | 1,538 |
| 3 | 10,867 |
| 2 | |||||||||
Total operating revenue |
| 1,049,471 | 100 | 58,763 |
| 100 | 578,602 |
| 100 | |||||||||
Operating expense: |
|
|
|
|
|
|
| |||||||||||
Medical expense |
| 1,057,224 | 101 | 66,877 |
| 114 | 592,465 |
| 102 | |||||||||
Premium deficiency reserve |
| (11,461) | (1) | 26,277 |
| 45 | 11,559 |
| 2 | |||||||||
Corporate, general & administrative expense |
| 157,284 | 15 | 16,983 |
| 29 | 100,243 |
| 17 | |||||||||
Sales and marketing expense |
| 5,096 | 0 | 364 |
| 1 | 1,818 |
| — | |||||||||
Depreciation and amortization |
| 87,289 | 8 | 7,149 |
| 12 | 1,575 |
| — | |||||||||
Goodwill impairment | 1,314,952 | 125 | — | — | — | — | ||||||||||||
Total operating expense |
| 2,610,384 | 248 | 117,650 |
| 201 | 707,660 |
| 121 | |||||||||
Operating loss |
| (1,560,913) | (149) | (58,887) |
| (101) | (129,058) |
| (21) | |||||||||
Other income (expense): |
|
|
|
|
|
|
| |||||||||||
Interest expense, net |
| (11,404) | (1) | (851) |
| (2) | (9,824) |
| (2) | |||||||||
Mark-to-market of stock warrants | 9,865 | 1 | 2,272 | 4 | (7,665) | (1) | ||||||||||||
Other |
| 2,757 | 0 | (471) |
| — | 147 |
| — | |||||||||
Total other income (expense) |
| 1,218 | 0 | 950 |
| 2 | (17,342) |
| (3) | |||||||||
Loss before income taxes |
| (1,559,695) | (149) | (57,937) |
| (99) | (146,400) |
| (24) | |||||||||
Provision for income taxes | (1,862) | 0 | — | — | — | — | ||||||||||||
Net loss | (1,561,557) | (149) | (57,937) | (99) | (146,400) | (24) | ||||||||||||
Net loss attributable to redeemable non-controlling interests |
| (1,291,430) | (123) | (47,857) |
| (81) | — |
| — | |||||||||
Net loss attributable to controlling interests | $ | (270,127) | (26) | % | $ | (10,080) |
| (18) | % | $ | (146,400) |
| (24) | % | ||||
(1) | Amounts may not sum due to rounding. |
Revenue
Capitated revenue was $1,034.8 million for the year ended December 31, 2022, an increase of $409.8 million, or 66%, compared to $625.0 million for the combined Successor and Predecessor periods included in the year ended December 31, 2021. This increase was driven primarily by a 50% increase in the total number of at-risk members from 67,000 at December 31, 2021 to 100,400 at December 31, 2022, as we increased the number of health plan contracts from 17 to 24, and a 10% increase in capitation revenue rates, due to increased premiums from patients with a higher average level of acuity. Capitated revenue was approximately 99% and 98% of total operating revenue for the years ended December 31, 2022 and 2021, respectively.
66
Other patient service revenue was $14.7 million for the year ended December 31, 2022, an increase of $2.3 million, or 18%, compared to $12.4 million for the combined Successor and Predecessor periods included in the year ended December 31, 2021. This increase was primarily driven by increased fees associated with care coordination services and additional fees earned at owned clinics. Other patient service revenue was approximately 1% and 2% of total operating revenue for the years ended December 31, 2022 and 2021, respectively.
Operating Expense
Medical Expense
Medical expense was $1,057.2 million for the year ended December 31, 2022, an increase of $397.9 million, or 61%, compared to $659.3 million for the combined Successor and Predecessor periods included in the year ended December 31, 2021. The increase was primarily due to a 50% increase in the total number of at-risk members year-over-year.
Premium Deficiency Reserve
Premium deficiency reserve was a benefit of $11.5 million for the year ended December 31, 2022, a decrease of $49.3 million, or 130%, compared to expense of $37.8 million for the combined Successor and Predecessor periods included in the year ended December 31, 2021. The change was due to management’s assessment of the profitability of contracts, wherein increased membership and the maturation of our overall contractual arrangements are expected to reduce our future losses.
Corporate, General and Administrative Expense
Corporate, general and administrative expense was $157.3 million for the year ended December 31, 2022, an increase of $40.1 million, or 34.2%, compared to $117.2 million for the combined Successor and Predecessor periods included in the year ended December 31, 2021. The increase was primarily driven by increases in professional fees of $19.5 million supporting our operations as a public company and restatement-related costs, and salaries and benefits of $19.2 million, as headcount increased 33% from December 31, 2021 to December 31, 2022.
Sales and Marketing Expense
Sales and marketing expense was $5.1 million for the year ended December 31, 2022, an increase of $2.9 million, or 133%, compared to $2.2 million for the combined Successor and Predecessor periods included in the year ended December 31, 2021. The increase was driven by increases in community outreach spend and higher spending related to patient and provider marketing initiatives.
Depreciation and Amortization Expense
Depreciation and amortization expense was $87.3 million for the year ended December 31, 2022, an increase of $78.6 million, or 900.6%, compared to $8.7 million for the combined Successor and Predecessor periods included in the year December 31, 2021. The increase was primarily due to there being a full year of amortization expense recorded on acquired definite lived intangible assets, including trademarks and tradenames, customer contracts, provider network agreements, and payor contracts, during the year ended December 31, 2022.
Goodwill Impairment
During the year ended December 31, 2022, we recorded a $1,315.0 million goodwill impairment charge due to the presence of certain macroeconomic and financial market conditions, industry-specific considerations, our performance, and the sustained decrease in the price of our Class A common stock.
Other
Other income was $2.8 million for the year ended December 31, 2022, compared to other expense of $0.3 million for the combined Successor and Predecessor periods included in the year ended December 31, 2021. During the year ended December 31,
67
2022, we recorded income of $2.5 million related to the release of indemnity funds previously escrowed as part of the Medcore Acquisition.
Income Taxes
Provision for income taxes was $1.9 million for the year ended December 31, 2022 which primarily consisted of Oregon corporate activity tax, a quasi-gross receipts tax that is levied on our Oregon sourced revenue.
Liquidity and Capital Resources
P3 Health Partners Inc. is a holding company and has no material assets other than its ownership of equity interests in P3 LLC. As such, we have no independent means of generating revenue or cash flow, and our ability to pay taxes, make payments under the Tax Receivable Agreement (“TRA”), and to pay dividends will depend on the financial results and cash flows of P3 LLC and the distributions received from P3 LLC. Deterioration in the financial condition, earnings or cash flow of P3 LLC for any reason could limit or impair P3 LLC’s ability to pay such distributions. Additionally, to the extent that we need funds and P3 LLC is restricted from making such distributions under applicable law or regulation or under the terms of any financing arrangements, or P3 LLC is otherwise unable to provide such funds, it could materially adversely affect our liquidity and financial condition. It is anticipated that the distributions we will receive from P3 LLC may, in certain periods, exceed the actual tax liabilities and obligations to make payments under the TRA.
Cash Sources
To date, we have financed our operations principally through the cash we obtained as a result of the Business Combinations, private placements of our equity securities, payments from our payors, issuances of promissory notes, and borrowings under the Term Loan Facility (as defined below). We generate cash from our operations, generally from our contracts with payors. As of December 31, 2022, we had cash and restricted cash of $18.5 million.
We expect to continue to incur operating losses and generate negative cash flows from operations for the foreseeable future due to the strong growth we have experienced over the last five years and the investments we intend to make in expanding our business, which will require up-front expenses. Our future capital requirements will depend on many factors, including the pace of our growth, ability to manage medical costs, the maturity of our members, and our ability to raise capital. We may need to raise additional capital through a combination of debt financing, other non-dilutive financing and/or equity financing and to the extent we are unsuccessful at doing so, we may need to adjust our growth trajectory to accommodate our capital needs and look for additional ways to generate cost efficiencies.
Term Loan
In November 2020, the Company entered a Term Loan and Security Agreement with CRG Servicing, LLC (as amended, the “Term Loan Agreement”) providing for funding of up to $100 million (the “Term Loan Facility”). The Term Loan Facility’s maturity date is December 31, 2025. As of December 31, 2022, we had $65.0 million of borrowings outstanding under the Term Loan Facility, and remaining availability under the Term Loan Facility ended upon termination of the commitment period on February 28, 2022. Interest is payable at 12.0% per annum on a quarterly cycle (in arrears), which began on March 31, 2021. In March 2021, we elected to pay interest at 8.0% with the remaining interest at 4.0% being added to principal as paid in-kind (“PIK”) for a period of three years (or 12 payments).
We are required to remain in compliance with financial covenants such as minimum liquidity of $5.0 million and annual minimum revenue levels. In addition, the Term Loan Agreement restricts our ability and the ability of our subsidiaries to, among other things, incur indebtedness and liens. On an annual basis, we must post a minimum amount of annual revenue equal to or greater than $460.0 million in 2022; $525.0 million in 2023; $585.0 million in 2024 and $650.0 million in 2025. The maturity date may be accelerated as a remedy under the certain default provisions in the Term Loan Agreement, or in the event a mandatory prepayment event occurs.
68
In connection with the issuance of the VGS Promissory Note and entry into the Subordination Agreement (as described below), on December 13, 2022, we entered into an amendment to the Term Loan Agreement to permit the issuance of the VGS Promissory Note and the entry into the Subordination Agreement.
VGS Promissory Note
On December 13, 2022, we entered into a financing transaction with VGS which included the issuance of the VGS Promissory Note and the entry into the VGS Warrant Agreement and the Subordination Agreement. The VGS Promissory Note provides for funding of up to $40.0 million, available for us to draw in three tranches as follows: (i) a first tranche of $15.0 million available on December 13, 2022, (ii) a second tranche of up to $15.0 million in a single draw at our option after January 5, 2023, and (iii) a third tranche of up to $10.0 million available at our option in a single draw after January 5, 2023 and on or prior to February 3, 2023. We will pay VGS an up-front fee of 1.5% at the time of each draw and a back-end fee at the time the VGS Promissory Note is paid as follows: (i) if paid from March 1, 2023 through June 30, 2023, 4.5%; (ii) if paid from July 1, 2023 through December 31, 2023, 6.75% and (iii) if paid on January 1, 2024 or later, 9.0%. The maturity date of the Promissory Note is May 19, 2026. Interest is payable at 14.0% per annum on a quarterly cycle (in arrears) beginning March 31, 2023. We may elect to pay interest of 6.0% in kind and 8.0% in cash, subject to certain limitations.
The VGS Promissory Note may be prepaid, at our option, either in whole or in part, without penalty or premium, at any time and from time to time, subject to the payment of the back-end fee; provided that prepayments must be in increments of at least $2.0 million. The VGS Promissory Note provides for mandatory prepayments with the proceeds of certain asset sales, and the Lender has the right to demand payment in full upon (i) a change of control of the Company and (ii) certain qualified financings (as defined in the VGS Promissory Note).
The VGS Promissory Note restricts our ability to, among other things, incur indebtedness and liens, and make investments and restricted payments. The maturity date may be accelerated as a remedy under the certain default provisions in the agreement, or in the event a mandatory prepayment event occurs.
In connection with the issuance of the VGS Promissory Note, we also entered into the VGS Warrant Agreement pursuant to which we issued VGS warrants to purchase 429,180 shares of Class A common stock at an exercise price of $4.26 per share. The number of shares of common stock for which the VGS Warrant is exercisable and the exercise price may be adjusted upon any event involving subdivisions, combinations, distributions, recapitalizations, and similar transactions. Pursuant to the VGS Warrant Agreement, the warrants and the right to purchase securities upon the exercise of the warrants will terminate upon the earliest to occur of the following: (a) December 13, 2027; and (b) the consummation of (i) a sale, conveyance, consolidation with any other corporation (other than a wholly owned subsidiary corporation) or (ii) any other transaction or series of related transactions in which more than 50% of the voting power of which the Company or P3 LLC is disposed.
In connection with the issuance of the VGS Promissory Note, we also entered into a subordination agreement, dated as of December 13, 2022 (the “Subordination Agreement”) with VGS which subordinates VGS’s right of payment under the VGS Promissory Note to the right of payment and security interests of the lenders under the Term Loan Facility. Under the terms of the Subordination Agreement, we will be required to pay all interest under the VGS Promissory Note in-kind. The VGS Promissory Note may be prepaid, at our option, either in whole or in part, without penalty or premium subject to certain conditions. As of December 31, 2022, $15.0 million had been drawn on the VGS Promissory Note. Between January and March 2023, we borrowed a total of $12.9 million on the VGS Promissory Note and have $12.1 million in remaining borrowing capacity.
As of December 31, 2022, we were not in compliance with its Term Loan Facility and VGS Promissory Note covenants related to issuance of the 2022 financial statements with an audit opinion free of a “going concern” qualification. The Term Loan Facility and VGS Promissory Note lenders have granted us a waiver of the covenant under the Term Loan Facility related to the existence of a “going concern” qualification in the audit opinion for our audited financial statements for the fiscal year ended December 31, 2022. We were in compliance with all other covenants under the Term Loan Facility and VGS Promissory Note as of December 31, 2022; however, there can be no assurance that we will be able to maintain compliance with these covenants in the future or that the lenders under the Term Loan Facility VGS Promissory Note or the lenders of any future indebtedness we may incur will grant any such waiver or forbearance in the future.
69
Repurchase Promissory Note
In June 2019, we issued a share repurchase promissory note (the “Repurchase Promissory Note”) to a former equity investor for $15.0 million, which was subsequently amended in November 2020. The amended agreement stipulated that the Repurchase Promissory Note would automatically mature and be due and payable on the earlier of June 30, 2026, a change in control transaction, or an underwritten primary public offering, each as defined in the agreement. The note accrues PIK interest of 11.0% per year. The principal balance, accrued interest, and an exit fee of $0.6 million are due at maturity. Accrued interest was $9.0 million and $6.5 million at December 31, 2022 and 2021, respectively.
For additional discussion of our long-term debt, see Note 12 “Debt” in our consolidated financial statements included elsewhere in this Form 10-K.
On March 30, 2023, we entered into a Securities Purchase Agreement pursuant to which we agreed to sell certain of our securities for gross proceeds of approximately $89.5 million. See Note 25 “Subsequent Events” to the consolidated financial statements contained elsewhere in this Form 10-K.
Cash Uses
Our primary uses of cash include payments for medical expenses, administrative expenses, cost associated with our care model, debt service, and capital expenditures. Final reconciliation and receipts of amounts due from payors are typically settled in arrears.
Pursuant to our election under Section 754 of the Internal Revenue Code (the “Code”), we expect to obtain an increase in our share of the tax basis in the net assets of P3 LLC when its units are redeemed or exchanged. We intend to treat any redemptions and exchanges of P3 LLC units as direct purchases of the units for U.S. federal income tax purposes. These increases in tax basis may reduce the amounts that we would otherwise pay in the future to various tax authorities. They may also decrease gains (or increase losses) on future dispositions of certain capital assets to the extent the tax basis is allocated to those capital assets.
In connection with the Business Combinations, we entered into a TRA that provides for the payment by us of 85% of the amount of any tax benefits that we actually realize, or in some cases are deemed to realize, as a result of (i) increases in our share of the tax basis in the net assets of P3 LLC resulting from any redemptions or exchanges of P3 LLC, (ii) tax basis increases attributable to payments made under the TRA, and (iii) deductions attributable to imputed interest pursuant to the TRA (the “TRA Payments”). We expect to benefit from the remaining 15% of any tax benefits that we may actually realize.
The estimation of a liability under the TRA is, by its nature, imprecise and subject to significant assumptions regarding a number of factors, including (but not limited to) the amount and timing of taxable income generated by the Company each year as well as the tax rate then applicable. As a result of the Business Combinations, we may recognize an estimated liability under the TRA of approximately $530.0 million if all P3 Equityholders redeem or exchange their Common Units for Class A common stock or cash at the earliest possible date permitted under the P3 LLC A&R LLC Agreement and assuming (a) the generation of sufficient future taxable income, (b) a trading price of $10 per share of Class A common stock at the time of the redemption or exchange, (c) a constant corporate combined U.S. federal and state income tax rate of 23.89% and (d) no material changes in tax law. The TRA liability is estimated to be $4.6 million as of December 31, 2022. Due to the Company’s history of losses, the Company has not recorded tax benefits associated with the increase in tax basis as a result of the Business Combinations. As a result, the Company determined that payments to TRA holders are not probable and no TRA liability has been recorded as of December 31, 2022.
As non-controlling interest holders exercise their right to exchange their units in P3 LLC, a TRA liability may be recorded based on 85% of the estimated future tax benefits that the Company may realize as a result of increases in the tax basis of P3 LLC. The amount of the increase in the tax basis, the related estimated tax benefits, and the related TRA liability to be recorded will depend on the price of the Company’s Class A common stock at the time of the relevant redemption or exchange.
70
The following table summarizes current and long-term material cash requirements as of December 31, 2022 (in thousands):
| Material Cash Requirements | ||||||||||||||
| Less than |
| 1-3 |
| 3-5 |
| More than | ||||||||
Total | 1 year | years | years | 5 years | |||||||||||
Unpaid claims(1) | $ | 151,207 | $ | 151,207 | $ | — | $ | — | $ | — | |||||
Long-term debt, principal(2) |
| 95,000 |
| — |
| 65,000 |
| 30,000 |
| — | |||||
Long-term debt, interest(3) |
| 78,216 |
| 13,429 |
| 42,001 |
| 22,786 |
| — | |||||
Operating lease liabilities(4) |
| 12,790 |
| 704 |
| 4,292 |
| 3,538 |
| 4,256 | |||||
Total | $ | 337,213 | $ | 165,340 | $ | 111,293 | $ | 56,324 | $ | 4,256 | |||||
(1) | Represents unpaid claims due to third parties for health care services provided to members, including estimates for incurred but not reported claims. Estimates for incurred claims are based on historical enrollment and cost trends while also taking into consideration operational changes. Future and actual results typically differ from estimates. Differences could result from an overall change in medical expenses per members, changes in member mix or simply due to addition of new members. |
(2) | Represents principal payments only. We will pay interest on outstanding indebtedness based on the rates and terms summarized in Note 12 “Debt” in our consolidated financial statements. |
(3) | Represents interest expected to be incurred on our long-term debt based on amounts outstanding as of December 31, 2022 as summarized in Note 12 “Debt” in our consolidated financial statements. |
(4) | Represents minimum operating lease payments, excluding potential lease renewals. See Note 17 “Leases” in our consolidated financial statements. |
Liquidity and Going Concern
As of the date of this Form 10-K, management believes that our existing cash resources are not sufficient to support planned operations for at least the next year from the issuance of this Form 10-K. As a result, management has concluded that there is substantial doubt about our ability to continue as a going concern within one year after the date the consolidated financial statements contained elsewhere in this Form 10-K are issued. In evaluating the Company’s ability to continue as a going concern, management considered the Company’s current projections of future cash flows, current financial condition, sources of liquidity, including funds available under the VGS Promissory Note, and debt obligations for at least one year from the date of issuance of this Form 10-K in considering whether it has the ability to meet its obligations. This evaluation of our cash resources available over the next year from the date of issuance of this Form 10-K does not take into consideration the potential mitigating effect of our ongoing efforts to raise capital or management’s plans that have not been fully implemented or the many factors that determine the Company’s capital requirements, including the pace of our growth, ability to manage medical costs and the maturity of our members. Management continues to explore raising additional capital through a combination of debt financing and equity issuances. If we raise funds by issuing debt securities or preferred stock, or by incurring loans, these forms of financing would have rights, preferences, and privileges senior to those of holders of our common stock. If we raise capital through the issuance of additional equity, such sales and issuance would dilute the ownership interests of the existing holders of our Class A common stock. The availability and the terms under which we may be able to raise additional capital could be disadvantageous, and the terms of debt financing or other non-dilutive financing may involve restrictive covenants and dilutive financing instruments, which could place significant restrictions on our operations. Macroeconomic conditions and credit markets could also impact the availability and cost of potential future debt financing. There can be no assurances that any additional debt, other non-dilutive and/or equity financing would be available to us on favorable terms, or potentially at all. We expect to continue to incur net losses, comprehensive losses, and negative cash flows from operating activities in accordance with our operating plan. If we are unable to obtain additional funding when needed, we will need to curtail planned activities in order to reduce costs, which will likely have an unfavorable effect on our ability to execute on our business plan, and have an adverse effect on our business, results of operations, and future prospects.
The audited consolidated financial statements included elsewhere in this Form 10-K have been prepared assuming the Company will continue as a going concern and do not include any adjustments that might result from the outcome of these uncertainties.
Our independent registered public accounting firm, in its report on the Company’s consolidated financial statements for the year ended December 31, 2022, has also expressed substantial doubt about our ability to continue as a going concern.
71
Cash Flows
The following table summarizes our cash flows (in thousands):
Successor | Predecessor | |||||||||
Year Ended | December 3, 2021 | January 1, 2021 | ||||||||
December 31, | through December | through December | ||||||||
| 2022 |
| 31, 2021 |
|
| 2, 2021 | ||||
Net cash used in operating activities | $ | (126,019) | $ | (15,342) | $ | (51,129) | ||||
Net cash used in investing activities | (7,733) | (47,856) | (8,209) | |||||||
Net cash provided by financing activities | 11,375 | 198,677 | 24,790 | |||||||
Net change in cash | $ | (122,377) | $ | 135,479 | $ | (34,548) | ||||
Operating Activities
Net cash used in operating activities was $126.0 million for the year ended December 31, 2022, compared to net cash used in operating activities of $66.5 million for the combined Successor and Predecessor periods included in the year ended December 31, 2021. Significant changes impacting net cash used in operating activities during the year ended December 31, 2022 as compared to the year ended December 31, 2021 were primarily due to the timing of cash sweeps received in 2022, but recognized in 2021 in accordance with our revenue recognition policy resulting from the extended reporting period related to the 2021 audit, and payments of professional fees supporting our operations as a public company and restatement-related costs.
Investing Activities
Net cash used in investing activities was $7.7 million for the year ended December 31, 2022, primarily consisting of the acquisition of two medical practices for a total purchase price of $5.5 million, net of cash acquired. Net cash used in investing activities was $56.1 million for the combined Successor and Predecessor periods included in the year ended December 31, 2021, primarily consisting of the cash paid for the Business Combinations and Medcore Acquisition.
Financing Activities
Net cash provided from financing activities was $11.4 million for the year ended December 31, 2022, consisting of proceeds from the issuance of the VGS Promissory Note, offset by repayments of debt. Net cash provided from financing activities was $223.5 million for the combined Successor and Predecessor periods included in the year December 31, 2021, primarily consisting of $195.3 million of proceeds from the issuance of PIPE Shares.
JOBS Act
We qualify as an “emerging growth company” pursuant to the provisions of the JOBS Act. For as long as we are an “emerging growth company,” we may take advantage of certain exemptions from various reporting requirements that are applicable to other public companies that are not “emerging growth companies,” including, but not limited to, not being required to comply with the auditor attestation requirements of Section 404(b) of the Sarbanes-Oxley Act, reduced disclosure obligations regarding executive compensation in our periodic reports and proxy statements, exemptions from the requirements of holding advisory “say-on-pay” votes on executive compensation and shareholder advisory votes on golden parachute compensation.
In addition, under the JOBS Act, emerging growth companies can delay adopting new or revised accounting standards until such time as those standards apply to private companies. We intend to take advantage of the longer phase-in periods for the adoption of new or revised financial accounting standards under the JOBS Act until we are no longer an emerging growth company. Our election to use the phase-in periods permitted by this election may make it difficult to compare our financial statements to those of non-emerging growth companies and other emerging growth companies that have opted out of the longer phase-in periods permitted under the JOBS Act and who will comply with new or revised financial accounting standards. If we were to subsequently elect instead to comply with public company effective dates, such election would be irrevocable pursuant to the JOBS Act.
72
Critical Accounting Policies and Estimates
The discussion and analysis of our financial condition and results of operations are based upon our consolidated financial statements, which have been prepared in accordance with GAAP. The preparation of these consolidated financial statements requires management use judgment in the application of accounting policies, including making estimates and assumptions that could affect assets and liabilities, revenue and expenses and related disclosures of contingent assets and liabilities at the date of our financial statements. Management bases its estimates on the best information available at the time, its experiences and various other assumptions believed to be reasonable under the circumstances. Actual results could differ from those estimates. To the extent that there are differences between our estimates and actual results, our future financial statement presentation, financial condition, results of operations, and cash flows will be affected. For a more detailed discussion of our significant accounting policies, see Note 3 “Significant Accounting Policies” in our consolidated financial statements included elsewhere in this Form 10-K. Below is a discussion of accounting policies that are particularly important to the portrayal of our financial condition and results of operations and require the application of significant judgment by our management.
Capitated Revenue
The transaction price for our capitated payor contracts is variable as it primarily includes PMPM fees associated with unspecified membership. Medicare pays capitation using a “risk adjustment model”, which compensates providers based on the health status (acuity) of each individual patient. Medicare Advantage plans with higher acuity patients receive higher premiums. Conversely, Medicare Advantage plans with lower acuity patients receive lesser premiums. Under the risk adjustment model, capitation is paid on an interim basis based on enrollee data submitted for the preceding year and is adjusted in subsequent periods after final data is compiled. As premiums are adjusted via this risk adjustment model (via a RAF), the Company’s PMPM payments will change commensurately with how our contracted Medicare Advantage plans’ premiums change with CMS. In certain contracts, PMPM fees also include adjustments for items such as performance incentives or penalties based on the achievement of certain clinical quality metrics as contracted with payors.
Capitated revenue is recognized based on an estimated PMPM transaction price to transfer the service for a distinct increment of the series (e.g., month), net of projected acuity adjustments and performance incentives or penalties as management can reasonably estimate the ultimate PMPM payment of those contracts. The Company recognizes revenue in the month in which eligible members are entitled to receive healthcare benefits during the contract term. The capitation amount is subject to possible retroactive premium risk adjustments based on the member’s individual acuity.
Medical Expense and Claims Payable
The cost of healthcare services is recognized in the period services are provided. Medical expense includes costs of all covered services provided to members assigned by the health plans under P3’s at-risk model. Medical expense includes the cost for third-party healthcare service providers, the cost for overseeing the quality of care and programs, and from time to time, remediation of certain claims that might result from periodic reviews conducted by various regulatory agencies. This also includes an estimate of the cost of services that have been incurred, but not yet reported (“IBNR”).
Management estimates the Company’s IBNR by applying standard actuarial methodologies, which utilize historical data, including the period between the date services are rendered and the date claims received (and paid), denied claims activity, expected medical cost inflation, seasonality patterns, and changes in membership mix. Such estimates are subject to impact from changes in both the regulatory and economic environments. The Company’s claims payable represents management’s best estimate of its liability for unpaid medical costs. We have included incurred but not reported claims of $151.2 million and $102.0 million on our consolidated balance sheets as of December 31, 2022 and 2021, respectively.
Our consolidated financial statements could be materially impacted if actual claims expense is different from our estimates. If our liability for incurred and not reported claims at December 31, 2022 were to differ by plus or minus 5%, the impact on medical claims expense would be approximately $7.6 million.
73
Warrant Liability
We have Public and Private Placement Warrants that are classified as liabilities at their fair value at inception and adjusted to fair value at each reporting period. This liability is subject to re-measurement at each balance sheet date until exercised and any change in fair value is recognized in our statement of operations.
The Public Warrants are publicly traded and are recorded at fair value using the closing price as of the measurement date. The Private Placement Warrants have no observable traded price and are valued using an option pricing model (Black-Scholes-Merton). The assumptions used in preparing these models include estimates such as volatility, contractual terms, discount rates, dividend yield, expiration dates and risk-free rates. We have historically been a private company and lacked sufficient company-specific historical and implied volatility information. Therefore, we estimated our expected stock volatility based on the historical volatility of a publicly traded set of peer companies. The risk-free interest rate assumption is determined by using the U.S. Treasury rates of the same period as the expected term of the private placement warrants at each reporting period. Changes in these assumptions can materially affect the estimate of the fair value of these instruments and could cause a material increase or decrease to expense realized from the change in fair value of warrants, and to the underlying warrant liability.
Goodwill and Other Identified Intangible Assets
Goodwill represents the excess of cost over the fair value of net tangible and identifiable intangible assets acquired in a business combination. Goodwill is not amortized and instead is tested for impairment on an annual basis or more frequently if we believe indicators of impairment exist.
We have determined that there is only one reporting unit for the purpose of testing goodwill impairment. In circumstances where we conclude that it is more likely than not (i.e., a likelihood of greater than 50%) that the fair value of the reporting unit is less than its carrying amount, a quantitative fair value test is performed. Factors we consider when performing the qualitative assessment primarily include general economic conditions and changes in forecasted operating results.
In a quantitative impairment test, we assess goodwill by comparing the carrying amount of each reporting unit to its fair value. We estimate the fair value of our reporting unit using a weighted combination of the income approach and market-based approach. The income approach discounts the reporting unit’s estimated future cash flows using an estimated discount rate, both of which are considered Level 3 inputs. The market approach is based on comparable companies’ market multiples of revenue and EBITDA. Publicly traded companies in the same industry and target companies with transactions that are similar in nature are selected as guideline companies for the market-based approach. The resulting fair value is then compared to the carrying amount.
Our annual impairment review measurement date is in the fourth quarter of each year. For 2022, we completed the required annual assessment of goodwill for impairment for our reporting unit using a qualitative assessment and determined that a quantitative assessment of goodwill impairment was required (i.e., it is more likely than not that the fair value of goodwill exceeds the carrying amount). Based on the results of our quantitative assessment, we recorded a $1,315.0 million goodwill impairment charge during the year ended December 31, 2022.
We review identified intangible assets with defined useful lives and subject to amortization for impairment whenever events or changes in circumstances indicate that the related carrying amounts may not be recoverable. Determining whether an impairment loss occurred requires comparing the carrying amount of the asset to the sum of undiscounted cash flows expected to be generated by the asset.
Intangible assets with indefinite lives are tested for impairment annually.
Income Taxes
We account for income taxes under the asset and liability method. Under this method, deferred tax assets and liabilities are determined based on differences between the consolidated financial statement carrying amounts and tax bases of assets and liabilities and operating loss and tax credit carryforwards and are measured using the enacted tax rates that are expected to be in effect when the differences reverse. The effect on deferred tax assets and liabilities of a change in tax rates is recognized in our consolidated
74
statements of operations in the period that includes the enactment date. Valuation allowances are established when necessary to reduce deferred tax assets to an amount that, in the opinion of management, is more likely than not to be realized.
We account for uncertain tax positions by reporting a liability for unrecognizable tax benefits resulting from uncertain tax positions taken or expected to be taken in a tax return. We recognize interest and penalties, if any, related to unrecognized tax benefits in income tax expense.
Judgment is required in assessing the future tax consequences of events that have been recognized in our consolidated financial statements or tax returns. Variations in the actual outcome of these future tax consequences could materially impact our consolidated financial statements.
Premium Deficiency Reserves
A PDR is recorded when there is a probable future loss on unearned capitated premiums after estimated expected claim costs and claim adjustment expenses. Losses under prepaid health care services contracts shall be recognized when it is probable that expected future health care costs and maintenance costs under a group of existing contracts will exceed anticipated future premiums and stop-loss insurance recoveries on those contracts. To determine the need to recognize a loss, contracts shall be grouped in a manner consistent with the provider’s method of establishing premium rates, for example, by community rating practices, geographical area, or statutory requirements, to determine whether a loss has been incurred. In our at-risk arrangements, the more we improve health outcomes and lower the overall cost of care, the more profitable we will be over time.
We assess the profitability of our at-risk arrangements to identify contracts where current operating results or forecasts indicate probable future losses. Management estimates the Company’s PDR by utilizing estimates of membership growth rates, changes in membership mix, estimated PMPM payments under contracts, historical claims data, seasonality patterns, our ability to lower the overall cost of care and incremental medical costs, such as those related to COVID-19 admissions. Such estimates are subject to impact from changes in both the regulatory and economic environments. The Company’s PDR represents management’s best estimate of its probable future losses. We have included premium deficiency reserve liabilities of $26.4 million and $37.8 million on our accompanying consolidated balance sheets as of December 31, 2022 and 2021, respectively.
Equity-based Compensation
We measure the cost of the employee services received in exchange for an award of equity instruments based on the grant-date fair value or, in certain circumstances, the calculated value of the award. Under our unit-based incentive plan, the Company may reward grantees with various types of awards, including but not limited to profits interests on a service-based or performance-based schedule. These awards may also contain market conditions.
For performance-vesting units, P3 recognizes unit-based compensation expense when it is probable that the underlying performance condition will be achieved. The Company will analyze if a performance condition is probable for each reporting period through the settlement date for awards subject to performance vesting. For service-vesting units, P3 recognizes unit-based compensation expense over the requisite service period for each separately vesting portion of the profits interest as if the award was, in substance, multiple awards.
Recent Accounting Pronouncements
See Note 4 “Recent Accounting Pronouncements” in our consolidated financial statements included elsewhere in this Form 10-K for a description of recent accounting standards issued and the anticipated effects on our consolidated financial statements.
Item 7A. Quantitative and Qualitative Disclosures About Market Risk.
Not required for Smaller Reporting Companies.
75
Item 8. Financial Statements and Supplementary Data.
The financial statements required to be filed pursuant to this Item 8 are appended to this report. An index of those financial statements is found in Item 15 of Part IV of this Form 10-K.
Item 9. Changes in and Disagreements With Accountants on Accounting and Financial Disclosure.
None.
Item 9A. Controls and Procedures.
Limitations on effectiveness of controls and procedures
In designing and evaluating our disclosure controls and procedures, management recognizes that any controls and procedures, no matter how well designed and operated, can provide only reasonable assurance of achieving the desired control objectives. In addition, the design of disclosure controls and procedures must reflect the fact that there are resource constraints and that management is required to apply judgment in evaluating the benefits of possible controls and procedures relative to their costs.
Evaluation of disclosure controls and procedures
Our management, with the participation of our Chief Executive Officer and Chief Financial Officer, evaluated, as of the end of the period covered by this Form 10-K, the effectiveness of our disclosure controls and procedures (as defined in Rules 13a-15(e) and 15d-15(e) under the Exchange Act). Based on that evaluation, our Chief Executive Officer and Chief Financial Officer concluded that, due to the material weaknesses described below, our disclosure controls and procedures were not effective at the reasonable assurance level as of December 31, 2022.
Material Weaknesses
In connection with the audit of our financial statements for the year ended December 31, 2021, and as previously reported, the restatement of the Company’s financial statements for the years ended December 31, 2020 and 2019, we concluded that there were material weaknesses in our internal control over financial reporting. A material weakness is a deficiency, or a combination of deficiencies, in internal control over financial reporting such that there is a reasonable possibility that a material misstatement of our annual or interim financial statements will not be prevented or detected on a timely basis.
Management has determined that the Company had the following material weaknesses in its internal control over financial reporting, which continued to exist as of December 31, 2022:
Control Environment, Risk Assessment and Monitoring Activities
We did not maintain appropriately designed entity-level controls impacting the control environment, risk assessment procedures, and effective monitoring activities to prevent or detect material misstatements to the consolidated financial statements. These material weaknesses are specifically attributed to the following:
| ● | We did not have adequate policies and procedure or sufficient qualified resources with sufficient technical knowledge to maintain effective controls over the accounting related to significant accounts and related financial statement disclosures. |
| ● | We did not design and implement a sufficient risk assessment process to identify and assess risks impacting control over financial reporting. |
| ● | We had ineffective evaluation and determination as to whether the components of internal control were present and functioning. |
76
Control Activities and Information and Communication
As a consequence of these entity-level material weaknesses, we did not design, implement, and maintain effective control activities within certain business processes and the information technology environment to mitigate the risk of material misstatement in financial reporting. Specifically:
| ● | We did not maintain effective controls over our information systems to ensure that relevant and reliable information was communicated on a timely basis across the organization to support the financial reporting process, including: |
| o | We did not design and implement effective information technology general controls in the areas of user access related to certain information technology systems that support our financial reporting process. |
| o | We did not maintain sufficient segregation of duties over the performance of control activities for financial close and reporting, including over the review of account reconciliations and journal entries. |
| ● | We did not design and maintain effective management review controls at a sufficient level of precision over account reconciliations and the accounting for transactions related to the risk adjustment factor receivable and related revenue, capitated revenue classification, premium deficiency reserves, business combinations, goodwill and intangibles, income taxes, warrant valuation, equity awards, and the inaccurate attribution of net income or loss to the controlling and non-controlling interests for subsidiaries that are variable interest entities. |
| ● | We did not design and maintain effective controls at a sufficient level of precision over the estimation of claims expense and payable including controls over the review of historical claims data, including the completeness and accuracy of data used to determine the financial statement amounts. |
Remediation Activities
We have taken and are taking steps to remediate these material weaknesses through (i) hiring qualified accounting, financial reporting, IT, and other key management personnel with public company experience, (ii) engaging an external advisor to assist with documenting internal controls, including enhancing controls to ensure proper communication of critical information, review and approvals; evaluating effectiveness of internal controls and assist with the remediation of deficiencies and training of personnel, as necessary, and establishment of a formal internal audit function and (iii) enhancing policies, procedures, and documentation for significant areas of accounting, including each area where a material weakness was identified. We are still in the process of implementing these steps and cannot assure investors that these measures will significantly improve or remediate the material weaknesses described above.
Management’s annual report on internal control over financial reporting
Our management is responsible for establishing and maintaining adequate internal control over financial reporting (as defined in Rules 13a-15(f) and 15d-15(f) under the Exchange Act). Our internal control over financial reporting is designed to provide reasonable assurance regarding the reliability of financial reporting and the preparation of consolidated financial statements for external purposes in accordance with GAAP.
Our management conducted an assessment of the effectiveness of our internal control over financial reporting based on the criteria set forth in “Internal Control – Integrated Framework (2013)” issued by the Committee of Sponsoring Organizations of the Treadway Commission.
Based on this assessment, our management concluded that our internal control over financial reporting was not effective as of December 31, 2022 due to the material weaknesses in our internal control over financial reporting described above.
Our independent registered public accounting firm is not yet required to formally attest to the effectiveness of our internal controls over financial reporting, and will not be required to do so for as long as we are an “emerging growth company” pursuant to the provisions of the JOBS Act.
77
Changes in internal control over financial reporting
There were no changes in our internal control over financial reporting (as defined in Rules 13a-15(f) and 15d-15(f) under the Exchange Act) during the quarter ended December 31, 2022 that have materially affected, or are reasonably likely to materially affect, our internal control over financial reporting.
Item 9B. Other Information.
None.
Item 9C. Disclosure Regarding Foreign Jurisdictions that Prevent Inspections.
None.
78
PART III
Item 10. Directors, Executive Officers and Corporate Governance.
The following table provides information regarding our executive officers and members of our board of directors (ages as of the date of this Form 10-K):
Name |
| Age |
| Position |
Executive Officers | ||||
Sherif Abdou, M.D. | 62 | Chief Executive Officer, Director and Co-Founder | ||
Amir Bacchus, M.D. | 58 | Chief Medical Officer, Director and Co-Founder | ||
Atul Kavthekar | 54 | Chief Financial Officer | ||
Non-Employee Directors | ||||
Mark Thierer | 62 | Chairman of the Board | ||
Greg Wasson | 63 | Director | ||
Lawrence B. Leisure | 72 | Director | ||
Mary Tolan | 62 | Director | ||
Greg Kazarian | 60 | Director | ||
Thomas E. Price, M.D. | 68 | Director | ||
Jeffrey G. Park | 50 | Director |
Sherif Abdou, M.D. is a Co-founder of P3 and has served as P3’s Chief Executive Officer and on the Legacy P3 Board of Managers since 2017 and as a Director of the Company since December 2021. Dr. Abdou served as Chief Executive Officer of P3 Health Group from 2015 to 2017. Dr. Abdou received a Bachelor of Medicine and Surgery degree from Mansoura University and a Master of Medical Management degree from the University of Southern California. Dr. Abdou was selected to serve on our board of directors for his experience in the healthcare industry, his role as one of P3’s founders and his service as P3’s Chief Executive Officer.
Amir Bacchus, M.D. is a Co-founder of P3 and has served as P3’s Chief Medical Officer and on the Legacy P3 Board of Managers since 2017 and as a Director of the Company since December 2021. Dr. Bacchus served as Chief Medical Officer of P3 Health Group from 2015 to 2017. Dr. Bacchus served as a director of the University of Nevada, Las Vegas—School of Medicine Advisory Board, a position he held from 2014 to 2020. Dr. Bacchus received a Bachelor of Arts degree from California State University, Northridge, a Doctor of Medicine from Wayne State University School of Medicine and an MBA from the University of Nevada, Las Vegas. Dr. Bacchus was selected to serve on our board of directors for his experience in the healthcare industry, his role as one of P3’s founders and his service as P3’s Chief Medical Officer.
Atul Kavthekar has served as our Chief Financial Officer since December 12, 2022. Prior to joining the Company, Mr. Kavthekar served as Executive Vice President and Chief Financial Officer of EyeCare Partners, a clinically-integrated comprehensive eyecare platform, since March 2021. From July 2020 to March 2021, Mr. Kavthekar served as Chief Financial Officer of Encyclopedia Britannica, a digital media, publishing and educational curriculum company. From May 2017 to April 2019, Mr. Kavthekar served as Chief Financial Officer and Treasurer of Diplomat Pharmacy, Inc., an independent provider of specialty pharmacy services. Mr. Kavthekar served as Chief Financial Officer of LivingSocial, Inc., an e-commerce retailer, from June 2015 to December 2016. Mr. Kavthekar also served as Chief Financial Officer and Head of Corporate Development for the health and wellness division of Sears Holding Corporation, which included the Kmart Pharmacy business, from December 2013 to May 2015, and as Division Chief Financial Officer of e-commerce for Walgreen Co. from December 2009 to December 2013. Prior to these positions, he held a number of positions in the financial industry, focusing on investment banking and mergers and acquisitions. Mr. Kavthekar received an MBA from The University of Chicago Booth School of Business.
Mark Thierer has served as a Director of the Company since December 2021 and an advisor to Foresight since October 2020. Mr. Thierer currently serves as the managing partner of the investment firm he formed, AssetBlue Investment Group, a position he has held since June 2017. From October 2017 through February 2018, Mr. Thierer also served as the interim Chief Executive Officer of Dentsply Sirona Inc. (Nasdaq: XRAY), a manufacturer of dental implants. Mr. Thierer was Chief Executive Officer of OptumRx, a pharmacy care services company, from July 2015 until September 2017. He previously served as chairman and Chief Executive Officer of Catamaran Corporation (Nasdaq: CTRX), one of the nation’s largest pharmacy benefit management companies, from
79
March 2011 until it combined with OptumRx in 2015. Mr. Thierer has experience as a Chief Executive Officer leading a national pharmacy benefit and healthcare information technology solutions company. His skills include strategy and business development, technology, finance and marketing. He brings valuable leadership experience and knowledge of operations and the day-to-day management of a national corporation. Mr. Thierer also has experience in the structuring and execution of strategic corporate transactions, including mergers and acquisitions. Mr. Thierer is a member of the board of directors of Discover Financial Services (NYSE: DFS) since 2014 and Senior Connect Acquisition Corp. (Nasdaq: SNRH). Mr. Thierer received a BS in Finance from the University of Minnesota and an MBA from Nova Southeastern University. Mr. Thierer also holds the designation of CEBS (Certified Employee Benefits Specialist) from The Wharton School of the University of Pennsylvania. Mr. Thierer was selected to serve on our board of directors for his extensive experience in both the financial and healthcare sectors.
Greg Wasson has served continually as a director of P3 Health Partners Inc. and its predecessor, Foresight Acquisition Corp, since November 2020. Mr. Wasson currently serves as President and Founder of his own family office, Wasson Enterprise. Wasson Enterprise’s focus is to partner with entrepreneurs and operators to build sustainable, high-growth businesses that do well by doing good. As the former President and CEO of Walgreens Boots Alliance, Inc., Mr. Wasson has extensive global operational and management experience, as well as extensive knowledge of the retail and healthcare industries. Mr. Wasson attended Purdue University’s School of Pharmacy, receiving his pharmacy degree in 1981. Before his senior year, he was invited to become one of the first pharmacy services interns in Walgreens’ corporate offices—an opportunity that led to his being hired by Walgreens upon graduation and that changed the course of his future career. Mentored by many company leaders through the years, together with his outstanding performance in positions of increasing responsibility, Mr. Wasson served Walgreens for 34 years. As Walgreens CEO, Mr. Wasson led the Fortune 35 company to record fiscal 2014 sales of $76.4 billion. He is credited with creating significant financial and shareholder value, initiating and completing transformative mergers and investments, leading complex organizational and structural change, assembling a diverse and high- performance senior leadership team, and establishing Walgreens’ position as an industry leader. Before retiring from Walgreens, Mr. Wasson had transformed an iconic 114-year-old domestic company into the first global pharmacy-led, health, well-being and beauty enterprise via the successful merger with European-based Alliance Boots to create Walgreens Boots Alliance, Inc. Mr. Wasson currently serves on the Board of Directors of OptimizeRx Corp. (Nasdaq: OPRX), a position he has held since August 2020. Mr. Wasson also served on the Board of Directors of PNC Financial Services Group, Inc. (NYSE: PNC) from July 2015 to October 2018 and Verizon Communications Inc. (NYSE: VZ) from February 2013 to October 2018. Mr. Wasson was selected to serve on our board of directors for his deep experience as an executive in the healthcare services industry and broad industry relationships.
Lawrence B. Leisure has served as a Director of the Company since December 2021 and on the Legacy P3 Board of Managers since April 2017. Mr. Leisure co-founded and has served as a Managing Partner of Chicago Pacific Founders, a private equity fund focused exclusively on healthcare services and senior living, since 2014. Mr. Leisure currently serves as a director of BioIntelliSense, a position he has held since January 2019, as a manager of Recovery Ways Holdings, a position he has held since July 2014. Mr. Leisure serves as a manager of Chicago Pacific Capital, L.P., a position he has held since July 2014, a manager of Chicago Pacific Founders UGP I, a position he has held since July 2014, a manager of Chicago Pacific Founders UPP II, a position he has held since June 2019, a manager of Wellbe Senior Medical, LLC, a position he has held since March 2019, a manager of Impact Advisors Holdings, LLC, a position he has held since December 2019, and a manager of Allymar Health Solutions, LLC, a position he has held since March 2021. Mr. Leisure also served as a manager of FEMG Holdings, LLC, from August 2018 to July 2021. He also serves on the board of IrsVision, and Cahrus Technologies, both early-stage startup companies. From a not-for-profit perspective, he is a Senior Advisor to the Byers Center for BIODESIGN at Stanford University, a member of the Board of Advisors of the UCLA Anderson School of Management, and Chair of the Advisory Board of the UCSF Rosenman Institute. Mr. Leisure received a Bachelor of Arts degree from Stanford University and an MBA degree from the University of California, Los Angeles. Mr. Leisure was selected to serve on our board of directors for his deep experience in value-based healthcare delivery models and broad industry relationships.
Mary Tolan has served as a Director of the Company since December 2021 and on the Legacy P3 Board of Managers since April 2017. Ms. Tolan co-founded and has served as a Managing Partner of Chicago Pacific Founders, a private equity fund focused exclusively on healthcare services, technology and healthcare real estate, since 2014. Previously, Ms. Tolan was the founder of R1 RCM, Inc. (Nasdaq: RCM), a provider of comprehensive end-to-end healthcare revenue-cycle management services and population health management services infrastructure. Prior to R1 RCM, Ms. Tolan was a Group Chief Executive at Accenture, the global management consulting, technology services, and outsourcing company. Ms. Tolan currently serves as a director of Tredence, Inc., Atrio, WellBe, Duo, Peeq, Novum Health, SightMD, and Ascend. Ms. Tolan serves on the Board of Trustees for the University of Chicago. Ms. Tolan received a Bachelor of Business Administration degree from Loyola University and an MBA from the University
80
of Chicago. Ms. Tolan was selected to serve on our board of directors for her extensive experience in value-based care as an executive in the healthcare services industry and her investing experience.
Greg Kazarian has served as a Director of the Company since December 2021 and on the Legacy P3 Board of Managers since May 2017. Mr. Kazarian has served as an Operating Partner of Chicago Pacific Founders since 2014. Mr. Kazarian currently serves as a director of Recovery Ways Holdings, LLC, a position he has held since July 2014, and a director of CPF Outpatient Holdings, LLC, a position he has held since October 2020. Mr. Kazarian was one of the four Executive Officers of Accretive Health (now R1 RCM, Inc. (Nasdaq: RCM)) a provider of comprehensive end-to-end healthcare revenue-cycle management services and population health management services infrastructure. Mr. Kazarian served in a variety of roles during his tenure at Accretive Health including General Counsel, Head of the Physician Advisory Services Business and Senior Vice President of Operations with P&L responsibility for one third of the Company’s revenue cycle business. Prior to joining Accretive Health, Mr. Kazarian was a partner at Pedersen and Houpt in Chicago, where he spent 16 years representing mid-sized growth companies. Mr. Kazarian received his law degree and his Bachelor of Science degree in Biophysics from the University of Illinois. Mr. Kazarian was selected to serve on our board of directors for his experience as an executive in the healthcare services industry and his investing experience.
Thomas E. Price, M.D. has served as a Director of the Company since December 2021 and on the Legacy P3 Board of Managers since January 2018. Dr. Price currently serves as a director of Triumph Orthopedics, LLC, a position he has held since 2021, a sole director of HealthWiseFirst, LLC, a position he has held since 2018, a director of Association Health Plans of America, LLC, a position he has held since 2018, a director of Transformation Care Network, LLC, a position he has held since 2020, a director of Botanicals Sciences, LLC, a position he has held since 2020, a director of Capital Ministries (non-profit), a position he has held since 2018. Dr. Price entered private medical practice in 1984, returned to Emory University as an assistant professor of orthopedic surgery in 2002 and subsequently serviced as director of the orthopedic clinic at Atlanta’s Grady Memorial Hospital. Dr. Price served in the US House of Representatives from Georgia’s 6th district from 2005 to 2017, during which time he served as Chair of the House Budget Committee from 2015 to 2017. In February 2017, he was confirmed by the Senate as the United States Secretary of Health and Human Services (HHS) and remained in that position until September 2017. Currently, Dr. Price serves on the boards of several privately held health care companies and non-profits as well as consulting and advising companies. Dr. Price holds Bachelor’s and Doctor of Medicine degrees from the University of Michigan. He completed his residency at Emory University and was in private orthopedic practice from 1984 to 2004. Dr. Price was selected to serve on our board of directors for his extensive experience in public service and medical practice that bring a deep perspective on P3’s business.
Jeffrey G. Park has served as a Director of the Company since December 2021. Mr. Park was the Chairman and Chief Executive Officer of WellDyneRx, an independent pharmacy benefits manager, from April 2019 until April 2022 and since October 2019 as a director of Progyny (Nasdaq: PGNY). From January 2018 until May 2018, he was the Interim Chief Executive Officer of Diplomat Pharmacy, Inc., or Diplomat (NYSE: DPLO), a provider of specialty pharmacy services. Additionally, from June 2017 to February 2019, he served on the board of directors of Diplomat. Prior to that, from July 2015 until July 2016, he was the Chief Operating Officer of OptumRX, the entity resulting from the merger of Catamaran Corporation, or Catamaran, and OptumRX, UnitedHealthcare Group’s free-standing pharmacy care services business. Before the merger, from March 2014 until July 2015, he was Catamaran’s Executive Vice President, Operations, and previously served as Catamaran’s Chief Financial Officer, beginning in 2006. Mr. Park holds a B.S. in Accounting from Brock University. Mr. Park was selected to serve on our board of directors for his extensive leadership experience in the pharmaceutical industry.
The remaining information required by this item will be included in our definitive Proxy Statement for the 2023 Annual Meeting of Stockholders, if filed with the SEC within 120 days after December 31, 2022, and incorporated herein by reference, or will be provided in an amendment filed on Form 10-K/A with the SEC no later than 120 days after December 31, 2022.
Item 11. Executive Compensation.
The information required by this item will be included in our definitive Proxy Statement for the 2023 Annual Meeting of Stockholders, if filed with the SEC within 120 days after December 31, 2022, and incorporated herein by reference, or will be provided in an amendment filed on Form 10-K/A with the SEC no later than 120 days after December 31, 2022.
81
Item 12. Security Ownership of Certain Beneficial Owners and Management and Related Stockholder Matters.
The information required by this item will be included in our definitive Proxy Statement for the 2023 Annual Meeting of Stockholders, if filed with the SEC within 120 days after December 31, 2022, and incorporated herein by reference, or will be provided in an amendment filed on Form 10-K/A with the SEC no later than 120 days after December 31, 2022.
Item 13. Certain Relationships and Related Transactions, and Director Independence.
The information required by this item will be included in our definitive Proxy Statement for the 2023 Annual Meeting of Stockholders, if filed with the SEC within 120 days after December 31, 2022, and incorporated herein by reference, or will be provided in an amendment filed on Form 10-K/A with the SEC no later than 120 days after December 31, 2022.
Item 14. Principal Accountant Fees and Services.
The information required by this item will be included in our definitive Proxy Statement for the 2023 Annual Meeting of Stockholders, if filed with the SEC within 120 days after December 31, 2022, and incorporated herein by reference, or will be provided in an amendment filed on Form 10-K/A with the SEC no later than 120 days after December 31, 2022.
82
PART IV
Item 15. Exhibit and Financial Statement Schedules.
(a)(1) Financial Statements. Reference is made to the Index to Consolidated Financial Statements beginning on Page F-1 hereof.
(a)(2) Financial Statement Schedules.
Financial statements schedules are omitted because they are not applicable, not required, or because the required information is included in the consolidated financial statements or notes thereto.
(a)(3) Exhibits.
The following is a list of exhibits filed as part of this Form 10-K.
Exhibit | Incorporated by Reference | Filed/Furnished | ||||||||||
Number |
| Exhibit Description |
| Form |
| File No. |
| Exhibit |
| Filing Date |
| Herewith |
2.1 | 8-K | 001-40033 | 2.1 | 6/1/21 | ||||||||
2.2 | 8-K | 001-40033 | 2.2 | 6/1/21 | ||||||||
2.3 | 8-K | 001-40033 | 2.1 | 11/22/21 | ||||||||
2.4 | 8-K | 001-40033 | 2.4 | 12/9/21 | ||||||||
2.5 | 8-K | 001-40033 | 2.5 | 12/9/21 | ||||||||
3.1 | Amended and Restated Certificate of Incorporation of the Company. | 8-K | 001-40033 | 3.1 | 12/9/21 | |||||||
3.2 | 8-K | 001-40033 | 3.2 | 12/9/21 | ||||||||
4.1 | S-1 | 333-251978 | 4.2 | 1/19/21 | ||||||||
4.2 | 8-K | 001-40033 | 4.1 | 2/16/21 | ||||||||
4.3 | 8-K | 001-40033 | 4.1 | 2/16/21 | ||||||||
4.4 | 10-K | 001-40033 | 4.4 | 10/21/22 | ||||||||
83
4.5 | 8-K | 001-4033 | 10.2 | 2/13/22 | ||||||||
10.1 | 8-K | 001-40033 | 10.1 | 12/9/21 | ||||||||
10.2 | 8-K | 001-40033 | 10.2 | 6/1/21 | ||||||||
10.3 | 8-K | 001-40033 | 10.1 | 11/22/21 | ||||||||
10.4 | 8-K | 001-40033 | 10.4 | 12/9/21 | ||||||||
10.5 | 8-K | 001-40033 | 10.5 | 12/9/21 | ||||||||
10.6 | 8-K | 001-40033 | 10.6 | 12/9/21 | ||||||||
10.7† | Form of Indemnification Agreement for directors and executive officers. | 8-K | 001-40033 | 10.7 | 12/9/21 | |||||||
10.8† | Form of Indemnification Agreement for sponsor affiliated directors. | 8-K | 001-40033 | 10.8 | 12/9/21 | |||||||
10.9† | 8-K | 001-4033 | 10.2 | 12/1/22 | ||||||||
10.10† | 8-K | 001-40033 | 10.12 | 12/9/21 | ||||||||
10.11† | First Amendment to the P3 Health Partners Inc. 2021 Incentive Award Plan. | 10-K | 001-40033 | 10.11 | 10/21/22 | |||||||
10.12† | 8-K | 001-40033 | 10.13 | 12/9/21 | ||||||||
10.13† | Form of Stock Option Award Agreement under the P3 Health Partners Inc. 2021 Incentive Award Plan. | 8-K | 001-40033 | 10.14 | 12/9/21 | |||||||
10.14† | P3 Health Group Holdings, LLC 2017 Management Incentive Plan. | 8-K | 001-40033 | 10.15 | 12/9/21 |
84
10.15† | 8-K | 001-40033 | 10.16 | 12/9/21 | ||||||||
10.16 | 8-K | 001-40033 | 10.17 | 12/9/21 | ||||||||
10.17 | 8-K | 001-40033 | 10.18 | 12/9/21 | ||||||||
10.18 | 10-K | 001-40033 | 10.18 | 10/21/22 | ||||||||
10.19 | 10-K | 001-40033 | 10.19 | 10/21/22 | ||||||||
10.20 | 10-K | 001-40033 | 10.20 | 10/21/22 | ||||||||
10.21† | 8-K | 001-40033 | 10.1 | 5/18/22 | ||||||||
10.22† | 8-K | 001-40033 | 10.2 | 5/18/22 | ||||||||
10.23† | 8-K | 001-40033 | 10.3 | 5/18/22 | ||||||||
10.24† | 8-K | 001-40033 | 10.4 | 5/18/22 | ||||||||
10.25† | 10-K | 001-40033 | 10.25 | 10/21/22 | ||||||||
10.26 | 8-K | 001-4033 | 10.1 | 12/13/22 | ||||||||
10.27 | 8-K | 001-4033 | 10.3 | 12/13/22 | ||||||||
10.28 | 8-K | 001-4033 | 10.4 | 12/13/22 |
85
10.29† | 10-Q | 001-4033 | 10.1 | 11/14/22 | ||||||||
21.1 | * | |||||||||||
23.1 | * | |||||||||||
31.1 | * | |||||||||||
31.2 | * | |||||||||||
32.1 | ** | |||||||||||
32.2 | ** | |||||||||||
101.INS | Inline XBRL Instance Document | * | ||||||||||
101.SCH | Inline XBRL Taxonomy Extension Schema Document | * | ||||||||||
101.CAL | Inline XBRL Taxonomy Extension Calculation Linkbase Document | * | ||||||||||
101.DEF | Inline XBRL Taxonomy Extension Definition Linkbase Document | * | ||||||||||
101.LAB | Inline XBRL Taxonomy Extension Label Linkbase Document | * | ||||||||||
101.PRE | Inline XBRL Taxonomy Extension Presentation Document | * | ||||||||||
104 | Cover Page Interactive Data File (formatted as Inline XBRL and contained in Exhibit 101) | * |
* | Filed herewith. |
** | Furnished herewith. |
† | Indicates management contract or compensatory plan. |
Item 16. Form 10-K Summary.
None.
86
SIGNATURES
Pursuant to the requirements of Section 13 or 15(d) of the Securities Exchange Act of 1934, the registrant has duly caused this report to be signed on its behalf by the undersigned, thereunto duly authorized.
P3 Health Partners Inc. | ||
By: | /s/ Sherif W. Abdou | |
Name: | Sherif W. Abdou, M.D. | |
Date: March 31, 2023 | Title: | Chief Executive Officer |
Pursuant to the requirements of the Securities Exchange Act of 1934, this report has been signed below by the following persons on behalf of the registrant and in the capacities and on the dates indicated.
Signature |
| Title |
| Date |
/s/ Sherif W. Abdou | Chief Executive Officer and Director | March 31, 2023 | ||
Sherif W. Abdou, M.D. | (Principal Executive Officer) | |||
/s/ Atul Kavthekar | Chief Financial Officer | March 31, 2023 | ||
Atul Kavthekar | (Principal Financial Officer and Principal Accounting Officer) | |||
/s/ Mark Thierer | Chairman of the Board of Directors | March 31, 2023 | ||
Mark Thierer | ||||
/s/ Amir S. Bacchus | Chief Medical Officer and Director | March 31, 2023 | ||
Amir S. Bacchus, M.D. | ||||
/s/ Gregory N. Kazarian | Director | March 31, 2023 | ||
Gregory N. Kazarian | ||||
/s/ Lawrence B. Leisure | Director | March 31, 2023 | ||
Lawrence B. Leisure | ||||
/s/ Jeffrey G. Park | Director | March 31, 2023 | ||
Jeffrey G. Park | ||||
/s/ Thomas E. Price | Director | March 31, 2023 | ||
Thomas E. Price, M.D. | ||||
/s/ Mary A. Tolan | Director | March 31, 2023 | ||
Mary A. Tolan | ||||
/s/ Greg Wasson | Director | March 31, 2023 | ||
Greg Wasson |
Index to Consolidated Financial Statements
Page | |
Report of Independent Registered Public Accounting Firm (BDO USA, LLP; Las Vegas, Nevada; PCAOB ID#243) | F-2 |
Consolidated Balance Sheets as of December 31, 2022 and 2021 | F-3 |
F-4 | |
F-5 | |
F-6 | |
F-7 |
F-1
REPORT OF INDEPENDENT REGISTERED PUBLIC ACCOUNTING FIRM
Shareholders and Board of Directors
P3 Health Partners Inc.
Henderson, Nevada
Opinion on the Consolidated Financial Statements
We have audited the accompanying consolidated balance sheets of P3 Health Partners Inc. (the “Company”), as of December 31, 2022 and 2021 (Successor), and the related statements of operations, changes in stockholders’/members’ equity (deficit) and mezzanine equity, and cash flows for the year ended December 31, 2022 and for the period from December 3, 2021 to December 31, 2021 (Successor) and the period from January 1, 2021 to December 2, 2021 (Predecessor), and the related notes to the consolidated financial statements (collectively referred to as the “consolidated financial statements”). In our opinion, the consolidated financial statements present fairly, in all material respects, the financial position of the Company at December 31, 2022 and 2021 (Successor), and the results of its operations and its cash flows for the year ended December 31, 2022 and for the period from December 3, 2021 to December 31, 2021 (Successor) and the period from January 1, 2021 to December 2, 2021 (Predecessor), in conformity with accounting principles generally accepted in the United States of America.
Going Concern Uncertainty
The accompanying consolidated financial statements have been prepared assuming that the Company will continue as a going concern. As discussed in Note 2 to the consolidated financial statements, the Company has suffered recurring losses from operations that raises substantial doubt about its ability to continue as a going concern. Management’s plans in regard to this matter is also described in Note 2. The consolidated financial statements do not include any adjustments that might result from the outcome of this uncertainty.
Basis for Opinion
These consolidated financial statements are the responsibility of the Company’s management. Our responsibility is to express an opinion on the Company’s consolidated financial statements based on our audits. We are a public accounting firm registered with the Public Company Accounting Oversight Board (United States) (“PCAOB”) and are required to be independent with respect to the Company in accordance with the U.S. federal securities laws and the applicable rules and regulations of the Securities and Exchange Commission and the PCAOB.
We conducted our audits in accordance with the standards of the PCAOB. Those standards require that we plan and perform the audit to obtain reasonable assurance about whether the consolidated financial statements are free of material misstatement, whether due to error or fraud. The Company is not required to have, nor were we engaged to perform, an audit of its internal control over financial reporting. As part of our audits we are required to obtain an understanding of internal control over financial reporting but not for the purpose of expressing an opinion on the effectiveness of the Company’s internal control over financial reporting. Accordingly, we express no such opinion.
Our audits included performing procedures to assess the risks of material misstatement of the consolidated financial statements, whether due to error or fraud, and performing procedures that respond to those risks. Such procedures included examining, on a test basis, evidence regarding the amounts and disclosures in the consolidated financial statements. Our audits also included evaluating the accounting principles used and significant estimates made by management, as well as evaluating the overall presentation of the consolidated financial statements. We believe that our audits provide a reasonable basis for our opinion.
/s/ BDO USA, LLP
We have served as the Company’s auditor since 2021.
Las Vegas, Nevada
March 31, 2023
F-2
P3 HEALTH PARTNERS INC and SUBSIDIARIES
CONSOLIDATED BALANCE SHEETS
(Dollars in thousands, except per share amounts)
December 31, | ||||||
| 2022 |
| 2021 | |||
ASSETS | ||||||
CURRENT ASSETS: |
|
|
| |||
Cash | $ | 17,537 | $ | 140,478 | ||
Restricted cash |
| 920 |
| 356 | ||
Health plan receivable |
| 72,092 |
| 50,251 | ||
Clinic fees and insurance receivable, net |
| 822 |
| 1,090 | ||
Other receivable |
| 6,678 |
| 727 | ||
Prepaid expenses and other current assets | 2,643 |
| 6,959 | |||
TOTAL CURRENT ASSETS |
| 100,692 |
| 199,861 | ||
LONG-TERM ASSETS: |
|
|
| |||
Property and equipment, net | 8,839 | 8,048 | ||||
Goodwill |
| — |
| 1,309,750 | ||
Intangible assets, net | 751,050 | 835,839 | ||||
Other long-term assets | 15,990 | 10,611 | ||||
TOTAL LONG-TERM ASSETS |
| 775,879 |
| 2,164,248 | ||
TOTAL ASSETS (1) | $ | 876,571 | $ | 2,364,109 | ||
LIABILITIES, MEZZANINE EQUITY, and STOCKHOLDERS’ EQUITY |
|
|
| |||
CURRENT LIABILITIES: |
|
|
| |||
Accounts payable | $ | 11,542 | $ | 5,469 | ||
Accrued expenses and other current liabilities | 16,647 | 12,261 | ||||
Accrued payroll |
| 8,224 |
| 6,304 | ||
Health plan settlements payable |
| 13,608 |
| 22,549 | ||
Claims payable |
| 151,207 |
| 101,958 | ||
Premium deficiency reserve |
| 26,375 |
| 37,836 | ||
Accrued interest |
| 14,061 |
| 8,771 | ||
Current portion of long-term debt |
| — |
| 46 | ||
Short-term debt | — | 3,579 | ||||
TOTAL CURRENT LIABILITIES | 241,664 | 198,773 | ||||
LONG-TERM LIABILITIES: |
|
| ||||
Operating lease liability |
| 11,516 |
| 6,297 | ||
Warrant liabilities |
| 1,517 |
| 11,383 | ||
Contingent consideration | 4,794 | 3,487 | ||||
Long-term debt, net |
| 94,421 |
| 80,000 | ||
TOTAL LONG-TERM LIABILITIES |
| 112,248 |
| 101,167 | ||
TOTAL LIABILITIES (1) |
| 353,912 |
| 299,940 | ||
COMMITMENTS AND CONTINGENCIES (NOTE 17 AND NOTE 21) | ||||||
MEZZANINE EQUITY | ||||||
Redeemable non-controlling interest | 516,805 | 1,790,617 | ||||
STOCKHOLDERS’ EQUITY: |
|
|
|
| ||
Class A common stock, $0.0001 par value; 800,000,000 shares authorized; 41,578,890 shares issued and outstanding as of December 31, 2022 and 2021 | 4 | 4 | ||||
Class V common stock, $0.0001 par value; 205,000,000 shares authorized; 201,592,012 and 196,553,523 shares and as of December 31, 2022 and 2021, respectively | 20 | 20 | ||||
Additional paid in capital | 315,375 | 312,946 | ||||
Accumulated deficit | (309,545) | (39,418) | ||||
TOTAL STOCKHOLDERS’ EQUITY |
| 5,854 |
| 273,552 | ||
TOTAL LIABILITIES, MEZZANINE EQUITY, and STOCKHOLDERS’ EQUITY | $ | 876,571 | $ | 2,364,109 | ||
(1) | The Company’s consolidated balance sheets include the assets and liabilities of its consolidated variable interest entities (“VIEs”). As discussed in Note 23: Variable Interest Entities, P3 LLC is itself a VIE. P3 LLC represents substantially all the assets and liabilities of the Company. As a result, the language and numbers below refer only to VIEs held at the P3 LLC level. The consolidated balance sheets include total assets that can be used only to settle obligations of P3 LLC’s consolidated VIEs totaling $3.1 million and $8.1 million as of December 31, 2022 and 2021, respectively, and total liabilities of P3 LLC’s consolidated VIEs for which creditors do not have recourse to the general credit of the Company totaled $9.9 million and $6.1 million as of December 31, 2022 and 2021, respectively. These VIE assets and liabilities do not include $33.0 million of net amounts due to affiliates as of December 31, 2022 and $6.0 million of investment in affiliates and $24.1 million of amounts due to affiliates as of December 31, 2021 as these are eliminated in consolidation and not presented within the consolidated balance sheets. |
See accompanying notes to consolidated financial statements.
F-3
P3 HEALTH PARTNERS INC and SUBSIDIARIES
CONSOLIDATED STATEMENTS OF OPERATIONS
(In thousands, except per share amounts)
Successor | Predecessor | ||||||||||
Year Ended | December 3, 2021 | January 1, 2021 | |||||||||
December 31, | through December 31, | through December 2, | |||||||||
| 2022 |
|
| 2021 |
| ||||||
| |||||||||||
OPERATING REVENUE: |
|
|
|
| |||||||
Capitated revenue | $ | 1,034,800 | $ | 57,224 | $ | 567,735 | |||||
Other patient service revenue |
| 14,671 |
| 1,538 |
| 10,867 | |||||
TOTAL OPERATING REVENUE |
| 1,049,471 |
| 58,762 |
| 578,602 | |||||
OPERATING EXPENSE: |
|
|
|
|
| ||||||
Medical expense |
| 1,057,224 |
| 66,877 |
| 592,465 | |||||
Premium deficiency reserve |
| (11,461) |
| 26,277 |
| 11,559 | |||||
Corporate, general and administrative expense |
| 157,284 |
| 16,983 |
| 100,243 | |||||
Sales and marketing expense |
| 5,096 |
| 364 |
| 1,818 | |||||
Depreciation and amortization |
| 87,289 |
| 7,149 |
| 1,575 | |||||
Goodwill impairment | 1,314,952 | — | — | ||||||||
TOTAL OPERATING EXPENSE |
| 2,610,384 |
| 117,650 |
| 707,660 | |||||
OPERATING LOSS |
| (1,560,913) |
| (58,888) |
| (129,058) | |||||
OTHER INCOME (EXPENSE): |
|
|
|
|
| ||||||
Interest expense, net |
| (11,404) |
| (851) |
| (9,824) | |||||
Mark-to-market of stock warrants | 9,865 | 2,272 | (7,665) | ||||||||
Other |
| 2,757 |
| (471) |
| 147 | |||||
TOTAL OTHER INCOME (EXPENSE) |
| 1,218 |
| 950 |
| (17,342) | |||||
LOSS BEFORE INCOME TAXES | (1,559,695) | (57,938) | (146,400) | ||||||||
PROVISION FOR INCOME TAXES | (1,862) | — | — | ||||||||
NET LOSS |
| (1,561,557) |
| (57,938) |
| (146,400) | |||||
LESS: NET LOSS ATTRIBUTABLE TO REDEEMABLE NON-CONTROLLING INTERESTS | (1,291,430) |
| (47,857) |
| — | ||||||
NET LOSS ATTRIBUTABLE TO CONTROLLING INTERESTS | $ | (270,127) | $ | (10,081) | $ | (146,400) | |||||
NET LOSS PER SHARE (BASIC) | $ | (6.50) | $ | (0.24) | N/A(1) | ||||||
NET LOSS PER SHARE (DILUTED) | $ | (6.50) | $ | (0.24) | N/A(1) | ||||||
WEIGHTED AVERAGE COMMON SHARES OUTSTANDING (BASIC) | 41,579 | 41,579 | N/A(1) | ||||||||
WEIGHTED AVERAGE COMMON SHARES OUTSTANDING (DILUTED) | 41,579 | 41,579 | N/A(1) | ||||||||
(1) | The Company analyzed the calculation of net loss per member unit for predecessor periods prior to the Business Combinations (Note 5) and determined that it resulted in values that would not be meaningful to the users of these consolidated financial statements; therefore, net loss per member unit information has not been presented for predecessor periods prior to the Business Combinations (Note 5) on December 3, 2021. |
See accompanying notes to consolidated financial statements.
F-4
P3 HEALTH PARTNERS INC and SUBSIDIARIES
CONSOLIDATED STATEMENTS OF STOCKHOLDERS’/MEMBERS’ DEFICIT AND MEZZANINE EQUITY
(Dollars in thousands)
| Predecessor | |||||||||||||||||||||||||||||
Class A Units Subject to | Class D Units Subject to | |||||||||||||||||||||||||||||
Possible Redemption | Possible Redemption | Class B-1 | Class C | Redemption | Total | |||||||||||||||||||||||||
|
|
|
|
|
|
| of | Accumulated | Members’ | |||||||||||||||||||||
| Units |
| Amount |
| Units |
| Amount |
| Units |
| Amount |
| Units |
| Amount |
| Profit Interests |
| Deficit |
| Deficit | |||||||||
MEMBERS’ DEFICIT, as of December 31, 2020 |
| 43,000,000 | $ | 43,656 | 16,130,034 | $ | 47,042 |
| 6,000,000 | $ | 380 |
| 1,302,083 | $ | 67 | $ | (180) | $ | (130,485) | $ | (130,218) | |||||||||
Class B-1 and Class C Unit Based Compensation |
| — |
| — |
| — |
| — |
| 2,000,000 |
| 380 |
| 660,417 |
| 902 |
| — |
| — |
| 1,282 | ||||||||
Class B-2 Units Accelerated on Merger Date |
| — |
| — |
| — |
| — |
| 4,054,054 |
| 81 |
| — |
| — |
| — |
| — |
| 81 | ||||||||
Class B-3 Units Accelerated on Merger Date |
| — |
| — | — |
| — |
| 5,647,438 |
| 56 |
| — |
| — |
| — |
| — |
| 56 | |||||||||
Class C-1 Units Accelerated on Merger Date |
| — |
| — |
| — |
| — |
| — |
| — |
| 1,035,833 |
| 2,243 |
| — |
| — |
| 2,243 | ||||||||
Class C-2 Units Accelerated on Merger Date |
| — |
| — | — |
| — |
| — |
| — |
| 1,685,000 |
| 39 |
| — |
| — |
| 39 | |||||||||
Net Loss |
| — |
| — | — |
| — |
| — |
| — |
| — |
| — |
| — |
| (146,400) |
| (146,400) | |||||||||
MEMBERS’ DEFICIT, as of December 2, 2021 |
| 43,000,000 | $ | 43,656 | 16,130,034 | $ | 47,042 |
| 17,701,492 | $ | 897 |
| 4,683,333 | $ | 3,251 | $ | (180) | $ | (276,885) | $ | (272,917) | |||||||||
Successor | |||||||||||||||||||||||||
Redeemable | |||||||||||||||||||||||||
Non-controlling | Class A Common Stock | Class V Common Stock | Additional Paid | Accumulated | Total Stockholders’ | ||||||||||||||||||||
| Interest |
|
| Shares |
| Amount |
| Shares |
| Amount |
| in Capital (1) |
| Deficit |
| Equity | |||||||||
STOCKHOLDERS’ EQUITY, December 3, 2021 |
| $ | 1,833,838 | 41,578,890 | $ | 4 | 196,553,523 |
| $ | 20 | $ | 312,946 |
| $ | (29,337) | $ | 283,633 | ||||||||
Equity-based compensation |
| 4,635 | — |
| — |
| — |
| — |
| — |
| — |
| — | ||||||||||
Net loss |
| (47,856) | — |
| — | — |
| — |
| — |
| (10,081) |
| (10,081) | |||||||||||
STOCKHOLDERS’ EQUITY, December 31, 2021 |
| | 1,790,617 | 41,578,890 | | 4 | 196,553,523 |
| 20 | 312,946 |
| (39,418) | 273,552 | ||||||||||||
Vesting of Class V common stock awards | — | — | — | 5,038,489 | — | — | — | — | |||||||||||||||||
Equity-based compensation | 17,618 | — | — | — | — | 1,786 | — | 1,786 | |||||||||||||||||
Class A common stock warrants issued | — | — | — | — | — | 643 | — | 643 | |||||||||||||||||
Net loss | | | (1,291,430) | | | | — | | | — | | | — | | | — | | | — | | | (270,127) | | | (270,127) |
STOCKHOLDERS’ EQUITY, December 31, 2022 | | $ | 516,805 | | | 41,578,890 | | $ | 4 | | 201,592,012 | | $ | 20 | | $ | 315,375 | | $ | (309,545) | | $ | 5,854 | ||
(1) | Included in the opening balance are transactions completed in connection with the Business Combinations (Note 5), including the PIPE Investment (Note 1) of $195.3 million (net of issuance costs), the equity consideration to P3 shareholders of $80.3 million, and the trust proceeds (net of redemptions) of $37.4 million. |
See accompanying notes to consolidated financial statements.
F-5
P3 HEALTH PARTNERS INC and SUBSIDIARIES
CONSOLIDATED STATEMENTS OF CASH FLOWS
(In thousands)
Successor | Predecessor | |||||||||
Year Ended | December 3, 2021 | January 1, 2021 | ||||||||
December 31, | through December 31, | through December 2, | ||||||||
| 2022 |
| 2021 |
|
| 2021 | ||||
CASH FLOWS FROM OPERATING ACTIVITIES: | ||||||||||
Net loss | $ | (1,561,557) | $ | (57,938) | $ | (146,400) | ||||
Adjustments to reconcile net loss to net cash used in operating activities: | ||||||||||
Depreciation and amortization |
| 87,289 |
| 7,149 |
| 1,575 | ||||
Equity-based compensation | 19,404 | 4,635 | 3,701 | |||||||
Goodwill impairment | 1,314,952 | — | — | |||||||
Amortization of original issue discount and debt issuance costs | — | — | 1,798 | |||||||
Accretion of contingent consideration | 400 | — | — | |||||||
Mark-to-market of stock warrants | (9,865) | (2,272) | 7,665 | |||||||
Premium deficiency reserve |
| (11,461) |
| 26,277 |
| 11,559 | ||||
Changes in operating assets and liabilities: | ||||||||||
Health plan receivable |
| (21,841) |
| 3,236 |
| (2,770) | ||||
Clinic fees, insurance, and other receivables | (5,338) | 1,467 | (1,485) | |||||||
Prepaid expenses and other current assets | 4,266 | (4,704) | 4,254 | |||||||
Other long-term assets |
| 100 |
| — |
| — | ||||
Accounts payable, accrued expenses, and other current liabilities | 6,082 | 7,732 | 34,224 | |||||||
Accrued payroll |
| 1,920 |
| 3,159 |
| (1,134) | ||||
Health plan settlements payable | (8,941) | (2,592) | 11,265 | |||||||
Claims payable | 49,249 | (971) | 19,097 | |||||||
Accrued interest | 5,290 | (498) | 5,216 | |||||||
Operating lease liability | 4,032 | (22) | 306 | |||||||
Net cash used in operating activities |
| (126,019) |
| (15,342) |
| (51,129) | ||||
CASH FLOWS FROM INVESTING ACTIVITIES: | ||||||||||
Purchases of property and equipment | (2,233) | (120) | (3,290) | |||||||
Acquisitions, net of cash acquired |
| (5,500) |
| (47,879) |
| (4,989) | ||||
Notes receivable | — | 143 | 70 | |||||||
Net cash used in investing activities |
| (7,733) |
| (47,856) |
| (8,209) | ||||
CASH FLOWS FROM FINANCING ACTIVITIES: | ||||||||||
Proceeds from PIPE, net of issuance costs | — | 195,308 | — | |||||||
Proceeds from long-term debt, net of original issue discount | 15,000 | — | 25,000 | |||||||
Proceeds from short-term debt | — | 3,377 | 351 | |||||||
Payment of long-term debt |
| (46) |
| (8) |
| (186) | ||||
Payment of debt issuance costs | — | — | (375) | |||||||
Payment of short-term debt | (3,579) | — | — | |||||||
Net cash provided by financing activities |
| 11,375 |
| 198,677 |
| 24,790 | ||||
Net change in cash and restricted cash | (122,377) | 135,479 | (34,548) | |||||||
Cash and restricted cash at beginning of period |
| 140,834 |
| 5,355 |
| 39,903 | ||||
Cash and restricted cash at end of period | $ | 18,457 | $ | 140,834 | $ | 5,355 | ||||
Supplemental disclosure of cash flow information: | | |||||||||
Cash paid for interest | | $ | 5,714 | $ | 1,346 | $ | 2,796 | |||
Supplemental disclosures of non-cash investing and financing information: | | |||||||||
Operating lease liabilities arising from obtaining new right-of-use assets | | $ | 6,839 | $ | 314 | $ | 4,073 | |||
Warrants issued in connection with new debt | | $ | 643 | $ | — | $ | — | |||
Increase in accrued expenses related to debt issuance costs and original issue discount | | $ | 525 | $ | — | $ | — | |||
Reconciliation of cash and restricted cash: | | |||||||||
Cash | | $ | 17,537 | $ | 140,478 | $ | 5,301 | |||
Restricted cash | | 920 | 356 | 54 | ||||||
Total cash and restricted cash | | $ | 18,457 | $ | 140,834 | $ | 5,355 | |||
See accompanying notes to consolidated financial statements.
F-6
P3 HEALTH PARTNERS INC. and SUBSIDIARIES
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS
(Dollars in thousands except per share amounts, or as otherwise stated)
Note 1: Organization
P3 Health Partners Inc. (“P3”), f/k/a Foresight Acquisition Corp., is a patient-centered and physician-led population health management company and, for accounting purposes, the successor to P3 Health Group Holdings, LLC and its subsidiaries (collectively, “P3 LLC,” and together with P3, the “Company”).
P3 LLC was founded on April 12, 2017 and began commercial operations on April 20, 2017 to provide population health management services on an at-risk basis to insurance plans offering medical coverage to Medicare beneficiaries under Medicare Advantage programs. Medicare Advantage programs are insurance products created solely for Medicare beneficiaries. Insurance plans contract directly with the Centers for Medicare and Medicaid Services (“CMS”) to offer Medicare beneficiaries benefits that replace traditional Medicare fee-for-service (“FFS”) coverage.
On December 3, 2021, (the “Closing Date”), P3 and P3 LLC consummated a series of business combinations pursuant to which, among other things, P3 LLC merged with and into FAC Merger Sub LLC, a Delaware limited liability company and wholly owned subsidiary of the Company (“Merger Sub”) (the “P3 Merger”), with Merger Sub as the surviving company, which was renamed P3 LLC, and FAC-A Merger Sub Corp., a Delaware corporation and a wholly owned subsidiary of P3, FAC-B Merger Sub Corp., a Delaware corporation and a wholly owned subsidiary of the P3 (together with FAC-A Merger Sub Corp., the “Merger Corps”) merged with and into CPF P3 Blocker-A, LLC, a Delaware limited liability company, CPF P3 Blocker-B, LLC a Delaware limited liability company (together with CPF P3 Blocker-A, LLC, the “Blockers”), with the Blockers as the surviving entities and wholly owned subsidiaries of P3 (collectively, the “Business Combinations”). Upon completion of the Business Combinations (the “Closing”), the Company was organized in an “Up-C” structure in which P3 directly owned approximately 17.1% of the common units of P3 LLC (“Common Units”) and became the sole manager of P3 LLC. Following the Closing, substantially all of the Company’s assets are held and operations are conducted by P3 LLC, and P3’s only assets are equity interests in P3 LLC.
Upon closing of the Business Combinations:
| ● | 8.7 million shares of Class A common stock were issued as part of the purchase consideration; |
| ● | 3.7 million shares of Class A common stock (after redemptions) were no longer subject to redemption; |
| ● | 8.8 million shares of Class A common stock held by the founder holders remained outstanding; and |
| ● | 20.4 million shares of Class A common stock were issued in a private placement pursuant to subscription agreements entered into effective as of March 25, 2021 (the “PIPE Investment”). |
The Company’s contracts with health plans are based on an at-risk shared savings model. Under this model, the Company is financially responsible for the cost of all contractually-covered services provided to members assigned to the Company by health plans in exchange for a fixed monthly “capitation” payment, which is generally a percentage of the payment health plans receive from CMS. Under this arrangement, Medicare beneficiaries generally receive all their healthcare coverage through the Company’s network of employed and affiliated physicians and specialists.
The services provided to health plans’ members vary by contract. These may include utilization management, care management, disease education, and maintenance of a quality improvement and quality management program for members assigned to the Company. The Company is also responsible for the credentialing of its providers, processing and payment of claims, and the establishment of a provider network for certain health plans.
In addition to the Company’s contracts with health plans, the Company provides primary healthcare services through its employed physician clinic locations. These primary care clinics are reimbursed for services provided under FFS contracts with various payers and through capitated – per member, per month (“PMPM”) arrangements.
F-7
Note 2: Going Concern and Liquidity
The accompanying consolidated financial statements have been prepared assuming the Company will continue as a going concern. The Company has experienced losses since its inception and net losses of $1,561.6 million for the year ended December 31, 2022, $57.9 million for the Successor Period of 2021 (as defined in Note 3), and $146.4 million for the Predecessor Period of 2021 (as defined in Note 3). Such losses were primarily the result of goodwill impairment charges in 2022 and costs incurred in adding new members, building relationships with physician partners and payors, and developing new services. The Company anticipates operating losses and negative cash flows to continue for the foreseeable future as it continues to grow membership.
As of December 31, 2022 and 2021, the Company had $17.5 million and $140.5 million, respectively, in cash available to fund future operations. The Company’s capital requirements will depend on many factors, including the pace of its growth, ability to manage medical costs, the maturity of its members, and its ability to raise capital, and the Company will need to use available capital resources and/or raise additional capital earlier than currently anticipated. When the Company pursues additional debt and/or equity financing, there can be no assurance that such financing will be available on terms commercially acceptable to the Company. If the Company is unable to obtain additional funding when needed, it will need to curtail planned activities in order to reduce costs, which will likely have an unfavorable effect on the Company’s ability to execute on its business plan, and have an adverse effect on its business, results of operations, and future prospects. As a result of these matters, substantial doubt exists about the Company’s ability to continue as a going concern within one year after the date the financial statements are issued. The accompanying consolidated financial statements do not include any adjustments that might result from the outcome of these uncertainties.
Note 3: Significant Accounting Policies
Basis of Presentation and Principles of Consolidation
The accompanying consolidated financial statements are prepared in accordance with accounting principles generally accepted in the United States (“GAAP”) and include the accounts of the Company. All intercompany accounts and transactions have been eliminated.
The Company periodically evaluates entities for consolidation either through ownership of a majority voting interest, or through means other than voting interest, in accordance with the Variable Interest Entity (“VIE”) accounting model. This evaluation includes a qualitative review of the design of the entity, its organizational structure, including decision making ability and financial agreements, as well as a quantitative review. The Company consolidates a VIE when it has a variable interest that provides it with a controlling financial interest in the VIE, referred to as the primary beneficiary of the VIE. See Note 23 “Variable Interest Entities.”
As the sole managing manager of P3 LLC, P3 has the right to direct the most significant activities of P3 LLC and the obligation to absorb losses and receive benefits. The rights of the non-managing members of P3 LLC are limited and protective in nature and do not give substantive participation rights over the sole managing member. Accordingly, P3 identifies itself as the primary beneficiary of P3 LLC and began consolidating P3 LLC as of the Closing Date resulting in a noncontrolling interest related to the Common Units held by members other than P3. Additionally, as more fully described in Note 23 “Variable Interest Entities,” P3 LLC is the primary beneficiary of the following physician practices (collectively, the “Network”):
| ● | Kahan, Wakefield, Abdou, PLLC |
| ● | Bacchus, Wakefield, Kahan, PC |
| ● | P3 Health Partners Professional Services, P.C. |
| ● | P3 Medical Group, P.C. |
| ● | P3 Health Partners California, P.C. (f/k/a Omni IPA Medical Group, Inc.) |
F-8
As a result of the Business Combinations, P3 LLC has been determined to be the predecessor for accounting purposes and, accordingly, the consolidated financial statements and notes to consolidated financial statements of P3 LLC are presented herein as “Predecessor” for the period prior to the Closing Date (the “Predecessor Period”) and the consolidated financial statements and notes to consolidated financial statements of the Company are presented herein as “Successor” for the period after the Closing Date (the “Successor Period”), which include the consolidated operations of P3 LLC. The accompanying consolidated financial statements include a black line division that indicates that the Predecessor and Successor reporting entities shown are presented on a different basis and are, therefore, not comparable.
Comprehensive Loss
Comprehensive loss includes net loss to common stockholders as well as other changes in equity that result from transactions and economic events other than those with stockholders. There was no difference between comprehensive loss and net loss to common stockholders for the periods presented.
Management’s Use of Estimates
Preparation of these consolidated financial statements and accompanying footnotes, in conformity with GAAP, requires management to make estimates and assumptions that could affect amounts reported here. Management bases its estimates on the best information available at the time, its experiences and various other assumptions believed to be reasonable under the circumstances, including estimates of the impact of COVID-19. See Note 21 “Commitments and Contingencies” for further discussion on the impact of COVID-19.
The areas where significant estimates are used in these accompanying consolidated financial statements include revenue recognition, the liability for unpaid claims, equity-based compensation, premium deficiency reserves, fair value and impairment recognition of long-lived assets (including intangible assets and goodwill), fair value of acquired assets and liabilities in business combinations, fair value of liability classified instruments, and judgments related to deferred income taxes. Actual results could differ from those estimates.
Commitments and Contingencies
An accrual is established for commitments and contingencies when management, after considering the facts and circumstances of each matter as then known to management, has determined a specific contingency is probable and estimable. The Company also faces contingencies that are reasonably possible to occur that cannot currently be estimated. When only a range of amounts is reasonably estimable and no amount within the range is more likely than another, the low end of the range is recorded. The Company expenses costs associated with loss contingencies, including any related legal fees, as they are incurred. Due to the inherent uncertainties surrounding gain contingencies, the Company does not recognize potential gains until realized.
Loss per Share
Basic net loss per share attributable to common stockholders is computed by dividing the net loss attributable to common stockholders by the weighted-average number of shares of common stock outstanding during the period. Diluted earnings per share attributable to common stockholders adjusts basic earnings per share for the potentially dilutive impact of public warrants, private placement warrants, stock options, and Common Units convertible into shares of Class A common stock during the period by applying the treasury stock method or if-converted method, as applicable.
Net loss per member unit has not been presented for Predecessor Period as the Company’s management determined it would not be meaningful to the users of these consolidated financial statements.
Cash and Restricted Cash
Cash includes all cash and liquid investments with an initial maturity of three months or less. Cash deposits held in accounts at each financial institution are insured up to $250,000 by the Federal Deposit Insurance Corporation (“FDIC”). The Company maintains its cash in bank deposit accounts that, at times, may exceed FDIC insured limits. Management does not expect any losses to occur on such accounts.
F-9
At December 31, 2022 and 2021, the Company had cash of $17.5 million and $140.5 million, respectively, deposited at banking institutions which are subject to the FDIC insured limit.
Restricted cash is held for a specific purpose (such as payment of employee healthcare claims) and is thus not available to the Company for immediate or general business use. At December 31, 2022 and 2021, the Company had restricted cash of $0.9 million and $0.4 million, respectively.
Revenue Recognition
The Company categorizes revenue based on various factors such as the nature of contracts as follows:
Successor | Predecessor | ||||||||||||||||
Year Ended | December 3, 2021 | January 1, 2021 | |||||||||||||||
December 31, | through December 31, | through December 2, | |||||||||||||||
Revenue Type |
| 2022 |
| % of Total |
| 2021 |
| % of Total |
|
| 2021 |
| % of Total |
| |||
Capitated revenue | $ | 1,034,800 | 99 | % | $ | 57,224 | 97 | % | $ | 567,735 | 98 | % | |||||
Other patient service revenue: | |||||||||||||||||
Clinical fees & insurance revenue |
| 6,158 | 0 | % | 751 |
| 2 | % | 4,318 |
| 1 | % | |||||
Shared risk revenue |
| 351 | 0 | % | 181 |
| 0 | % | 602 |
| 0 | % | |||||
Care coordination / management fees | 7,924 | 1 | % | 600 | 1 | % | 5,880 | 1 | % | ||||||||
Incentive fees |
| 238 | 0 | % | 6 |
| 0 | % | 67 |
| 0 | % | |||||
Total other patient service revenue |
| 14,671 | 1 | % | 1,538 |
| 3 | % | 10,867 |
| 2 | % | |||||
Total revenue | $ | 1,049,471 | 100 | % | $ | 58,762 |
| 100 | % | $ | 578,602 |
| 100 | % | |||
During the year ended December 31, 2022, the Period of 2021, and the Period of 2021, four health plan customers each accounted for 10% or more of total revenue and collectively comprised 66%, 70%, and 78%, respectively, of the Company’s total revenue.
Capitated Revenue
The Company contracts with health plans using an at-risk model. Under the at-risk model, the Company is responsible for the cost of all covered services provided to members assigned by the health plans to the Company in exchange for a fixed premium payment, which generally is a percentage of the payment (“POP”) based on health plans’ premiums received from CMS. Through this capitation arrangement, the Company stands ready to provide assigned Medicare Advantage beneficiaries all their medical care via the Company’s directly employed and affiliated physician/specialist network.
The capitated revenue the Company receives is determined via a competitive bidding process with CMS and is based on the costs of care in local markets and the average utilization of services by patients enrolled. Medicare pays capitation using a “risk adjustment model,” which compensates providers based on the health status (acuity) of each individual patient. Medicare Advantage plans with higher acuity patients receive higher premiums. Conversely, Medicare Advantage plans with lower acuity patients receive lesser premiums. Under the risk adjustment model, capitation is paid on an interim basis based on enrollee data submitted for the preceding year and is adjusted in subsequent periods after final data is compiled. The Company generally estimates transaction prices using the most likely methodology. Amounts are only included in the transaction price to the extent any significant uncertainty of reversal on cumulative revenue will not occur and is resolved. In certain contracts, PMPM fees also include adjustments for items such as performance incentives or penalties based on the achievement of certain clinical quality metrics as contracted with payors.
F-10
Capitated revenue is recognized based on an estimated PMPM transaction price to transfer the service for a distinct increment of the series (e.g., month), net of projected acuity adjustments and performance incentives or penalties as the Company cannot reasonably estimate the ultimate PMPM payment of those contracts. The Company recognizes revenue in the month in which eligible members are entitled to receive healthcare benefits during the contract term. The capitation amount is subject to possible retroactive premium risk adjustments based on the member’s individual acuity. Premium risk adjustments recorded in 2022 which relate to 2021 were $3.3 million. There were no premium risk adjustments recorded in 2021 related to prior years. As the period between the time of service and time of payment is typically one year or less, the Company elected the practical expedient not to adjust for the effects of a significant financing component.
The Company’s contracts with health plans may include core functions and services for managing assigned patients’ medical care, the combination of which is offered as a single solution. Capitation contracts have a single performance obligation that is a stand ready obligation to perform healthcare services to the population of enrolled members and constitutes a series for the provision of managed healthcare services for the term of the contract, which is deemed to be one month since the mix of patients-customers can change month over month. The Company does not offer nor price each individual function as a standalone service to health plans; however, the addition or exclusion of certain services may be negotiated and reflected in each health plan’s specific total POP.
At December 31, 2022 and 2021, the Company had POP contracts in effect with 24 health plans (across five states) and 17 health plans (across four states), respectively.
Each month, in accordance with contractual obligations (for non-delegated health plans; e.g., those for which the Company has not been delegated for claims processing), each plan funds a medical claims payment reserve equal to a defined percentage of premium attributable to members assigned to the Company. In turn, the Company administers and funds medical claims for contractually covered services, for assigned health plan members, from that health plan’s reserve. On a quarterly or monthly basis, health plans conduct a settlement of the reserve to determine any surplus or deficit amount. The reconciliation and distribution of the reserve occur within 120 days following the end of each quarter. An annual settlement reconciliation and distribution from all funds occurs within months following each year-end.
Three health plan customers accounted for 10% or more of total health plan receivables as of December 31, 2022. Two health plan customers accounted for 10% or more of total health plan receivables as of December 31, 2021.
At December 31, 2022 and 2021, Management has deemed the Company’s settlement receivables to be fully collectible from those health plans where the Company is not delegated for claims processing. Accordingly, a constraint on the variable consideration associated with settlement receivables was not recorded.
Other Patient Service Revenue – Clinical Fees and Insurance Revenue
Clinical fees and insurance revenue relates to net patient fees received from various payors and direct patients under contracts in which the Company’s sole performance obligation is to provide healthcare services through the operation of medical clinics. The Company recognizes clinic fees and insurance revenue in the period in which services are provided. Under FFS payment arrangements, revenue is recognized on the date of service using a portfolio approach. The Company’s performance obligations are typically satisfied in the same day services are provided. All the Company’s contracts with its customers under these arrangements include a single performance obligation.
The Company’s contractual relationships with patients, in most cases, also involve third-party payors (Medicare, Medicaid, managed care health plans and commercial insurance companies, including plans offered through state-sponsored health insurance exchanges). Transaction prices for services provided are dependent upon specific rules in place with third party payors–specifically, Medicare/Medicaid and pre-negotiated rates with managed care health plans and commercial insurance companies. Contractual arrangements with third parties typically include payments at amounts which are less than standard charges. These charges generally have predetermined rates for diagnostic service codes or discounted FFS rates. The Company perpetually reviews its contractual estimation processes to consider and incorporate updates to laws, regulations, and frequent changes in the managed care system. Contractual terms are negotiated and updated accordingly upon renewal.
F-11
Clinical fees and insurance revenue is based upon the estimated amounts the Company expects to receive from patients and third-party payors. Estimates of explicit price concessions under managed care and commercial insurance plans are tied to payment terms specified in related contractual agreements. Retroactively calculated explicit price concessions tied to reimbursement agreements with third-party payers are recognized on an estimated basis in the period related services are rendered and adjusted in future periods as final payments are received. Revenue related to uninsured patients, uninsured co-payments, and deductibles (for patients with healthcare coverage) may also be discounted. The Company records implicit price concessions (based on historical collection experience) related to uninsured accounts to recognize self-pay revenue at their most likely amounts to be collected.
The Company deems FFS revenue to be variable consideration and its estimates of associated transaction prices will not result in a significant revenue reversal in the future.
The Company has elected the practical expedient not to adjust the transaction price for any financing components as those were deemed to be insignificant and to expense all incremental customer contract acquisition costs as incurred as such costs are not material and would be amortized over a period less than one year.
Other Patient Service Revenue – Shared Risk Revenue
P3 LLC (via one of its wholly owned subsidiaries) receives 30% of the shared risk savings from parties with whom it contracts under four separate arrangements. These arrangements are driven solely by medical cost containment year-over-year (“YoY”) expense reductions. This key performance indicator (“KPI”) is measured by the aggregate change in per member, per year (“PMPY”) medical costs. If the sequential YoY PMPY aggregate change yields a reduction, the Company receives 30% of the associated total cost savings for that year. Conversely, if the sequential YoY PMPY aggregate change yields an increase in medical costs, no monies are due to the Company that year. This KPI is compiled and reviewed on a calendar year basis. The Company recognizes shared risk revenue only upon the receipt of cash.
Other Patient Service Revenue – Care Coordination Fees and Management Fees
The Company’s delegated health plans may also pay a Care Coordination Fee (“CCF”) or management fee to the Company. CCFs and management fees are intended to fund the costs of delegated services provided to certain health plans. CCFs are specifically identified and separated in each monthly capitation payment the Company receives from these parties. None of the Company’s other health plans bifurcate CCFs nor are any of them contractually required to do so. Based on similarities of the terms of the care coordination and administrative services, the Company uses a portfolio approach to record revenue from CCFs and management fees.
Patient Fees Receivable
Substantially all client fees and insurance receivables are due under FFS contracts with third party payors, such as commercial insurance companies, government-sponsored healthcare programs, or directly from patients. The Company has agreements with third-party payors that provide for payments at amounts different from the established rates. Payment arrangements include prospectively determined rates per discharge, reimbursed costs, discounted charges, and per diem payments. Patient fees receivable, where a third-party payor is responsible for the amount due, are recorded at the invoiced amount, net of any expected contractual adjustments and implicit price concessions, and do not bear interest. Contractual adjustments arising under reimbursement arrangements with third-party payors are accrued on an estimated basis in the period the related services are rendered and are adjusted in future periods as final settlements are determined. The Company continuously monitors activities from payors (including patients) and records an implicit price concession based on specific contracts and actual historical collection patterns to reflect the estimated amounts the Company expects to collect. Patient fees receivable of $0.8 million and $0.7 million are included in clinic fees and insurance receivables in the Company’s consolidated balance sheets as of December 31, 2022 and 2021, respectively, and are recorded net of contractual allowances of $5.8 million and $2.0 million as of December 31, 2022 and 2021, respectively.
F-12
Property and Equipment
Property and equipment is carried at acquisition cost, net of accumulated depreciation. Costs for repairs and maintenance of property and equipment, after such property and equipment has been placed in service, are expensed as incurred. Costs and related accumulated depreciation are eliminated when property and equipment is sold or otherwise disposed. Sales and disposals may result in asset-specific gains or losses. Any such gains or losses are included as a component of operations. The Company records depreciation using the straight-line method over the estimated useful lives of the respective assets. The following table summarizes the estimated useful lives of the Company’s property and equipment:
Classification |
| Depreciation Cycle |
Leasehold improvements (cycle: lease term) |
| 1 to 10 Years |
Furniture and fixtures |
| 7 Years |
Computer equipment |
| 3 Years |
Medical equipment |
| 7 Years |
Software |
| 3 Years |
The Company capitalizes certain costs incurred in connection with developing its own proprietary technology to serve core functions of its business operations such as revenue and medical cost analysis, care management and various facets that promote impactful utilization. At December 31, 2022 and 2021, the Company has capitalized $3.5 million and $2.4 million, respectively, to property and equipment for these software costs (specifically to work in progress). In 2022 and 2021, $0.7 million and $2.1 million of capitalized costs were placed into service, respectively. All costs associated with internally developed technology following deployment, or that otherwise do not meet capitalization criteria, are expensed as incurred.
Fair Value Measurements
The Company uses valuation approaches that maximize the use of observable inputs and minimize the use of unobservable inputs to the extent possible. The Company determines fair value based on assumptions that market participants would use in pricing an asset or liability in the principal or most advantageous market. When considering market participant assumptions in fair value measurements, the following fair value hierarchy distinguishes between observable and unobservable inputs, which are categorized in one of the following levels (see Note 6 “Fair Value Measurements and Hierarchy” for further discussion):
Level 1 inputs: Unadjusted quoted prices in active markets for identical assets or liabilities accessible to the reporting entity at the measurement date.
Level 2 inputs: Other than quoted prices included in Level 1 inputs that are observable for the asset or liability, either directly or indirectly, for substantially the full term of the asset or liability.
Level 3 inputs: Unobservable inputs for the asset or liability used to measure fair value to the extent that observable inputs are not available, thereby allowing for situations in which there is little, if any, market activity for the asset or liability at measurement date.
Impairment of Long-Lived Assets
The Company reviews its long-lived assets for impairment whenever events or changes in circumstances indicate their carrying amounts may not be recoverable. Recoverability of an asset or asset group is measured by comparing its carrying amount to the future undiscounted net cash flows the asset or asset group is expected to generate. If such assets are considered impaired (e.g., future undiscounted cash flows are less than net book value), an impairment charge is recognized, measured by the difference between the carrying value and the estimated fair value of the assets. Assets to be disposed of are reported at the lower of the carrying amount or fair value less costs to sell.
F-13
Goodwill
Goodwill represents the excess of the purchase price over the fair value assigned to tangible and identifiable intangible assets acquired and liabilities assumed. Goodwill is tested for impairment at the reporting unit level on an annual basis in the fourth quarter, or more frequently if events or changes in circumstances indicate the carrying value of goodwill may not be recoverable (a “triggering event”). On the occurrence of a triggering event, an entity has the option to first assess qualitative factors to determine whether a quantitative impairment test is necessary. If it is more likely than not that goodwill is impaired, the fair value of the reporting unit is compared with its carrying value. An impairment charge is recognized for the amount by which the carrying amount exceeds the fair value, provided, the loss recognized cannot exceed the total amount of goodwill.
Intangible Assets
Intangible assets with finite useful lives are amortized on a straight-line basis over their estimated useful lives. In determining the estimated useful lives of definite-lived intangibles, the Company considers the nature, competitive position, life cycle position and historical and expected future operating cash flows of each acquired asset, as well as its commitment to support these assets through continued investment and legal infringement protection.
The Company reviews intangible assets for impairment whenever events or changes in circumstances indicate that the related carrying amounts may not be recoverable. Determining whether an impairment loss occurred requires comparing the carrying amount to the sum of undiscounted cash flows expected to be generated by the asset. Such events and circumstances include the occurrence of an adverse change in the market involving the business employing the assets or a situation in which it is more likely than not that the Company will dispose of such assets. If the comparison indicates that there is impairment, the impairment loss to be recognized as a non-cash charge to earnings is measured by the amount by which the carrying amount of the asset exceeds its fair value and the impaired asset is written down to its fair value or, if fair value is not readily determinable, to an estimated fair value based on discounted expected future cash flows.
Leases
The Company determines whether a contract is or contains a lease at the inception of the contract. For leases with terms greater than 12 months, the Company records the related operating or finance right-of-use asset and lease liability at the present value of lease payments over the lease term. The Company is generally not able to readily determine the implicit rate in the lease and therefore uses the determined incremental borrowing rate at lease commencement to compute the present value of lease payments. The incremental borrowing rate represents an estimate of the market interest rate the Company would incur at lease commencement to borrow an amount equal to the lease payments on a collateralized basis over the term of a lease. Renewal options are not included in the measurement of the right-of-use assets and lease liabilities unless the Company is reasonably certain to exercise the optional renewal periods. Some leases also include early termination options, which can be exercised under specific conditions. Additionally, certain leases contain incentives, such as construction allowances from landlords, which reduce the right-of-use asset related to the lease.
Certain of the Company’s leases contain rent escalations over the lease term. The Company recognizes expense for operating leases on a straight-line basis over the lease term. The Company’s lease agreements contain variable payments for common area maintenance and utilities. The Company has elected the practical expedient to combine lease and non-lease components for all asset categories; therefore, the lease payments used to measure the lease liability for these leases include fixed minimum rentals along with fixed non-lease component charges. Variable lease payments are excluded from the measurement of right-of-use assets and lease liabilities and are recognized in the period in which the obligation for those payments is incurred. The Company does not have significant residual value guarantees or restrictive covenants in its lease portfolio.
F-14
Business Combinations
The price tendered in business combinations is allocated using the acquisition method of accounting among the identifiable tangible and intangible assets and assumed liabilities and non-controlling interests, all of which are based on estimates of corresponding fair value as of the acquisition date. The Company applies valuation methods which are ultimately used in the Company’s purchase price allocations. Goodwill is recorded based on the difference between the fair value of consideration exchanged and the fair value of the net assets and liabilities assumed. Such fair values that are not finalized for reporting periods following the acquisition date are estimated and recorded as provisional amounts. Adjustments to these provisional amounts during the measurement period (defined as the date through which all information required to identify and measure the consideration transferred, the assets acquired, the liabilities assumed, and the non-controlling interests obtained, limited to one year from the acquisition date) are recorded when identified.
Equity-Based Compensation
Equity-based compensation cost is measured at the grant date for all equity-based awards based on the fair value of the awards. For equity awards that vest subject to the satisfaction of service-based conditions, compensation cost is recognized on a straight-line basis over the requisite service period, which varies by award. For equity awards that vest subject to the satisfaction of performance-based conditions, the Company evaluates the probability of achieving each performance-based condition at each reporting date and recognizes compensation cost when it is deemed probable that the performance-based condition will be met on an accelerated basis over the requisite service period, which varies by award. Equity-based compensation is classified in the accompanying consolidated statements of operations based on the function to which the related services are provided. The Company accounts for forfeitures as they occur.
P3 LLC used the Black-Scholes option-pricing model to determine the fair value of P3 LLC’s incentive unit awards (“Incentive Units”). The risk-free interest rate estimate was based on constant maturity, which is the theoretical value of a U.S. Treasury that is based on recent values of auctioned U.S. Treasuries with remaining terms similar to the expected term of the incentive unit awards. The expected dividend yield was based on P3 LLC’s expectation of not paying dividends in the foreseeable future. The expected term was calculated primarily based upon the estimated time to a liquidation event. The expected volatility was estimated using company-specific historical information, guideline company information, and implied volatility information.
The Company uses the Black-Sholes option-pricing model to determine the fair value of the Company’s stock option awards. The risk-free interest rate estimate was based on constant maturity, which is the theoretical value of a U.S. Treasury that is based on recent values of auctioned U.S. Treasuries with remaining terms similar to the expected term of the stock option awards. The expected dividend yield was based on the Company’s expectation of not paying dividends in the foreseeable future. The expected term was calculated using the “simplified” method; whereby, the expected term equals the arithmetic average of the vesting term and the original contractual term of the stock option due to P3’s lack of sufficient historical data. The expected volatility was estimated using an average of the historical volatilities of a peer group comprised of publicly traded companies in the same industry. The Company assesses the impact of material nonpublic information on its share price or expected volatility, as applicable, at the time of grant.
Warrant Liability
The Company has public and private placement warrants of Class A common stock classified as liabilities as well as warrants of Class A common stock issued to a lender classified as equity. The Company classifies as equity any equity-linked contracts that (1) require physical settlement or net-share settlement or (2) give the Company a choice of net-cash settlement or settlement in the Company’s own shares (physical settlement or net-share settlement). Warrants classified as equity are initially measured at fair value. Subsequent changes in fair value are not recognized as long as the warrants continue to be classified as equity.
F-15
The Company classifies as assets or liabilities any equity-linked contracts that (1) require net-cash settlement (including a requirement to net-cash settle the contract if an event occurs and if that event is outside the Company’s control) or (2) give the counterparty a choice of net-cash settlement or settlement in shares (physical settlement or net-share settlement). For equity-linked contracts that are classified as liabilities, the Company records the fair value of the equity-linked contracts at each balance sheet date and records the change in the statements of operations as a gain (loss) from change in fair value of warrant liability. The Company’s public warrant liability is valued using observable market prices for those public warrants. The Company’s private placement warrants are valued using a binomial lattice pricing model when the warrants are subject to the make-whole table, or otherwise are valued using a Black-Scholes pricing model. The Company’s warrants issued to a capital provider are valued using a Black-Scholes-Merton pricing model based on observable market prices for public shares and warrants. The assumptions used in preparing these models include estimates such as volatility, contractual terms, discount rates, dividend yield, expiration dates and risk-free rates.
The Company accounts for warrants as either equity-classified or liability-classified instruments based on an assessment of the warrant’s specific terms. The assessment considers whether the warrants are freestanding financial instruments, meet the definition of a liability, and whether the warrants meet all of the requirements for equity classification, including whether the warrants are indexed to the Company’s own ordinary shares, among other conditions for equity classification. This assessment, which requires the use of professional judgment, is conducted at the time of warrant issuance and as of each subsequent quarterly period end date while the warrants are outstanding.
Premium Deficiency Reserve
Premium deficiency reserve (“PDR”) liabilities are established when it is probable that expected future health care costs and maintenance costs under a group of existing contracts will exceed anticipated future premiums and stop-loss insurance recoveries on those contracts. The Company assesses if a PDR liability is needed through review of current results and forecasts. For purposes of determining premium deficiency losses, contracts are grouped consistent with our method of acquiring, servicing, and measuring the profitability of such contracts. The Company grouped its Medicare Advantage health plan contracts together as a single group as it operates in one line of business. The Company further concluded that the costs to administer these contracts are based on centralized and shared service functions. As of December 31, 2022 and 2021, the PDR liability was $26.4 million and $37.8 million, respectively, which represented its estimate of probable contract losses expected to be generated by the Company’s health plans.
Medical Expense and Claims Payable
The cost of healthcare services is recognized in the period services are provided. This also includes an estimate of the cost of services that have been incurred, but not yet reported (“IBNR”). Medical expenses also include costs for overseeing the quality of care and programs, which focus on patient wellness. Additionally, healthcare expenses can include, from time to time, remediation of certain claims that might result from periodic reviews conducted by various regulatory agencies.
Management estimates the Company’s IBNR by applying standard actuarial methodologies, which utilize historical data, including the period between the date services are rendered and the date claims are received (and paid), denied claims activity, expected medical cost inflation, seasonality patterns, and changes in membership mix. IBNR estimates are made on an accrual basis and adjusted in future periods as required. Any adjustments to prior period estimates are included in the current period. Such estimates are subject to the impact from changes in both the regulatory and economic environments.
The Company’s claims payable represents management’s best estimate of its liability for unpaid medical costs as of December 31, 2022 and 2021.
Income Taxes
The Company uses the asset and liability method of accounting for income taxes. Under this method, deferred tax assets and liabilities are determined based on the differences between the financial reporting and the tax bases of assets and liabilities and are measured using the enacted tax rates and laws that will be in effect when the differences are expected to reverse.
F-16
Deferred tax assets are evaluated for future realization and reduced by a valuation allowance to the extent the Company believes it is more likely than not that they will not be realized. The Company considers all available positive and negative evidence, including future reversals of existing taxable temporary differences, projected future taxable income, tax-planning strategies, carryback potential if permitted under tax law, and results of recent operations.
The Company records uncertain tax positions on the basis of a two-step process in which (1) the Company determines whether it is more likely than not that the tax positions will be sustained on the basis of the technical merits of the position and (2) for those tax positions that meet the more-likely-than-not recognition threshold, the Company recognizes the largest amount of tax benefit that is more than 50% likely to be realized upon ultimate settlement with the related tax authority. The Company considers many factors when evaluating its uncertain tax positions during the course of the year through a review of policies and procedures, reviews of customary and regular tax filings, and discussions with third party experts. This review can involve significant judgment and may require periodic adjustments. The resolution of these uncertain tax positions in a manner inconsistent with management’s expectations could have a material impact on the Company’s consolidated financial statements. The Company recognizes interest and penalties related to uncertain tax positions as a component of its provision for income taxes. Accrued interest and penalties are included with the related tax liability.
See Note 13 “Income Taxes” for further information.
Advertising Expense
The Company uses advertising primarily to promote the health plans with which it conducts business as well as its physician clinics throughout the geographic areas it serves. Advertising costs are charged directly to operations as incurred. Advertising expense totaled $4.5 million, $0.3 million, and $1.8 million in the year ended December 31, 2022, the Successor Period of 2021, and the Predecessor Period of 2021, respectively.
Reclassifications
Certain amounts in the consolidated balance sheet as of December 31, 2021 and the consolidated statements of operations and cash flows for the Successor Period of 2021 and Predecessor Period of 2021 have been reclassified to be consistent with the current period presentation. These reclassifications were to (i) present notes receivable, net and right-of-use asset collectively as other long-term assets on the consolidated balance sheet; (ii) separately present accounts payable from accrued expenses and other current liabilities on the consolidated balance sheet; (iii) present depreciation expense and amortization of intangible assets collectively as depreciation and amortization expense on the consolidated statements of operations and cash flows; (iv) present amortization of debt origination fees and amortization of discount from issuance of debt collectively as amortization of original issue discount and debt issuance costs on the consolidated statements of cash flows; and (v) present payment of debt issuance costs separately from debt proceeds on the consolidated statements of cash flows. The reclassifications had no impact on the Company’s financial condition, results of operations, or net cash flows.
Note 4: Recent Accounting Pronouncements
The Company qualifies as an emerging growth company (“EGC”) and as such, has elected the extended transition period for complying with certain new or revised accounting pronouncements. During the extended transition period, the Company is not subject to certain new or revised accounting standards applicable to public companies. The accounting pronouncements pending adoption as described below reflect effective dates for the Company as an EGC with the extended transition period.
F-17
Recently Adopted Accounting Pronouncements
Accounting Standards Update (“ASU”) 2021-10, Government Assistance (Topic 8352), Disclosures by Business Entities about Government Assistance (“ASU 2021-10”)
ASU 2021-10 requires annual disclosures about transactions with a government entity that are accounted for by applying a grant or contribution accounting model including (i) information about the nature of the transactions and the related accounting policy used to account for the transaction; (ii) the line items on the balance sheet and income statement that are affected by the transactions, and the amounts applicable to each financial statement line item; and (iii) significant terms and conditions of the transactions, including commitments and contingencies. ASU 2021-10 is effective for annual periods beginning after December 15, 2021. The Company adopted the ASU prospectively on January 1, 2022. The adoption of this standard did not have a material effect on the Company’s consolidated financial statements and related disclosures.
ASU 2021-04, Earnings Per Share (Topic 260), Debt—Modifications and Extinguishments (Subtopic 470-50), Compensation—Stock Compensation (Topic 718), and Derivatives and Hedging—Contracts in Entity’s Own Equity (Subtopic 815-40), Issuer’s Accounting for Certain Modifications or Exchanges of Freestanding Equity-Classified Written Call Options (“ASU 2021-04”)
ASU 2021-04 requires issuers to account for modifications or exchanges of freestanding equity-classified written call options (e.g., warrants) that remain equity classified after the modification or exchange based on the economic substance of the modification or exchange. The Company adopted ASU 2014-04 in the first quarter of 2022 on a prospective basis. The adoption of this standard did not have a material effect on the Company’s consolidated financial statements and related disclosures.
ASU 2020-10, Codification Improvements (“ASU 2020-10”)
The amendments in ASU 2020-10 improve codification by ensuring that all guidance that includes an option for an entity to provide information in the notes to financial statements is codified within the disclosure section of the codification. The amendments are effective for annual periods beginning after December 15, 2021, and interim periods beginning after December 15, 2022. The Company adopted this guidance retrospectively in the 2022 annual period. The adoption of this guidance did not have a material effect on the Company’s consolidated financial statements.
ASU 2019-12, Income Taxes (Topic 740), Simplifying the Accounting for Income Taxes (“ASU 2019-12”)
ASU 2019-12 eliminates certain exceptions related to the approach for intra-period tax allocation, the methodology for calculating income taxes in an interim period and the recognition of deferred tax liabilities for outside basis differences. It also clarifies and simplifies other aspects of the accounting for income taxes. It is effective for fiscal years beginning after December 15, 2021, and interim periods within fiscal years beginning after December 15, 2022. The Company adopted the ASU in the first quarter of 2022 on a prospective basis. The adoption of this standard did not have a material effect on the Company’s consolidated financial statements and related disclosures
Recent Accounting Pronouncements Not Yet Adopted
ASU 2021-08, Business Combinations (Topic 805): Accounting for Contract Assets and Contract Liabilities from Contracts with Customers (“ASU 2021-08”)
ASU 2021-08 requires that an entity (acquirer) recognize and measure contract assets and contract liabilities acquired in a business combination in accordance with Topic 606. At the acquisition date, an acquirer should account for the related revenue contracts as if it had originated the contracts. The amendments in this update are effective for fiscal years beginning after December 15, 2023. Early adoption is permitted. Upon adoption, the Company will apply this guidance to future business combinations.
F-18
ASU 2020-06, Debt – Debt with Conversion and Other Options (Subtopic 470-20) and Derivatives and Hedging — Contracts in Entity’s Own Equity (Subtopic 815-40), Accounting for Convertible Instruments and Contracts in an Entity’s Own Equity (“ASU 2020-06”)
ASU 2020-06 eliminates two of the three models in ASC 470-20 that require issuers to separately account for embedded conversion features and eliminates some of the requirements for equity classification in ASC 815-40-25 for contracts in an entity’s own equity. The guidance also requires entities to use the if-converted method for all convertible instruments in the diluted earnings per share calculation and generally requires them to include the effect of potential share settlement for instruments that may be settled in cash or shares. It is effective for annual periods beginning after December 15, 2023, and interim periods therein. Early adoption is permitted, but the Company must adopt the guidance as of the beginning of a fiscal year. The Company is evaluating the effect ASU 2020-06 will have on its financial statements and related disclosures.
ASU 2016-13, Financial Instruments – Credit Losses (Topic 326): Measurement of Credit Losses on Financial Instruments (“ASU 2016-13”)
ASU 2016-13 introduces a new model for recognizing credit losses on financial instruments based on an estimate of current expected credit losses. The new current expected credit losses model generally calls for the immediate recognition of all expected credit losses and applies to loans, accounts and trade receivables as well as other financial assets measured at amortized cost, loan commitments and off-balance sheet credit exposures, debt securities and other financial assets measured at fair value through other comprehensive income, and beneficial interests in securitized financial assets. The new guidance replaces the current incurred loss model for measuring expected credit losses, requires expected losses on available for sale debt securities to be recognized through an allowance for credit losses rather than as reductions in the amortized cost of the securities, and provides for additional disclosure requirements. In April 2019, the Financial Accounting Standards Board (“FASB”) issued ASU 2019-04, which, among other amendments, allows for certain policy elections and practical expedients related to accrued interest on financial instruments. In May 2019, the FASB issued ASU 2019-05, which granted targeted transition relief by allowing entities to irrevocably elect the fair value option for certain financial assets previously measured at amortized cost. In November 2019, the FASB issued ASU 2019-10 and ASU 2019-11, which addressed certain aspects of the guidance related to effective dates, expected recoveries, troubled debt restructurings, accrued interest receivables, and financial assets secured by collateral. ASU 2016-13 is effective for fiscal years beginning after December 15, 2022, including interim periods within those fiscal years, and is effective for the Company beginning January 1, 2023. The Company is currently evaluating the impact the adoption of this standard will have on its consolidated financial statements.
Note 5: Business Combinations
P3 Business Combinations
The Business Combinations represented a forward merger and was accounted for using the acquisition method of accounting under which P3 LLC was the acquired company and P3 was the accounting acquirer for financial reporting purposes. This determination is based primarily on the following:
| (i) | P3 is the sole managing member of P3 LLC subsequent to the Closing, and the managing member conducts, directs, and exercises full control over all activities of P3 LLC. The non-managing members of P3 LLC do not have substantive kick-out or participating rights; and |
| (ii) | No one predecessor stakeholder of P3 had a controlling interest in P3 before or has a controlling interest in the combined company after the Business Combinations. The Business Combinations is not a transaction between entities under common control. |
F-19
The following summarizes the purchase price consideration:
Equity |
| $ | 80,301 |
Fair value of redeemable non-controlling interest | 1,807,428 | ||
Stock compensation pre-combination services |
| 26,313 | |
Cash consideration | 18,405 | ||
Payment of P3 LLC’s transaction costs | 19,152 | ||
Total purchase consideration | $ | 1,951,599 |
The Company recorded the allocation of the purchase consideration to the tangible and intangible assets acquired and liabilities assumed based on their estimated fair values as of the Closing Date. The purchase consideration and allocation includes the fair value of assets and liabilities associated with the Company’s acquisitions of three medical practices in the Predecessor Period of 2021 described below.
The aggregate purchase price consideration for the Business Combinations has been allocated as follows at the acquisition date:
Assets acquired: | |||
Cash |
| $ | 5,301 |
Restricted cash | 54 | ||
Health plan receivables | 47,733 | ||
Clinic fees and insurance receivables, net | 426 | ||
Other receivables | 1,881 | ||
Prepaid expenses and other current assets | 939 | ||
Property and equipment | 7,875 | ||
Definite lived intangible assets: | |||
Customer relationships | 684,000 | ||
Provider network | 3,700 | ||
Trademarks | 147,700 | ||
Goodwill | 1,278,453 | ||
Operating lease right-of-use assets(1) | 10,604 | ||
Total assets acquired | 2,188,666 | ||
Liabilities assumed: | |||
Accounts payable and accrued expenses | 25,819 | ||
Accrued payroll | 2,869 | ||
Health plan settlements payable | 25,008 | ||
Claims payable | 76,031 | ||
Premium deficiency reserve | 11,559 | ||
Accrued interest | 9,269 | ||
Current portion of long-term debt | 301 | ||
Operating lease liability | 6,211 | ||
Long-term debt, net of current portion | 80,000 | ||
Total liabilities assumed | 237,067 | ||
Net assets acquired | $ | 1,951,599 |
(1) | Included within other long-term assets on the consolidated balance sheet. |
F-20
Fair value of property and equipment acquired consists of the following at the acquisition date:
Leasehold improvements |
| $ | 1,537 |
Furniture and fixtures |
| 1,081 | |
Computer equipment and software |
| 3,066 | |
Medical equipment |
| 414 | |
Software (development in process) |
| 1,777 | |
Total property and equipment | $ | 7,875 |
Working capital accounts, property and equipment, and notes receivable were measured at the existing carrying values, which approximated fair values. The fair value of long-term debt was measured at face value, which approximated the fair value. The fair value of customer relationships was measured at the acquisition date under the excess earnings method using Level 3 inputs, such as projected cash flows, annual retention rates attributable to the existing relationships, and a selected discount rate. The fair value of the provider network was measured at the acquisition date under the cost approach using Level 3 inputs, such as estimated direct costs, estimates of allocated overhead costs, and an estimated mark-up percentage to apply to such costs. The fair value of trademarks was measured at the acquisition date under the relief-from-royalty method using Level 3 inputs, such as projected cash flows, benchmark royalty rates, and a selected discount rate. Goodwill arising from the acquisition is primarily attributable to the assembled workforce of P3 LLC and expected future market opportunities. Goodwill of $3.8 million recognized in the Business Combinations is expected to be deductible for tax purposes. The useful life of acquired definite lived intangible assets is 10 years.
Other Acquisitions
The Company acquired 100% of the outstanding equity interests of Medcore Health Plan, Inc. (“Medcore HP”) on December 31, 2021 and the net assets of IPA Medical Group, Inc. (“Omni”) on December 27, 2021 (collectively, the “Medcore Acquisition”). Medcore HP is a health plan licensed under the California Knox-Keen Health Care Service Plan Act of 1975 and Omni is an independent practice association located in California. Omni serves as Medcore HP’s contracted and fully delegated physician network providing medical services to Medcore HP’s patients and members. Due to the extensive inter-reliance of these two businesses, the Company accounted for the purchases as a single, combined business. The total purchase price of $40.0 million includes $3.5 million to be paid to the sellers upon resolution of the assumed claims payable and risk adjustment factor, which is considered to be a Level 3 fair value measurement. The change in fair value of the contingent consideration from the acquisition date to December 31, 2022 was not material. Release of this payment, currently expected in the first half of 2023, is not subject to resolution of a substantive future contingent event and has therefore been included in the total consideration to be transferred. The cash payment, net of cash acquired and the amount retained payment of $3.5 million, was $15.7 million.
The Company also purchased three medical practices during the Predecessor Period of 2021 for a total net cash purchase price of $5.0 million. As referenced above, the assets acquired and liabilities assumed in these acquisitions were included in the purchase consideration and allocation for the Business Combinations.
Goodwill arising from the acquisition is primarily attributable to the assembled workforce and expected future market opportunities. Goodwill of $8.1 million recognized in these other acquisitions is expected to be deductible for tax purposes. The useful life of acquired definite lived intangible assets is 10 years.
F-21
The aggregate purchase price consideration of the other acquisitions in 2021 has been allocated as follows at the acquisition dates:
Successor | Predecessor | ||||||
| Period |
|
| Period | |||
Assets acquired: |
|
| |||||
Cash | $ | 20,547 | $ | 3 | |||
Restricted cash |
| 302 |
| — | |||
Health plan receivables |
| 5,754 |
| — | |||
Clinic fees and insurance receivables, net |
| 141 |
| — | |||
Other receivables |
| 726 |
| — | |||
Prepaid expenses and other current assets |
| 1,190 |
| — | |||
Property and equipment |
| 113 |
| 6 | |||
Definite lived intangible assets: |
|
|
| ||||
Customer relationships |
| — |
| 2,046 | |||
Payor contracts | 4,700 | — | |||||
Provider network |
| 1,100 |
| — | |||
Trademarks |
| 900 |
| — | |||
Indefinite lived intangible assets: | |||||||
Medical licenses |
| 700 |
| — | |||
Goodwill |
| 31,298 |
| 2,934 | |||
Total assets acquired | $ | 67,471 | $ | 4,989 | |||
Liabilities assumed: |
|
|
| ||||
Accounts payable |
| 150 |
| — | |||
Accrued payroll |
| 277 |
| — | |||
Health plan settlements payable |
| 133 |
| — | |||
Claims payable |
| 26,898 |
| — | |||
Total liabilities assumed |
| 27,458 |
| — | |||
Net assets acquired | $ | 40,013 | $ | 4,989 | |||
In the third quarter of 2022, the Company acquired two medical practices in separate transactions. The total cash purchase price was $5.5 million, net of cash acquired, and was allocated primarily to goodwill.
Pro Forma Financial Information (Unaudited)
The following unaudited pro forma financial information summarizes the results of operations for the Company as though the Business Combinations and the Medcore Acquisition had occurred on January 1, 2020 and has been derived from the historical consolidated financial statements of the Company’s Predecessor Periods and the Successor Period. The Successor and Predecessor Periods for the year ended December 31, 2021 have been combined. The unaudited pro forma financial information has been presented for illustrative purposes only and is not necessarily indicative of results of operations that would have been achieved had the acquisition taken place on the date indicated, or the future consolidated results of operations of the Company.
| Year Ended | ||
December 31,2021 | |||
(Unaudited) | |||
Total operating revenue | $ | 793,447 | |
Net loss | $ | (259,282) | |
Net loss attributable to non-controlling interest | $ | (214,167) | |
Net loss attributable to controlling interest | $ | (45,115) | |
The unaudited pro forma results reflect the step-up amortization adjustments for the fair value of intangible assets acquired, transaction expenses, accelerated vesting of equity-based compensation, debt discount amortization, and income attributable to non-controlling interest holders.
F-22
Note 6: Fair Value Measurements and Hierarchy
Information about the Company’s financial liabilities measured at fair value on a recurring basis is presented below:
December 31, 2022 | ||||||||||||
| Carrying Value |
| Level 1 |
| Level 2 |
| Level 3 | |||||
Financial liabilities: |
|
|
|
| ||||||||
Liability for private placement warrants | $ | 40 | $ | — | $ | — | $ | 40 | ||||
Liability for public warrants | $ | 1,477 | $ | 1,477 | $ | — | $ | — | ||||
| December 31, 2021 | |||||||||||
Carrying Value | Level 1 | Level 2 | Level 3 | |||||||||
Financial liabilities: |
|
|
|
|
|
|
|
| ||||
Liability for private placement warrants | $ | 502 | $ | — | $ | — | $ | 502 | ||||
Liability for public warrants | $ | 10,881 | $ | 10,881 | $ | — | $ | — | ||||
The key Level 3 inputs into the option pricing model related to the private placement warrants to purchase Class A common stock were as follows:
December 31, | |||||||
| 2022 |
| 2021 | ||||
Volatility |
| 55 | % | 60 | % | ||
Risk-free interest rate |
| 4.11 | % | 1.26 | % | ||
Exercise price | $ | 11.50 | $ | 11.50 | |||
Expected term | 3.9 | Years |
| 4.9 | Years | ||
Generally, an increase in the market price of the Company’s shares of common stock, an increase in the volatility of the Company’s shares of common stock, and an increase in the remaining term of the warrants would each result in a directionally similar change in the estimated fair value of the Company’s warrant liabilities. Such changes would increase the associated liability while decreases in these assumptions would decrease the associated liability. An increase in the risk-free interest rate would result in a decrease in the estimated fair value measurement and thus a decrease in the associated liability. The Company has not, and does not plan to, declare dividends on its common stock and, as such, there is no change in the estimated fair value of the warrant liabilities due to the dividend assumption.
The following table sets forth a summary of changes in the fair value of the Company’s private placement warrants, which are considered to be Level 3 fair value measurements:
| Successor |
|
| Predecessor | ||||||
| Year |
| December 3, 2021 |
|
| |||||
Ended | through | |||||||||
December | December 31, | January 1, 2021 | ||||||||
31, 2022 | 2021 | through | ||||||||
(Private | (Private | December 2, 2021 | ||||||||
Placement | Placement | (Class D | ||||||||
Warrants) | Warrants) | Warrants) | ||||||||
Beginning balance | $ | 502 | $ | 793 | $ | 6,316 | ||||
(462) |
| (291) |
| 7,665 | ||||||
Ending balance | $ | 40 | $ | 502 | $ | 13,981 | ||||
The Company recorded gains on the changes in the fair value of public warrants of $9.4 million and $2.3 million during the year ended December 31, 2022 and the Successor Period of 2021, respectively.
F-23
Note 7: Property and Equipment
The Company’s property and equipment balances consisted of the following:
December 31, | |||||||
2022 |
|
| 2021 | ||||
Leasehold improvements | | $ | 1,810 | $ | 1,537 | ||
Furniture & fixtures |
| 1,262 |
| 1,108 | |||
Computer equipment & software |
| 3,206 |
| 2,701 | |||
Medical equipment |
| 1,067 |
| 414 | |||
Software (development in process) |
| 3,460 |
| 2,433 | |||
Vehicles | 618 | — | |||||
Other | 37 | 37 | |||||
11,460 | 8,230 | ||||||
Less: accumulated depreciation |
| (2,621) |
| (182) | |||
Property and equipment, net | $ | 8,839 | $ | 8,048 | |||
Total depreciation of property and equipment recognized on the consolidated statements of operations was $2.4 million, $0.2 million, and $1.5 million for the year ended December 31, 2022, the Successor Period of 2021, and the Predecessor Period of 2021, respectively.
Note 8: Goodwill
The following table provides a reconciliation of goodwill and accumulated goodwill impairment losses as of:
Balance at December 3, 2021(1) | |||
Goodwill | $ | 1,278,453 | |
Accumulated goodwill impairment losses |
| — | |
1,278,453 | |||
Acquisitions | 31,297 | ||
Balance at December 31, 2021 | |||
Goodwill | 1,309,750 | ||
Accumulated goodwill impairment losses | — | ||
1,309,750 | |||
Acquisitions | 5,202 | ||
Impairment losses | (1,314,952) | ||
Balance at December 31, 2022 | |||
Goodwill | 1,314,952 | ||
Accumulated goodwill impairment losses | (1,314,952) | ||
$ | — |
(1) | Represents the opening balance of goodwill due to the Business Combinations (Note 5) |
F-24
In the second quarter of 2022, the Company identified indicators of impairment related to goodwill due to a significant deterioration in the overall market and a sustained decrease in the price of the Company’s Class A common stock. As a result, the Company performed an interim assessment for impairment as of June 30, 2022 and noted that the Company’s share price (i) was significantly lower than its opening price on December 2, 2021, (ii) had not surpassed its opening price since December 15, 2021, and (iii) had steadily declined through the end of the second quarter of 2022, which did not follow the overall rebound pattern in the healthcare industry. Management concluded that, given the macroeconomic and financial market conditions, industry-specific considerations, the decline in the Company’s performance as a result of higher than expected medical expenses due to the COVID-19 pandemic, and the sustained decrease in share price, it was more likely than not that the Company’s fair value was less than its carrying amount at June 30, 2022. Accordingly, management performed the two-step impairment test by estimating the Company’s fair value using a weighted combination of (i) discounted cash flows, using Level 3 inputs such as revenue, profit margin, and discount rate and (ii) market-based approach, using Level 3 inputs such as comparable companies’ market multiples. Based on management’s comparison of the Company’s weighted estimated fair value to its carrying amount, an $851.5 million goodwill impairment charge was recorded for the three-month period ended June 30, 2022.
In the fourth quarter of 2022, the Company identified indicators of impairment related to goodwill due to the Company’s overall financial performance and a sustained decrease in the price of the Company’s Class A common stock. As a result, the Company performed an assessment for impairment as of December 31, 2022 and noted that the Company’s share price closed at its lowest price in its trading history and had steadily declined through the end of December 2022, which was not consistent or was significantly worse when compared to the performance of its peers and the healthcare industry as a whole. Management concluded that, given the decline in the Company’s performance and the sustained decrease in its share price, it was more likely than not that the Company’s fair value was less than its carrying amount at December 31, 2022. Accordingly, management performed the two-step impairment test by estimating the Company’s fair value using a weighted combination of (i) discounted cash flows, using Level 3 inputs such as revenue, profit margin, and discount rate; and (ii) market-based approach, using Level 3 inputs such as comparable companies’ market multiples. Based on management’s comparison of the Company’s weighted estimated fair value to its carrying amount, a $463.5 million goodwill impairment charge was recorded for the three-month period ended December 31, 2022.
Based on the Company’s qualitative analyses, no goodwill impairment charges were recorded in the Successor Period of 2021 or the Predecessor Period of 2021.
Note 9: Intangible Assets, Net
Intangible assets, net consisted of the following as of:
December 31, | ||||||||||||||||||
2022 | 2021 | |||||||||||||||||
Gross Carrying | Accumulated | Net Carrying | Gross Carrying | Gross Carrying | Net Carrying | |||||||||||||
| Amount |
| Amortization |
| Amount |
| Amount |
| Amount |
| Amount | |||||||
Indefinite lived intangible assets: | ||||||||||||||||||
Medical licenses | $ | 700 | $ | — | $ | 700 | $ | 700 | $ | — | $ | 700 | ||||||
Definite lived intangible assets: |
|
|
|
|
|
| ||||||||||||
Customer relationships | 684,000 | (74,100) | 609,900 | 684,000 | (5,700) | 678,300 | ||||||||||||
Trademarks | 148,635 | (16,704) | 131,931 | 148,600 | (1,230) | 147,370 | ||||||||||||
Payor contracts | 4,700 | (470) | 4,230 | 4,700 | — | 4,700 | ||||||||||||
Provider network | 4,800 | (511) | 4,289 | 4,800 | (31) | 4,769 | ||||||||||||
Total | $ | 842,835 | $ | (91,785) | $ | 751,050 | $ | 842,800 | $ | (6,961) | $ | 835,839 | ||||||
Amortization of intangible assets was $84.8 million and $7.0 million during the year ended December 31, 2022, and Successor Period of 2021, respectively. Estimated future amortization of intangible assets is $84.6 million for the year 2023 and $84.2 of the years 2024 through 2027.
F-25
Note 10: Notes Receivable, Net
The Company has entered into Promissory Notes (the “Notes”) with certain family medical practices (each a “Practice”) to fund their working capital needs. The Company simultaneously entered into separate Provider Agreements with each Practice. Each Provider Agreement establishes a preferred, predetermined reimbursement rate for services rendered to the Company’s members and requires that Practice to furnish healthcare services to the Company’s members for the term of the related Notes. As long as the Provider Agreement is in effect on the maturity date of the related Note and has not been terminated by the Practice for any reason, or the Company terminates the Provider Agreement prior to maturity without cause, the Company will forgive the entire principal, plus accrued interest, on the maturity date. Upon early termination of the Provider Agreement by the Practice, all principal and accrued interest will become immediately payable and due to the Company. Due to the probable likelihood of forgiveness at maturity, the Company records a valuation allowance on a straight-line basis following the early termination date through the maturity date, with a full valuation allowance recorded at the maturity date.
As of December 31, 2022 and 2021, the Company has recorded notes receivable of $3.5 million and $3.6 million, respectively, accrued interest receivable of $1.0 million and $0.9 million, respectively, and net of valuation allowances of $0.7 million and $0.5 million, respectively, within other long-term assets on the consolidated balance sheets. As of December 31, 2022, the Notes have maturity dates ranging from March 31, 2025 through December 31, 2028 with interest rates ranging from 5.0% to 10.0%. During the Successor Period of 2021, the Company forgave notes receivable on their maturity date of December 31, 2021 comprised of principal and interest of $0.3 million and $0.1 million, respectively, both of which were fully reserved.
Note 11: Claims Payable
Claims payable includes claims reported as of the end of the reporting period, including estimates for IBNR, due to third parties for health care services provided to members. Activity in the liability for claims payable and healthcare expenses was as follows:
December 31, | ||||||
| 2022 |
| 2021 | |||
Claims unpaid, beginning of period | $ | 101,958 | $ | 76,031 | ||
Incurred, related to: | ||||||
Current period |
| 942,570 | 55,149 | |||
Prior period(s) |
| 882 | 174 | |||
Total incurred |
| 943,452 | 55,323 | |||
Paid, related to: |
|
| ||||
Current period |
| 794,026 | 53,366 | |||
Prior period(s) |
| 100,177 | 2,928 | |||
Total paid |
| 894,203 | 56,294 | |||
Claims unpaid assumed in acquisitions | — | 26,898 | ||||
Claims unpaid, end of period | $ | 151,207 | $ | 101,958 | ||
Estimates for incurred claims are based on historical enrollment and cost trends while also taking into consideration operational changes. Future and actual results typically differ from estimates. Differences could result from an overall change in medical expenses per member, changes in member mix or simply due to the addition of new members.
F-26
Note 12: Debt
Long-Term Debt
Long-term debt consists of the following:
December 31, | ||||||
| 2022 |
| 2021 | |||
Repurchase Promissory Note | $ | 15,000 | $ | 15,000 | ||
Term Loan Facility |
| 65,000 |
| 65,000 | ||
Unsecured Promissory Note |
| 15,000 |
| — | ||
Other |
| — |
| 46 | ||
Long-term debt, gross |
| 95,000 |
| 80,046 | ||
Less: unamortized debt issuance costs and original issue discount |
| (579) |
| — | ||
| 94,421 |
| 80,046 | |||
Less: current portion of long-term debt |
| — |
| (46) | ||
Long-term debt, net | $ | 94,421 | $ | 80,000 | ||
Repurchase Promissory Note
In June 2019, the Company issued a share repurchase promissory note (the “Repurchase Promissory Note”) to a former equity investor for $15.0 million, which was subsequently amended in November 2020. The amended agreement stipulated that the Repurchase Promissory Note would automatically mature and be due and payable on the earlier of June 30, 2026, a change in control transaction, or an underwritten primary public offering, each as defined in the agreement. The note accrues paid in-kind (“PIK”) interest of 11.0% per year. The principal balance, accrued interest, and an exit fee of $0.6 million are due at maturity. Accrued interest was $9.0 million and $6.5 million at December 31, 2022 and 2021, respectively.
Term Loan Facility
In November 2020, the Company entered into a Term Loan Agreement and Security Agreement with a commercial lender (as amended, the “Term Loan Agreement”), which provided funding up to $100.0 million (the “Term Loan Facility”), of which $65.0 million was drawn as of December 31, 2022 and 2021. The Company’s access to additional borrowings under the Term Loan Facility ended upon termination of the commitment period on February 28, 2022. The Term Loan Agreement was amended on November 16, 2021 to provide for certain modifications and to obtain consent from the lenders to consummate the Business Combinations. At Closing, the balance of unamortized debt issuance costs and original issue discount related to the Term Loan Facility was written off and the debt was recorded at face value, which approximated fair value. The Term Loan Agreement was amended on December 21, 2021 to provide for certain modifications and to permit the consummation of the Medcore Acquisition and related transactions. The Term Loan Agreement was amended on December 13, 2022 to provide for certain modifications and to permit the issuance of the Unsecured Promissory Note (as defined below) and related transactions. The Security Agreement provides the lenders collateral in 100% of the Company’s pledged stock, its subsidiaries (including tangible and intangible personal property), and bank accounts.
The principal balance is due in full on the maturity date, which is December 31, 2025. This maturity date may be accelerated as a remedy under certain default provisions in the agreement or in the event a mandatory prepayment trigger occurs. Interest is payable at 12.0% per annum on a quarterly cycle (in arrears) beginning March 31, 2021. The Company has elected to pay interest of 8.0% per annum in cash with the remaining 4.0% per annum being added to principal as PIK interest for a period of three years (or 12 payments). The PIK is subject to acceleration in the event certain occurrences in the Term Loan Facility’s agreement are triggered. Accrued interest was $5.0 million and $2.3 million at December 31, 2022 and 2021, respectively.
The Term Loan Facility includes certain restrictive covenants, including restrictions on the payment of cash dividends. The Company must remain in compliance with financial covenants such as minimum liquidity of $5.0 million and annual minimum revenue levels. On an annual basis, the Company must post a minimum amount of annual revenue equal to or greater than $460.0 million in 2022, $525.0 million in 2023, $585.0 million in 2024, and $650.0 million in 2025. The Company is also subject to certain restrictions that include indebtedness and liens.
F-27
As of December 31, 2022, the Company was not in compliance with its Term Loan Facility covenants related to issuance of the 2022 financial statements with an audit opinion free of a “going concern” qualification. The Term Loan Facility lenders granted a waiver of the covenant under the Term Loan Facility related to the existence of a “going concern” qualification in the audit opinion for our audited financial statements for the fiscal year ended December 31, 2022. The Company was in compliance with all other covenants under the Term Loan Facility as of December 31, 2022; however, there can be no assurance that the Company will be able to maintain compliance with these covenants in the future or that the lenders under the Term Loan Facility or the lenders of any future indebtedness the Company may incur will grant any such waiver or forbearance in the future.
Unsecured Promissory Note
In December 2022, the Company entered into a related party financing transaction (see Note 22 “Related Parties”) with VBC Growth SPV LLC (“VGS”) which included an unsecured promissory note (the “Unsecured Promissory Note”); warrant agreement, pursuant to which the Company issued warrants to purchase 429,180 shares of Class A common stock at an exercise price of $4.26 per share to VGS (see Note 24 “Warrants”); and a subordination agreement (the “Subordination Agreement”), pursuant to which VGS agreed to subordinate its right of payment under the Unsecured Promissory Note to the right of payment and security interests of the lenders under the Term Loan Facility. The Unsecured Promissory Note provides for funding of up to $40.0 million, available for draw by the Company in three tranches as follows: (i) a first tranche of $15.0 million available on December 13, 2022, (ii) a second tranche of up to $15.0 million in a single draw at the Company’s option after January 5, 2023, and (iii) a third tranche of up to $10.0 million available at the Company’s option in a single draw after January 5, 2023 and on or prior to February 3, 2023. The Company will pay VGS an up-front fee of 1.5% at the time of each draw. As of December 31, 2022, $15.0 million had been drawn on the Unsecured Promissory Note and the Company had recorded original issue discount of $0.2 million and debt issuance costs comprising the fair value of the warrants issued to VGS and other costs incurred related to this financing totaling $0.9 million, of which $0.6 million is deferred as other long-term assets until the subsequent tranches are drawn.
The Unsecured Promissory Note matures on May 19, 2026. Interest is payable at 14.0% per annum on a quarterly cycle (in arrears) beginning March 31, 2023. The Company may elect to pay interest 6.0% in kind and 8.0% in cash, but if the terms of the Subordination Agreement do not permit the Company to pay interest in cash, interest will be paid entirely in-kind. Accrued interest was $0.1 million at December 31, 2022.
The Company will pay VGS a back-end fee at the time the Unsecured Promissory Note is paid as follows: (i) if paid from March 1, 2023 through June 30, 2023, 4.5%; (ii) if paid from July 1, 2023 through December 31, 2023, 6.75%; and (iii) if paid on January 1, 2024 or later, 9.0%. The Unsecured Promissory Note may be prepaid, at the Company’s option, either in whole or in part, without penalty or premium, at any time and from time to time, subject to the payment of the back-end fee; provided that prepayments must be in increments of at least $2.0 million.
The Unsecured Promissory Note restricts the Company’s ability and the ability of its subsidiaries to, among other things, incur indebtedness and liens, and make investments and restricted payments. The maturity date may be accelerated as a remedy under the certain default provisions in the agreement, or in the event a mandatory prepayment event occurs.
As of December 31, 2022, long-term debt maturities are as follows:
2023 |
| $ | — |
2024 |
| — | |
2025 |
| 65,000 | |
2026 |
| 30,000 | |
95,000 | |||
Less: unamortized debt issuance costs and original issue discount | (579) | ||
$ | 94,421 |
Short-Term Debt
In 2021, the Company entered into short term financing agreements totaling $3.7 million for the funding of certain insurance policies. The terms of the agreements ranged from to 10 months and the weighted average annual interest rate was 2.6%. The debt was repaid during the third quarter of 2022.
F-28
Note 13: Income Taxes
As a result of the Business Combinations, substantially all of the Company’s assets and operations are held and conducted by P3 LLC and its subsidiaries, and the Company’s only assets are equity interests in P3 LLC. P3 LLC is treated as a partnership for U.S. federal and most applicable state and local income tax jurisdictions. As a partnership, P3 LLC is generally not subject to U.S. federal, state, and local income taxes. Any taxable income or loss generated by P3 LLC is passed through to and included within the taxable income or loss of its members in accordance with the terms of the P3 LLC operating agreement. Prior to the Business Combinations, the income and losses of P3 LLC were passed through to its members and nontaxable to P3 LLC.
The Company is taxed as a corporation and pays corporate federal, state, and local taxes on income allocated to it from P3 LLC based on the Company’s economic interest held in P3 LLC. While the Company consolidates P3 LLC for financial purposes as a VIE, the Company will not be taxed on the earnings attributed to the non-controlling interests. As a result, the income tax burden on the earnings taxed on the non-controlling interests is not reported by the Company in its consolidated financial statements.
The components of loss before income taxes were as follows:
| Successor |
|
| Predecessor | ||||||
Year Ended | December 3, 2021 | January 1, 2021 | ||||||||
December 31, | through December 31, | through December 2, | ||||||||
2022 |
| 2021 | 2021 | |||||||
Domestic | $ | (1,559,695) | $ | (57,938) | $ | (146,400) | ||||
Foreign |
| — |
| — |
| — | ||||
Total | $ | (1,559,695) | $ | (57,938) | $ | (146,400) | ||||
The components of income tax expense were as follows:
Successor | Predecessor | |||||||||
Year Ended | December 3, 2021 | January 1, 2021 | ||||||||
| December 31, |
| through December 31, | through December 2, | ||||||
| 2022 |
| 2021 |
|
| 2021 | ||||
Current income taxes: | ||||||||||
Federal | $ | 111 | $ | — | $ | — | ||||
State | 1,751 | — | — | |||||||
Total current income taxes | $ | 1,862 | $ | — | $ | — | ||||
Deferred income taxes: | ||||||||||
Federal | — | — | — | |||||||
State | — | — | — | |||||||
Total deferred income taxes | — | — | — | |||||||
Total income tax expense | $ | 1,862 | $ | — | $ | — | ||||
F-29
A reconciliation of the statutory federal income tax to the Company’s provision for income taxes is as follows:
| Successor | Predecessor | |||||||||
Year Ended | December 3, 2021 | January 1, 2021 | |||||||||
December 31, | through December 31, | through December 2, | |||||||||
2022 |
| 2021 |
|
| 2021 | ||||||
Tax at federal statutory rate | $ | (327,536) | $ | (12,166) | $ | (30,744) | |||||
Non-controlling interest and nontaxable income |
| 260,020 |
| 8,359 |
| 30,744 | |||||
Change in valuation allowance |
| 33,961 |
| 2,832 |
| — | |||||
Investment in P3 LLC |
| 35,147 |
| 1,550 |
| — | |||||
Other reconciling items | 270 | (575) | — | ||||||||
Total | $ | 1,862 | $ | — | $ | — | |||||
Effective tax rate |
| (0.1) | % |
| — | % |
| — | % | ||
The Company’s tax rate is affected primarily by the recognition of a valuation allowance and the portion of income and expense allocated to the non-controlling interest. It is also affected by discrete items that may occur in any given year such as benefits from changes in the fair value of private placement and public warrants.
Deferred Income Taxes
Deferred income taxes result from differences in the recognition of amounts for tax and financial reporting purposes, as well as operating loss and tax credit carryforwards. Significant components of the Company’s deferred income tax assets and liabilities are as follows:
December 31, | ||||||
2022 |
| 2021 | ||||
Deferred tax assets: |
|
|
|
| ||
Investment in P3 LLC | $ | 20,684 | $ | — | ||
Net operating loss carryforwards |
| 17,601 |
| 6,922 | ||
Accrued liabilities | 2,764 | 3,307 | ||||
Goodwill and identifiable intangible assets | 589 | — | ||||
Section 163j interest limitation |
| 1,995 |
| 1,232 | ||
Other deferred tax assets |
| 94 |
| 3 | ||
Total deferred tax assets |
| 43,727 |
| 11,464 | ||
Less: valuation allowance |
| (43,558) |
| (9,621) | ||
Net deferred tax assets |
| 169 |
| 1,843 | ||
Deferred tax liabilities: |
|
|
| |||
Other deferred tax liabilities | (150) | (87) | ||||
Operating lease, right-of-use assets | (19) | — | ||||
Goodwill and identifiable intangible assets |
| — |
| (1,756) | ||
Total deferred tax liabilities |
| (169) |
| (1,843) | ||
Net deferred tax asset | $ | — | $ | — | ||
The Company recognizes deferred tax assets to the extent it believes that these assets are more likely than not to be realized. The realization of tax benefits of net deferred tax assets is dependent upon future levels of taxable income, of an appropriate character, in the periods the items are expected to be deductible or taxable. Based on the available evidence as of December 31, 2022, the Company believes that it is more likely than not that the tax benefits of the U.S. losses incurred will not be realized. Accordingly, the Company has recorded a valuation allowance against the tax benefits of the U.S. losses incurred. The Company intends to maintain the valuation allowance on the U.S. net deferred tax assets until sufficient positive evidence exists to support a reversal of, or decrease in, the valuation allowance.
F-30
The Company has recognized no deferred taxes in connection with the Medcore Acquisition. Because Medcore HP does not file a consolidated corporate income tax return with the Company, the deferred tax assets of Medcore HP are separately assessed for realizability. Based on the weight of all available evidence, including cumulative losses in recent years, the Company believes that it is more likely than not that the tax benefits of the deferred tax assets will not be realized. Accordingly, the Company has recorded a valuation allowance against the tax benefits of the acquired deferred tax assets.
The Company has recognized no deferred taxes in connection with the Network VIEs. Because the Network VIEs do not file a consolidated corporate income tax return with the Company, the deferred tax assets are separately assessed for realizability. Based on the weight of all available evidence as of December 31, 2022, including cumulative losses in recent years, the Company believes that it is more likely than not that the tax benefits of the deferred tax assets will not be realized. Accordingly, the Company has recorded a valuation allowance against the tax benefits of the related deferred tax assets.
The Company has not recognized a deferred tax liability in connection with its investment in P3 LLC due to the deferred tax liability recognition exception in circumstances where book goodwill exceeds tax-deductible of goodwill.
As of December 31, 2022, the Company had net operating loss carryforwards of approximately $31.4 million for federal income tax purposes. Federal net operating losses have an unlimited carryforward period but utilization for a given tax year is limited to 80% of taxable income.
The federal and state net operating loss carryforwards may be subject to limitations under Section 382 and Section 383 of the Internal Revenue Code of 1986 (the “Code”) and similar provisions under state law. The Tax Reform Act of 1986 contains provisions that limit the federal net operating loss carryforwards that may be used in any given year in the event of special occurrences, including significant ownership changes. The Company has yet to complete a Section 382 review to determine if its tax attributes will be limited in the future; however, the Company’s federal operating loss carryforwards have an unlimited carryforward life and therefore do not expire.
The Company will file income tax returns in the U.S. federal jurisdiction and various state jurisdictions. Generally, federal and state tax authorities provide that the statutes of limitations remain open for three or four years from the tax year in which net operating losses or tax credits are utilized.
On March 11, 2021, the American Rescue Plan Act of 2021 (“American Rescue Plan Act”) was passed into law and amended portions of relevant tax laws. The American Rescue Plan Act did not have a significant impact on the provision for income taxes for the year ended December 31, 2021.
Tax Receivable Agreement
In connection with the Business Combinations, the Company entered into a TRA that provides for the payment by the Company of 85% of the amount of any tax benefits that are realized, or in some cases are deemed to realize, as a result of (i) increases in the Company’s share of the tax basis in the net assets of P3 LLC resulting from any redemptions or exchanges of P3 LLC, (ii) tax basis increases attributable to payments made under the TRA, and (iii) deductions attributable to imputed interest pursuant to the TRA (the “TRA Payments”). The Company expects to benefit from the remaining 15% of any tax benefits that are realized.
Pursuant to the Company’s election under Section 754 of the Code, the Company expects to obtain an increase in its share of the tax basis in the net assets of P3 LLC when Common Units are redeemed or exchanged. The Company intends to treat any redemptions and exchanges of Common Units as direct purchases of the units for U.S. federal income tax purposes. These increases in tax basis may reduce the amounts that the Company would otherwise pay in the future to various tax authorities. They may also decrease gains (or increase losses) on future dispositions of certain capital assets to the extent the tax basis is allocated to those capital assets.
The estimation of liability under the TRA is, by its nature, imprecise and subject to significant assumptions regarding a number of factors, including the timing and amount of taxable income generated by the Company each year, as well as the tax rate then applicable, among other factors. Actual tax benefits realized by the Company may differ from tax benefits calculated under the TRA as a result of the use of certain assumptions in the TRA, including the use of an assumed weighted-average state and local income tax rate to calculate tax benefits.
F-31
The payment obligation under the TRA is an obligation of the Company and not of P3 LLC. The payments that the Company will be required to make will generally reduce the amount of the overall cash flow that might have otherwise been available, but the Company expects the cash tax savings realized from the utilization of the related tax benefits will exceed the amount of any required payments.
As of December 31, 2022 and 2021, the TRA liability is estimated to be $4.6 million; however, due to the full valuation allowance recorded by the Company, which results in no tax benefits that are to be realized related to the amortization of the step-up, the Company determined that payments to TRA holders are not probable and no TRA liability has been recorded as of December 31, 2022 and 2021. As non-controlling interest holders exercise their right to exchange their Common Units, a TRA liability may be recorded based on 85% of the estimated future tax benefits that the Company may realize as a result of increases in its tax basis of P3 LLC. The amount of the increase in the tax basis, the related estimated tax benefits, and the related TRA liability to be recorded will depend on the price of a share of the Company’s Class A common stock at the time of the relevant redemption or exchange.
Note 14: Capitalization
As of December 31, 2022, under the Company’s amended and restated certificate of incorporation dated August 20, 2020, the Company is authorized to issue: (i) 800,000,000 shares of Class A common stock with a par value of $0.0001 per share, (ii) 205,000,000 shares of Class V common stock with a par value of $0.0001 per share, and (iii) 10,000,000 shares of preferred stock with a par value of $0.0001 per share, of which no shares were issued or as of December 31, 2022 and 2021. Holders of shares of Class A common stock and Class V common stock are each entitled to one on all matters to be voted upon by stockholders. The declaration, amount, and payment of any future dividends on shares of Class A common stock will be at the discretion of the Company’s Board of Directors and will depend upon many factors, including the Company’s results of operations, financial condition, capital requirements, restrictions in its debt agreements, and other factors that the Company’s Board of Directors deems relevant. Holders of shares of Class A common stock are entitled to receive such dividends declared by the Company’s Board of Directors. Holders of shares of Class V common stock are not entitled to participate in any such dividends declared by the Company’s Board of Directors. The Company’s Board of Directors has not declared any cash dividends during the year ended December 31, 2022, the Successor Period of 2021, or the Predecessor Period of 2021.
Note 15: Equity-Based Compensation
Predecessor Awards
In 2017, the Predecessor Company adopted the Management Incentive Plan (the “Predecessor Equity Plan”). Under the Predecessor Equity Plan, the Predecessor Company granted awards in the form of profits interests to employees, officers, and directors or in the form of common equity to founders. The Predecessor Equity Plan was administered by the Predecessor Company’s board of managers which had full power and authority to select the participants to whom awards were granted, to make any combination of awards to participants, to accelerate the exercisability or vesting of any award, and to determine the specific terms and conditions of each award, subject to the provisions of the Predecessor Equity Plan. Following the Business Combinations, the Predecessor Equity Plan was terminated.
Under the Predecessor Equity Plan, 6,845,297 Class C units were authorized and 5,235,833 were issued to non-employee directors and officers as of December 2, 2021. Time-based Class C units generally vested over a period of to five years. The Class C units were equity-classified awards. Vesting of performance-based Class C units was based on the Predecessor Company’s achievement of specified performance hurdles established by the Predecessor Company’s board of managers, such as the achievement of specified returns (the range of which varied on an individual award-by-award basis), a change of control, or an initial public offering. Since such a qualifying event was not probable of occurring until it was consummated, the Predecessor Company did not recognize any compensation cost related to performance-based Class C units until the Business Combinations were completed.
On the Closing Date, each Incentive Unit that was outstanding immediately prior to the effective time of the Business Combinations and vested (after taking into account any accelerated vesting that occurred in connection with the Business Combinations) was canceled and converted into the right to receive a portion of the merger consideration, which consisted of Common Units and cash.
F-32
Additionally, the vesting of Incentive Units totaling 4,319,964 held by two executive officers was accelerated such that all of the merger consideration received by these executive officers was not subject to any vesting restrictions, which resulted in an acceleration of equity-based compensation cost of $2.4 million recognized by the Predecessor Company.
Certain of the performance-based Incentive Units issued to directors, executive officers, and employees vested on the Closing Date to the extent the applicable performance hurdles were achieved, and were converted into the right to receive a portion of the merger consideration. To the extent not vested on the Closing Date, each unvested performance-based Incentive Unit was forfeited without consideration. Each Common Unit received as merger consideration was paired with a share of Class V common stock issued in the Successor Company. The acquisition date fair value of the unvested profits interests attributable to post-combination services was $24.0 million which will be expensed over the relevant vesting period by the Successor Company. The acquisition date fair value of the unvested profits interest attributable to pre-combination services was $26.3 million and was included in consideration transferred in connection with the Business Combinations.
Successor Awards
In connection with the Closing, unvested Incentive Units granted under the Predecessor Equity Plan totaling 587,500 were converted into 5,471,400 Common Units, which were paired with an equal number of shares of the Company’s Class V common stock, and remained subject to the original vesting conditions. If a forfeiture of unvested Common Units occurs, the associated shares of Class V common stock are also forfeited.
The following summarizes Common Unit award activity for the year ended December 31, 2022:
Weighted |
| ||||
| Average |
| Number of | ||
Grant-Date | Units | ||||
Fair Value | (in thousands) | ||||
Non-vested at December 31, 2021 | $ | 9.20 |
| 5,471 | |
Granted |
| — |
| — | |
Vested |
| 9.20 |
| (5,038) | |
Forfeited |
| 9.20 |
| (53) | |
Non-vested at December 31, 2022 | $ | 9.20 |
| 380 | |
Total fair value of Common Unit awards vested during the year ended December 31, 2022 was $17.6 million. There were no Common Unit awards vested during the Successor Period of 2021. The weighted-average grant date fair value for Common Unit awards granted during the Successor Period of 2021 was $9.20 per award.
The Common Unit awards vest ratably over a period between one month and two years, so long as the grantee stays employed. As of December 31, 2022, there was $1.1 million of unrecognized equity-based compensation cost related to all unvested Common Unit awards, which is expected to be recognized over a weighted-average period of 0.95 years.
In connection with the Business Combinations, the Company’s Board of Directors adopted, and its stockholders approved, the 2021 Incentive Award Plan (the “2021 Plan”), effective on its adoption date, in order to facilitate the grant of cash and equity incentives to employees, consultants, and directors of the Company and certain affiliates. The 2021 Plan provides that the initial aggregate number of shares reserved and available for issuance is 14.6 million plus an increase each January 1, beginning on January 1, 2022 and ending on and including January 1, 2031, equal to the lesser of (i) 1% of the aggregate number of shares of Class A common stock and Class V common stock outstanding on the final day of the immediately preceding quarter and (ii) such smaller number of shares of Class A common stock as is determined by the Company’s Board of Directors.
F-33
The 2021 Plan allows for the grant of (i) stock options, including incentive stock options, (ii) stock appreciation rights, (iii) restricted stock awards, (iv) restricted stock unit awards, or (v) other stock or cash based awards as may be determined by the plan’s administrator from time to time. The term of each option award shall be no more than 10 years from the date of grant. Options exercised under the 2021 Plan provide the purchaser with full rights equivalent to those of existing Class A common stockholders and holders as of the date of exercise. The Company’s policy for issuing shares upon stock option exercise is to issue new shares of Class A common stock. Additionally, the P3 LLC operating agreement states that P3 LLC will maintain at all times a one-to-one ratio between the number of Common Units owned by the Company and the number of outstanding shares of Class A common stock, including those issued as result of stock option exercises and vesting of restricted stock unit awards.
The 2021 Plan also provides for dividend equivalent units based on the value of the dividends per share paid on the Company’s Class A common stock, which are accumulated on restricted stock units during the vesting period.
The following table summarizes time-based stock option activity for the year ended December 31, 2022:
|
|
| Weighted |
| ||||||
Average | ||||||||||
Weighted | Remaining | Aggregate | ||||||||
Number of | Average | Contractual | Intrinsic | |||||||
Stock Options | Exercise | Life | Value | |||||||
(in thousands) | Price | (in years) | (in thousands) | |||||||
Outstanding at December 31, 2021 |
| — | $ | — |
|
|
|
| ||
Granted |
| 3,589 |
| 5.57 |
|
|
|
| ||
Forfeited |
| (187) |
| 5.02 |
|
|
|
| ||
Outstanding at December 31, 2022 |
| 3,402 | $ | 5.60 |
| 9.62 | $ | — | ||
Fully vested and expected to vest at December 31, 2022 |
| 3,402 | $ | 5.60 |
| 9.62 | $ | — | ||
Exercisable at December 31, 2022 |
| 117 | $ | 5.02 |
| 9.22 | $ | — | ||
The following table summarizes performance-based stock option activity for the year ended December 31, 2022:
|
|
| Weighted |
| ||||||
Average | ||||||||||
Weighted | Remaining | Aggregate | ||||||||
Number of | Average | Contractual | Intrinsic | |||||||
Stock Options | Exercise | Life | Value | |||||||
(in thousands) | Price | (in years) | (in thousands) | |||||||
Outstanding at December 31, 2021 |
| — | $ | — |
|
|
|
| ||
Granted |
| 1,500 |
| 4.95 |
|
|
|
| ||
Outstanding at December 31, 2022 |
| 1,500 | $ | 4.95 |
| 9.83 | $ | — | ||
Fully vested and expected to vest at December 31, 2022 |
| 1,500 | $ | 4.95 |
| 9.83 | $ | — | ||
Exercisable at December 31, 2022 |
| — | $ | — |
| — | $ | — | ||
The vesting criteria for 0.1 million performance-based stock option awards has not yet been achieved; therefore, no expense has been recorded.
There were no stock options granted, , or during the Successor Period of 2021.
The weighted average assumptions used in estimating the grant date fair value of stock options are listed in the table below:
| Year Ended |
| |
December 31, |
| ||
2022 |
| ||
Expected volatility |
| 51 | % |
Risk-free interest rate |
| 3.2 | % |
Expected term (in years) |
| 7.28 | |
Dividend rate |
| 0.0 | % |
F-34
Time-based stock options vest ratably over a period between and five years, so long as the optionee continues to provide services to the Company. As of December 31, 2022, there was $7.2 million and $5.3 million of unrecognized equity-based compensation cost related to time-based and performance-based stock options, respectively, which is expected to be recognized over a weighted-average period of 3.66 years and 9.83 years, respectively.
Compensation Expense
Equity-based compensation recorded within corporate, general and administrative expense on the consolidated statements of operations was $19.4 million, $4.6 million, and $3.5 million during the year ended December 31, 2022, the Successor Period of 2021, and the Predecessor Period of 2021, respectively.
The Company did not recognize any tax benefits related to equity-based compensation for the year ended December 31, 2022, Period of 2021, and the Period of 2021.
Note 16: Loss per Share
The following table provides the computation of basic and diluted net loss per share:
Year Ended | December 3, 2021 | |||||
December 31, | through December 31, | |||||
| 2022 |
| 2021 | |||
Net loss attributable to Class A common stockholders-basic and diluted | $ | (270,127) | $ | (10,081) | ||
| | |||||
Weighted average Class A common shares outstanding-basic and diluted | 41,579 | | | 41,579 | ||
| | | ||||
Loss per share attributable to Class A common stockholders-basic and diluted | $ | (6.50) | | $ | (0.24) | |
Shares of Class V common stock do not share in the earnings or losses of P3 Health Partners, Inc. and are therefore not participating securities. As such, separate presentation of basic and diluted net income per share for Class V common stock under the two-class method is not required. The following table presents potentially dilutive securities excluded from the computation of diluted net loss per share for the periods presented because their effect would have been anti-dilutive.
Year Ended | December 3, 2021 | |||||
December 31, | through December 31, | |||||
| 2022 |
| 2021 | |||
Stock warrants(1) | 11,248 | 10,819 | ||||
Stock options(1) | 3,402 | — | ||||
Shares of Class V common stock(2) | 201,972 | 202,025 | ||||
Total | 216,622 | 212,844 | ||||
| (1) | Represents the number of instruments outstanding at the end of the period. Application of the treasury stock method would reduce this amount if they had a dilutive effect and were included in the computation of diluted net loss per share |
| (2) | Shares of Class V common stock at the end of the period, including shares tied to unvested Common Units, are considered potentially dilutive shares of Class A common stock under application of the if-converted method. |
Note 17: Leases
The Company leases real estate, in the form of corporate office space and operating facilities, and certain office equipment. The Company’s real estate leases have noncancelable terms expiring in 2023 to 2032, certain of which have one to two renewal options of to 10 years. The Company’s equipment leases have noncancelable terms expiring in 2025 to 2027.
Operating lease right-of-use assets of $11.7 million and $7.0 million were included within other long-term assets on the Company’s consolidated balance sheets as of December 31, 2022 and 2021, respectively.
F-35
Operating lease costs are included within operating expenses on the consolidated statements of operations and were $3.1 million, $0.3 million, and $2.3 million for the year ended December 31, 2022, the Successor Period of 2021, and the Predecessor Period of 2021, respectively.
Lease terms and discount rates consisted of the following as of:
December 31, | |||||
| 2022 |
| 2021 |
| |
Weighted average remaining lease term (years) |
| 6.22 | 5.01 |
| |
Weighted average discount rate |
| 11.7 | % | 11.1 | % |
Maturities of operating lease liabilities as of December 31, 2022 are as follows:
Year Ending December 31, |
| ||
2023 | $ | 1,082 | |
2024 |
| 3,212 | |
2025 |
| 3,382 | |
2026 |
| 2,836 | |
2027 |
| 2,599 | |
Thereafter |
| 6,539 | |
Total undiscounted future cash flows |
| 19,650 | |
Less: interest |
| (6,860) | |
Present value of operating lease liabilities | $ | 12,790 | |
The current portions of right-of-use liabilities of $1.6 million and $2.1 million are included in accrued expenses and other current liabilities in the Company’s consolidated balance sheets as of December 31, 2022 and 2021, respectively.
Supplemental cash flows and other information related to leases are as follows:
Successor | Predecessor | ||||||||||
Year Ended | December 3, 2021 | January 1, 2021 | |||||||||
December 31, | through December 31, | through December 2, | |||||||||
| 2022 |
| 2021 |
|
| 2021 |
| ||||
Operating cash flows paid for operating leases | $ | 3,339 | $ | 255 | $ | 2,256 | |||||
As of December 31, 2022, the Company had entered into an office space lease resulting in an aggregate lease commitment of $0.6 million during the five-year lease term, which commences on February 1, 2023.
Note 18: Retirement Plan
The Company maintains a retirement savings 401(k) Plan (the “401(k) Plan”) for full-time employees. Participants may elect to contribute to the 401(k) Plan, through payroll deductions, subject to Internal Revenue Service limitations. At its discretion, the Company can make a matching contribution to the 401(k) Plan. The Company recognized expense related to its contributions to the 401(k) Plan of $0.8 million during the year ended December 31, 2022. The Company did not any contributions to the 401(k) Plan in the Successor Period of 2021 and the Predecessor Period of 2021.
F-36
Note 19: Redeemable Non-controlling Interest
Non-controlling interest represents the portion of P3 LLC that the Company controls and consolidates but does not own (i.e., the Common Units held directly by equityholders other than the Company). The ownership of the Common Units is summarized as follows:
December 31, 2022 |
| December 31, 2021 |
| ||||||
| Units |
| Ownership % | Units |
| Ownership % | |||
P3 Health Partners Inc.’s ownership of Common Units |
| 41,578,890 |
| 17.1 | % | 41,578,890 |
| 17.5 | % |
Non-controlling interest holders’ ownership of Common Units |
| 201,592,012 |
| 82.9 | % | 196,553,523 |
| 82.5 | % |
Total Common Units |
| 243,170,902 |
| 100.0 | % | 238,132,413 |
| 100.0 | % |
Common Units participate in net income or loss allocations and distributions and entitle their holder to the right, subject to the terms set forth in the limited liability company agreement, to require the Company to redeem all or a portion of the Common Units held by such participant, together with a corresponding number of shares of Class V common stock, in exchange for Class A common stock or at the Company’s option, and subject to certain limitations, in cash. As the non-controlling interest holders had an approximate 83% voting interest in the Company through their Class V common stock as of the Closing Date and appointed most of the initial members to the Board of Directors, the ability to elect cash settlement upon redemption is outside of the control of the Company. As a result, the Common Units held by outside shareholders have been classified as redeemable non-controlling interest and presented as temporary equity in the Company’s consolidated balance sheets.
The redeemable non-controlling interest was initially measured at its fair value on December 3, 2021. Net income or loss is attributed to the redeemable non-controlling interest during each reporting period based on a daily weighted average ownership percentage. In subsequent periods, the redeemable non-controlling interest is measured at its fair value (i.e., based on the five-day volume-weighted average price of a share of Class A common stock) at the end of each reporting period, with the remeasurement amount being no less than the initial value, as adjusted for the redeemable non-controlling interest’s share of net income or loss and ownership changes. The offset of any fair value adjustment is recorded to equity, with no impact to net income or loss. As of December 31, 2022 and 2021, there was no remeasurement adjustment recorded as the fair value of redeemable non-controlling interest was lower than the initial value.
There was no Common Unit exchange or redemption activity during the year ended December 31, 2022 or Successor Period of 2021.
Note 20: Segment Reporting
The Company’s operations are organized under a single reportable segment. The Chief Executive Officer, who is the Company’s CODM, manages the Company’s operations and reviews financial information on a consolidated basis. Decisions regarding resource allocation and assessment of profitability are based on the Company’s responsibility to deliver high quality primary medical care services to its patient population. For the periods presented, all the Company’s revenue was earned in the United States. Likewise, all the Company’s long-lived assets were located in the United States.
Note 21: Commitments and Contingencies
The Company is a party to various claims, legal and regulatory proceedings, lawsuits, and administrative actions arising in the ordinary course of business and associated with the Business Combinations. The Company carries general and professional liability insurance coverage to mitigate the Company’s risk of potential loss in such cases. The Company believes that disposition of these matters will not have a material adverse effect on the Company’s consolidated financial position, net loss or cash flows.
F-37
In 2021, a discrepancy was identified in the service agreement with one of the Company’s health plans resulting in a renegotiation of the agreement. In the Predecessor Period of 2021, the Company recorded a $3.6 million reduction in operating revenue and a $7.0 million charge to operating expense to account for a probable settlement of $11.7 million within health plan settlements payable as of December 31, 2021. In January 2023, the renegotiation was settled and the Company recorded a $3.6 million increase in operating revenue and a $3.1 million reduction in operating expense during the year ended December 31, 2022 to reflect the known settlement of $5.0 million within health plan settlements payable as of December 31, 2022.
Uncertainties
The healthcare industry is subject to numerous laws and regulations of Federal, state, and local governments. These laws and regulations include, but are not limited to, matters of licensure, accreditation, government healthcare program participation requirements, reimbursement for patient services, and Medicare / Medicaid Fraud, Waste and Abuse Prevention. Recently, government activity has increased with respect to investigations and allegations concerning possible violations of Fraud, Waste and Abuse statutes and regulations by healthcare providers. Violations of these laws and regulations could result in expulsion from government healthcare programs together with imposition of significant fines and penalties as well as significant repayment for patient services billed.
Management believes the Company is compliant with Fraud, Waste and Abuse regulations as well as other applicable government laws. While no regulatory inquiries have been made, compliance with such laws and regulations is subject to government review and interpretation, as well as other regulatory actions which might be unknown at this time.
Healthcare reform legislation at both the Federal and state levels continues to evolve. Changes continue to impact existing and future laws and rules. Such changes may impact the manner in which the Company conducts business, restrict the Company’s revenue growth in certain eligibility categories, slow down revenue growth rates for certain eligibility categories, increase certain medical, administrative and capital costs, and expose the Company to increased risk of loss or further liabilities. As a result, the Company’s consolidated financial position could be impacted by such changes.
COVID-19 Pandemic
On March 11, 2020, the World Health Organization designated COVID-19 a global pandemic. The rapid spread of COVID-19 around the world and throughout the U.S. has altered the behavior of businesses and people, with significant negative effects on Federal, state, and local economies, the duration of which continues to remain unknown. Various mandates were implemented by Federal, state, and local governments in response to the pandemic, which caused many people to remain at home along with forced closure of or limitations on certain businesses. This included suspension of elective procedures by healthcare facilities. While some of these restrictions have been eased across the U.S. and most states have lifted moratoriums on non-emergent procedures, some restrictions remain in place, and many state and local governments are re-imposing certain restrictions due to an increase in reported COVID-19 cases. COVID-19 disproportionately impacts older adults, especially those with chronic illnesses, which describes many of the Company’s patients.
The COVID-19 pandemic did not have a material impact on the Company’s revenue for the years ended December 31, 2022 and 2021. Nearly 99% of the Company’s total revenue is recurring, consisting of fixed monthly PMPM capitation payments received from Medicare Advantage health plans. Management instituted multiple safety measures for the Company’s employees including a work-from-home policy and access to free vaccinations and personal protective equipment.
The full extent to which COVID-19 will directly or indirectly impact the Company, its future results of operations and financial condition will depend on factors which are highly uncertain and cannot be accurately predicted. This includes new and emerging information from the impact of new variants of the virus, the actions taken to contain it or treat its impact and the economic impact on the Company’s markets. Such factors include, but are not limited to, the scope and duration of stay-at-home practices and business closures and restrictions, government- imposed or recommended suspensions of elective procedures, and expenses required for supplies and personal protective equipment. Because of these and other uncertainties, Management cannot estimate the length or severity of the impact of the pandemic on the Company’s business. Furthermore, because of the Company’s business model, the full impact of COVID-19 may not be fully reflected in the Company’s results of operations and overall financial condition until future periods. However, Management will continue to closely evaluate and monitor the nature and extent of these potential impacts to the Company’s business, results of operations, and liquidity.
F-38
Note 22: Related Parties
Atrio Health Plans
Chicago Pacific Founders (“CPF”), a principal equity holder of P3 LLC, has an equity investment in Atrio Health Plans (“Atrio”). The Company has a full-risk capitation agreement in place with Atrio whereby the Company is delegated to perform services on behalf of Atrio’s members assigned to the Company. These delegated services include but are not limited to provider network credentialing, patient authorizations, and medical management (care management, quality management and utilization management). The following tables summarize the Company’s transactions with Atrio:
Successor |
|
| Predecessor | |||||||
| Year Ended |
| December 3, 2021 | January 1, 2021 | ||||||
December 31, | through December 31, | through December 2, | ||||||||
2022 | 2021 |
|
| 2021 | ||||||
Capitated revenue | $ | 158,941 | $ | 11,483 | $ | 142,905 | ||||
Other patient service revenue | $ | 2,286 | $ | 181 | $ | 2,022 | ||||
Medical expenses | $ | 178,300 | $ | 14,684 | $ | 146,216 | ||||
| December 31, | |||||
2022 |
| 2021 | ||||
Health plan receivables | $ | 177 | $ | 4,696 | ||
Claims payable | $ | 27,838 | $ | 16,349 | ||
Health plan settlements payable | $ | 2,536 | $ | — | ||
Unsecured Promissory Note
As described in Note 12, in December 2022, the Company issued an Unsecured Promissory Note to VGS, an entity managed by CPF and whose equity holders consist of two members of the Company’s Board of Directors and the Company’s Chief Executive Officer and Chief Medical Officer, among others. The following tables summarize the Company’s transactions with VGS:
| Year Ended | ||
December 31, | |||
2022 | |||
Interest expense, net | $ | 105 | |
| December 31, 2022 | ||
Long-term debt, net | $ | 14,421 | |
Accrued interest | $ | 105 | |
Accrued expenses | $ | 225 | |
Note 23: Variable Interest Entities
P3 LLC has Management Services Agreements (“MSAs”) and deficit funding agreements with the Network. The MSAs provide that the P3 LLC will furnish administrative personnel, office supplies and equipment, general business services, contract negotiation, and billing and collection services to the Network. Fees for these services are the excess of the Network’s revenue over expenses. Per the deficit funding agreements, P3 LLC is obligated to advance funds, as needed, to support the Network’s working capital needs to the extent operating expenses exceed gross revenue. These advances accrue interest at a rate of prime plus 2%. Net advances made to the Network and accrued interest on those advances are presented within due to consolidated entities of P3 in the table below. Additionally, P3 LLC entered into stock transfer restriction agreements with the practice shareholders of the Network, which, by way of a call option, unequivocally permit P3 LLC to appoint successor physicians if a practice shareholder vacates their ownership position. Accordingly, P3 LLC identifies itself as the primary beneficiary of the Network. Practice shareholders, who are employees of P3 LLC, retain equity ownership in the Network, which represents nominal non-controlling interests; however, the non-controlling interests do not participate in the profit or loss of the Network.
F-39
P3 LLC, directly or indirectly via its wholly owned subsidiaries, may not use or access any net assets of these VIEs to settle its obligations or the obligations of its wholly owned subsidiaries. Additionally, the creditors of the VIEs do not have recourse to the net assets of P3 LLC.
Since P3 LLC represents substantially all the assets and liabilities of the Company, the following tables provide a summary of the assets, liabilities, and operating performance of only VIEs held at the P3 LLC level.
December 31, | ||||||
2022 | 2021 | |||||
ASSETS | ||||||
Cash | $ | 1,759 | $ | 7,570 | ||
Clinic fees and insurance receivables, net |
| 323 |
| 61 | ||
Prepaid expenses and other current assets |
| 121 |
| 407 | ||
Other receivable | 855 | — | ||||
Property and equipment, net |
| 44 |
| 36 | ||
Goodwill | — | — | ||||
Due from consolidated entities of P3 | 3,012 | — | ||||
Investment in other P3 entities | — | 6,000 | ||||
TOTAL ASSETS | $ | 6,114 | $ | 14,074 | ||
LIABILITIES AND MEMBERS’ DEFICIT |
|
|
| |||
Accounts payable | $ | 7,800 | $ | 4,779 | ||
Accrued expenses and other current liabilities | 262 | 26 | ||||
Accrued payroll |
| 1,885 |
| 1,303 | ||
Due to consolidated entities of P3 |
| 36,025 |
| 24,111 | ||
TOTAL LIABILITIES |
| 45,972 |
| 30,219 | ||
MEMBERS’ DEFICIT |
| (39,858) |
| (16,145) | ||
TOTAL LIABILITIES AND MEMBERS’ DEFICIT | $ | 6,114 | $ | 14,074 | ||
Successor | Predecessor | |||||||||
Year Ended | December 3, 2021 | January 1, 2021 | ||||||||
December 31, | through December 31, | through December 2, | ||||||||
| 2022 |
| 2021 |
|
| 2021 | ||||
Revenue | $ | 55,237 | $ | 844 | $ | 7,580 | ||||
Expenses |
| 69,638 | 1,203 |
| 12,293 | |||||
Net loss | $ | (14,401) | $ | (359) | $ | (4,713) | ||||
F-40
Note 24: Warrants
As of December 31, 2022 and 2021, there were an aggregate of 11,248,285 and 10,819,105 warrants outstanding, respectively, which include the public warrants, private placement warrants, and VGS Warrants (as defined below).
Public and Private Placement Warrants
Each public and private placement warrant entitles the holder to purchase one share of Class A common stock at a price of $11.50 per share. The public warrants will expire five years after the completion of the Business Combinations. The Company has the right to redeem the public warrants when the price per share of Class A common stock equals or exceeds $18.00 for 20 days within a trading period. The private placement warrants are identical to the public warrants, except that the private placement warrants are subject to certain transfer restrictions, are not redeemable by the Company if they are held by Sponsors, and are exercisable on a cashless basis.
The public and private placement warrants are recorded as a liability on the consolidated balance sheets with a balance of $1.5 million and $11.4 million as of December 31, 2022 and 2021, respectively. The Company recorded a gain of $9.9 million, a gain of $2.3 million, and a loss of $7.7 million from the change in fair value of the warrants during the year ended December 31, 2022, the Successor Period of 2021, and the Predecessor Period of 2021, respectively. No exercised during the year ended December 31, 2022, the Successor Period of 2021, and the Predecessor Period of 2021.
VGS Warrants
In connection with the Unsecured Promissory Note issued in December 2022 (see Note 12 “Debt”), the Company and VGS entered into a warrant agreement (the “VGS Warrant Agreement”) pursuant to which the Company issued warrants to purchase 429,180 shares of Class A common stock of the Company at an exercise price of $4.26 per share to VGS (the “VGS Warrants”). The number of shares of common stock for which the VGS Warrants is exercisable and the exercise price may be adjusted upon any event involving subdivisions, combinations, distributions, recapitalizations, and similar transactions. Pursuant to the VGS Warrant Agreement, the warrants and the right to purchase securities upon the exercise of the warrants will terminate upon the earliest to occur of the following: (a) December 13, 2027; and (b) the consummation of (i) a sale, conveyance, consolidation with any other corporation (other than a wholly owned subsidiary corporation) or (ii) any other transaction or series of related transactions in which more than 50% of the voting power of which the Company or P3 LLC is disposed. The Company recorded the fair value of the VGS Warrants of $0.6 million as an increase to additional paid in capital during the year ended December 31, 2022.
The key Level 3 inputs into the option pricing model related to the VGS Warrants were as follows:
Volatility |
| 49 | % | |
Risk-free interest rate |
| 3.80 | % | |
Exercise price | $ | 4.26 |
| |
Expected term |
| 5.0 | Years |
F-41
Note 25: Subsequent Events
Between January and March 2023, the Company borrowed a total of $12.9 million under the Unsecured Promissory Note.
On March 30, 2023, the Company entered into a Securities Purchase Agreement with the purchasers named therein (the “Purchasers”), certain of which are related parties, pursuant to which the Company will issue approximately 79.9 million units at a price of approximately $1.12 per unit for institutional investors, and a purchase price of approximately $1.19 per unit for employees and consultants. Each unit consists of one share of Class A common stock and 0.75 of a warrant to purchase one share of Class A common stock at an exercise price of $1.13. Certain institutional investors have elected to receive pre-funded warrants to purchase Class A common stock in lieu of a portion of their Class A common stock. In total, the Company agreed to sell (i) an aggregate of approximately 69.2 million shares of its Class A common stock, (ii) warrants to purchase an aggregate of approximately 59.9 million shares of Class A common stock, and (iii) pre-funded warrants to purchase an aggregate of approximately 10.8 million shares of Class A common stock, to the Purchasers for aggregate gross proceeds of approximately $89.5 million (collectively, the “Private Placement”). The Private Placement is subject to certain conditions and is expected to close on April 6, 2023.
F-42
Similar companies
See also Oak Street Health, Inc. - Annual report 2022 (10-K 2022-12-31) Annual report 2023 (10-Q 2023-03-31)See also Privia Health Group, Inc. - Annual report 2022 (10-K 2022-12-31) Annual report 2024 (10-Q 2024-03-31)
See also LifeStance Health Group, Inc. - Annual report 2022 (10-K 2022-12-31) Annual report 2024 (10-Q 2024-06-30)
See also Agape ATP Corp - Annual report 2022 (10-K 2022-12-31) Annual report 2023 (10-Q 2023-09-30)
See also DocGo Inc. - Annual report 2022 (10-K 2022-12-31) Annual report 2023 (10-Q 2023-09-30)
